Virtual Reality-Based Immersive Rehabilitation for Cognitive- and Behavioral-Impairment-Related Eating Disorders: A VREHAB Framework Scoping Review
Abstract
:1. Introduction
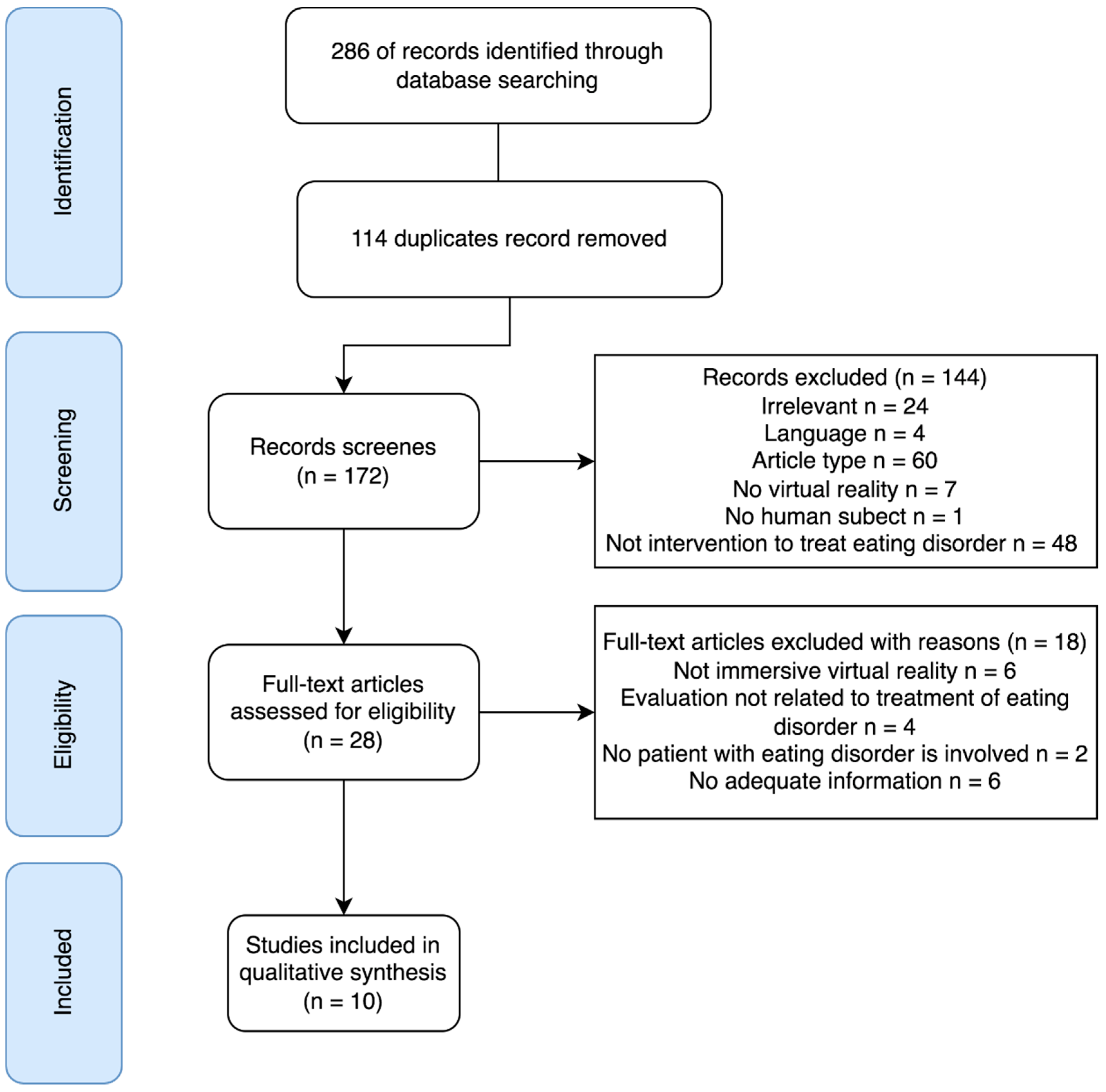
2. Materials and Methods
3. Search Results
4. Review Theme
4.1. Recipients and Providers
4.2. Virtual Environments and Objects
4.3. Application in Healthcare
4.3.1. Enhanced/Experimental Cognitive Behavior Therapy (ECT)
4.3.2. VR Based Cue Exposure Therapy (CET)
4.3.3. VR-Based Body Exposure Therapy (BET)
4.3.4. Treatment Effects
4.4. Social Engagement
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schultheis, M.T.; Rizzo, A.A. The application of virtual reality technology in rehabilitation. Rehabil. Psychol. 2001, 46, 296–311. [Google Scholar] [CrossRef]
- Howard, M.C. A meta-analysis and systematic literature review of virtual reality rehabilitation programs. Comput. Hum. Behav. 2017, 70, 317–327. [Google Scholar] [CrossRef]
- Demain, S.; Burridge, J.; Ellis-Hill, C.; Hughes, A.M.; Yardley, L.; Tedesco-Triccas, L.; Swain, I. Assistive technologies after stroke: Self-management or fending for yourself? A focus group study. BMC Health Serv. Res. 2013, 13, 334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fung, V.; Ho, A.; Shaffer, J.; Chung, E.; Gomez, M. Use of Nintendo Wii Fit™ in the rehabilitation of outpatients following total knee replacement: A preliminary randomised controlled trial. Physiotherapy 2012, 98, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Kwakkel, G.; van Peppen, R.; Wagenaar, R.C.; Wood Dauphinee, S.; Richards, C.; Ashburn, A.; Miller, K.; Lincoln, N.; Partridge, C.; Wellwood, I.; et al. Effects of augmented exercise therapy time after stroke: A meta-analysis. Stroke 2004, 35, 2529–2539. [Google Scholar] [CrossRef] [Green Version]
- Merians, A.S.; Jack, D.; Boian, R.; Tremaine, M.; Burdea, G.C.; Adamovich, S.V.; Recce, M.; Poizner, H. Virtual reality-augmented rehabilitation for patients following stroke. Phys. Ther. 2002, 82, 898–915. [Google Scholar] [CrossRef] [Green Version]
- Chau, P.H.; Kwok, Y.Y.J.; Chan, M.K.M.; Kwan, K.Y.D.; Wong, K.L.; Tang, Y.H.; Chau, K.L.P.; Lau, S.W.M.; Yiu, Y.Y.Y.; Kwong, M.Y.F. Feasibility, Acceptability, and Efficacy of Virtual Reality Training for Older Adults and People with Disabilities: Single-Arm Pre-Post Study. J. Med. Internet Res. 2021, 23, e27640. [Google Scholar] [CrossRef]
- Köyağasıoğlu, O.; Özgürbüz, C. The Effects of Virtual Reality Nonphysical Mental Training on Coordination and Skill Transfer in Healthy Adults. J. Sport Rehabil. 2022, 1, 442–451. [Google Scholar] [CrossRef]
- Larsen, C.R.; Soerensen, J.L.; Grantcharov, T.P.; Dalsgaard, T.; Schouenborg, L.; Ottosen, C.; Schroeder, T.V.; Ottesen, B.S. Effect of virtual reality training on laparoscopic surgery: Randomised controlled trial. BMJ 2009, 338, b1802. [Google Scholar] [CrossRef] [Green Version]
