A Luciferase Immunosorbent Assay Based on Attachment Glycoprotein for the Rapid and Easy Detection of Nipah Virus IgG Antibodies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Samples and Reagents
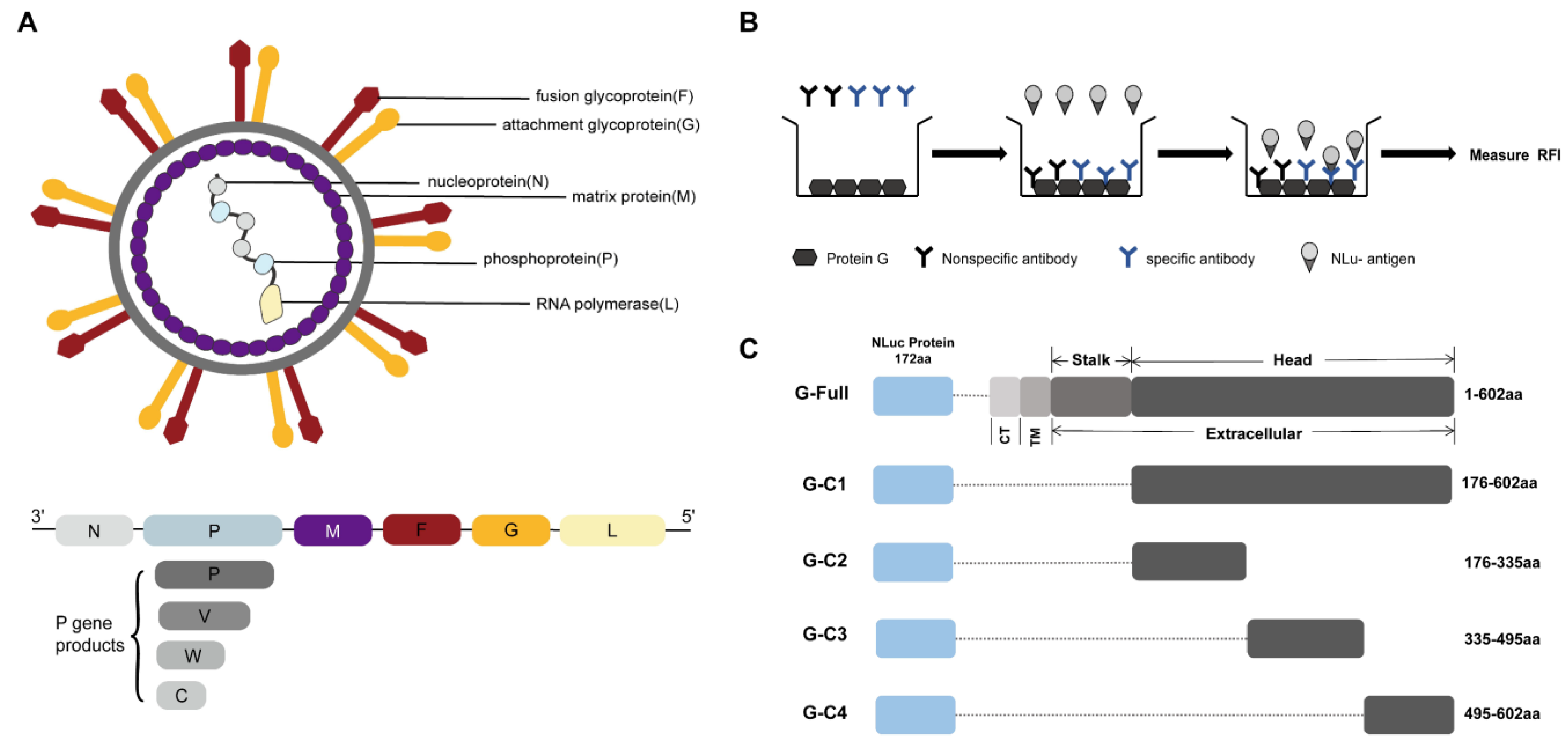
2.2. Design and Construction of Recombinant Plasmids Based on G Proteins
2.3. Expression of the Luciferase Fusion Antigen
2.4. Western Blot
2.5. Serum Preparation
2.6. Establishment of the NiV-G-LISA
2.7. ELISA
2.8. Statistical Analysis
3. Results
3.1. Expression of Different Fragments of the NiV G Protein Luciferase Fusion Antigen
3.2. Establishment of the LISA for the Detection of NiV IgG Antibody
3.3. Optimal Structural Domains for NiV IgG Antibody Detection
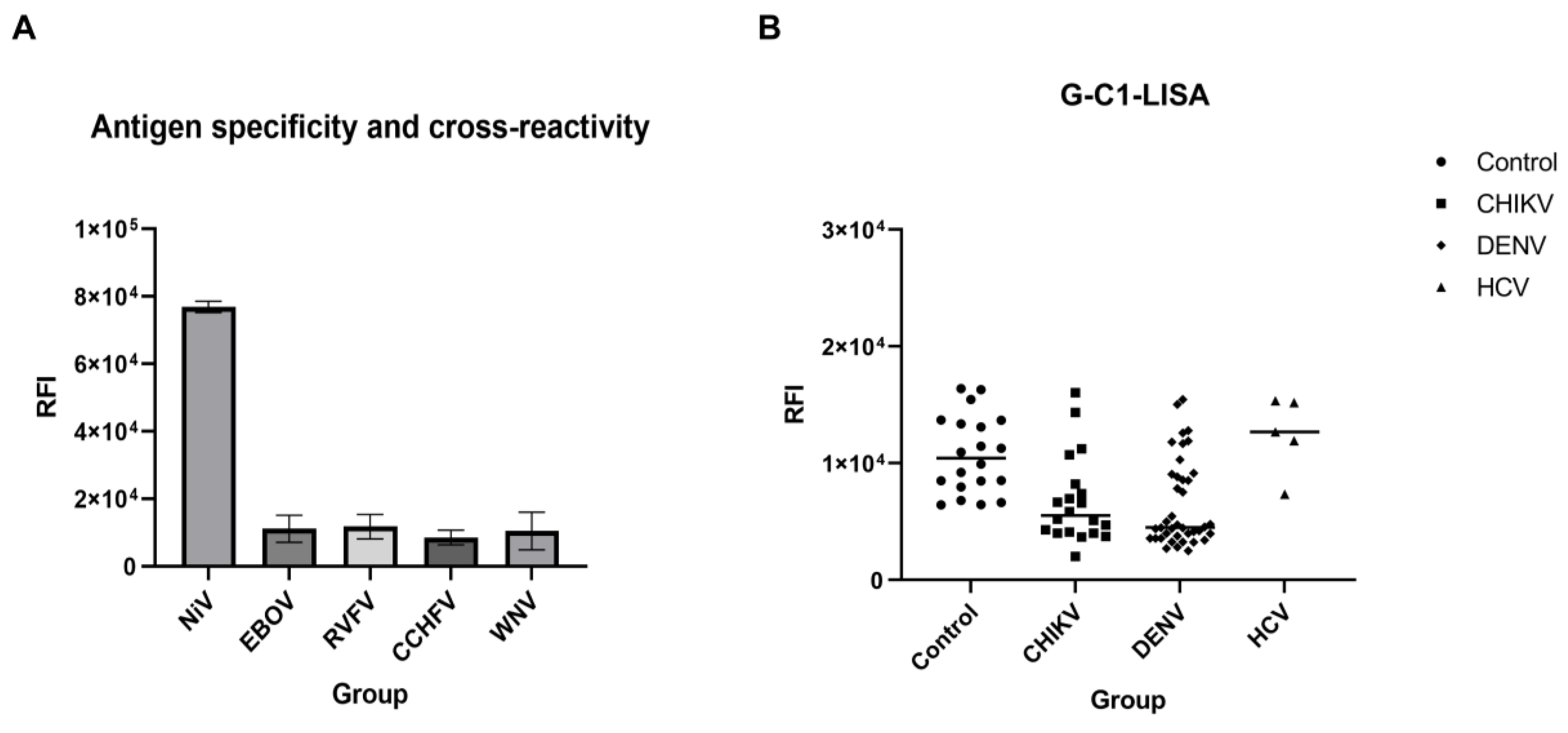
3.4. Sensitivity and Cross-Reactivity Analysis of the G-C1-LISA
4. Discussion
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chua, K.B.; Bellini, W.J.; Rota, P.A.; Harcourt, B.H.; Tamin, A.; Lam, S.K.; Ksiazek, T.G.; Rollin, P.E.; Zaki, S.R.; Shieh, W.J.; et al. Nipah virus: A recently emergent deadly paramyxovirus. Science 2000, 288, 1432–1435. [Google Scholar] [CrossRef]
- Chua, K.B.; Goh, K.J.; Wong, K.T.; Kamarulzaman, A.; Tan, P.S.K.; Ksiazek, T.G.; Zaki, S.R.; Paul, G.; Lam, S.K.; Tan, C.T. Fatal encephalitis due to Nipah virus among pig-farmers in Malaysia. Lancet 1999, 354, 1257–1259. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.Z.; Islam, M.M.; Hossain, M.E.; Rahman, M.M.; Islam, A.; Siddika, A.; Hossain, M.S.S.; Sultana, S.; Rahman, M.; Klena, J.D.; et al. Genetic diversity of Nipah virus in Bangladesh. Int. J. Infect. Dis. 2021, 102, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Cui, Z.; Li, J.; Meng, L.; Zhang, Z. Nipah virus: A re-emerging public health concern. The Lancet. Microbe 2023, 5, e212. [Google Scholar] [CrossRef] [PubMed]
- Cox, R.M.; Plemper, R.K. Structure and organization of paramyxovirus particles. Curr. Opin. Virol. 2017, 24, 105–114. [Google Scholar] [CrossRef]
