Low Bone Mineral Density on Computed Tomography: Association with Poor Survival after Transcatheter Aortic Valve Replacement
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Transcatheter Aortic Valve Replacement
2.3. Study Design
2.4. CT Assessment
2.5. Data Collection
2.6. Definition of Endpoints
2.7. Statistical Analysis
3. Results
3.1. Baseline Clinical Characteristics
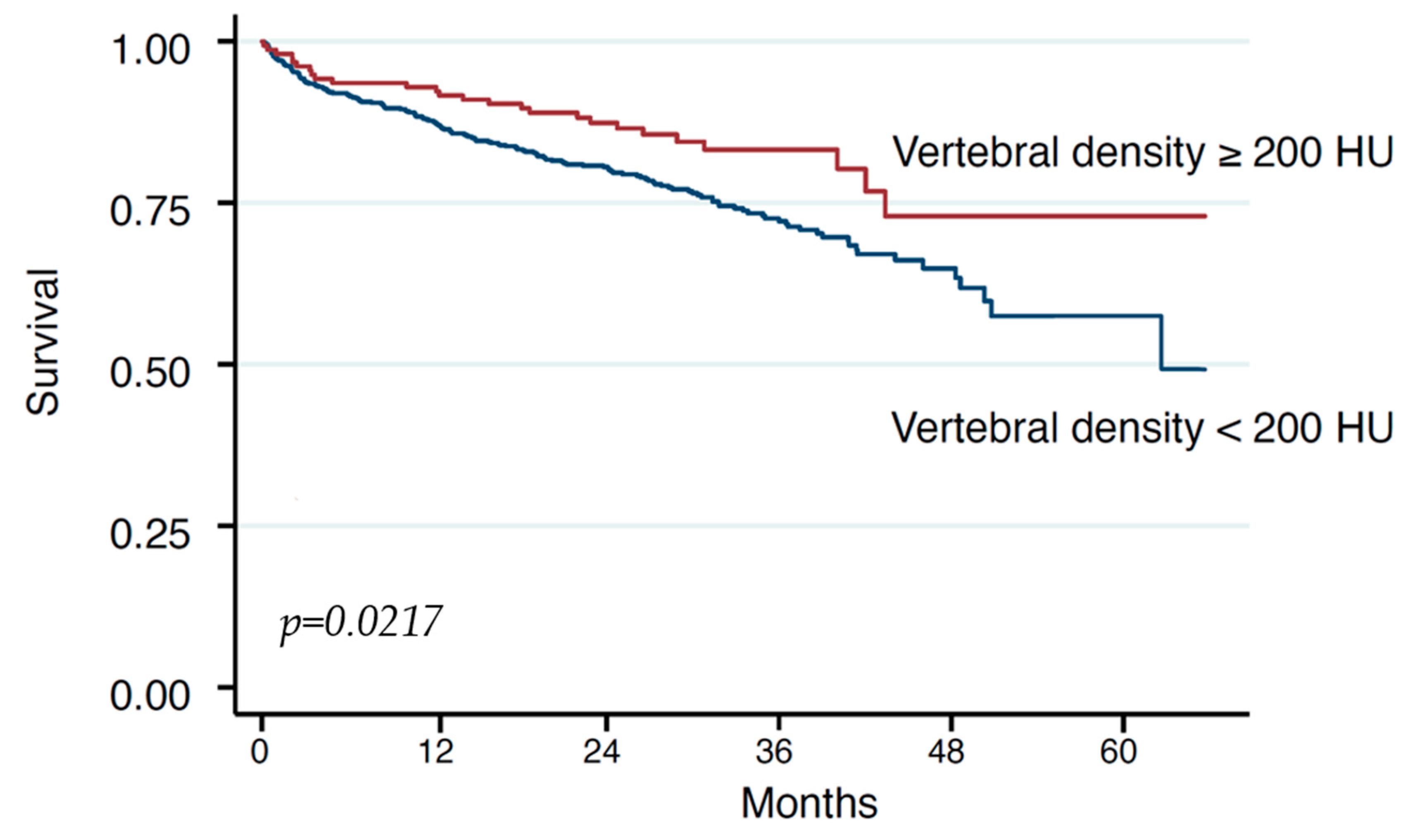
3.2. Survival
4. Discussion
5. Study Limitations and Future Directions
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TAVR | Transcatheter Aortic Valve Replacement |
| SAVR | Surgical Aortic Valve Replacement |
| BMD | Bone Mineral Density |
| OP | Osteoporosis |
| AS | Aortic Valve Stenosis |
| CT | Computed Tomography |
References
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Russo, M.; Kapadia, S.R.; Malaisrie, S.C.; Cohen, D.J.; Pibarot, P.; et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1695–1705. [Google Scholar] [CrossRef]
- Popma, J.J.; Deeb, G.M.; Yakubov, S.J.; Mumtaz, M.; Gada, H.; O’Hair, D.; Bajwa, T.; Heiser, J.C.; Merhi, W.; Kleiman, N.S.; et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1706–1715. [Google Scholar] [CrossRef]
- Reardon, M.J.; Van Mieghem, N.M.; Popma, J.J.; Kleiman, N.S.; Søndergaard, L.; Mumtaz, M.; Adams, D.H.; Deeb, G.M.; Maini, B.; Gada, H.; et al. Surgical or Transcatheter Aortic-Valve Replacement in Intermediate-Risk Patients. N. Engl. J. Med. 2017, 376, 1321–1331. [Google Scholar] [CrossRef]
- Leon, M.B.; Smith, C.R.; Mack, M.J.; Makkar, R.R.; Svensson, L.G.; Kodali, S.K.; Thourani, V.H.; Tuzcu, E.M.; Miller, D.C.; Herrmann, H.C.; et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N. Engl. J. Med. 2016, 374, 1609–1620. [Google Scholar] [CrossRef]
- Dowling, C.; Kondapally Seshasai, S.R.; Firoozi, S.; Brecker, S.J. Transcatheter aortic valve replacement versus surgery for symptomatic severe aortic stenosis: A reconstructed individual patient data meta-analysis. Catheter. Cardiovasc. Interv. 2020, 96, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Makkar, R.R.; Thourani, V.H.; Mack, M.J.; Kodali, S.K.; Kapadia, S.; Webb, J.G.; Yoon, S.H.; Trento, A.; Svensson, L.G.; Herrmann, H.C.; et al. Five-Year Outcomes of Transcatheter or Surgical Aortic-Valve Replacement. N. Engl. J. Med. 2020, 382, 799–809. [Google Scholar] [CrossRef]
