Surfactant Phospholipid Kinetics in Ventilated Children after Therapeutic Surfactant Supplementation
Abstract
:1. Introduction
2. Results
2.1. Participant Demographics
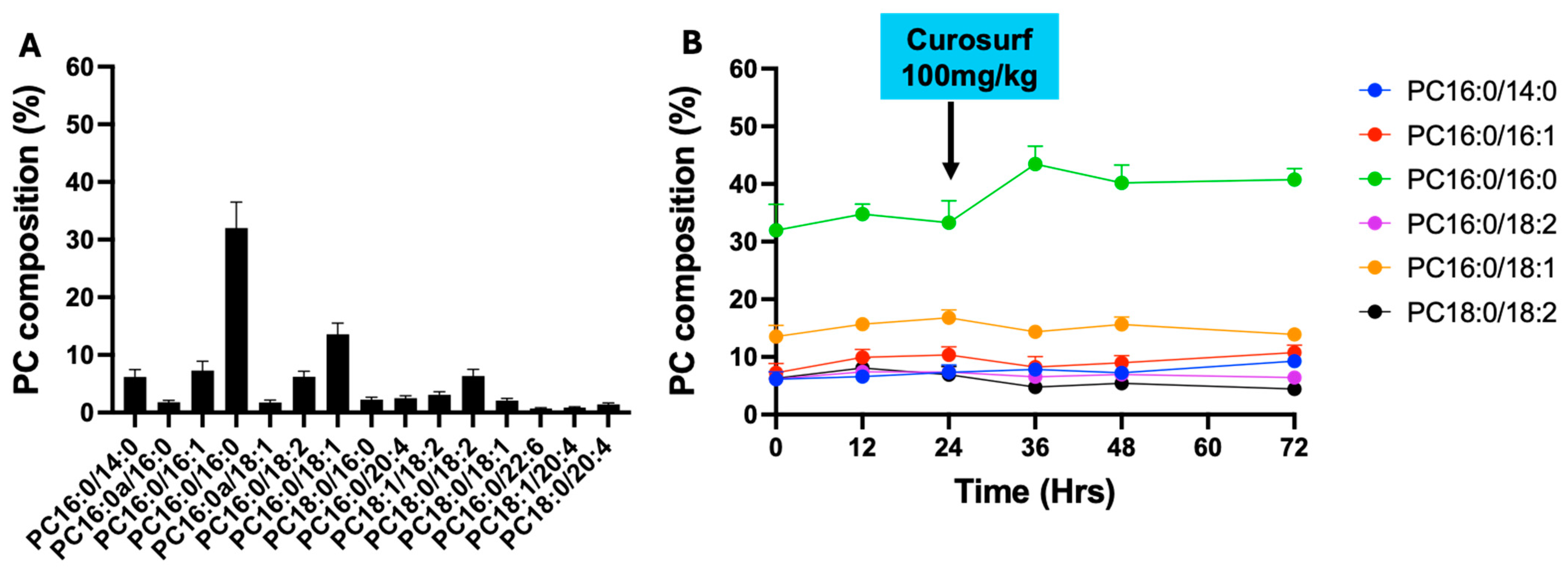
2.2. Phosphatidylcholine (PC) Composition in Bronchoalveoalr Lavage Fluid (BALF)
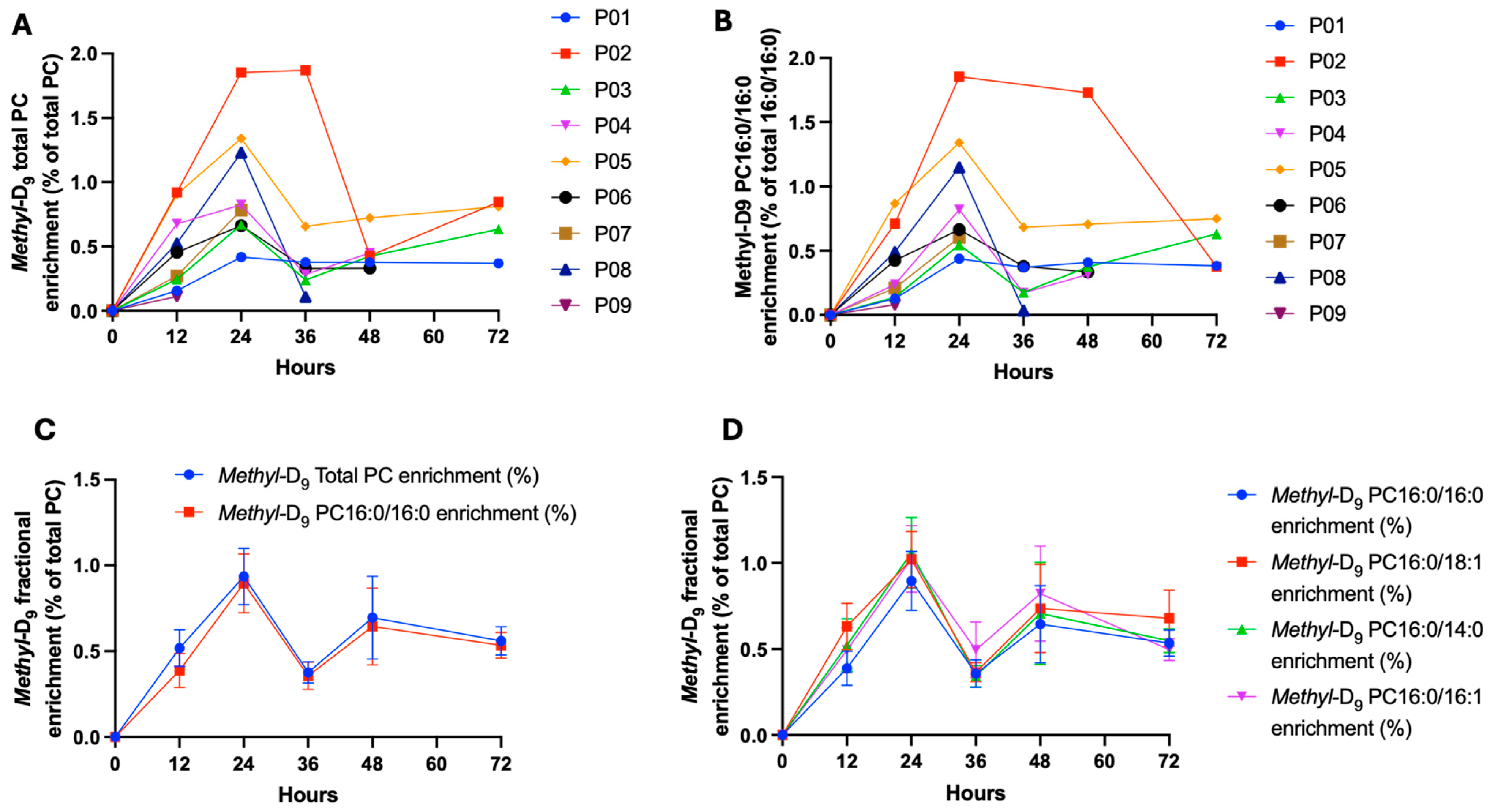
2.3. The Total PC and Fractional PC16:0/16:0 Methyl-D9 Choline Enrichment
2.4. Fractional Composition of Methyl-D9-Labelled PC
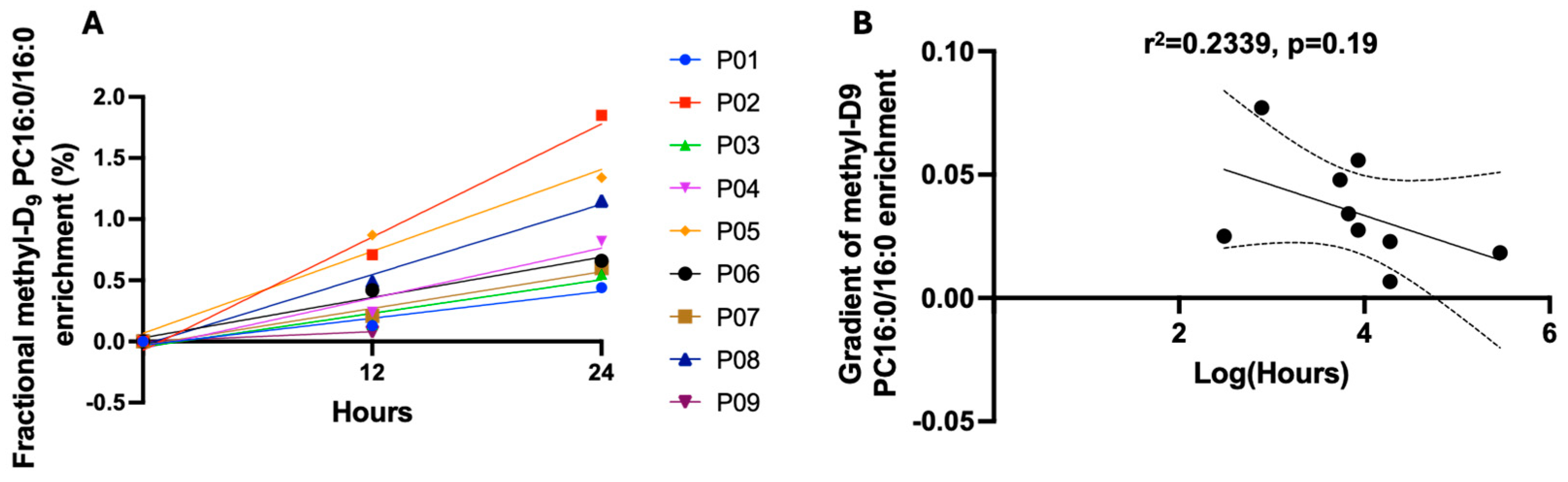
2.5. Enrichment into BALF PC16:0/16:0 and Duration of Mechanical Ventilation Prior to Recruitment
3. Discussion
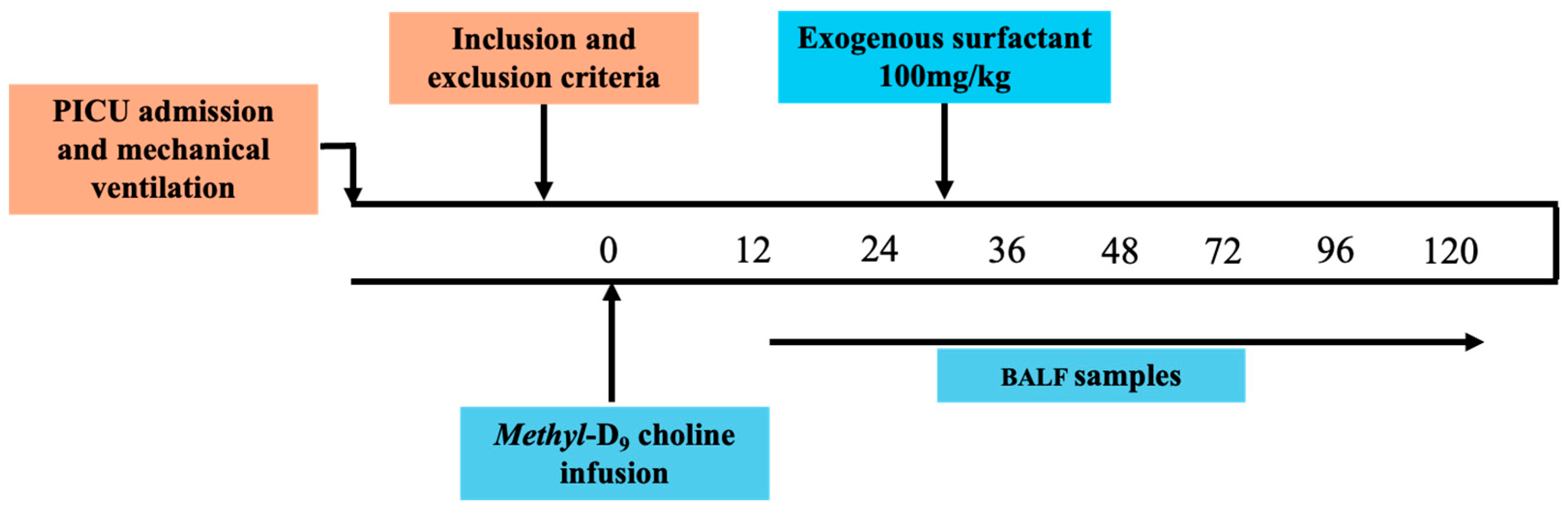
4. Materials and Methods
4.1. Ethics and Participants
4.2. Study Procedures
4.3. Lipid Extraction
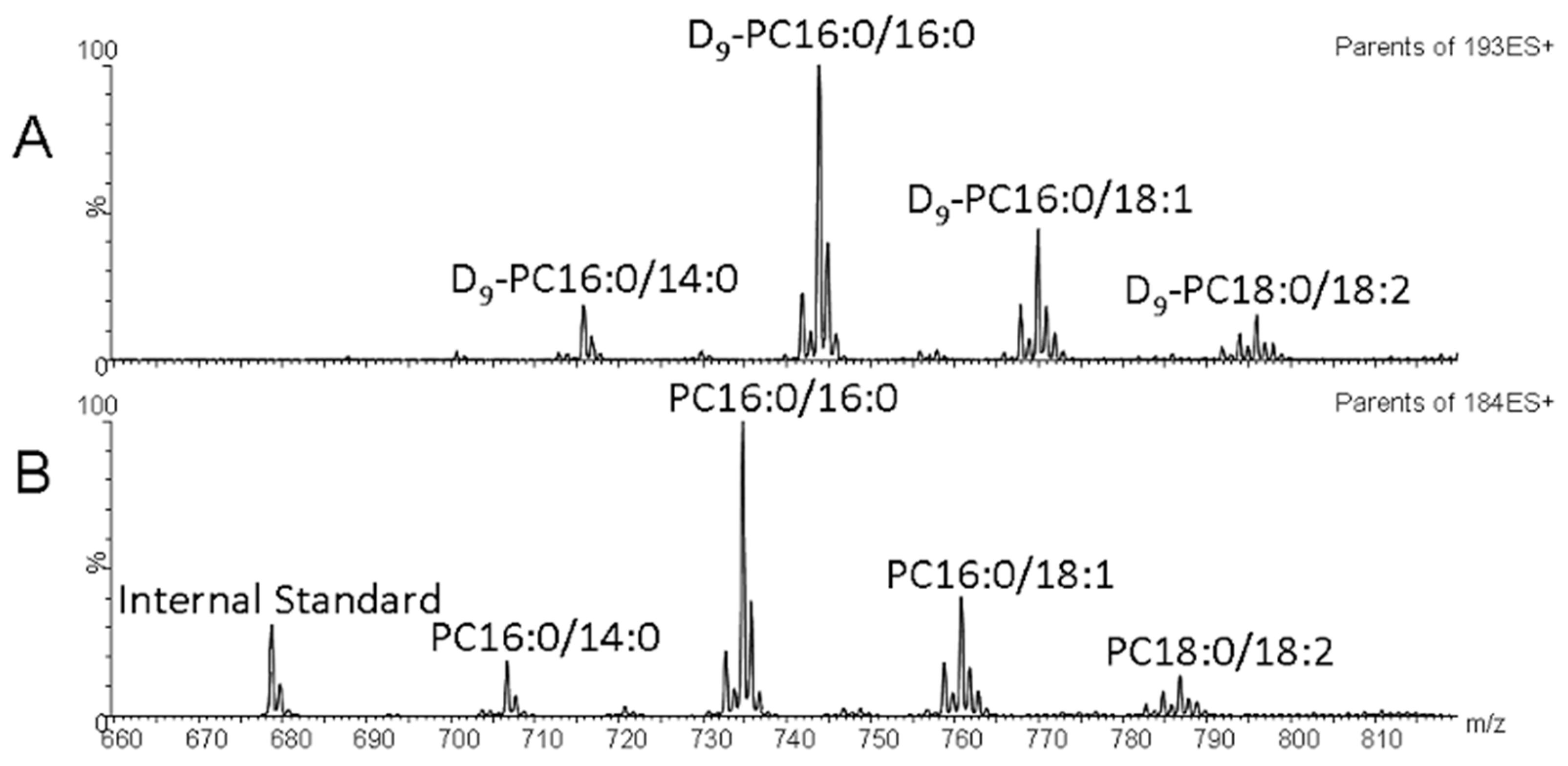
4.4. Lipid Mass Spectrometry
4.5. Statistics
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Clements, J.A. Functions of the alveolar lining. Am. Rev. Respir. Dis. 1977, 115, 67–71. [Google Scholar] [PubMed]
- Haagsman, H.P.; van Golde, L.M. Synthesis and assembly of lung surfactant. Annu. Rev. Physiol. 1991, 53, 441–464. [Google Scholar] [CrossRef] [PubMed]
- Goerke, J.; Gonzales, J. Temperature dependence of dipalmitoyl phosphatidylcholine monolayer stability. J. Appl. Physiol. 1981, 51, 1108–1114. [Google Scholar] [CrossRef] [PubMed]
