Molecular Role of Protein Phosphatases in Alzheimer’s and Other Neurodegenerative Diseases
Abstract
:1. Introduction
| Protein Name | Amino Acid | Coding Gene | Disease | Ref | ||
|---|---|---|---|---|---|---|
| PP1 | 330 | PPP1CA | AD, Parkinson disease (PD), Huntington’s disease (HD), Schizophrenia | [20,21,22,23] | ||
| PP2A | Structural | 595 | Structural | PPP2R1A | AD, PD, Down syndrome, Frontotemporal dementia, Glioblastoma multiforme | [24,25,26,27,28,29,30] |
| Catalytic | 309–310 | Catalytic | PPP2CA | |||
| Regulatory | 285–595 | Regulatory | PPP2R2A PPP2R2B PPP2R2C PPP2R3A PPP2R3B PPP2R5A PPP2R5B PPP2R5C PPP2R5D | |||
| PP2B | 526 | PPP3CA | AD, PD, HD Schizophrenia | [31,32,33] | ||
| PP4 | Catalytic | 320 | Catalytic | PPP4C | AD | [34] |
| Regulatory | 1700, 500 | Regulatory | PPP4R2 PPP4R3 | |||
| PP5 | 525 | PPP5C | AD, PD, HD | [35,36] | ||
| PP6 | Catalytic | 348 | Catalytic | PPP6C | AD, PD | [34,37] |
| Regulatory | 343, 382 | Regulatory | PPP6R1 PPP6R2 | |||
| PP7 | 653 | PPM1G | Retinitis Pigmentosa Retinoblastoma | [38] | ||
2. Protein Phosphatases and Their Involvement in AD
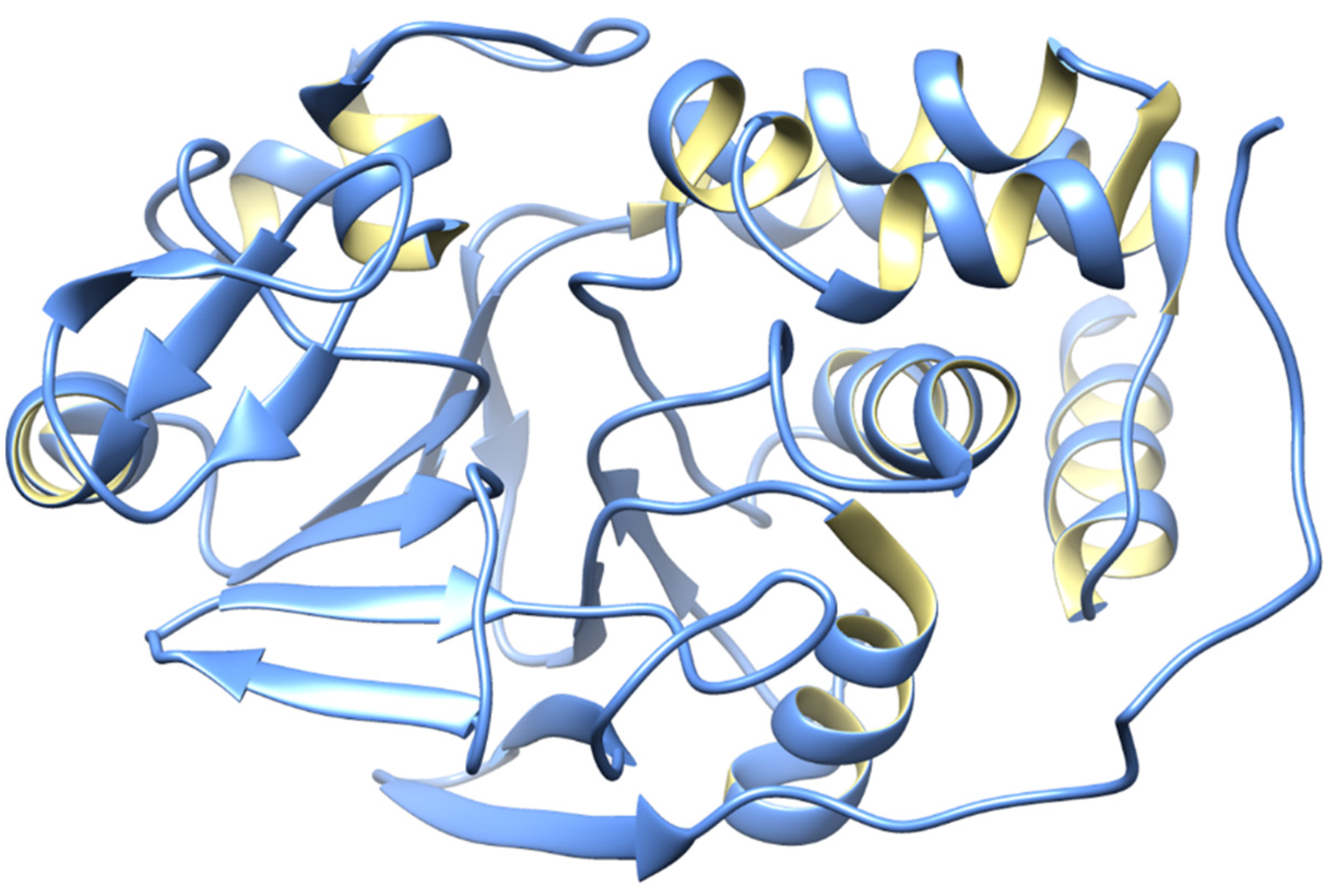
2.1. Protein Phosphatase 1 (PP1)
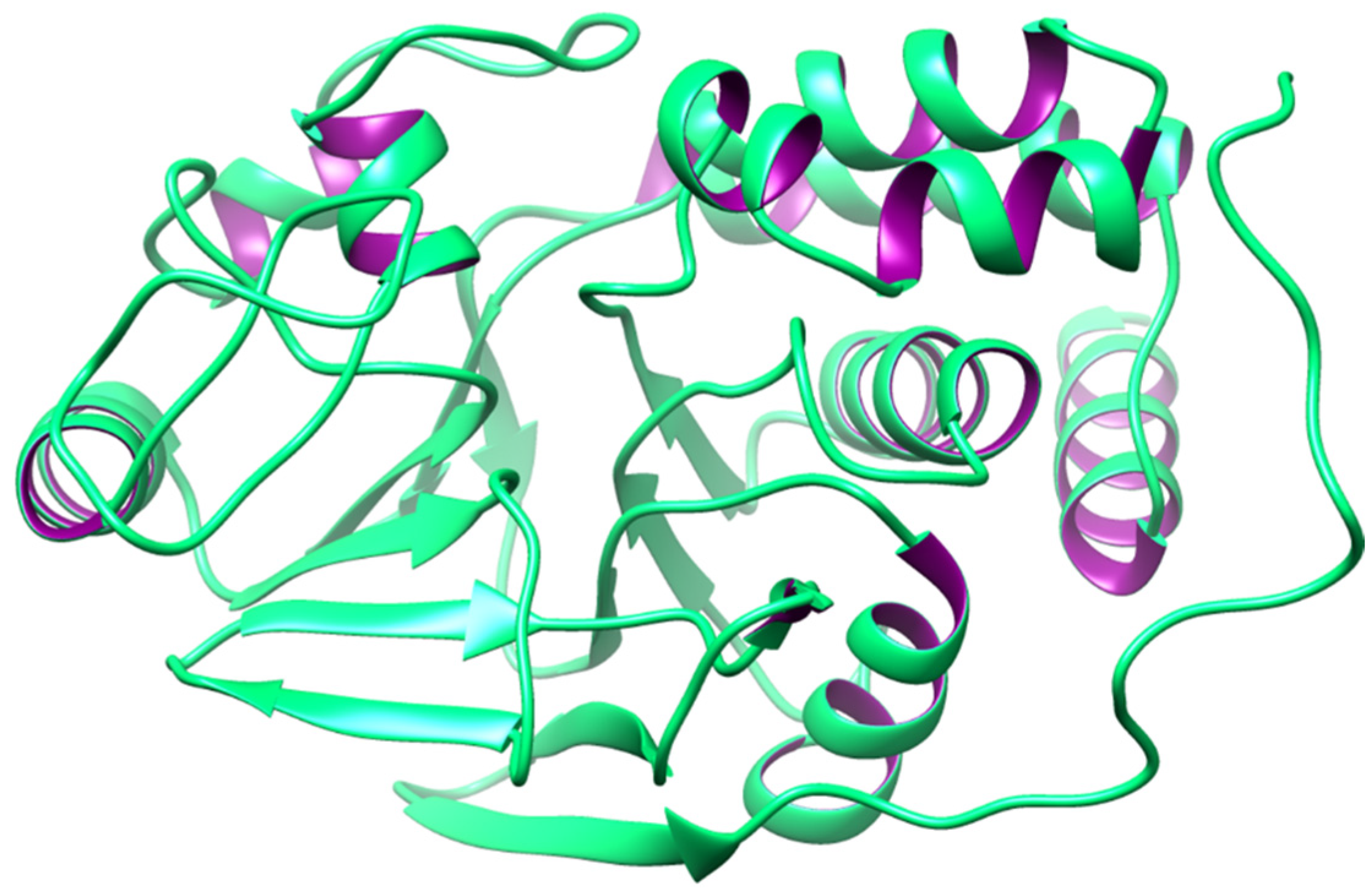
2.2. Protein Phosphatase 2A (PP2A)
2.3. Protein Phosphatase 2B (PP2B)
2.4. Protein Phosphatase 3 (PP3)
2.5. Protein Phosphatase 4 (PP4)
2.6. Protein Phosphatase 5 (PP5)
2.7. Protein Phosphatase 6 (PP6)
2.8. Protein Phosphatases 7 (PP7)
3. Pharmacological Agents Directly Targeting PP Receptors
3.1. Lithium
3.2. Okadaic Acid (OKA)
3.3. Cantharidin, Cyclosporine A, and Tideglusib
3.4. CIGB-300, Anle138b, LB-100, and Salubrinal
3.5. AV-1451 and Fingolimod
4. Conclusions and Future Prospects
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Seok, S.-H. Structural insights into protein regulation by phosphorylation and substrate recognition of protein kinases/phosphatases. Life 2021, 11, 957. [Google Scholar] [CrossRef] [PubMed]
- Choy, M.S.; Hieke, M.; Kumar, G.S.; Lewis, G.R.; Gonzalez-DeWhitt, K.R.; Kessler, R.P.; Stein, B.J.; Hessenberger, M.; Nairn, A.C.; Peti, W. Understanding the antagonism of retinoblastoma protein dephosphorylation by PNUTS provides insights into the PP1 regulatory code. Proc. Natl. Acad. Sci. USA 2014, 111, 4097–4102. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.J.; Yaffe, M.B. Protein Regulation in Signal Transduction. Cold Spring Harb. Perspect. Biol. 2016, 8, a005918. [Google Scholar] [CrossRef] [PubMed]
- Manning, G.; Plowman, G.D.; Hunter, T.; Sudarsanam, S. Evolution of protein kinase signaling from yeast to man. Trends Biochem. Sci. 2002, 27, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.T. Novel protein serine/threonine phosphatases: Variety is the spice of life. Trends Biochem. Sci. 1997, 22, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Denu, J.M.; Dixon, J.E. Protein tyrosine phosphatases: Mechanisms of catalysis and regulation. Curr. Opin. Chem. Biol. 1998, 2, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Janssens, V.; Goris, J. Protein phosphatase 2A: A highly regulated family of serine/threonine phosphatases implicated in cell growth and signalling. Biochem. J. 2001, 353, 417–439. [Google Scholar] [CrossRef] [PubMed]
- Ceulemans, H.; Bollen, M. Functional diversity of protein phosphatase-1, a cellular economizer and reset button. Physiol. Rev. 2004, 84, 1–39. [Google Scholar] [CrossRef] [PubMed]
- Honkanen, R.; Golden, T. Regulators of serine/threonine protein phosphatases at the dawn of a clinical era? Curr. Med. Chem. 2002, 9, 2055–2075. [Google Scholar] [CrossRef]
- Li, R.; Liu, Y. Physical activity and prevention of Alzheimer’s disease. J. Sport Health Sci. 2016, 5, 381–382. [Google Scholar] [CrossRef]