- Whitmer, S.L.; Lo, M.K.; Sazzad, H.M.; Zufan, S.; Gurley, E.S.; Sultana, S.; Amman, B.; Ladner, J.T.; Rahman, M.Z.; Doan, S.; et al. Inference of Nipah virus evolution, 1999–2015. Virus Evol. 2021, 7, veaa062. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Yan, S.; Wang, N.; He, W.; Guan, H.; He, C.; Wang, Z.; Lu, M.; He, W.; Ye, R.; et al. Emergence and adaptive evolution of Nipah virus. Transbound. Emerg. Dis. 2020, 67, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Weatherman, S.; Feldmann, H.; de Wit, E. Transmission of henipaviruses. Curr. Opin. Virol. 2018, 28, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Goh, K.J.; Tan, C.T.; Chew, N.K.; Tan, P.S.K.; Kamarulzaman, A.; Sarji, S.A.; Wong, K.T.; Abdullah, B.J.J.; Chua, K.B.; Lam, S.K. Clinical Features of Nipah Virus Encephalitis among Pig Farmers in Malaysia. N. Engl. J. Med. 2000, 342, 1229–1235. [Google Scholar] [CrossRef]
- Mohandas, S.; Shete, A.; Sarkale, P.; Kumar, A.; Mote, C.; Yadav, P. Genomic characterization, transcriptome analysis, and pathogenicity of the Nipah virus (Indian isolate). Virulence 2023, 14, 2224642. [Google Scholar] [CrossRef]
- Sharma, V.; Kaushik, S.; Kumar, R.; Yadav, J.P.; Kaushik, S. Emerging trends of Nipah virus: A review. Rev. Med. Virol. 2019, 29, e2010. [Google Scholar] [CrossRef]
- Hyatt, A.D.; Zaki, S.R.; Goldsmith, C.S.; Wise, T.G.; Hengstberger, S.G. Ultrastructure of Hendra virus and Nipah virus within cultured cells and host animals. Microbes Infect. 2001, 3, 297–306. [Google Scholar] [CrossRef]
- Feldman, K.S.; Foord, A.; Heine, H.G.; Smith, I.L.; Boyd, V.; Marsh, G.A.; Wood, J.L.N.; Cunningham, A.A.; Wang, L.F. Design and evaluation of consensus PCR assays for henipaviruses. J. Virol. Methods 2009, 161, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Dhama, K.; Chakraborty, S.; Tiwari, R.; Natesan, S.; Khandia, R.; Munjal, A.; Vora, K.S.; Latheef, S.K.; Karthik, K.; et al. Nipah virus: Epidemiology, pathology, immunobiology and advances in diagnosis, vaccine designing and control strategies—A comprehensive review. Vet. Q. 2019, 39, 26–55. [Google Scholar] [CrossRef]
- Lu, X.; Liu, Q.; Benavides-Montano, J.A.; Nicola, A.V.; Aston, D.E.; Rasco, B.A.; Aguilar, H.C. Detection of receptor-induced glycoprotein conformational changes on enveloped virions by using confocal micro-Raman spectroscopy. J. Virol. 2013, 87, 3130–3142. [Google Scholar] [CrossRef]