- Cheung, J.C.W.; Ni, M.; Tam, A.Y.C.; Chan, T.T.C.; Cheung, A.K.Y.; Tsang, O.Y.H.; Yip, C.B.; Lam, W.K.; Wong, D.W.C. Virtual Reality Based Multiple Life Skill Training for Intellectual Disability: A Multicenter Randomized Controlled Trial. Eng. Regen. 2022, 3, 121–130. [Google Scholar] [CrossRef]
- De Luca, R.; Lo Buono, V.; Leo, A.; Russo, M.; Aragona, B.; Leonardi, S.; Buda, A.; Naro, A.; Calabrò, R.S. Use of virtual reality in improving poststroke neglect: Promising neuropsychological and neurophysiological findings from a case study. Appl. Neuropsychol. Adult 2019, 26, 96–100. [Google Scholar] [CrossRef] [PubMed]
- De Luca, R.; Russo, M.; Naro, A.; Tomasello, P.; Leonardi, S.; Santamaria, F.; Desireè, L.; Bramanti, A.; Silvestri, G.; Bramanti, P. Effects of virtual reality-based training with BTs-Nirvana on functional recovery in stroke patients: Preliminary considerations. Int. J. Neurosci. 2018, 128, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Hsu, S.Y.; Fang, T.Y.; Yeh, S.C.; Su, M.C.; Wang, P.C.; Wang, V.Y. Three-dimensional, virtual reality vestibular rehabilitation for chronic imbalance problem caused by Ménière’s disease: A pilot study. Disabil. Rehabil. 2017, 39, 1601–1606. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; Latella, D.; Maresca, G.; Sciarrone, F.; Manuli, A.; Naro, A.; De Luca, R.; Calabrò, R.S. Virtual reality and cognitive rehabilitation in people with stroke: An overview. J. Neurosci. Nurs. 2019, 51, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Gaggioli, A. Advanced Technologies in Rehabilitation: Empowering Cognitive, Physical, Social and Communicative Skills through Virtual Reality, Robots, Wearable Systems and Brain-Computer Interfaces; IOS Press: Amsterdam, The Netherlands, 2009; p. 305. [Google Scholar]
- Weiss, P.L.; Kizony, R.; Feintuch, U.; Katz, N. Virtual reality in neurorehabilitation. In Textbook of Neural Repair and Rehabilitation: Volume 2: Medical Neurorehabilitation; Gage, F., Cohen, L., Selzer, M., Duncan, P., Clarke, S., Eds.; Cambridge University Press: Cambridge, UK, 2006; Volume 2, pp. 182–197. [Google Scholar]
- Hwang, N.K.; Choi, J.B.; Choi, D.-K.; Park, J.-M.; Hong, C.-W.; Park, J.-S.; Yoon, T.-H. Effects of Semi-Immersive Virtual Reality-Based Cognitive Training Combined with Locomotor Activity on Cognitive Function and Gait Ability in Community-Dwelling Older Adults. Healthcare 2021, 9, 814. [Google Scholar] [CrossRef] [PubMed]
- McEwen, D.; Taillon-Hobson, A.; Bilodeau, M.; Sveistrup, H.; Finestone, H. Two-week virtual reality training for dementia: Single-case feasibility study. J. Rehabil. Res. Dev. 2014, 51, 1069. [Google Scholar] [CrossRef]