- Veldhuizen, E.J.; Haagsman, H.P. Role of pulmonary surfactant components in surface film formation and dynamics. Biochim. Biophys. Acta 2000, 1467, 255–270. [Google Scholar] [CrossRef]
- Todd, D.A.; Marsh, M.J.; George, A.; Henderson, N.G.; Barr, H.; Sebastian, S.; Clark, G.T.; Koster, G.; Clark, H.W.; Postle, A.D. Surfactant phospholipids, surfactant proteins, and inflammatory markers during acute lung injury in children. Pediatr. Crit. Care Med. 2010, 11, 82–91. [Google Scholar] [CrossRef]
- Dushianthan, A.; Cusack, R.; Goss, V.; Postle, A.D.; Grocott, M.P. Clinical review: Exogenous surfactant therapy for acute lung injury/acute respiratory distress syndrome—Where do we go from here? Crit. Care 2012, 16, 238. [Google Scholar] [CrossRef]
- Arbibe, L.; Koumanov, K.; Vial, D.; Rougeot, C.; Faure, G.; Havet, N.; Longacre, S.; Vargaftig, B.B.; Bereziat, G.; Voelker, D.R.; et al. Generation of lyso-phospholipids from surfactant in acute lung injury is mediated by type-ii phospholipase a2 and inhibited by a direct surfactant protein a-phospholipase a2 protein interaction. J. Clin. Investig. 1998, 102, 1152–1160. [Google Scholar] [CrossRef]
- Holm, B.A.; Matalon, S. Role of pulmonary surfactant in the development and treatment of adult respiratory distress syndrome. Anesth. Analg. 1989, 69, 805–818. [Google Scholar] [CrossRef]