- Ortega, V.; Zamora, J.L.R.; Monreal, I.A.; Hoffman, D.T.; Ezzatpour, S.; Johnston, G.P.; Contreras, E.M.; Vilchez-Delgado, F.J.; Aguilar, H.C. Novel Roles of the Nipah Virus Attachment Glycoprotein and Its Mobility in Early and Late Membrane Fusion Steps. mBio 2022, 13, e0322221. [Google Scholar] [CrossRef]
- Negrete, O.A.; Levroney, E.L.; Aguilar, H.C.; Bertolotti-Ciarlet, A.; Nazarian, R.; Tajyar, S.; Lee, B. EphrinB2 is the entry receptor for Nipah virus, an emergent deadly paramyxovirus. Nature 2005, 436, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z. Architecture and antigenicity of the nipah virus attachment glycoprotein. Biophys. J. 2022, 121, 29a. [Google Scholar] [CrossRef]
- de Wit, E.; Feldmann, F.; Cronin, J.; Goldin, K.; Mercado-Hernandez, R.; Williamson, B.N.; Meade-White, K.; Okumura, A.; Callison, J.; Weatherman, S.; et al. Distinct VSV-based Nipah virus vaccines expressing either glycoprotein G or fusion protein F provide homologous and heterologous protection in a nonhuman primate model. eBioMedicine 2023, 87, 104405. [Google Scholar] [CrossRef]
- Dong, J.; Cross, R.W.; Doyle, M.P.; Kose, N.; Mousa, J.J.; Annand, E.J.; Borisevich, V.; Agans, K.N.; Sutton, R.; Nargi, R.; et al. Potent Henipavirus Neutralization by Antibodies Recognizing Diverse Sites on Hendra and Nipah Virus Receptor Binding Protein. Cell 2020, 183, 1536–1550.e17. [Google Scholar] [CrossRef]
- Fischer, K.; Diederich, S.; Smith, G.; Reiche, S.; Pinho dos Reis, V.; Stroh, E.; Groschup, M.H.; Weingartl, H.M.; Balkema-Buschmann, A. Indirect ELISA based on Hendra and Nipah virus proteins for the detection of henipavirus specific antibodies in pigs. PLoS ONE 2018, 13, e0194385. [Google Scholar] [CrossRef] [PubMed]
- Kashiwazaki, Y.; Na, Y.N.; Tanimura, N.; Imada, T. A solid-phase blocking ELISA for detection of antibodies to Nipah virus. J. Virol. Methods 2004, 121, 259–261. [Google Scholar] [CrossRef] [PubMed]
- Ludolfs, D.; Reinholz, M.; Schmitz, H. Highly specific detection of antibodies to tick-borne encephalitis (TBE) virus in humans using a domain III antigen and a sensitive immune complex (IC) ELISA. J. Clin. Virol. 2009, 45, 125–128. [Google Scholar] [CrossRef]
