Efficacy of Lesion Specific Portals in Endoscopic Treatment of Calcaneal Bone Cyst: A Case Report and Literature Review
Abstract
:1. Background
2. Case Presentation
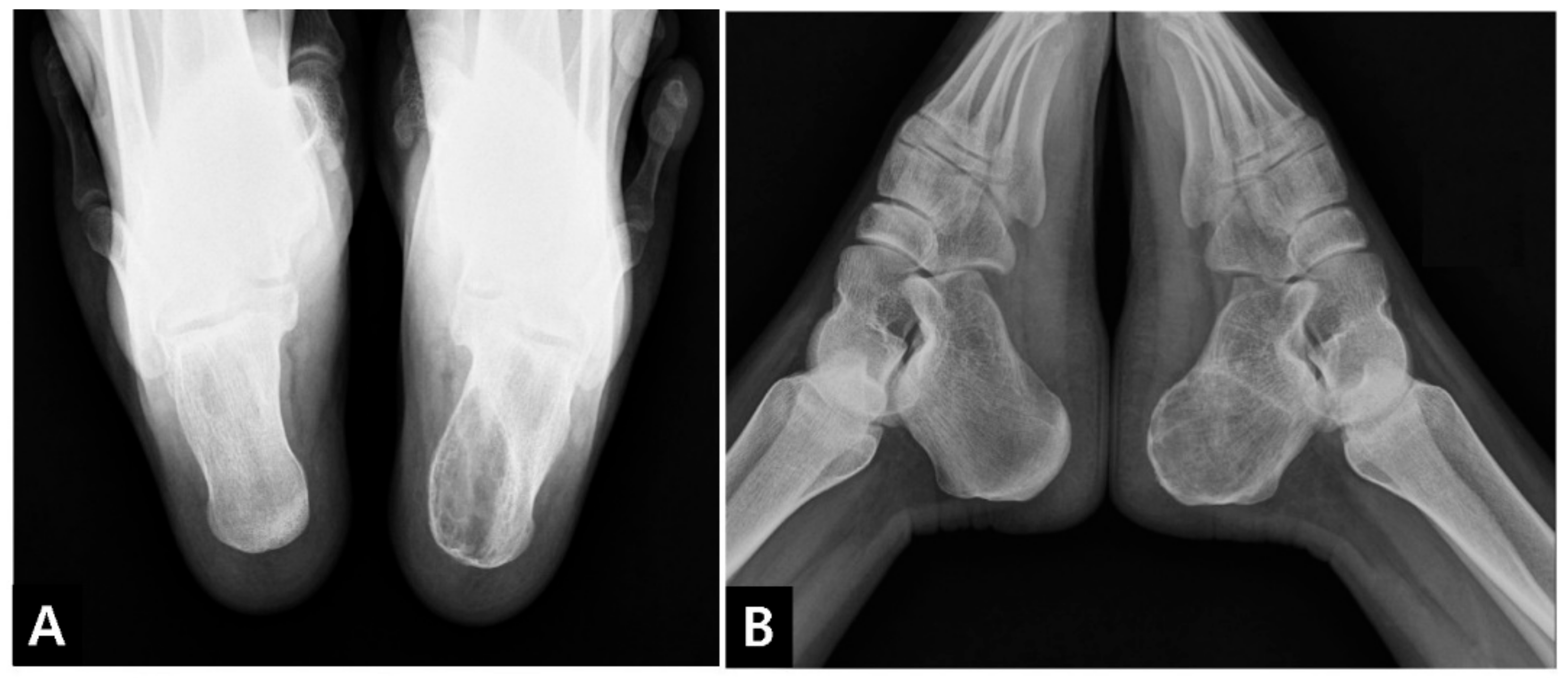
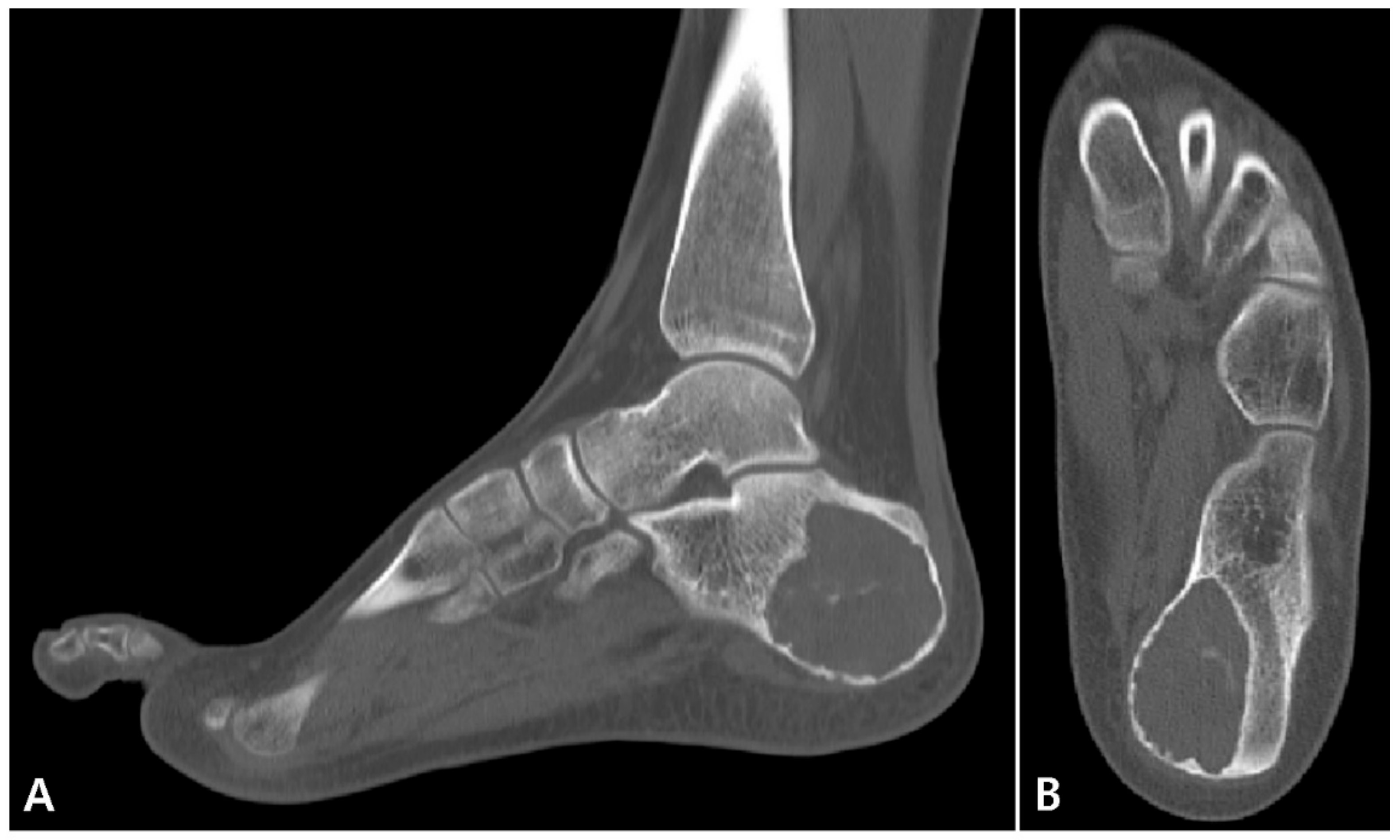
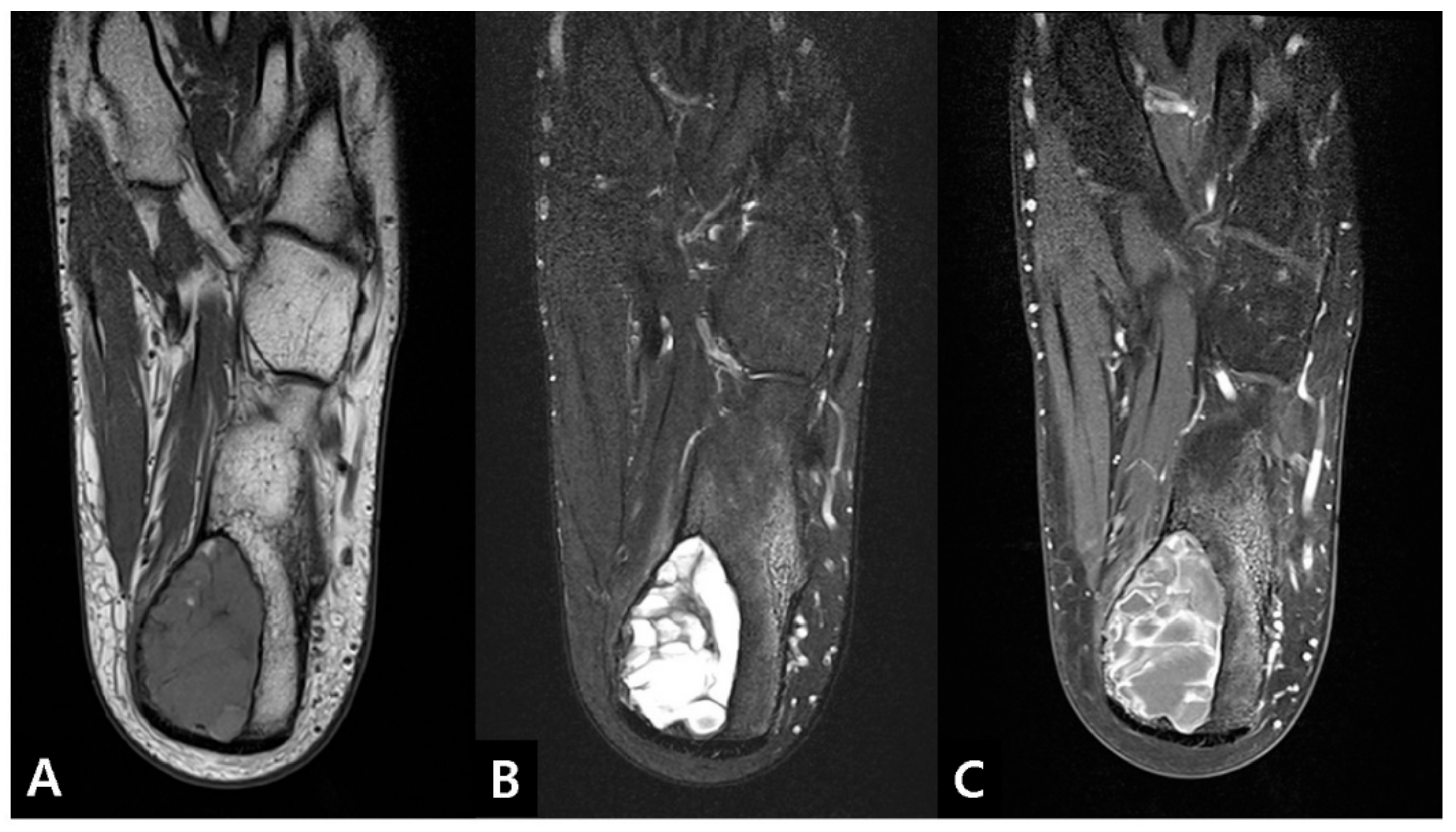
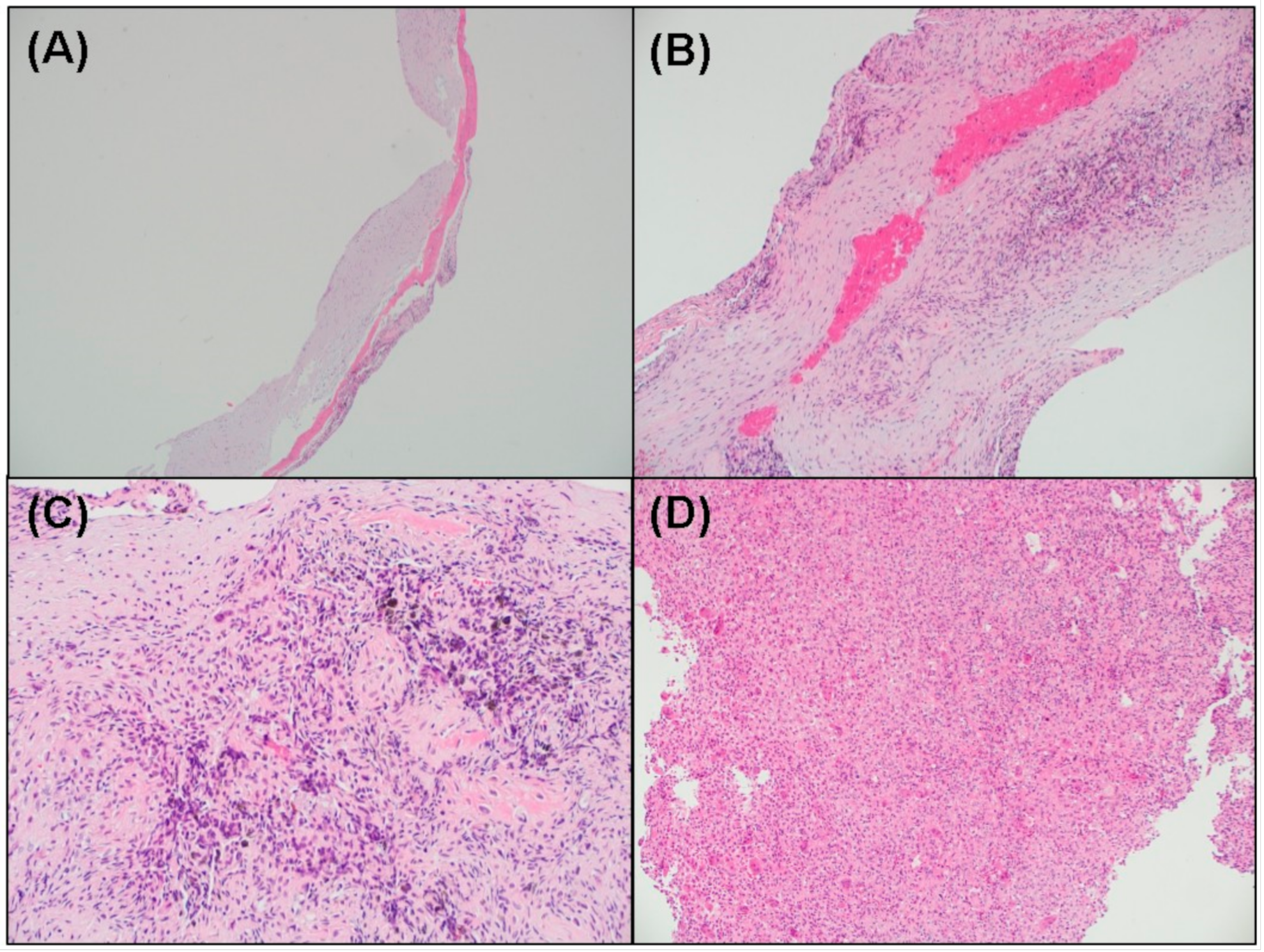
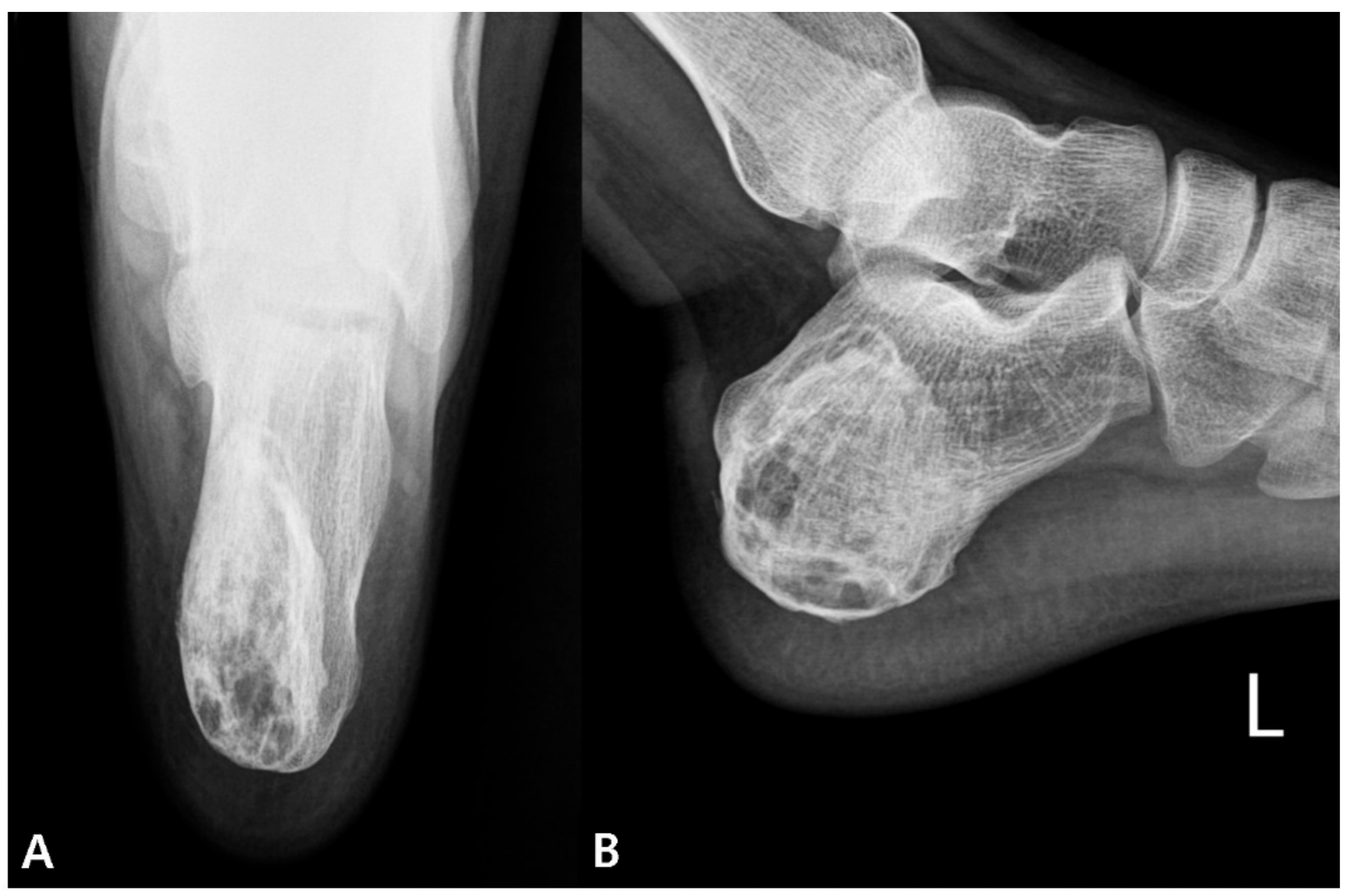
2.1. Preoperative Evaluation
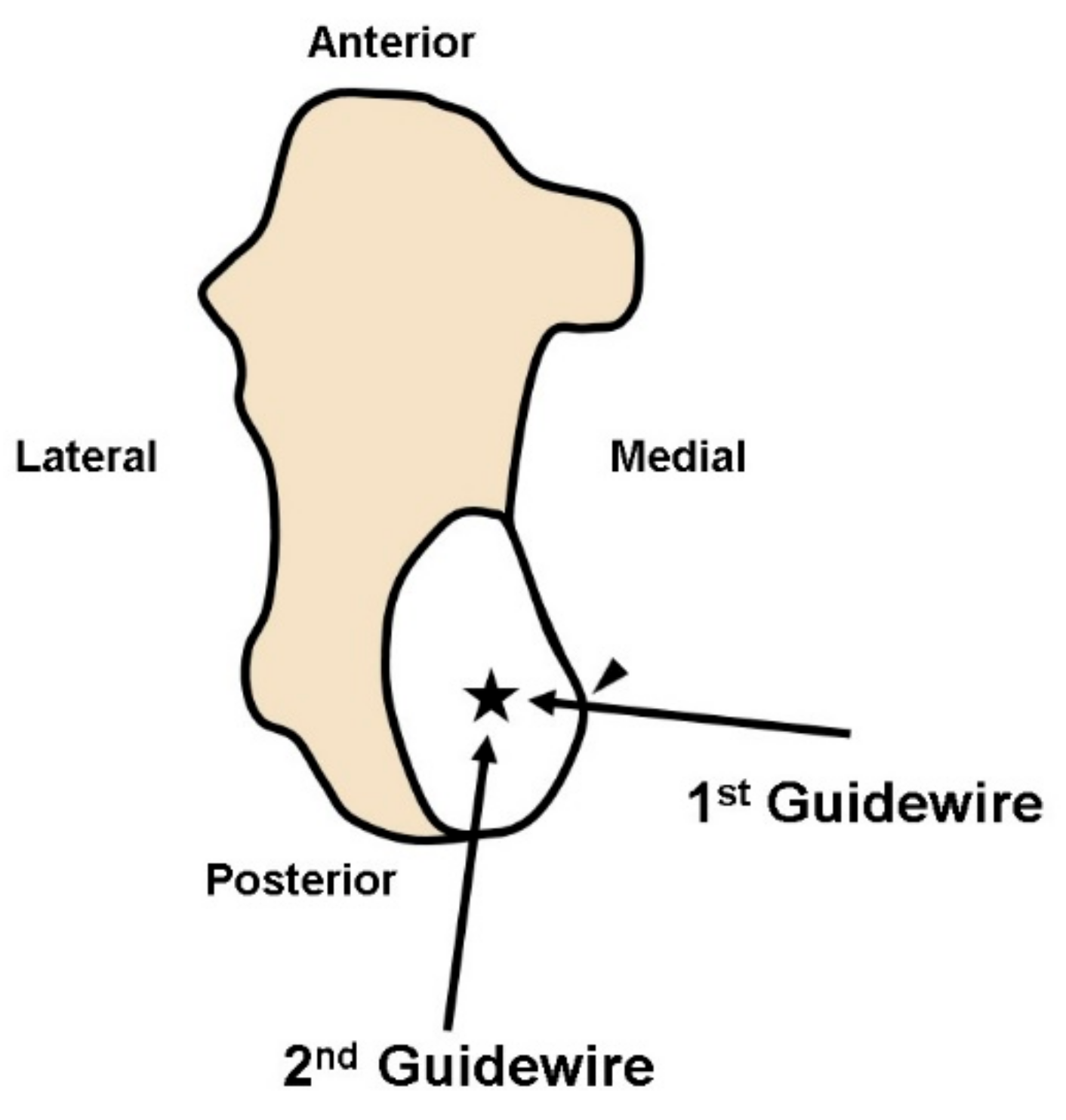
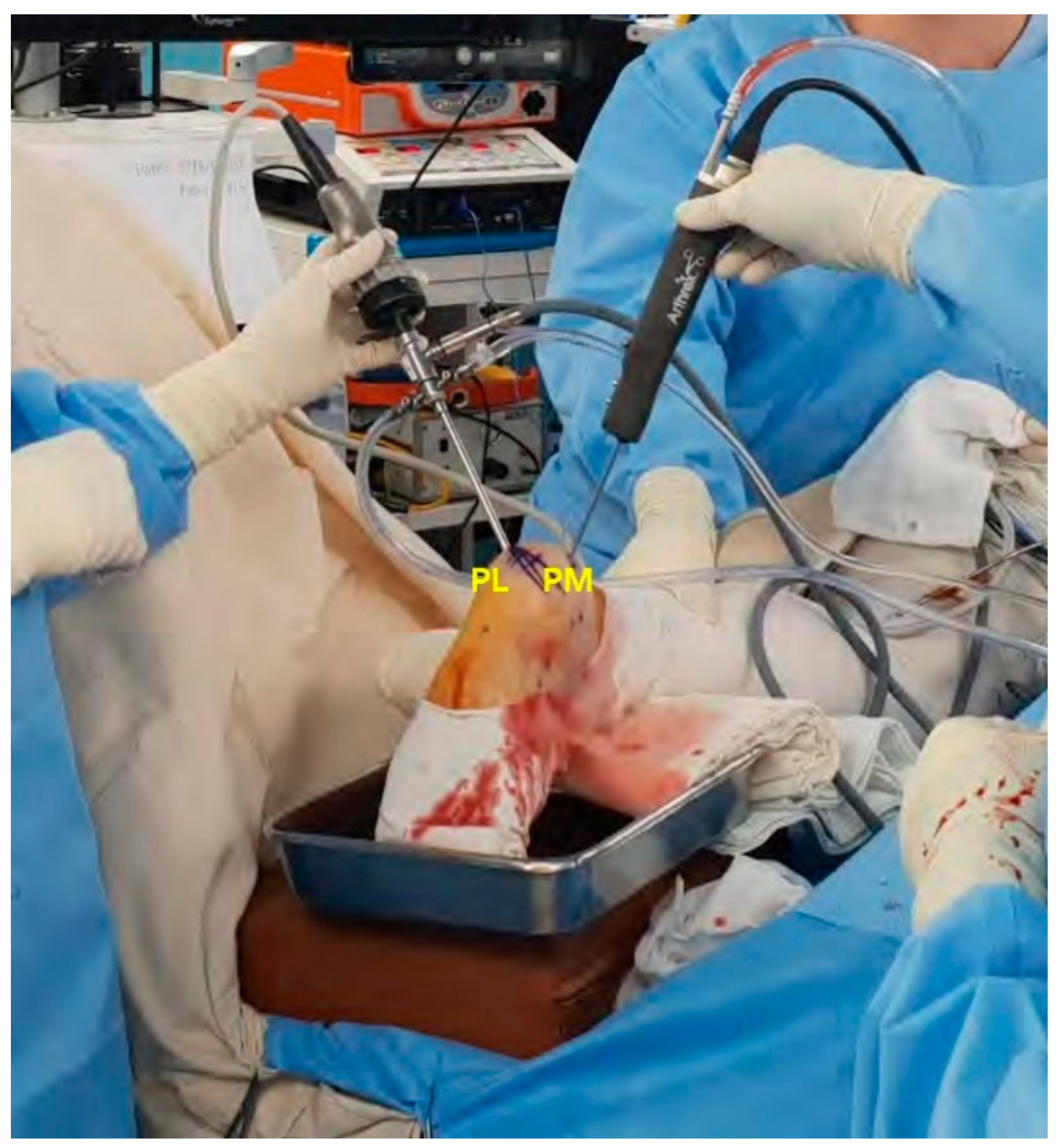
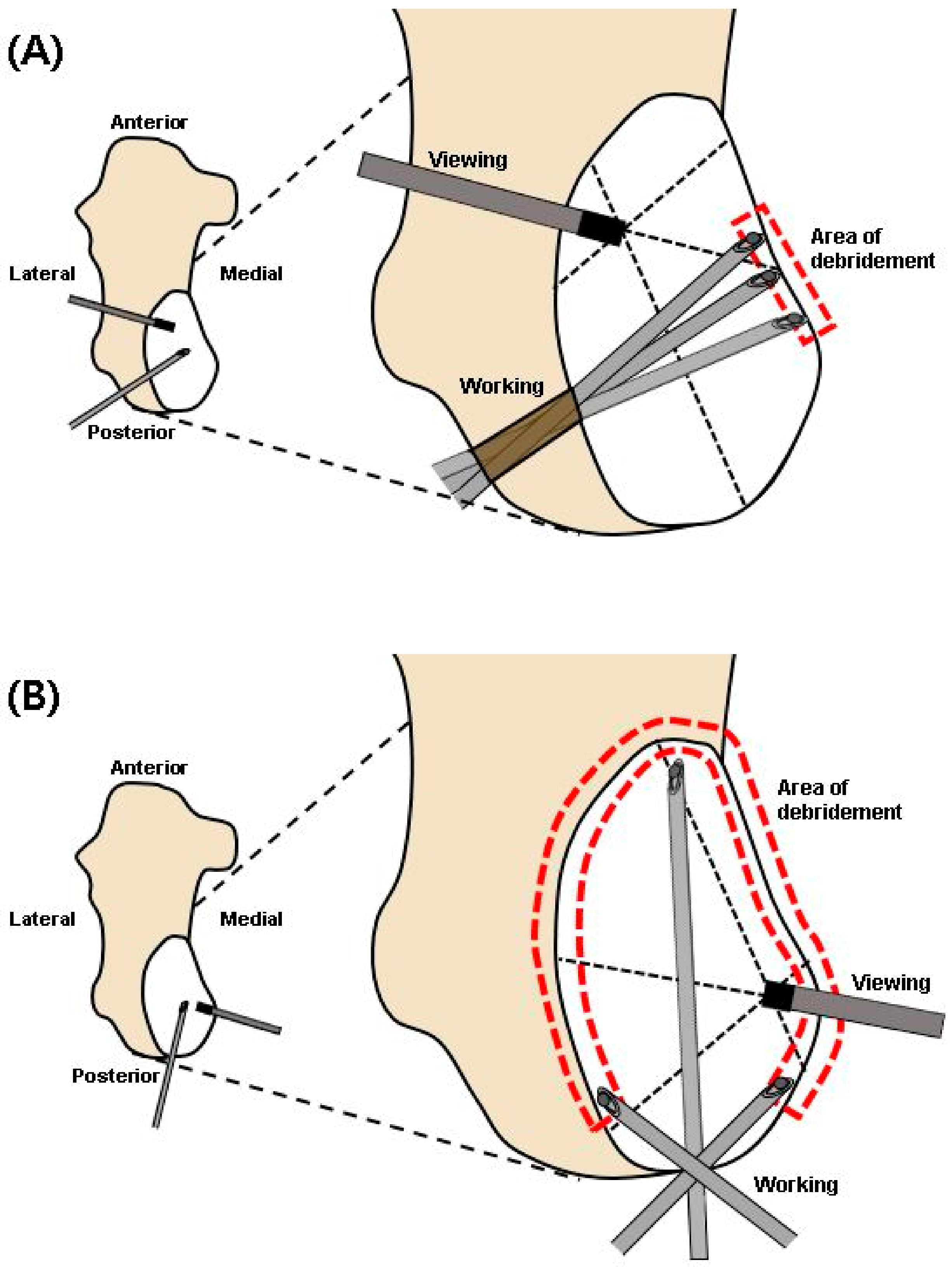
2.2. Surgical Procedure
2.3. Postoperative Progression
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SBC | simple bone cyst |
| CT | computed tomography |
| ABC | aneurysmal bone cyst |
| DBM | Demineralized bone material |