- Kim, O.; Pang, Y.; Kim, J.-H. The effectiveness of virtual reality for people with mild cognitive impairment or dementia: A meta-analysis. BMC Psychiatry 2019, 19, 219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weng, W.; Liang, J.; Xue, J.; Zhu, T.; Jiang, Y.; Wang, J.; Chen, S. The Transfer Effects of Cognitive Training on Working Memory among Chinese Older Adults with Mild Cognitive Impairment: A Randomized Controlled Trial. Front. Aging Neurosci. 2019, 11, 212. [Google Scholar] [CrossRef] [Green Version]
- Amujo, A.; Akpor, O. Dementia and the gap in nutrition: A review. SJPH 2015, 3, 1–9. [Google Scholar]
- Jackson, J.; Currie, K.; Graham, C.; Robb, Y. The effectiveness of interventions to reduce undernutrition and promote eating in older adults with dementia: A systematic review. JBI Evid. Synth. 2011, 9, 1509–1550. [Google Scholar]
- Altman, S.E.; Shankman, S.A. What is the association between obsessive-compulsive disorder and eating disorders? Clin. Psychol Rev. 2009, 29, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Zakzanis, K.K.; Campbell, Z.; Polsinelli, A. Quantitative evidence for distinct cognitive impairment in anorexia nervosa and bulimia nervosa. J. Neuropsychol. 2010, 4, 89–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keel, P.K.; Forney, K.J. Psychosocial risk factors for eating disorders. Int. J. Eat. Disord. 2013, 46, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Katterman, S.N.; Goldstein, S.P.; Butryn, M.L.; Forman, E.M.; Lowe, M.R. Efficacy of an acceptance-based behavioral intervention for weight gain prevention in young adult women. J. Contextual Behav. Sci. 2014, 3, 45–50. [Google Scholar] [CrossRef]
- Kristeller, J.; Wolever, R.Q.; Sheets, V. Mindfulness-based eating awareness training (MB-EAT) for binge eating: A randomized clinical trial. Mindfulness 2014, 5, 282–297. [Google Scholar] [CrossRef]
- Brown, T.; Vogel, E.N.; Adler, S.; Bohon, C.; Bullock, K.; Nameth, K.; Riva, G.; Safer, D.L.; Runfola, C.D. Bringing virtual reality from clinical trials to clinical practice for the treatment of eating disorders: An example using virtual reality cue exposure therapy. J. Med. Internet Res. 2020, 22, e16386. [Google Scholar] [CrossRef]
- Campelo, A.M.; Hashim, J.A.; Weisberg, A.; Katz, L. Virtual Rehabilitation in the elderly: Benefits, issues, and considerations. In Proceedings of the 2017 International Conference on Virtual Rehabilitation (ICVR), Montreal, QC, Canada, 19–22 June 2017; pp. 1–2. [Google Scholar]
- Cesa, G.L.; Manzoni, G.M.; Bacchetta, M.; Castelnuovo, G.; Conti, S.; Gaggioli, A.; Mantovani, F.; Molinari, E.; Cárdenas-López, G.; Riva, G. Virtual reality for enhancing the cognitive behavioral treatment of obesity with binge eating disorder: Randomized controlled study with one-year follow-up. J. Med. Internet Res. 2013, 15, e113. [Google Scholar] [CrossRef]