- Demirel, C.; Rothenbühler, C.F.; Huber, M.; Schweizer, M.; Todorski, I.; Gloor, D.A.; Windecker, S.; Lanz, J.; Stortecky, S.; Pilgrim, T.; et al. Total Muscle Area and Visceral Adipose Tissue Measurements for Frailty Assessment in TAVR Patients. J. Clin. Med. 2024, 13, 1322. [Google Scholar] [CrossRef]
- Søndergaard, L.; Kirk, B.H.; Jørgensen, T.H. Frailty: An Important Measure in Patients Considered for Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2018, 11, 404–406. [Google Scholar] [CrossRef]
- Afilalo, J.; Lauck, S.; Kim, D.H.; Lefèvre, T.; Piazza, N.; Lachapelle, K.; Martucci, G.; Lamy, A.; Labinaz, M.; Peterson, M.D.; et al. Frailty in Older Adults Undergoing Aortic Valve Replacement: The FRAILTY-AVR Study. J. Am. Coll. Cardiol. 2017, 70, 689–700. [Google Scholar] [CrossRef]
- Ilic, I.; Faron, A.; Heimann, M.; Potthoff, A.L.; Schäfer, N.; Bode, C.; Borger, V.; Eichhorn, L.; Giordano, F.A.; Güresir, E.; et al. Combined Assessment of Preoperative Frailty and Sarcopenia Allows the Prediction of Overall Survival in Patients with Lung Cancer (NSCLC) and Surgically Treated Brain Metastasis. Cancers 2021, 13, 3353. [Google Scholar] [CrossRef]
- Bentov, I.; Kaplan, S.J.; Pham, T.N.; Reed, M.J. Frailty assessment: From clinical to radiological tools. Br. J. Anaesth. 2019, 123, 37–50. [Google Scholar] [CrossRef]
- Flexman, A.M.; Street, J.; Charest-Morin, R. The impact of frailty and sarcopenia on patient outcomes after complex spine surgery. Curr. Opin. Anaesthesiol. 2019, 32, 609–615. [Google Scholar] [CrossRef]
- Kołodziejska, K.; Witowski, J.; Tylec, P.; Grochowska, A.; Przytuła, N.; Lis, M.; Pędziwiatr, M.; Rubinkiewicz, M. Radiological Features for Frailty Assessment in Patients Requiring Emergency Laparotomy. J. Clin. Med. 2022, 11, 5365. [Google Scholar] [CrossRef]
- de Bree, R.; Meerkerk, C.D.A.; Halmos, G.B.; Mäkitie, A.A.; Homma, A.; Rodrigo, J.P.; López, F.; Takes, R.P.; Vermorken, J.B.; Ferlito, A. Measurement of Sarcopenia in Head and Neck Cancer Patients and Its Association with Frailty. Front. Oncol. 2022, 12, 884988. [Google Scholar] [CrossRef]
- Okamura, H.; Kimura, N.; Mieno, M.; Yuri, K.; Yamaguchi, A. Preoperative sarcopenia is associated with late mortality after off-pump coronary artery bypass grafting. Eur. J. Cardiothorac. Surg. 2020, 58, 121–129. [Google Scholar] [CrossRef]
- Canales, C.; Mazor, E.; Coy, H.; Grogan, T.R.; Duval, V.; Raman, S.; Cannesson, M.; Singh, S.P. Preoperative Point-of-Care Ultrasound to Identify Frailty and Predict Postoperative Outcomes: A Diagnostic Accuracy Study. Anesthesiology 2022, 136, 268–278. [Google Scholar] [CrossRef]