- Simonato, M.; Baritussio, A.; Ori, C.; Vedovelli, L.; Rossi, S.; Dalla Massara, L.; Rizzi, S.; Carnielli, V.P.; Cogo, P.E. Disaturated-phosphatidylcholine and surfactant protein-b turnover in human acute lung injury and in control patients. Respir. Res. 2011, 12, 36. [Google Scholar] [CrossRef]
- Ainsworth, S.B.; Milligan, D.W. Surfactant therapy for respiratory distress syndrome in premature neonates: A comparative review. Am. J. Respir. Med. 2002, 1, 417–433. [Google Scholar] [CrossRef]
- Willson, D.F.; Notter, R.H. The future of exogenous surfactant therapy. Respir. Care 2011, 56, 1369–1386. [Google Scholar] [CrossRef] [PubMed]
- Willson, D.F.; Thomas, N.J.; Tamburro, R.; Truemper, E.; Truwit, J.; Conaway, M.; Traul, C.; Egan, E.E. Pediatric calfactant in acute respiratory distress syndrome trial. Pediatr. Crit. Care Med. 2013, 14, 657–665. [Google Scholar] [CrossRef]
- Meng, S.S.; Chang, W.; Lu, Z.H.; Xie, J.F.; Qiu, H.B.; Yang, Y.; Guo, F.M. Effect of surfactant administration on outcomes of adult patients in acute respiratory distress syndrome: A meta-analysis of randomized controlled trials. BMC Pulm. Med. 2019, 19, 9. [Google Scholar] [CrossRef] [PubMed]
- Proudfoot, A.G.; Hind, M.; Griffiths, M.J. Biomarkers of acute lung injury: Worth their salt? BMC Med. 2011, 9, 132. [Google Scholar] [CrossRef] [PubMed]