| PMMA | polymethylmethacrylate |
References
- Yan, L.; Zong, J.; Chu, J.; Wang, W.; Li, M.; Wang, X.; Song, M.; Wang, S. Primary tumours of the calcaneus. Oncol. Lett. 2018, 15, 8901–8914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noordin, S.; Allana, S.; Umer, M.; Jamil, M.; Hilal, K.; Uddin, N. Unicameral bone cysts: Current concepts. Ann. Med. Surg. 2018, 34, 43–49. [Google Scholar] [CrossRef]
- Dormans, J.; Pill, S. Fractures through bone cysts: Unicameral bone cysts, aneurysmal bone cysts, fibrous cortical defects, and nonossifying fibromas. Instr. Course Lect. 2002, 51, 457–467. [Google Scholar]
- Pretell-Mazzini, J.; Murphy, R.F.; Kushare, I.; Dormans, J.P. Unicameral bone cysts: General characteristics and management controversies. J. Am. Acad. Orthop. Surg. 2014, 22, 295–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mainard, D.; Galois, L. Treatment of a solitary calcaneal cyst with endoscopic curettage and percutaneous injection of calcium phosphate cement. J. Foot Ankle Surg. Off. Publ. Am. Coll. Foot Ankle Surg. 2006, 45, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Kadhim, M.; Thacker, M.; Kadhim, A.; Holmes, L., Jr. Treatment of unicameral bone cyst: Systematic review and meta analysis. J. Child. Orthop. 2014, 8, 171–191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoshi, M.; Oebisu, N.; Iwai, T.; Shimatani, A.; Takada, N.; Aono, M.; Ieguchi, M.; Takami, M.; Nakamura, H. Possible pathogenesis of calcaneal bone cysts. Arch. Orthop. Trauma Surg. 2019, 140, 1303–1310. [Google Scholar] [CrossRef]