- Zissimopoulos, J.; Crimmins, E.; St. Clair, P. The value of delaying Alzheimer’s disease onset. Forum Health Econ. Policy 2015, 18, 25–39. [Google Scholar] [CrossRef]
- Werner, P. Like beauty and contact lenses, the meaning of dementia behavioral changes is in the eyes of the beholder. Int. Psychogeriatr. 2023, 35, 59–61. [Google Scholar] [CrossRef] [PubMed]
- Insel, K.C.; Badger, T.A. Deciphering the 4 D’s: Cognitive decline, delirium, depression and dementia–a review. J. Adv. Nurs. 2002, 38, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, A.A.; Hassan, M.; Hewedi, D.H.; Hewedi, I.; Garami, J.K.; Al Ashwal, H.; Zaki, N.; Seo, S.-Y.; Cutsuridis, V.; Angulo, S.L. Genetic underpinnings in Alzheimer’s disease–a review. Rev. Neurosci. 2018, 29, 21–38. [Google Scholar] [CrossRef]
- Isik, A.T. Late onset Alzheimer’s disease in older people. Clin. Interv. Aging 2010, 5, 307–311. [Google Scholar] [CrossRef]
- Wang, J.-Z.; Wang, Z.-H.; Tian, Q. Tau hyperphosphorylation induces apoptotic escape and triggers neurodegeneration in Alzheimer’s disease. Neurosci. Bull. 2014, 30, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Wang, Z.; Cai, F.; Zhang, M.; Wu, Y.; Zhang, J.; Song, W. BACE1 cleavage site selection critical for amyloidogenesis and Alzheimer’s pathogenesis. J. Neurosci. 2017, 37, 6915–6925. [Google Scholar] [CrossRef]
- Gong, C.X.; Shaikh, S.; Wang, J.Z.; Zaidi, T.; Grundke-Iqbal, I.; Iqbal, K. Phosphatase activity toward abnormally phosphorylated τ: Decrease in Alzheimer disease brain. J. Neurochem. 1995, 65, 732–738. [Google Scholar] [CrossRef]
- Wang, J.-z.; Wu, Q.; Smith, A.; Grundke-Iqbal, I.; Iqbal, K.J.F.l. τ is phosphorylated by GSK-3 at several sites found in Alzheimer disease and its biological activity markedly inhibited only after it is prephosphorylated by A-kinase. FEBS Lett. 1998, 436, 28–34. [Google Scholar] [CrossRef]
- Vintém, A.P.B.; Henriques, A.G.; e Silva, O.A.d.C.; e Silva, E.F.d.C. PP1 inhibition by Aβ peptide as a potential pathological mechanism in Alzheimer’s disease. Neurotoxicol. Teratol. 2009, 31, 85–88. [Google Scholar] [CrossRef]
- Cankara, F.N.; Kuş, M.S.; Günaydın, C.; Şafak, S.; Bilge, S.S.; Ozmen, O.; Tural, E.; Kortholt, A. The beneficial effect of salubrinal on neuroinflammation and neuronal loss in intranigral LPS-induced hemi-Parkinson disease model in rats. Immunopharmacol. Immunotoxicol. 2022, 44, 168–177. [Google Scholar] [CrossRef]
- Lontay, B.; Kiss, A.; Virág, L.; Tar, K. How do post-translational modifications influence the pathomechanistic landscape of Huntington’s disease? A comprehensive review. Int. J. Mol. Sci. 2020, 21, 4282. [Google Scholar] [CrossRef]
- Li, M.-L.; Peng, Y.; An, Y.; Li, G.-Y.; Lan, Y. LY395756 promotes NR2B expression via activation of AKT/CREB signaling in the juvenile methylazoxymethanol mice model of schizophrenia. Brain Behav. 2022, 12, e2466. [Google Scholar] [CrossRef]
- Leslie, S.N.; Nairn, A.C. cAMP regulation of protein phosphatases PP1 and PP2A in brain. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2019, 1866, 64–73. [Google Scholar] [CrossRef]
- Wei, H.; Zhang, H.-l.; Wang, X.-c.; Xie, J.-z.; An, D.-d.; Wan, L.; Wang, J.-z.; Zeng, Y.; Shu, X.-j.; Westermarck, J. Direct activation of protein phosphatase 2A (PP2A) by tricyclic sulfonamides ameliorates Alzheimer’s disease pathogenesis in cell and animal models. Neurotherapeutics 2020, 17, 1087–1103. [Google Scholar] [CrossRef] [PubMed]
- Su, J.; Zhang, J.; Bao, R.; Xia, C.; Zhang, Y.; Zhu, Z.; Lv, Q.; Qi, Y.; Xue, J. Mitochondrial dysfunction and apoptosis are attenuated through activation of AMPK/GSK-3β/PP2A pathway in Parkinson’s disease. Eur. J. Pharmacol. 2021, 907, 174202. [Google Scholar] [CrossRef] [PubMed]
- Javadpour, P.; Dargahi, L.; Ahmadiani, A.; Ghasemi, R. To be or not to be: PP2A as a dual player in CNS functions, its role in neurodegeneration, and its interaction with brain insulin signaling. Cell. Mol. Life Sci. 2019, 76, 2277–2297. [Google Scholar] [CrossRef]