- Cornfield, D.N. Acute respiratory distress syndrome in children: Physiology and management. Curr. Opin. Pediatr. 2013, 25, 338–343. [Google Scholar] [CrossRef]
- Cogo, P.E.; Gucciardi, A.; Traldi, U.; Hilkert, A.W.; Verlato, G.; Carnielli, V. Measurement of pulmonary surfactant disaturated-phosphatidylcholine synthesis in human infants using deuterium incorporation from body water. J. Mass. Spectrom. 2005, 40, 876–881. [Google Scholar] [CrossRef]
- Cavicchioli, P.; Zimmermann, L.J.; Cogo, P.E.; Badon, T.; Giordano, G.; Torresin, M.; Zacchello, F.; Carnielli, V.P. Endogenous surfactant turnover in preterm infants with respiratory distress syndrome studied with stable isotope lipids. Am. J. Respir. Crit. Care Med. 2001, 163, 55–60. [Google Scholar] [CrossRef]
- Cogo, P.E.; Toffolo, G.M.; Ori, C.; Vianello, A.; Chierici, M.; Gucciardi, A.; Cobelli, C.; Baritussio, A.; Carnielli, V.P. Surfactant disaturated-phosphatidylcholine kinetics in acute respiratory distress syndrome by stable isotopes and a two compartment model. Respir. Res. 2007, 8, 13. [Google Scholar] [CrossRef]
- Bernhard, W.; Pynn, C.J.; Jaworski, A.; Rau, G.A.; Hohlfeld, J.M.; Freihorst, J.; Poets, C.F.; Stoll, D.; Postle, A.D. Mass spectrometric analysis of surfactant metabolism in human volunteers using deuteriated choline. Am. J. Respir. Crit. Care Med. 2004, 170, 54–58. [Google Scholar] [CrossRef]