- Innami, K.; Takao, M.; Miyamoto, W.; Abe, S.; Nishi, H.; Matsushita, T. Endoscopic surgery for young athletes with symptomatic unicameral bone cyst of the calcaneus. Am. J. Sports Med. 2011, 39, 575–581. [Google Scholar] [CrossRef]
- Stoica, I.; Pop, D.; Grosu, F. Unicameral bone cyst of the calcaneus-minimally invasive endoscopic surgical treatment. Case report. Rom. J. Morphol. Embryol. Rev. Roum. Morphol. Embryol. 2017, 58, 689–693. [Google Scholar]
- Toepfer, A.; Lenze, U.; Harrasser, N. Calcaneal ossoscopy. Arthrosc Tech. 2016, 5, 627–631. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.; Chung, C.; Kwon, S.; Sung, K.; Lee, S.; Won, S.; Lee, D.; Lee, S.; Park, M. Transcultural adaptation and testing psychometric properties of the Korean version of the Foot and Ankle Outcome Score (FAOS). Clin. Rheumatol. 2013, 32, 1443–1450. [Google Scholar] [CrossRef]
- Otsuka, T.; Kobayashi, M.; Yonezawa, M.; Kamiyama, F.; Matsushita, Y.; Matsui, N. Treatment of chondroblastoma of the calcaneus with a secondary aneurysmal bone cyst using endoscopic curettage without bone grafting. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 2002, 18, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Bonnel, F.; Canovas, F.; Faure, P. Treatment of a simple bone cyst of the calcaneus by endoscopic curettage with cancellous bone injection. Acta Orthop. Belg. 1999, 65, 528–531. [Google Scholar] [PubMed]
- Aiba, H.; Kobayashi, M.; Waguri-Nagaya, Y.; Goto, H.; Mizutani, J.; Yamada, S.; Okamoto, H.; Nozaki, M.; Mitsui, H.; Miwa, S.; et