- Marco, J.H.; Perpiñá, C.; Botella, C. Effectiveness of cognitive behavioral therapy supported by virtual reality in the treatment of body image in eating disorders: One year follow-up. Psychiatry Res. 2013, 209, 619–625. [Google Scholar] [CrossRef]
- Nameth, K.; Brown, T.; Bullock, K.; Adler, S.; Riva, G.; Safer, D.; Runfola, C. Translating virtual reality cue exposure therapy for binge eating into a real-world setting: An uncontrolled pilot study. J. Clin. Med. 2021, 10, 1511. [Google Scholar] [CrossRef]
- Perpiñá, C.; Botella, C.; Baños, R.; Marco, H.; Alcañiz, M.; Quero, S. Body image and virtual reality in eating disorders: Is exposure to virtual reality more effective than the classical body image treatment? CyberPsychol. Behav. 1999, 2, 149–155. [Google Scholar] [CrossRef]
- Porras-Garcia, B.; Serrano-Troncoso, E.; Carulla-Roig, M.; Soto-Usera, P.; Ferrer-Garcia, M.; Figueras-Puigderrajols, N.; Yilmaz, L.; Onur Sen, Y.; Shojaeian, N.; Gutiérrez-Maldonado, J. Virtual Reality Body Exposure Therapy for Anorexia Nervosa. A Case Report with Follow-Up Results. Front. Psychol. 2020, 11, 956. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Bacchetta, M.; Baruffi, M.; Rinaldi, S.; Vincelli, F.; Molinari, E. Virtual Reality-Based Experiential Cognitive Treatment of Obesity and Binge-Eating Disorders. Clin. Psychol. Psychother. 2000, 7, 209–219. [Google Scholar] [CrossRef]
- Riva, G.; Bacchetta, M.; Cesa, G.; Conti, S.; Molinari, E. Six-month follow-up of in-patient experiential cognitive therapy for binge eating disorders. Cyberpsychol. Behav. 2003, 6, 251–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riva, G.; Bacchetta, M.; Cesa, G.; Conti, S.; Molinari, E. The use of VR in the treatment of eating disorders. Stud. Health Technol Inf. 2004, 99, 121–163. [Google Scholar]
- Porras-Garcia, B.; Ferrer-Garcia, M.; Serrano-Troncoso, E.; Carulla-Roig, M.; Soto-Usera, P.; Miquel-Nabau, H.; Olivares, L.F.D.C.; Marnet-Fiol, R.; Santos-Carrasco, I.L.M.; Borszewski, B.; et al. AN-VR-BR. A randomized controlled trial for reducing fear of gaining weight and other eating disorder symptoms in anorexia nervosa through virtual reality-based body exposure. J. Clin. Med. 2021, 10, 1–23. [Google Scholar] [CrossRef]
- Riva, G.; Bacchetta, M.; Baruffi, M.; Rinaldi, S.; Molinari, E. Experiential cognitive therapy in anorexia nervosa. Eat. Weight Disord 1998, 3, 141–150. [Google Scholar] [CrossRef]
- First, M.B.; Spitzer, R.L.; Gibbon, M.; Williams, J.B. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P); Biometrics Research, New York State Psychiatric Institute: New York, NY, USA, 2002. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- De Zwaan, M. Binge eating disorder and obesity. Int. J. Obes. 2001, 25, S51–S55. [Google Scholar] [CrossRef] [Green Version]