- Xu, K.; Rajashankar, K.R.; Chan, Y.P.; Himanen, J.P.; Broder, C.C.; Nikolov, D.B. Host cell recognition by the henipaviruses: Crystal structures of the Nipah G attachment glycoprotein and its complex with ephrin-B3. Proc. Natl. Acad. Sci. USA 2008, 105, 9953–9958. [Google Scholar] [CrossRef] [PubMed]
- Nikolay, B.; Salje, H.; Hossain, M.J.; Khan, A.D.; Sazzad, H.M.; Rahman, M.; Daszak, P.; Ströher, U.; Pulliam, J.R.; Kilpatrick, A.M.; et al. Transmission of Nipah Virus—14 Years of Investigations in Bangladesh. N. Engl. J. Med. 2019, 380, 1804–1814. [Google Scholar] [CrossRef]
- Eshaghi, M.; Tan, W.S.; Yusoff, K. Identification of epitopes in the nucleocapsid protein of Nipah virus using a linear phage-displayed random peptide library. J. Med. Virol. 2005, 75, 147–152. [Google Scholar] [CrossRef]
- Tiong, V.; Lam, C.W.; Phoon, W.H.; AbuBakar, S.; Chang, L.Y. Serum from Nipah Virus Patients Recognises Recombinant Viral Proteins Produced in Escherichia coli. Jpn. J. Infect. Dis. 2017, 70, 26–31. [Google Scholar] [CrossRef]
- Lu, M.; Yao, Y.; Zhang, X.; Liu, H.; Gao, G.; Peng, Y.; Chen, M.; Zhao, J.; Zhang, X.; Yin, C.; et al. Both chimpanzee adenovirus-vectored and DNA vaccines induced long-term immunity against Nipah virus infection. NPJ Vaccines 2023, 8, 170. [Google Scholar] [CrossRef]
- Wang, T.; Zhan, Y.; Wu, D.; Chen, Z.; Wu, W.; Deng, Y.; Wang, W.; Tan, W.; Tang, S. Development and Evaluation of a Universal and Supersensitive NS1-Based Luciferase Immunosorbent Assay to Detect Zika Virus-Specific IgG. Virol. Sin. 2020, 35, 93–102. [Google Scholar] [CrossRef]
- Li, X.; Wan, X.; Liu, J.; Wang, H.; Li, A.; Ke, C.; Tang, S.; Zhao, W.; Cai, S.; Wan, C. Luciferase Immunosorbent Assay Based on Multiple E Antigens for the Detection of Chikungunya Virus-Specific IgG Antibodies. Microbiol. Spectr. 2022, 10, e01496-21. [Google Scholar]
- Letko, M.; Seifert, S.N.; Olival, K.J.; Plowright, R.K.; Munster, V.J. Bat-borne virus diversity, spillover and emergence. Nature Reviews. Microbiology 2020, 18, 461–471. [Google Scholar] [PubMed]