- Mamane, S.; Mullie, L.; Piazza, N.; Martucci, G.; Morais, J.; Vigano, A.; Levental, M.; Nelson, K.; Lange, R.; Afilalo, J. Psoas Muscle Area and All-Cause Mortality after Transcatheter Aortic Valve Replacement: The Montreal-Munich Study. Can. J. Cardiol. 2016, 32, 177–182. [Google Scholar] [CrossRef]
- Saji, M.; Lim, D.S.; Ragosta, M.; LaPar, D.J.; Downs, E.; Ghanta, R.K.; Kern, J.A.; Dent, J.M.; Ailawadi, G. Usefulness of Psoas Muscle Area to Predict Mortality in Patients Undergoing Transcatheter Aortic Valve Replacement. Am. J. Cardiol. 2016, 118, 251–257. [Google Scholar] [CrossRef]
- Mok, M.; Allende, R.; Leipsic, J.; Altisent, O.A.; Del Trigo, M.; Campelo-Parada, F.; DeLarochellière, R.; Dumont, E.; Doyle, D.; Côté, M.; et al. Prognostic Value of Fat Mass and Skeletal Muscle Mass Determined by Computed Tomography in Patients Who Underwent Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2016, 117, 828–833. [Google Scholar] [CrossRef]
- Okuno, T.; Koseki, K.; Nakanishi, T.; Ninomiya, K.; Tomii, D.; Tanaka, T.; Sato, Y.; Osanai, A.; Sato, K.; Koike, H.; et al. Prognostic Impact of Computed Tomography-Derived Abdominal Fat Area on Transcatheter Aortic Valve Implantation. Circ. J. 2018, 82, 3082–3089. [Google Scholar] [CrossRef]
- Rodríguez, A.J.; Scott, D.; Hodge, A.; English, D.R.; Giles, G.G.; Ebeling, P.R. Associations between hip bone mineral density, aortic calcification and cardiac workload in community-dwelling older Australians. Osteoporos. Int. 2017, 28, 2239–2245. [Google Scholar] [CrossRef]
- Shi, L.; Yu, X.; Pang, Q.; Chen, X.; Wang, C. The associations between bone mineral density and long-term risks of cardiovascular disease, cancer, and all-cause mortality. Front. Endocrinol. 2022, 13, 938399. [Google Scholar] [CrossRef]
- Johansson, H.; Odén, A.; Kanis, J.; McCloskey, E.; Lorentzon, M.; Ljunggren, Ö.; Karlsson, M.K.; Orwoll, E.; Tivesten, Å.; Ohlsson, C.; et al. Low bone mineral density is associated with increased mortality in elderly men: MrOS Sweden. Osteoporos. Int. 2011, 22, 1411–1418. [Google Scholar] [CrossRef]
- Sandberg, C.; Johansson, K.; Christersson, C.; Hlebowicz, J.; Thilén, U.; Johansson, B. Low bone mineral density in adults with complex congenital heart disease. Int. J. Cardiol. 2020, 319, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Jha, S.; Chapman, M.; Roszko, K. When Low Bone Mineral Density and Fractures Is Not Osteoporosis. Curr. Osteoporos. Rep. 2019, 17, 324–332. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Thabane, L.; Papaioannou, A.; Ioannidis, G.; Levine, M.A.; Adachi, J.D. An overview of osteoporosis and frailty in the elderly. BMC Musculoskelet. Disord. 2017, 18, 46. [Google Scholar] [CrossRef]