al. Treatment of simple bone cysts using endoscopic curettage: A case series analysis. J. Orthop. Surg. Res. 2018, 13, 168. [Google Scholar] [CrossRef]
- Choi, Y.; Kwak, J.M.; Chung, S.H.; Jung, G.H.; Kim, J.D. Tumor treated by endoscopy. Clin. Orthop. Surg. 2014, 6, 72–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, G.-H.; Kim, J.-D.; Kim, J.-Y. Treatment of Simple Bone Cyst in Calcaneus with Endoscopic Curettage and Autologous Bone Graft-Case Report. J. Kor. Bone Jt. Tumor Soci. 2008, 14, 182–186. [Google Scholar]
- Koo, B.-S.; Kim, K.-C.; Choi, J.-Y.; Jeong, H.-J.; Shin, H.-K.; Hong, C.-U.J.J.o.K.F.; Society, A. Endoscopic Curettage and Bone Graft of Simple Bone Cyst in the Calcaneus. J. Kor. Foot Ankle Soci. 2001, 5, 69–73. [Google Scholar]
- Nishimura, A.; Matsumine, A.; Kato, K.; Aasanuma, K.; Nakamura, T.; Fukuda, A.; Sudo, A. Endoscopic Versus Open Surgery for Calcaneal Bone Cysts: A Preliminary Report. J. Foot Ankle Surg. Off. Publ. Am. Coll. Foot Ankle Surg. 2016, 55, 782–787. [Google Scholar] [CrossRef]
- Yildirim, C.; Akmaz, I.; Sahin, O.; Keklikci, K. Simple calcaneal bone cysts: A pilot study comparing open versus endoscopic curettage and grafting. J. Bone Jt. Surg. Br. 2011, 93, 1626–1631. [Google Scholar] [CrossRef] [Green Version]
- Benevenia, J.; Martinez, M.; Gehrmann, R.J.M.R.A. Arthroscopically Assisted Surgical Treatment of a Calcaneal Bone Cyst in an Athlete. Med. Res. Arch. 2015. Available online: https://esmed.org/MRA/mra/article/view/81 (accessed on 26 January 2021).