- Postle, A.D.; Clark, H.W.; Fink, J.; Madsen, J.; Koster, G.; Panchal, M.; Djukanovic, R.; Brealey, D.; Grocott, M.P.W.; Dushianthan, A. Rapid Phospholipid Turnover after Surfactant Nebulization in Severe COVID-19 Infection: A Randomized Clinical Trial. Am. J. Respir. Crit. Care Med. 2022, 205, 471–473. [Google Scholar] [CrossRef]
- Postle, A.D.; Hunt, A.N. Dynamic lipidomics with stable isotope labelling. J. Chromatogr. B Analyt Technol. Biomed. Life Sci. 2009, 877, 2716–2721. [Google Scholar] [CrossRef] [PubMed]
- Postle, A.D.; Wilton, D.C.; Hunt, A.N.; Attard, G.S. Probing phospholipid dynamics by electrospray ionisation mass spectrometry. Prog. Lipid Res. 2007, 46, 200–224. [Google Scholar] [CrossRef] [PubMed]
- Fagone, P.; Jackowski, S. Phosphatidylcholine and the CDP-choline cycle. Biochim. Biophys. Acta 2013, 1831, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Vance, D.E. Phospholipid methylation in mammals: From biochemistry to physiological function. Biochim. Biophys. Acta 2014, 1838, 1477–1487. [Google Scholar] [CrossRef]
- Wang, B.; Tontonoz, P. Phospholipid Remodeling in Physiology and Disease. Annu. Rev. Physiol. 2019, 81, 165–188. [Google Scholar] [CrossRef]
- Dushianthan, A.; Grocott, M.P.W.; Murugan, G.S.; Wilkinson, T.M.A.; Postle, A.D. Pulmonary Surfactant in Adult ARDS: Current Perspectives and Future Directions. Diagnostics 2023, 13, 2964. [Google Scholar] [CrossRef]