- Di Domenico, F.; Tramutola, A.; Barone, E.; Lanzillotta, C.; Defever, O.; Arena, A.; Zuliani, I.; Foppoli, C.; Iavarone, F.; Vincenzoni, F. Restoration of aberrant mTOR signaling by intranasal rapamycin reduces oxidative damage: Focus on HNE-modified proteins in a mouse model of down syndrome. Redox Biol. 2019, 23, 101162. [Google Scholar] [CrossRef] [PubMed]
- Caberlotto, L.; Nguyen, T.-P. A systems biology investigation of neurodegenerative dementia reveals a pivotal role of autophagy. BMC Syst. Biol. 2014, 8, 65. [Google Scholar] [CrossRef]
- Hofstetter, C.P.; Burkhardt, J.-K.; Shin, B.J.; Gürsel, D.B.; Mubita, L.; Gorrepati, R.; Brennan, C.; Holland, E.C.; Boockvar, J.A. Protein phosphatase 2A mediates dormancy of glioblastoma multiforme-derived tumor stem-like cells during hypoxia. PLoS ONE 2012, 7, e30059. [Google Scholar] [CrossRef]
- Martin, L.; Latypova, X.; Wilson, C.M.; Magnaudeix, A.; Perrin, M.-L.; Terro, F. Tau protein phosphatases in Alzheimer’s disease: The leading role of PP2A. Ageing Res. Rev. 2013, 12, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Anantharam, V.; Lehrmann, E.; Kanthasamy, A.; Yang, Y.; Banerjee, P.; Becker, K.G.; Freed, W.J.; Kanthasamy, A.G. Microarray analysis of oxidative stress regulated genes in mesencephalic dopaminergic neuronal cells: Relevance to oxidative damage in Parkinson’s disease. Neurochem. Int. 2007, 50, 834–847. [Google Scholar] [CrossRef]
- Sawant, N.; Reddy, P.H. Role of phosphorylated Tau and glucose synthase kinase 3 beta in Huntington’s disease progression. J. Alzheimer’s Dis. 2019, 72, S177–S191. [Google Scholar] [CrossRef] [PubMed]
- Ohama, T. The multiple functions of protein phosphatase 6. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2019, 1866, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.-L.; Wang, X.-C.; Liu, R. Zinc in Regulating Protein Kinases and Phosphatases in Neurodegenerative Diseases. Biomolecules 2022, 12, 785. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Ortiz, E.; Hahm, B.K.; Armstrong, D.L.; Rossie, S. Protein phosphatase 5 protects neurons against amyloid-beta toxicity. J. Neurochem. 2009, 111, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Kitamura, N.; Fujiwara, N.; Hayakawa, K.; Ohama, T.; Sato, K. Protein phosphatase 6 promotes neurite outgrowth by promoting mTORC2 activity in N2a cells. J. Biochem. 2021, 170, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, K. Analysis of the Structure and Function of Protein Phosphatase 2A. Ph.D. Thesis, University of Basel, Basel, Switzerland, 2004. [Google Scholar]
- Wang, B.; Zhang, P.; Wei, Q. Recent progress on the structure of Ser/Thr protein phosphatases. Sci. China Ser. C Life Sci. 2008, 51, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Govindarajulu, M.; Pinky, P.D.; Bloemer, J.; Ghanei, N.; Suppiramaniam, V.; Amin, R. Signaling mechanisms of selective PPARγ modulators in Alzheimer’s disease. PPAR Res. 2018, 2018, 2010675. [Google Scholar] [CrossRef]
- Liu, F.; Grundke-Iqbal, I.; Iqbal, K.; Gong, C.X. Contributions of protein phosphatases PP1, PP2A, PP2B and PP5 to the regulation of tau phosphorylation. Eur. J. Neurosci. 2005, 22, 1942–1950. [Google Scholar] [CrossRef]
- da Cruz e Silva, E.F.; da Cruz e Silva, O.A.; Zaia, C.T.B.; Greengard, P. Inhibition of protein phosphatase 1 stimulates secretion of Alzheimer amyloid precursor protein. Mol. Med. 1995, 1, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Perluigi, M.; Barone, E.; Di Domenico, F.; Butterfield, D. Aberrant protein phosphorylation in Alzheimer disease brain disturbs pro-survival and cell death pathways. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2016, 1862, 1871–1882. [Google Scholar] [CrossRef] [PubMed]
