An Instrumented Apartment to Monitor Human Behavior: A Pilot Case Study in the NeuroTec Loft
Abstract
:1. Introduction
2. Materials and Methods
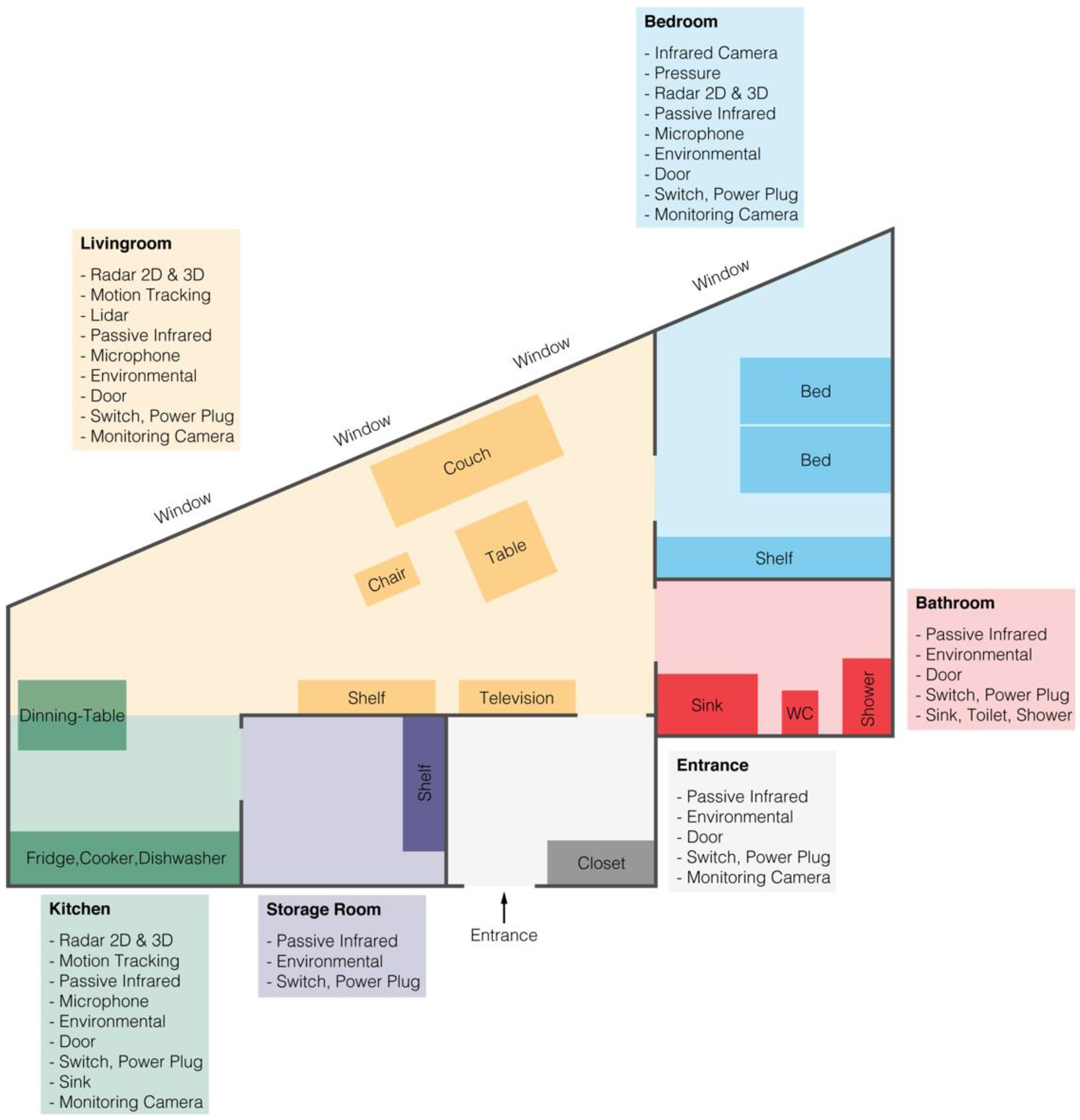
2.1. The Instrumented Apartment
2.2. The Data Flow and Analysis
2.3. Participant and Experiment
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Andersen, C.K.; Wittrup-Jensen, K.U.; Lolk, A.; Andersen, K.; Kragh-Sørensen, P. Ability to perform activities of daily living is the main factor affecting quality of life in patients with dementia. Health Qual. Life Outcomes 2004, 2, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mattimore, T.J.; Wenger, N.S.; Desbiens, N.A.; Teno, J.M.; Hamel, M.B.; Liu, H.; Califf, R.; Connors Jr, A.F.; Lynn, J.; Oye, R.K. Surrogate and physician understanding of patients’ preferences for living permanently in a nursing home. J. Am. Geriatr. Soc. 1997, 45, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Saner, H.; Schütz, N.; Botros, A.; Urwyler, P.; Buluschek, P.; Du Pasquier, G.; Nef, T. Potential of ambient sensor systems for early detection of health problems in older adults. Front. Cardiovasc. Med. 2020, 7. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Stroulia, E.; Nikolaidis, I.; Miguel-Cruz, A.; Rincon, A.R. Smart homes and home health monitoring technologies for older adults: A systematic review. Int. J. Med. Inform. 2016, 91, 44–59. [Google Scholar] [CrossRef] [PubMed]
- Iakovakis, D.; Hadjidimitriou, S.; Charisis, V.; Bostantzopoulou, S.; Katsarou, Z.; Hadjileontiadis, L.J. Touchscreen typing-pattern analysis for detecting fine motor skills decline in early-stage Parkinson’s disease. Sci. Rep. 2018, 8, 7662. [Google Scholar] [CrossRef] [PubMed]
- Schindhelm, C.K. Activity recognition and step detection with smartphones: Towards terminal based indoor positioning system. In Proceedings of the 2012 IEEE 23rd International Symposium on Personal, Indoor and Mobile Radio Communications-(PIMRC), Sydney, Australia, 9–12 September 2012; pp. 2454–2459. [Google Scholar]
- Schütz, N.; Saner, H.; Rudin, B.; Botros, A.; Pais, B.; Santschi, V.; Buluschek, P.; Gatica-Perez, D.; Urwyler, P.; Marchal-Crespo, L. Validity of pervasive computing based continuous physical activity assessment in community-dwelling old and oldest-old. Sci. Rep. 2019, 9, 9662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aicha, A.N.; Englebienne, G.; Kröse, B. Continuous gait velocity analysis using ambient sensors in a smart home. In Proceedings of the European Conference on Ambient Intelligence 2015, Athens, Greece, 11–13 November 2015; pp. 219–235. [Google Scholar] [CrossRef] [Green Version]
- Romeo, L.; Marani, R.; Lorusso, N.; Angelillo, M.T.; Cicirelli, G. Vision-based assessment of balance control in elderly people. In Proceedings of the 2020 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Bari, Italy, 1 June–1 July 2020; pp. 1–6. [Google Scholar]