- ARDS Definition Task Force; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar]
- Proudfoot, A.G.; McAuley, D.F.; Hind, M.; Griffiths, M.J. Translational research: What does it mean, what has it delivered and what might it deliver? Curr. Opin. Crit. Care 2011, 17, 495–503. [Google Scholar] [CrossRef]
- Agassandian, M.; Mallampalli, R.K. Surfactant phospholipid metabolism. Biochim. Biophys. Acta 2013, 1831, 612–625. [Google Scholar] [CrossRef]
- Albert, R.K. Constant VT ventilation and surfactant dysfunction. An overlooked cause of ventilator-induced lung injury. Am. J. Resp. Crit. Care Med. 2022, 205, 152–160. [Google Scholar] [CrossRef]
- Nicholas, T.E.; Power, J.H.; Barr, H.A. Surfactant homeostasis in the rat lung during swimming exercise. J. Appl. Physiol. 1982, 53, 1521–1528. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, T.E.; Power, J.H.; Barr, H.A. The pulmonary consequences of a deep breath. Respir. Physiol. 1982, 49, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Bligh, E.G.; Dyer, W.J. A rapid method of total lipid extraction and purification. Can. J. Biochem. Physiol. 1959, 37, 911–917. [Google Scholar] [CrossRef] [PubMed]

| Variable | Patients (n = 9) |
|---|---|
| Age (days) | 526 (±436) |
| Weight (kg) | 7.6 (±3.6) |
| Curosurf dose (mg) | 761 (±361) |