- Belmeguenai, A.; Hansel, C. A role for protein phosphatases 1, 2A, and 2B in cerebellar long-term potentiation. J. Neurosci. 2005, 25, 10768–10772. [Google Scholar] [CrossRef] [PubMed]
- Ishida, A.; Shigeri, Y.; Taniguchi, T.; Kameshita, I. Protein phosphatases that regulate multifunctional Ca2+/calmodulin-dependent protein kinases: From biochemistry to pharmacology. Pharmacol. Ther. 2003, 100, 291–305. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.X.; Paudel, H.K. Ser67-phosphorylated inhibitor 1 is a potent protein phosphatase 1 inhibitor. Proc. Natl. Acad. Sci. USA 2000, 97, 5824–5829. [Google Scholar] [CrossRef] [PubMed]
- Antunes, G.; Roque, A.C.; Simoes-de-Souza, F. Stochastic induction of long-term potentiation and long-term depression. Sci. Rep. 2016, 6, 30899. [Google Scholar] [CrossRef] [PubMed]
- Foley, K.; McKee, C.; Nairn, A.C.; Xia, H. Regulation of synaptic transmission and plasticity by protein phosphatase 1. J. Neurosci. 2021, 41, 3040–3050. [Google Scholar] [CrossRef] [PubMed]
- Gong, C.X.; Singh, T.J.; Grundke-Iqbal, I.; Iqbal, K. Phosphoprotein phosphatase activities in Alzheimer disease brain. J. Neurochem. 1993, 61, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Farkas, I.; Dombradi, V.; Miskei, M.; Szabados, L.; Koncz, C. Arabidopsis PPP family of serine/threonine phosphatases. Trends Plant Sci. 2007, 12, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Chiang, D.Y.; Heck, A.J.; Dobrev, D.; Wehrens, X.H. Regulating the regulator: Insights into the cardiac protein phosphatase 1 interactome. J. Mol. Cell. Cardiol. 2016, 101, 165–172. [Google Scholar] [CrossRef]
- Chiang, D.Y.; Alsina, K.M.; Corradini, E.; Fitzpatrick, M.; Ni, L.; Lahiri, S.K.; Reynolds, J.O.; Pan, X.; Scott Jr, L.; Heck, A.J. Rearrangement of the protein phosphatase 1 interactome during heart failure progression. Circulation 2018, 138, 1569–1581. [Google Scholar] [CrossRef] [PubMed]
- Jones, T.; Barker, H.; e Silva, E.d.C.; Mayer-Jaekel, R.; Hemmings, B.; Spurr, N.; Sheer, D.; Cohen, P. Localization of the genes encoding the catalytic subunits of protein phosphatase 2A to human chromosome bands 5q23→ q31 and 8p12→ p11. 2, respectively. Cytogenet. Genome Res. 1993, 63, 35–41. [Google Scholar] [CrossRef] [PubMed]
- O’Donoghue, J. Hydroquinone and its analogues in dermatology—A risk-benefit viewpoint. J. Cosmet. Dermatol. 2006, 5, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Sahab, Z.J.; Hall, M.D.; Zhang, L.; Cheema, A.K.; Byers, S.W. Tumor suppressor rarres1 regulates dlg2, pp2a, vcp, eb1, and ankrd26. J. Cancer 2010, 1, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Sontag, E. Protein phosphatase 2A: The Trojan Horse of cellular signaling. Cell. Signal. 2001, 13, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Seshacharyulu, P.; Pandey, P.; Datta, K.; Batra, S.K. Phosphatase: PP2A structural importance, regulation and its aberrant expression in cancer. Cancer Lett. 2013, 335, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Schuhmacher, D.; Sontag, J.M.; Sontag, E. Protein Phosphatase 2A: More Than a Passenger in the Regulation of Epithelial Cell-Cell Junctions. Front. Cell Dev. Biol. 2019, 7, 30. [Google Scholar] [CrossRef] [PubMed]
- Sents, W.; Ivanova, E.; Lambrecht, C.; Haesen, D.; Janssens, V. The biogenesis of active protein phosphatase 2A holoenzymes: A tightly regulated process creating phosphatase specificity. FEBS J. 2013, 280, 644–661. [Google Scholar] [CrossRef] [PubMed]
- Garcia, A.; Cayla, X.; Sontag, E. Protein phosphatase 2A: A definite player in viral and parasitic regulation. Microbes Infect. 2000, 2, 401–407. [Google Scholar] [CrossRef]
- Sontag, J.-M.; Sontag, E. Protein phosphatase 2A dysfunction in Alzheimer’s disease. Front. Mol. Neurosci. 2014, 7, 16. [Google Scholar] [CrossRef]