- Laskou, F.; Fuggle, N.R.; Patel, H.P.; Jameson, K.; Cooper, C.; Dennison, E. Associations of osteoporosis and sarcopenia with frailty and multimorbidity among participants of the Hertfordshire Cohort Study. J. Cachexia Sarcopenia Muscle 2022, 13, 220–229. [Google Scholar] [CrossRef]
- Suzuki, T.; Yoshida, H. Low bone mineral density at femoral neck is a predictor of increased mortality in elderly Japanese women. Osteoporos. Int. 2010, 21, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Lane, N.E. Epidemiology, etiology, and diagnosis of osteoporosis. Am. J. Obstet. Gynecol. 2006, 194, S3–S11. [Google Scholar] [CrossRef]
- Pickhardt, P.J.; Pooler, B.D.; Lauder, T.; del Rio, A.M.; Bruce, R.J.; Binkley, N. Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann. Intern. Med. 2013, 158, 588–595. [Google Scholar] [CrossRef]
- Lee, S.J.; Binkley, N.; Lubner, M.G.; Bruce, R.J.; Ziemlewicz, T.J.; Pickhardt, P.J. Opportunistic screening for osteoporosis using the sagittal reconstruction from routine abdominal CT for combined assessment of vertebral fractures and density. Osteoporos. Int. 2016, 27, 1131–1136. [Google Scholar] [CrossRef]
- Colantonio, D.F.; Saxena, S.K.; Vanier, A.; Rodkey, D.; Tintle, S.; Wagner, S.C. Cervical Spine Computed Tomography Hounsfield Units Accurately Predict Low Bone Mineral Density of the Femoral Neck. Clin. Spine Surg. 2020, 33, e58–e62. [Google Scholar] [CrossRef]
- Therkildsen, J.; Nissen, L.; Jørgensen, H.S.; Thygesen, J.; Ivarsen, P.; Frost, L.; Isaksen, C.; Langdahl, B.L.; Hauge, E.M.; Boettcher, M.; et al. Thoracic Bone Mineral Density Derived from Cardiac CT Is Associated with Greater Fracture Rate. Radiology 2020, 296, 499–508. [Google Scholar] [CrossRef]
- Francone, M.; Budde, R.P.J.; Bremerich, J.; Dacher, J.N.; Loewe, C.; Wolf, F.; Natale, L.; Pontone, G.; Redheuil, A.; Vliegenthart, R.; et al. CT and MR imaging prior to transcatheter aortic valve implantation: Standardisation of scanning protocols, measurements and reporting-a consensus document by the European Society of Cardiovascular Radiology (ESCR). Eur. Radiol. 2020, 30, 2627–2650. [Google Scholar] [CrossRef]