- Kessler, R.C.; Berglund, P.A.; Chiu, W.T.; Deitz, A.C.; Hudson, J.I.; Shahly, V.; Aguilar-Gaxiola, S.; Alonso, J.; Angermeyer, M.C.; Benjet, C. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol. Psychiatry 2013, 73, 904–914. [Google Scholar] [CrossRef] [Green Version]
- Grant, J.E.; Chamberlain, S.R. Neurocognitive findings in young adults with binge eating disorder. Int. J. Psychiatry Clin. Pract. 2020, 24, 71–76. [Google Scholar] [CrossRef]
- Silvestro, S.; Ashley Braun, R. Bulimia Nervosa: Signs and Treatments. Available online: https://ro.co/health-guide/bulimia-nervosa/ (accessed on 7 April 2022).
- Marzola, E.; Nasser, J.A.; Hashim, S.A.; Shih, P.A.B.; Kaye, W.H. Nutritional rehabilitation in anorexia nervosa: Review of the literature and implications for treatment. BMC Psychiatry 2013, 13, 290. [Google Scholar] [CrossRef] [Green Version]
- Van Eeden, A.E.; van Hoeken, D.; Hoek, H.W. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr. Opin. Psychiatry 2021, 34, 515. [Google Scholar] [CrossRef] [PubMed]
- Hudson, J.I.; Hiripi, E.; Pope, H.G.; Kessler, R.C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol. Psychiatry 2007, 61, 348–358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slater, M.; Spanlang, B.; Sanchez-Vives, M.V.; Blanke, O. First Person Experience of Body Transfer in Virtual Reality. PLoS ONE 2010, 5, e10564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maselli, A.; Slater, M. The building blocks of the full body ownership illusion. Front. Hum. Neurosci. 2013, 7, 83. [Google Scholar] [CrossRef] [Green Version]
- Giner-Bartolome, C.; Fagundo, A.B.; Sanchez, I.; Jimenez-Murcia, S.; Santamaria, J.J.; Ladouceur, R.; Menchon, J.M.; Fernandez-Aranda, F. Can an intervention based on a serious videogame prior to cognitive behavioral therapy be helpful in bulimia nervosa? A clinical case study. Front. Psychol. 2015, 6, 982. [Google Scholar] [CrossRef] [Green Version]
- Riva, G. Neuroscience and eating disorders: The allocentric lock hypothesis. Med. Hypotheses 2012, 78, 254–257. [Google Scholar] [CrossRef]
- Riva, G. Out of my real body: Cognitive neuroscience meets eating disorders. Front. Hum. Neurosci. 2014, 8, 236. [Google Scholar] [CrossRef]
- Riva, G. The key to unlocking the virtual body: Virtual reality in the treatment of obesity and eating disorders. J. Diabetes Sci. Technol. 2011, 5, 283–292. [Google Scholar] [CrossRef] [Green Version]
- Atwood, M.E.; Friedman, A. A systematic review of enhanced cognitive behavioral therapy (CBT-E) for eating disorders. Int. J. Eat. Disord. 2020, 53, 311–330. [Google Scholar] [CrossRef]