- Baskaran, R.; Velmurugan, B.K. Protein phosphatase 2A as therapeutic targets in various disease models. Life Sci. 2018, 210, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, Y.; Mercado, N.; Barnes, P.J.; Ito, K. Defects of protein phosphatase 2A causes corticosteroid insensitivity in severe asthma. PLoS ONE 2011, 6, e27627. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.P.; Bafna, S.; Chaudhary, K.; Venkatraman, G.; Smith, L.; Eudy, J.D.; Johansson, S.L.; Lin, M.-F.; Batra, S.K. Genome-wide expression profiling reveals transcriptomic variation and perturbed gene networks in androgen-dependent and androgen-independent prostate cancer cells. Cancer Lett. 2008, 259, 28–38. [Google Scholar] [CrossRef]
- Cheng, Y.; Liu, W.; Kim, S.-T.; Sun, J.; Lu, L.; Sun, J.; Zheng, S.L.; Isaacs, W.B.; Xu, J. Evaluation of PPP2R2A as a prostate cancer susceptibility gene: A comprehensive germline and somatic study. Cancer Genet. 2011, 204, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Calin, G.A.; Di Iasio, M.G.; Caprini, E.; Vorechovsky, I.; Natali, P.G.; Sozzi, G.; Croce, C.M.; Barbanti-Brodano, G.; Russo, G.; Negrini, M. Low frequency of alterations of the α (PPP2R1A) and β (PPP2R1B) isoforms of the subunit A of the serine-threonine phosphatase 2A in human neoplasms. Oncogene 2000, 19, 1191–1195. [Google Scholar] [CrossRef]
- Janghorban, M.; Farrell, A.S.; Allen-Petersen, B.L.; Pelz, C.; Daniel, C.J.; Oddo, J.; Langer, E.M.; Christensen, D.J.; Sears, R.C. Targeting c-MYC by antagonizing PP2A inhibitors in breast cancer. Proc. Natl. Acad. Sci. USA 2014, 111, 9157–9162. [Google Scholar] [CrossRef]
- Mumby, M. PP2A: Unveiling a reluctant tumor suppressor. Cell 2007, 130, 21–24. [Google Scholar] [CrossRef]
- Bryant, J.-P.; Levy, A.; Heiss, J.; Banasavadi-Siddegowda, Y.K. Review of PP2A tumor biology and antitumor effects of PP2A inhibitor LB100 in the nervous system. Cancers 2021, 13, 3087. [Google Scholar] [CrossRef]
- Braithwaite, S.P.; Voronkov, M.; Stock, J.B.; Mouradian, M.M. Targeting phosphatases as the next generation of disease modifying therapeutics for Parkinson’s disease. Neurochem. Int. 2012, 61, 899–906. [Google Scholar] [CrossRef]
- Voronkov, M.; Braithwaite, S.P.; Stock, J.B. Phosphoprotein phosphatase 2A: A novel druggable target for Alzheimer’s disease. Future Med. Chem. 2011, 3, 821–833. [Google Scholar] [CrossRef]
- Alothaid, H.; Aldughaim, M.S.K.; Alamri, S.S.; Alrahimi, J.S.M.; Al-Jadani, S.H. Role of calcineurin biosignaling in cell secretion and the possible regulatory mechanisms. Saudi J. Biol. Sci. 2021, 28, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Swulius, M.T.; Waxham, M. Ca2+/calmodulin-dependent protein kinases. Cell. Mol. Life Sci. 2008, 65, 2637–2657. [Google Scholar] [CrossRef]
- Carruthers, N.J.; Stemmer, P.M. Methionine oxidation in the calmodulin-binding domain of calcineurin disrupts calmodulin binding and calcineurin activation. Biochemistry 2008, 47, 3085–3095. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Grundke-Iqbal, I.; Iqbal, K.; Oda, Y.; Tomizawa, K.; Gong, C.-X. Truncation and activation of calcineurin A by calpain I in Alzheimer disease brain. J. Biol. Chem. 2005, 280, 37755–37762. [Google Scholar] [CrossRef]
- Baudry, M.; Chou, M.M.; Bi, X. Targeting calpain in synaptic plasticity. Expert Opin. Ther. Targets 2013, 17, 579–592. [Google Scholar] [CrossRef]
- Liu, F.; Liang, Z.; Gong, C. Hyperphosphorylation of tau and protein phosphatases in Alzheimer disease. Panminerva Medica 2006, 48, 97–108. [Google Scholar] [PubMed]
- Kashani, E.; Vassella, E. Pleiotropy of PP2A Phosphatases in Cancer with a Focus on Glioblastoma IDH Wildtype. Cancers 2022, 14, 5227. [Google Scholar] [CrossRef]
- Nygren, P.J.; Scott, J.D. Regulation of the phosphatase PP2B by protein–protein interactions. Biochem. Soc. Trans. 2016, 44, 1313–1319. [Google Scholar] [CrossRef]