- Ranta, J.; Aittokoski, T.; Tenhunen, M.; Alasaukko-Oja, M. EMFIT QS heart rate and respiration rate validation. Biomed. Phys. Eng. Express 2019, 5, 025016. [Google Scholar] [CrossRef]
- Kim, K.J.; Gimmon, Y.; Millar, J.; Schubert, M.C. Using inertial sensors to quantify postural sway and gait performance during the tandem walking test. Sensors 2019, 19, 751. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunn, J.; Runge, R.; Snyder, M. Wearables and the medical revolution. Pers. Med. 2018, 15, 429–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, X.; Ellul, J.; Azzopardi, G. Elderly Fall Detection Systems: A Literature Survey. Front. Robot. AI 2020, 7, 71. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Spicher, N.; Warnecke, J.M.; Haghi, M.; Schwartze, J.; Deserno, T.M. Unobtrusive health monitoring in private spaces: The smart home. Sensors 2021, 21, 864. [Google Scholar] [CrossRef] [PubMed]
- Son, H.; Kim, H. A Pilot Study to Test the Feasibility of a Home Mobility Monitoring System in Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2019, 16, 1512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chew, E.Y.; Clemons, T.E.; Bressler, S.B.; Elman, M.J.; Danis, R.P.; Domalpally, A.; Heier, J.S.; Kim, J.E.; Garfinkel, R.; Group, A.-H.S.R. Randomized trial of a home monitoring system for early detection of choroidal neovascularization home monitoring of the Eye (HOME) study. Ophthalmology 2014, 121, 535–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathie, M.J.; Coster, A.C.; Lovell, N.H.; Celler, B.G. Accelerometry: Providing an integrated, practical method for long-term, ambulatory monitoring of human movement. Physiol. Meas. 2004, 25, R1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tegou, T.; Kalamaras, I.; Tsipouras, M.; Giannakeas, N.; Votis, K.; Tzovaras, D. A Low-Cost Indoor Activity Monitoring System for Detecting Frailty in Older Adults. Sensors 2019, 19, 452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stavropoulos, T.G.; Papastergiou, A.; Mpaltadoros, L.; Nikolopoulos, S.; Kompatsiaris, I. IoT Wearable Sensors and Devices in Elderly Care: A Literature Review. Sensors 2020, 20, 2826. [Google Scholar] [CrossRef] [PubMed]
- Jacob Rodrigues, M.; Postolache, O.; Cercas, F. Physiological and Behavior Monitoring Systems for Smart Healthcare Environments: A Review. Sensors 2020, 20, 2186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butpheng, C.; Yeh, K.-H.; Xiong, H. Security and Privacy in IoT-Cloud-Based e-Health Systems—A Comprehensive Review. Symmetry 2020, 12, 1191. [Google Scholar] [CrossRef]
- Sedgwick, P.; Greenwood, N. Understanding the Hawthorne effect. BMJ 2015, 351, h4672. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Primary Parameters | Technology | Signal Format | Time | Contactless | Gold * | Device | |||
|---|---|---|---|---|---|---|---|---|---|
| Day | Night | Yes | No | ||||||
| Physiological | Heart rate, Breathing rate | Pressure Sensor | Piezoelectrical | X | X | EMFIT, Finland | |||