- Farouk, H.A.; Saladin, M.; Senna, W.A.; Ebeid, W. All-endoscopic management of benign bone lesions; a case series of 26 cases with minimum of 2 years follow-up. Sicot J. 2018, 4, 50. [Google Scholar] [CrossRef]
- Toepfer, A.; Lenze, U.; Gerdesmeyer, L.; Pohlig, F.; Harrasser, N. Endoscopic resection and allografting for benign osteolytic lesions of the calcaneus. Springerplus 2016, 5, 427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yıldırım, C.; Mahiroğulları, M.; Kuşkucu, M.; Akmaz, İ.; Keklikci, K. Treatment of a unicameral bone cyst of calcaneus with endoscopic curettage and percutaneous filling with corticocancellous allograft. J. Foot Ankle Surg. Off. Publ. Am. Coll. Foot Ankle Surg. 2010, 49, 93–97. [Google Scholar] [CrossRef]
- Pogoda, P.; Priemel, M.; Linhart, W.; Stork, A.; Adam, G.; Windolf, J.; Rueger, J.M.; Amling, M. Clinical relevance of calcaneal bone cysts: A study of 50 cysts in 47 patients. Clin. Orthop. Relat. Res. 2004, 424, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Weger, C.; Frings, A.; Friesenbichler, J.; Grimer, R.; Andreou, D.; Machacek, F.; Pfeiffenberger, K.; Liegl-Atzwanger, B.; Tunn, P.-U.; Leithner, A. Osteolytic lesions of the calcaneus: Results from a multicentre study. Int. Orthop. 2013, 37, 1851–1856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, E.V.; Leung, J.P. Complications of intraarticular calcaneal fractures. Clin. Orthop. Relat. Res. 2001, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Larson, J.; Chao, E.; Fitzgerald, R. Bypassing femoral cortical defects with cemented intramedullary stems. J. Orthop. Res. 1991, 9, 414–421. [Google Scholar] [CrossRef]
- Panjabi, M.M.; Trumble, T.; Hult, J.E.; Southwick, W.O. Effect of femoral stem length on stress raisers associated with revision hip arthroplasty. J. Orthop. Res. 1985, 3, 447–455. [Google Scholar] [CrossRef]
- Kaplanoğlu, V.; Ciliz, D.S.; Kaplanoğlu, H.; Elverici, E. Aneurysmal bone cyst of the calcaneus. J. Clin. Imaging Sci. 2014, 4, 60. [Google Scholar]
- Lenze, U.; Stolberg-Stolberg, J.; Pohlig, F.; Lenze, F.; von Eisenhart-Rothe, R.; Rechl, H.; Toepfer, A. Unicameral Bone Cyst in the Calcaneus of Mirror Image Twins. J. Foot Ankle Surg. Off. Publ. Am. Coll. Foot Ankle Surg. 2015, 54, 754–757. [Google Scholar] [CrossRef]
- O’Laughlin, S. Unicameral bone cyst of the calcaneus. J. Orthop. Sports Phys. Ther. 2012, 42, 43. [Google Scholar]
- Mohaidat, Z.M.; Al-gharaibeh, S.R.; Aljararhih, O.N.; Nusairat, M.T.; Al-omari, A.A. Challenges in the diagnosis and treatment of aneurysmal bone cyst in patients with unusual features. Adv. Orthop. 2019, 2019, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Authors | # | Type of Cyst | Portal Placement | Graft Material after Curettage | Recurrence |
|---|---|---|---|---|---|
| Mainard et al. [5] (2006) | 1 | SBC | One lateral | Calcium phosphate cement | No |
| Innami et al. [8] (2011) | 10 | SBC | Two lateral | Calcium phosphate cement | No |
| Stoica et al. [9] (2017) | 1 | SBC | Two lateral | Allograft | No |
| Bonnel et al. [13] (1999) | 1 | SBC | Two lateral | Autograft | No |
| Aiba et al. [14] (2018) | 6 | SBC | One medial, One lateral | None | No |
| Choi et al. [15] (2014) | 22 | SBC (9), Fibrous dysplasia (6) Enchondroma (5) Intraosseous lipoma (1) Brodie abscess (1) | Two lateral | Autograft or Allograft | Yes (One case) |
| Jung et al. [16] (2008) | 1 | SBC | Two lateral | Autograft | No |
| Koo et al. [17] (2001) | 3 | SBC | Two lateral | Autograft or Allograft | No |
| Nishimura et al. [18] (2016) | 8 | SBC | Two lateral | Calcium phosphate cement | No |
| Yildirim al. [19] (2011) | 13 | SBC | Two lateral | Allograft | No |
| Toepfer et al. [22] (2016) | 6 | SBC (6) IOL (4) | Two lateral | Allograft | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yi, Y.; Lee, J.S.; Kim, J.; Jin, S.Y.; Won, S.H.; Cho, J.; Chun, D.-I. Efficacy of Lesion Specific Portals in Endoscopic Treatment of Calcaneal Bone Cyst: A Case Report and Literature Review. Medicina 2021, 57, 111. https://doi.org/10.3390/medicina57020111
Yi Y, Lee JS, Kim J, Jin SY, Won SH, Cho J, Chun D-I. Efficacy of Lesion Specific Portals in Endoscopic Treatment of Calcaneal Bone Cyst: A Case Report and Literature Review. Medicina. 2021; 57(2):111. https://doi.org/10.3390/medicina57020111
Chicago/Turabian StyleYi, Young, Jeong Seok Lee, Jahyung Kim, So Young Jin, Sung Hun Won, Jaeho Cho, and Dong-Il Chun. 2021. "Efficacy of Lesion Specific Portals in Endoscopic Treatment of Calcaneal Bone Cyst: A Case Report and Literature Review" Medicina 57, no. 2: 111. https://doi.org/10.3390/medicina57020111