- Qian, W.; Yin, X.; Hu, W.; Shi, J.; Gu, J.; Grundke-Iqbal, I.; Iqbal, K.; Gong, C.-X.; Liu, F. Activation of protein phosphatase 2B and hyperphosphorylation of Tau in Alzheimer’s disease. J. Alzheimer’s Dis. 2011, 23, 617–627. [Google Scholar] [CrossRef]
- Tian, Q.; Wang, J. Role of serine/threonine protein phosphatase in Alzheimer’s disease. Neurosignals 2002, 11, 262–269. [Google Scholar] [CrossRef]
- Lakshmikuttyamma, A.; Selvakumar, P.; Kakkar, R.; Kanthan, R.; Wang, R.; Sharma, R.K. Activation of calcineurin expression in ischemia-reperfused rat heart and in human ischemic myocardium. J. Cell. Biochem. 2003, 90, 987–997. [Google Scholar] [CrossRef] [PubMed]
- Olson, E.N.; Williams, R.S. Remodeling muscles with calcineurin. Bioessays 2000, 22, 510–519. [Google Scholar] [CrossRef]
- Liu, J.; Farmer Jr, J.D.; Lane, W.S.; Friedman, J.; Weissman, I.; Schreiber, S.L. Calcineurin is a common target of cyclophilin-cyclosporin A and FKBP-FK506 complexes. Cell 1991, 66, 807–815. [Google Scholar] [CrossRef]
- Taglialatela, G.; Rastellini, C.; Cicalese, L. Reduced incidence of dementia in solid organ transplant patients treated with calcineurin inhibitors. J. Alzheimer’s Dis. 2015, 47, 329–333. [Google Scholar] [CrossRef]
- Norris, C.M. Calcineurin: Directing the damage in Alzheimer disease: An Editorial for ‘Neuronal calcineurin transcriptional targets parallel changes observed in Alzheimer disease brain’on page 24. J. Neurochem. 2018, 147, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Sumiyoshi, E.; Sugimoto, A.; Yamamoto, M. Protein phosphatase 4 is required for centrosome maturation in mitosis and sperm meiosis in C. elegans. J. Cell Sci. 2002, 115, 1403–1410. [Google Scholar] [CrossRef]
- Lee, D.-H.; Chowdhury, D. What goes on must come off: Phosphatases gate-crash the DNA damage response. Trends Biochem. Sci. 2011, 36, 569–577. [Google Scholar] [CrossRef] [PubMed]
- Yeh, P.Y.; Yeh, K.-H.; Chuang, S.-E.; Song, Y.C.; Cheng, A.-L. Suppression of MEK/ERK signaling pathway enhances cisplatin-induced NF-κB activation by protein phosphatase 4-mediated NF-κB p65 Thr dephosphorylation. J. Biol. Chem. 2004, 279, 26143–26148. [Google Scholar] [CrossRef]
- Cohen, P.T.; Philp, A.; Vázquez-Martin, C. Protein phosphatase 4–from obscurity to vital functions. FEBS Lett. 2005, 579, 3278–3286. [Google Scholar] [CrossRef] [PubMed]
- Melki, J. Spinal muscular atrophy. Curr. Opin. Neurol. 1997, 10, 381–385. [Google Scholar] [CrossRef]
- Kloeker, S.; Wadzinski, B.E. Purification and identification of a novel subunit of protein serine/threonine phosphatase 4. J. Biol. Chem. 1999, 274, 5339–5347. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.I.; Tisayakorn, S.; Jorgensen, C.; D’Ambrosio, L.M.; Goudreault, M.; Gingras, A.-C. PP4R4/KIAA1622 Forms a Novel Stable Cytosolic Complex with Phosphoprotein Phosphatase 4. J. Biol. Chem. 2008, 283, 29273–29284. [Google Scholar] [CrossRef] [PubMed]
- Virshup, D.M.; Shenolikar, S. From promiscuity to precision: Protein phosphatases get a makeover. Mol. Cell 2009, 33, 537–545. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, D.; Xu, X.; Zhong, X.; Ahmed, F.; Zhong, J.; Liao, J.; Dykxhoorn, D.M.; Weinstock, D.M.; Pfeifer, G.P.; Lieberman, J. A PP4-phosphatase complex dephosphorylates γ-H2AX generated during DNA replication. Mol. Cell 2008, 31, 33–46. [Google Scholar] [CrossRef] [PubMed]
- Tisayakorn, K.W.S. Structure-Function Analysis of the Trimeric PP4C-PP4R2-PP4R3 Phosphatase Complex. Master’s Thesis, University of Toronto, Toronto, ON, USA, 2009. [Google Scholar]
- Seumen, C.H.; Grimm, T.M.; Hauck, C.R. Protein phosphatases in TLR signaling. Cell Commun. Signal. 2021, 19, 45. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Rodriguez, M.; García-Rodríguez, C.; Villalobos, C.; Núñez, L. Role of toll like receptor 4 in Alzheimer’s disease. Front. Immunol. 2020, 11, 1588. [Google Scholar] [CrossRef] [PubMed]