- Schlundt, D.G.; Johnson, W.G. Eating Disorders: Assessment and Treatment; Allyn & Bacon: Needham Heights, MA, USA, 1990; p. 311. [Google Scholar]
- Butters, J.W.; Cash, T.F. Cognitive-behavioral treatment of women’s body-image dissatisfaction. J. Consult. Clin. Psychol 1987, 55, 889–897. [Google Scholar] [CrossRef]
- Wooley, S.C. Intensive outpatient and residential treatment for bulimia. In Handbook of Psychotherapy for Anorexia Nervosa and Bulimia; Garner, D.M., Garfinkel, P., Eds.; Guilford Press: New York, NY, USA, 1985; pp. 391–430. [Google Scholar]
- Ghaderi, A.; Welch, E.; Zha, C.; Holmes, E.A. Imagery Rescripting for Reducing Body Image Dissatisfaction: A Randomized Controlled Trial. Cogn. Ther. Res. 2022, in press. [Google Scholar] [CrossRef]
- Jansen, A. A learning model of binge eating: Cue reactivity and cue exposure. Behav. Res. 1998, 36, 257–272. [Google Scholar] [CrossRef]
- Boswell, R.G.; Kober, H. Food cue reactivity and craving predict eating and weight gain: A meta-analytic review. Obes Rev. 2016, 17, 159–177. [Google Scholar] [CrossRef]
- García-García, I.; Narberhaus, A.; Marqués-Iturria, I.; Garolera, M.; Rădoi, A.; Segura, B.; Pueyo, R.; Ariza, M.; Jurado, M.A. Neural responses to visual food cues: Insights from functional magnetic resonance imaging. Eur. Eat. Disord. Rev. 2013, 21, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Lyu, Z.; Zheng, P.; Jackson, T. Attention Disengagement Difficulties among Average Weight Women Who Binge Eat. Eur. Eat. Disord. Rev. 2016, 24, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Wolz, I.; Sauvaget, A.; Granero, R.; Mestre-Bach, G.; Baño, M.; Martín-Romera, V.; Veciana de las Heras, M.; Jiménez-Murcia, S.; Jansen, A.; Roefs, A.; et al. Subjective craving and event-related brain response to olfactory and visual chocolate cues in binge-eating and healthy individuals. Sci. Rep. 2017, 7, 41736. [Google Scholar] [CrossRef] [Green Version]
- Craske, M.G.; Treanor, M.; Conway, C.C.; Zbozinek, T.; Vervliet, B. Maximizing exposure therapy: An inhibitory learning approach. Behav. Res. Ther. 2014, 58, 10–23. [Google Scholar] [CrossRef] [Green Version]
- De Carvalho, M.R.; Dias, T.R.D.S.; Duchesne, M.; Nardi, A.E.; Appolinario, J.C. Virtual Reality as a Promising Strategy in the Assessment and Treatment of Bulimia Nervosa and Binge Eating Disorder: A Systematic Review. Behav. Sci. 2017, 7, 43. [Google Scholar] [CrossRef] [Green Version]
- Tomasi, D.; Ferris, H.; Booraem, P.; Enman, L.; Gates, S.; Reyns, E. Olfactory virtual reality (OVR) for wellbeing and reduction of stress, anxiety and pain. J. Med. Res. Health Sci. 2021, 4, 1212–1221. [Google Scholar]
- Wan, A.H.; Wong, D.W.; Ma, C.Z.; Zhang, M.; Lee, W.C. Wearable vibrotactile biofeedback device allowing identification of different floor conditions for lower-limb amputees. Arch. Phys. Med. Rehabil. 2016, 97, 1210–1213. [Google Scholar] [CrossRef] [Green Version]