- Olival, K.J.; Latinne, A.; Islam, A.; Epstein, J.H.; Hersch, R.; Engstrand, R.C.; Gurley, E.S.; Amato, G.; Luby, S.P.; Daszak, P. Population genetics of fruit bat reservoir informs the dynamics, distribution and diversity of Nipah virus. Mol. Ecol. 2020, 29, 970–985. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Zhang, M.; Wang, Y.; Koroma, M.M.; Yu, J.; Zhou, F.; Jing, D.; Li, J.; Tang, S.; Chen, Q.; et al. Development and evaluation of a new luciferase immunosorbent assay to detect GII.6 norovirus-specific IgG in different domestic and wild animals. Front. Microbiol. 2023, 14, 1213007. [Google Scholar] [CrossRef]
- Wang, Q.; Mo, R.; Zhang, Y.; Feng, N.; Yan, F.H.; Wang, T.C. Prokaryotic expression of truncated G protein of Nipah virus and establishment of indirect ELISA method. Chin. Vet. Sci. 2023, 53, 1223–1231. (In Chinese) [Google Scholar]



| Amplified Gene | Primer Name | Primer Sequence |
|---|---|---|
| G-C1 G-C1 | F R | TCGCTTCCGAATTCAGAGCTCAAGAAGGGGTGAGCAATCTAGTAGGATTAC AATTGGGCCCAAATCTAGATTAATGGTGATGGTGATGGTGTGTACATTGCTCTGG |
| G-C2 G-C2 | F R | TCGCTTCCGAATTCAGAGCTCAAGAAGGGGTGAGCAATCTAGTAGGATTAC AATTGGGCCCAAATCTAGATTAATGGTGATGGTGATGGTGAAGTTGATGTTGATTG |
| G-C3 G-C3 | F R | TCGCTTCCGAATTCAGAGCTCAACTTGCCCTACGAAGTATCGAGAA ATTGGGCCCAAATCTAGATTAATGGTGATGGTGATGGTGTCTAGGGCATTGTGATT |
| G-C4 G-C4 | F R | ATCGCTTCCGAATTCAGAGCTCAAAGATTCAATACATGTCCAGAGATCTG AATTGGGCCCAAATCTAGATTAATGGTGATGGTGATGGTGTGTACATTGCTCTGG |
| G-Full | G-C1 | G-C2 | G-C3 | G-C4 | |
|---|---|---|---|---|---|
| Anti-NiV IgG positive * | 1/2/3/4/5/6/7/8/9 | 1/2/3/4/5/6/7/8/9 | 4 | / | 1/3/4 |
| Anti-NiV IgG negative | / | / | 1/2/3/5/6/7/8/9 | 1/2/3/4/5/6/7/8/9 | 2/5/6/7/8/9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, X.; Fang, Y.; Huang, X.; Zhao, Y.; Wan, C. A Luciferase Immunosorbent Assay Based on Attachment Glycoprotein for the Rapid and Easy Detection of Nipah Virus IgG Antibodies. Microorganisms 2024, 12, 983. https://doi.org/10.3390/microorganisms12050983
Li X, Fang Y, Huang X, Zhao Y, Wan C. A Luciferase Immunosorbent Assay Based on Attachment Glycoprotein for the Rapid and Easy Detection of Nipah Virus IgG Antibodies. Microorganisms. 2024; 12(5):983. https://doi.org/10.3390/microorganisms12050983
Chicago/Turabian StyleLi, Xinyue, Yuting Fang, Xinyi Huang, Yongkun Zhao, and Chengsong Wan. 2024. "A Luciferase Immunosorbent Assay Based on Attachment Glycoprotein for the Rapid and Easy Detection of Nipah Virus IgG Antibodies" Microorganisms 12, no. 5: 983. https://doi.org/10.3390/microorganisms12050983