| Heart rate, Breathing rate | Radar Sensor 2D & 3D | Electromagnetic | X | X | Somnofy, Norway | ||||
| Blood pressure, Heart rate, Breathing rate | Infrared Camera | Temperature Image | X | X | Optris, Germany | ||||
| Skin resistance | Galvanic Sensor | Electrodermal activity | X | Empatica, United States of America, | |||||
| Heart rate, Breathing rate, Blood pressure, Oxygen saturation | Mobile polysomnography (Pleth- Sensor, Electrocardiogram (ECG)) | Reflection of light, Electrical activity | X | X | X | X | Somnomedics, Germany | ||
| Movement | Pressure Sensor | Piezoelectrical | X | X | SensingTex, Spain | ||||
| Radar Sensor 2D & 3D | Electromagnetic | X | X | Somnofy, Norway, RFbeam, Switzerland | |||||
| Accelerometer | Rate of change of velocity | X | X | X | Axivity, United Kingdom | ||||
| Gyroscope | Orientation and angular velocity | X | X | GaitUp, Switzerland | |||||
| Motion Tracking System | Video Image | X | X | X | Qualisis, Sweden | ||||
| Lidar-, PIR-sensors | Reflection of light | X | X | Hokuyo, Japan | |||||
| Environmental | Speech, Ambient noise | Microphone | Sound | X | X | X | Sennheiser, Germany | ||
| Illuminance, Humidity, Temperature | Environmental Sensor | Light, Humidity, Temperature | X | X | X | Rohm, Japan | |||
| Doors open and closed | Door sensor | Magnetic | X | X | Domosafety, Switzerland | ||||
| Devices on and off | Switch, Power plug | Electrical current | X | X | Shelly, United States | ||||
| Water on and off | Sink & Shower Senor | Water flow | X | X | Swissflow, Netherlands | ||||
| Sensor Type | n | Mean [ms] | Std [ms] | q25 [ms] | q75 [ms] |
|---|---|---|---|---|---|
| Flow Meters | 2,597,253 | 1087.38 | 100,928.71 | 1000 | 1000 |
| Door Sensors | 2,072,136 | 1946.29 | 36,916,172.47 | 1000 | 2000 |
| Power Meters | 2,274,511 | 666.66 | 47,101,113.59 | 333.33 | 1000 |
| Environmental Sensors | 935,192 | 2393.46 | 1362.13 | 1000 | 4000 |
| Bed Pressure Sensors | 566,748 | 2306.95 | 913,374.84 | 1000 | 1000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gerber, S.M.; Single, M.; Knobel, S.E.J.; Schütz, N.; Bruhin, L.C.; Botros, A.; Naef, A.C.; Schindler, K.A.; Nef, T. An Instrumented Apartment to Monitor Human Behavior: A Pilot Case Study in the NeuroTec Loft. Sensors 2022, 22, 1657. https://doi.org/10.3390/s22041657
Gerber SM, Single M, Knobel SEJ, Schütz N, Bruhin LC, Botros A, Naef AC, Schindler KA, Nef T. An Instrumented Apartment to Monitor Human Behavior: A Pilot Case Study in the NeuroTec Loft. Sensors. 2022; 22(4):1657. https://doi.org/10.3390/s22041657
Chicago/Turabian StyleGerber, Stephan M., Michael Single, Samuel E. J. Knobel, Narayan Schütz, Lena C. Bruhin, Angela Botros, Aileen C. Naef, Kaspar A. Schindler, and Tobias Nef. 2022. "An Instrumented Apartment to Monitor Human Behavior: A Pilot Case Study in the NeuroTec Loft" Sensors 22, no. 4: 1657. https://doi.org/10.3390/s22041657