- Meng, N.H.; Li, C.I.; Liu, C.S.; Lin, W.Y.; Lin, C.H.; Chang, C.K.; Li, T.C.; Lin, C.C. Sarcopenia Defined by Combining Height- and Weight-Adjusted Skeletal Muscle Indices is Closely Associated with Poor Physical Performance. J. Aging Phys. Act. 2015, 23, 597–606. [Google Scholar] [CrossRef]
- Ferreira Poloni, P.; Vespoli, H.L.; Almeida-Filho, B.S.; Bueloni-Dias, F.; Nahas-Neto, J.; Nahas, E.A.P. Low bone mineral density is associated with breast cancer in postmenopausal women: A case-control study. Climacteric 2017, 20, 491–497. [Google Scholar] [CrossRef]
- Watanabe, J.; Saitsu, A.; Miki, A.; Kotani, K.; Sata, N. Prognostic value of preoperative low bone mineral density in patients with digestive cancers: A systematic review and meta-analysis. Arch. Osteoporos. 2022, 17, 33. [Google Scholar] [CrossRef]
- Aspray, T.J.; Hill, T.R. Osteoporosis and the Ageing Skeleton. Subcell. Biochem. 2019, 91, 453–476. [Google Scholar] [CrossRef]
- Rinonapoli, G.; Ruggiero, C.; Meccariello, L.; Bisaccia, M.; Ceccarini, P.; Caraffa, A. Osteoporosis in Men: A Review of an Underestimated Bone Condition. Int. J. Mol. Sci. 2021, 22, 2105. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Gao, H.; Zhao, L.; Wang, J. Osteoporosis in COPD patients: Risk factors and pulmonary rehabilitation. Clin. Respir. J. 2022, 16, 487–496. [Google Scholar] [CrossRef]
- Chen, Y.W.; Ramsook, A.H.; Coxson, H.O.; Bon, J.; Reid, W.D. Prevalence and Risk Factors for Osteoporosis in Individuals with COPD: A Systematic Review and Meta-analysis. Chest 2019, 156, 1092–1110. [Google Scholar] [CrossRef]
- Khandkar, C.; Vaidya, K.; Karimi Galougahi, K.; Patel, S. Low bone mineral density and coronary artery disease: A systematic review and meta-analysis. Int. J. Cardiol. Heart Vasc. 2021, 37, 100891. [Google Scholar] [CrossRef]


| Total | HU < 200 | HU ≥ 200 | p-Value | |
|---|---|---|---|---|
| n = 770 | n = 614 | n = 156 | ||
| Demographics | ||||
| Age | 80.7 (6.7) | 81.0 (6.5) | 79.5 (7.6) | 0.009 |
| Sex (male) | 54.0% | 52.0% | 62.2% | 0.022 |
| Height | 167.3 (9.7) | 167.1 (9.8) | 168.1 (9.5) | 0.38 |
| Weight | 77.7 (16.9) | 77.0 (16.8) | 80.9 (17.1) | 0.055 |
| BMI kg/m2 | 27.7 (5.4) | 27.5 (5.4) | 28.6 (5.4) | 0.11 |
| Euro score II | 4.8 (3.5) | 4.8 (3.8) | 4.7 (1.6) | 0.79 |
| LVEF (%) | 56.7 (12.9) | 57.0 (13.1) | 55.5 (11.8) | 0.21 |
| Comorbidities | ||||
| AF before TAVR | 22.4% | 21.2% | 27.6% | 0.33 |
| Diabetes | 25.3% | 24.3% | 29.4% | 0.21 |
| Hypertension | 57.4% | 58.4% | 53.1% | 0.25 |