- Hinds Jr, T.D.; Sánchez, E.R. Protein phosphatase 5. Int. J. Biochem. Cell Biol. 2008, 40, 2358–2362. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Iqbal, K.; Grundke-Iqbal, I.; Rossie, S.; Gong, C.-X. Dephosphorylation of tau by protein phosphatase 5: Impairment in Alzheimer’s disease. J. Biol. Chem. 2005, 280, 1790–1796. [Google Scholar] [CrossRef] [PubMed]
- Gong, C.X.; Liu, F.; Wu, G.; Rossie, S.; Wegiel, J.; Li, L.; Grundke-Iqbal, I.; Iqbal, K. Dephosphorylation of microtubule-associated protein tau by protein phosphatase 5. J. Neurochem. 2004, 88, 298–310. [Google Scholar] [CrossRef] [PubMed]
- Reddy, P.H.; Beal, M.F. Amyloid beta, mitochondrial dysfunction and synaptic damage: Implications for cognitive decline in aging and Alzheimer’s disease. Trends Mol. Med. 2008, 14, 45–53. [Google Scholar] [CrossRef]
- Braithwaite, S.P.; Stock, J.B.; Lombroso, P.J.; Nairn, A.C. Protein phosphatases and Alzheimer’s disease. Prog. Mol. Biol. Transl. Sci. 2012, 106, 343–379. [Google Scholar]
- Zhong, J.; Liao, J.; Liu, X.; Wang, P.; Liu, J.; Hou, W.; Zhu, B.; Yao, L.; Wang, J.; Li, J. Protein phosphatase PP6 is required for homology-directed repair of DNA double-strand breaks. Cell Cycle 2011, 10, 1411–1419. [Google Scholar] [CrossRef]
- Kajino, T.; Ren, H.; Iemura, S.-i.; Natsume, T.; Stefansson, B.; Brautigan, D.L.; Matsumoto, K.; Ninomiya-Tsuji, J. Protein phosphatase 6 down-regulates TAK1 kinase activation in the IL-1 signaling pathway. J. Biol. Chem. 2006, 281, 39891–39896. [Google Scholar] [CrossRef]
- Tan, P.; He, L.; Cui, J.; Qian, C.; Cao, X.; Lin, M.; Zhu, Q.; Li, Y.; Xing, C.; Yu, X. Assembly of the WHIP-TRIM14-PPP6C mitochondrial complex promotes RIG-I-mediated antiviral signaling. Mol. Cell 2017, 68, 293–307.e5. [Google Scholar] [CrossRef]
- Li, M.; Shu, H.-B. Dephosphorylation of cGAS by PPP6C impairs its substrate binding activity and innate antiviral response. Protein Cell 2020, 11, 584–599. [Google Scholar] [CrossRef]
- Stefansson, B.; Brautigan, D.L. Protein phosphatase PP6 N terminal domain restricts G1 to S phase progression in human cancer cells. Cell Cycle 2007, 6, 1386–1392. [Google Scholar] [CrossRef]
- Kotak, S.; Afshar, K.; Busso, C.; Gönczy, P. Aurora A kinase regulates proper spindle positioning in C. elegans and in human cells. J. Cell Sci. 2016, 129, 3015–3025. [Google Scholar] [CrossRef]
- Mrak, R.E.; Griffin, W.S.T. Interleukin-1 and the immunogenetics of Alzheimer disease. J. Neuropathol. Exp. Neurol. 2000, 59, 471–476. [Google Scholar] [CrossRef]
- Campos, A.; Clemente-Blanco, A. Cell cycle and DNA repair regulation in the damage response: Protein phosphatases take over the reins. Int. J. Mol. Sci. 2020, 21, 446. [Google Scholar] [CrossRef]
- Forlenza, O.V.; de Paula, V.J.; Machado-Vieira, R.; Diniz, B.S.; Gattaz, W.F. Does lithium prevent Alzheimer’s disease? Drugs Aging 2012, 29, 335–342. [Google Scholar] [CrossRef]
- Chiu, C.-T.; Chuang, D.-M. Molecular actions and therapeutic potential of lithium in preclinical and clinical studies of CNS disorders. Pharmacol. Ther. 2010, 128, 281–304. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, A.; Briggs, K.; Poppe, M.; Higgins, A.; Velayudhan, L.; Lovestone, S. A feasibility and tolerability study of lithium in Alzheimer’s disease. Int. J. Geriatr. Psychiatry J. Psychiatry Late Life Allied Sci. 2008, 23, 704–711. [Google Scholar] [CrossRef]
- Kamat, P.K.; Rai, S.; Nath, C. Okadaic acid induced neurotoxicity: An emerging tool to study Alzheimer’s disease pathology. Neurotoxicology 2013, 37, 163–172. [Google Scholar] [CrossRef]