| Time from intubation to methyl-D9 choline infusion (hours) | 66.7 (±7.3) |
| PaO2/FiO2 ratio at enrolment (mmHg) | 166 (±19) |
| Diagnosis at admission | |
| n = 4 |
| n = 3 |
| n = 1 |
| n = 1 |
| Duration of mechanical ventilation (days) | 8.3 (±0.5) |
| ECMO (n, %) | 1 (11.1%) |
| Survival (n, %) | 9 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goss, V.M.; Dushianthan, A.; McCorkell, J.; Morton, K.; Goss, K.C.W.; Marsh, M.J.; Pappachan, J.V.; Postle, A.D. Surfactant Phospholipid Kinetics in Ventilated Children after Therapeutic Surfactant Supplementation. Int. J. Mol. Sci. 2024, 25, 10480. https://doi.org/10.3390/ijms251910480
Goss VM, Dushianthan A, McCorkell J, Morton K, Goss KCW, Marsh MJ, Pappachan JV, Postle AD. Surfactant Phospholipid Kinetics in Ventilated Children after Therapeutic Surfactant Supplementation. International Journal of Molecular Sciences. 2024; 25(19):10480. https://doi.org/10.3390/ijms251910480
Chicago/Turabian StyleGoss, Victoria M., Ahilanandan Dushianthan, Jenni McCorkell, Katy Morton, Kevin C. W. Goss, Michael J. Marsh, John V. Pappachan, and Anthony D. Postle. 2024. "Surfactant Phospholipid Kinetics in Ventilated Children after Therapeutic Surfactant Supplementation" International Journal of Molecular Sciences 25, no. 19: 10480. https://doi.org/10.3390/ijms251910480