| Smoking | 3.0% | 3.1% | 2.8% | 0.87 |
| PAD | 6.8% | 6.6% | 7.7% | 0.65 |
| CVD | 1.4% | 1.7% | 0.0% | 0.12 |
| CHF | 19.0% | 19.9% | 15.4% | 0.22 |
| CAD | 51.6% | 52.5% | 48.3% | 0.37 |
| CVI | 10.8% | 11.4% | 8.4% | 0.30 |
| CABG | 5.9% | 5.8% | 6.3% | 0.81 |
| COPD | 8.3% | 8.5% | 7.7% | 0.76 |
| Cancer | 14.5% | 15.4% | 10.5% | 0.13 |
| Laboratory findings | ||||
| Creatinin mg/dL | 1.3 (0.8) | 1.3 (0.8) | 1.3 (0.8) | 0.94 |
| Triglycerides mg/dL | 110.4 (57.1) | 109.5 (58.6) | 114.0 (50.6) | 0.41 |
| Cholesterol mg/dL | 144.1 (42.6) | 144.4 (43.3) | 142.7 (39.5) | 0.66 |
| HDL-C mg/dL | 55.1 (16.6) | 55.7 (17.1) | 52.6 (14.3) | 0.061 |
| LDL-C mg/dL | 74.6 (34.7) | 75.6 (35.3) | 70.3 (31.9) | 0.14 |
| Bilirubin mg/dL | 0.7 (0.5) | 0.6 (0.5) | 0.7 (0.4) | 0.59 |
| GOT U/L | 30.0 (72.4) | 30.8 (80.1) | 26.6 (18.3) | 0.53 |
| GPT U/L | 26.4 (53.4) | 27.3 (59.0) | 22.9 (15.9) | 0.37 |
| Hemoglobin g/dL | 12.1 (1.9) | 12.0 (2.0) | 12.3 (1.9) | 0.14 |
| INR | 1.1 (0.2) | 1.1 (0.2) | 1.1 (0.2) | 0.70 |
| Thrombocytes G/L | 218.1 (74.6) | 218.3 (75.7) | 217.0 (69.8) | 0.85 |
| HbA1c % | 6.0 (0.9) | 5.9 (0.9) | 6.1 (0.9) | 0.12 |
| NTproBNP pg/mL | 4286.8 (6158.1) | 4407.9 (6317.0) | 3773.4 (5425.0) | 0.29 |
| CT bone density | ||||
| Average HU in thoracal vertebra | 147.5 (75.4) | 120.0 (44.8) | 255.8 (73.8) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Demirel, C.; Halavina, K.; Hamzaraj, K.; Klement, J.; El-Shaer, M.; Hemetsberger, R.; Winter, M.P.; Koschatko, S.; Jantsch, C.; Andreas, M.; et al. Low Bone Mineral Density on Computed Tomography: Association with Poor Survival after Transcatheter Aortic Valve Replacement. J. Clin. Med. 2024, 13, 2698. https://doi.org/10.3390/jcm13092698
Demirel C, Halavina K, Hamzaraj K, Klement J, El-Shaer M, Hemetsberger R, Winter MP, Koschatko S, Jantsch C, Andreas M, et al. Low Bone Mineral Density on Computed Tomography: Association with Poor Survival after Transcatheter Aortic Valve Replacement. Journal of Clinical Medicine. 2024; 13(9):2698. https://doi.org/10.3390/jcm13092698
Chicago/Turabian StyleDemirel, Caglayan, Kseniya Halavina, Kevin Hamzaraj, Johanna Klement, Manar El-Shaer, Rayyan Hemetsberger, Max Paul Winter, Sophia Koschatko, Charlotte Jantsch, Martin Andreas, and et al. 2024. "Low Bone Mineral Density on Computed Tomography: Association with Poor Survival after Transcatheter Aortic Valve Replacement" Journal of Clinical Medicine 13, no. 9: 2698. https://doi.org/10.3390/jcm13092698