- Ferrero-Gutiérrez, A.; Pérez-Gómez, A.; Novelli, A.; Fernández-Sánchez, M.T. Inhibition of protein phosphatases impairs the ability of astrocytes to detoxify hydrogen peroxide. Free Radic. Biol. Med. 2008, 44, 1806–1816. [Google Scholar] [CrossRef]
- Puerto Galvis, C.E.; Vargas Mendez, L.Y.; Kouznetsov, V.V. Cantharidin-based small molecules as potential therapeutic agents. Chem. Biol. Drug Des. 2013, 82, 477–499. [Google Scholar] [CrossRef]
- Sieber, M.; Baumgrass, R. Novel inhibitors of the calcineurin/NFATc hub-alternatives to CsA and FK506? Cell Commun. Signal. 2009, 7, 25. [Google Scholar] [CrossRef]
- Sayas, C.L.; Ávila, J. GSK-3 and Tau: A key duet in Alzheimer’s disease. Cells 2021, 10, 721. [Google Scholar] [CrossRef]
- Venerando, A.; Ruzzene, M.; Pinna, L.A. Casein kinase: The triple meaning of a misnomer. Biochem. J. 2014, 460, 141–156. [Google Scholar] [CrossRef]
- Borgo, C.; D’Amore, C.; Sarno, S.; Salvi, M.; Ruzzene, M. Protein kinase CK2: A potential therapeutic target for diverse human diseases. Signal Transduct. Target. Ther. 2021, 6, 183. [Google Scholar] [CrossRef]
- Dehay, B.; Bourdenx, M.; Gorry, P.; Przedborski, S.; Vila, M.; Hunot, S.; Singleton, A.; Olanow, C.W.; Merchant, K.M.; Bezard, E. Targeting α-synuclein for treatment of Parkinson’s disease: Mechanistic and therapeutic considerations. Lancet Neurol. 2015, 14, 855–866. [Google Scholar] [CrossRef]
- Pan, J.; Zhou, L.; Zhang, C.; Xu, Q.; Sun, Y. Targeting protein phosphatases for the treatment of inflammation-related diseases: From signaling to therapy. Signal Transduct. Target. Ther. 2022, 7, 177. [Google Scholar] [CrossRef]
- Hayne, M.; DiAntonio, A. Protein phosphatase 2A restrains DLK signaling to promote proper Drosophila synaptic development and mammalian cortical neuron survival. Neurobiol. Dis. 2022, 163, 105586. [Google Scholar] [CrossRef]
- Gonzalez-Teuber, V.; Albert-Gasco, H.; Auyeung, V.C.; Papa, F.R.; Mallucci, G.R.; Hetz, C. Small molecules to improve ER proteostasis in disease. Trends Pharmacol. Sci. 2019, 40, 684–695. [Google Scholar] [CrossRef]
- Lemoine, L.; Leuzy, A.; Chiotis, K.; Rodriguez-Vieitez, E.; Nordberg, A. Tau positron emission tomography imaging in tauopathies: The added hurdle of off-target binding. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2018, 10, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Seripa, D.; Solfrizzi, V.; Imbimbo, B.P.; Daniele, A.; Santamato, A.; Lozupone, M.; Zuliani, G.; Greco, A.; Logroscino, G.; Panza, F. Tau-directed approaches for the treatment of Alzheimer’s disease: Focus on leuco-methylthioninium. Expert Rev. Neurother. 2016, 16, 259–277. [Google Scholar] [CrossRef]
- Cristóbal, I.; Madoz-Gúrpide, J.; Manso, R.; González-Alonso, P.; Rojo, F.; García-Foncillas, J. Potential anti-tumor effects of FTY720 associated with PP2A activation: A brief review. Curr. Med. Res. Opin. 2016, 32, 1137–1141. [Google Scholar] [CrossRef]
- Angelopoulou, E.; Piperi, C. Beneficial effects of fingolimod in Alzheimer’s disease: Molecular mechanisms and therapeutic potential. NeuroMol. Med. 2019, 21, 227–238. [Google Scholar] [CrossRef]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hassan, M.; Yasir, M.; Shahzadi, S.; Chun, W.; Kloczkowski, A. Molecular Role of Protein Phosphatases in Alzheimer’s and Other Neurodegenerative Diseases. Biomedicines 2024, 12, 1097. https://doi.org/10.3390/biomedicines12051097
Hassan M, Yasir M, Shahzadi S, Chun W, Kloczkowski A. Molecular Role of Protein Phosphatases in Alzheimer’s and Other Neurodegenerative Diseases. Biomedicines. 2024; 12(5):1097. https://doi.org/10.3390/biomedicines12051097
Chicago/Turabian StyleHassan, Mubashir, Muhammad Yasir, Saba Shahzadi, Wanjoo Chun, and Andrzej Kloczkowski. 2024. "Molecular Role of Protein Phosphatases in Alzheimer’s and Other Neurodegenerative Diseases" Biomedicines 12, no. 5: 1097. https://doi.org/10.3390/biomedicines12051097