- Ocampo, R.; Tavakoli, M. Improving user performance in haptics-based rehabilitation exercises by colocation of user’s visual and motor axes via a three-dimensional augmented-reality display. IEEE Robot. Autom. Lett. 2019, 4, 438–444. [Google Scholar] [CrossRef]
- Islam, M.K.; Brunner, I. Cost-analysis of virtual reality training based on the virtual reality for upper extremity in subacute stroke (VIRTUES) trial. Int. J. Technol. Assess. Health Care 2019, 35, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Delshad, S.D.; Almario, C.V.; Fuller, G.; Luong, D.; Spiegel, B.M. Economic analysis of implementing virtual reality therapy for pain among hospitalized patients. NPJ Digit. Med. 2018, 1, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray, S.B.; Loeb, K.L.; Le Grange, D. Dissecting the Core Fear in Anorexia Nervosa: Can We Optimize Treatment Mechanisms? JAMA Psychiatry 2016, 73, 891–892. [Google Scholar] [CrossRef] [PubMed]
- Reilly, E.E.; Anderson, L.M.; Gorrell, S.; Schaumberg, K.; Anderson, D.A. Expanding exposure-based interventions for eating disorders. Int. J. Eat. Disord. 2017, 50, 1137–1141. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, T.; Loeb, K.; Troupe, S.; Delinsky, S. Adjunctive mirror exposure for eating disorders: A randomized controlled pilot study. Behav. Res. Ther. 2012, 50, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Key, A.; George, C.L.; Beattie, D.; Stammers, K.; Lacey, H.; Waller, G. Body image treatment within an inpatient program for anorexia nervosa: The role of mirror exposure in the desensitization process. Int. J. Eat. Disord. 2002, 31, 185–190. [Google Scholar] [CrossRef]
- Jansen, A.; Voorwinde, V.; Hoebink, Y.; Rekkers, M.; Martijn, C.; Mulkens, S. Mirror exposure to increase body satisfaction: Should we guide the focus of attention towards positively or negatively evaluated body parts? J. Behav. Ther. Exp. Psychiatry 2016, 50, 90–96. [Google Scholar] [CrossRef]
- Levinson, C.A.; Rapp, J.; Riley, E.N. Addressing the fear of fat: Extending imaginal exposure therapy for anxiety disorders to anorexia nervosa. Eat. Weight. Disord. Stud. Anorex. Bulim. Obes. 2014, 19, 521–524. [Google Scholar] [CrossRef]
- Waltemate, T.; Gall, D.; Roth, D.; Botsch, M.; Latoschik, M.E. The Impact of Avatar Personalization and Immersion on Virtual Body Ownership, Presence, and Emotional Response. IEEE Trans. Vis. Comput Graph. 2018, 24, 1643–1652. [Google Scholar] [CrossRef]
- Probst, M.; Vandereycken, W.; Coppenolle, H.V.; Vanderlinden, J. The Body Attitude Test for patients with an eating disorder: Psychometric characteristics of a new questionnaire. Eat. Disord. 1995, 3, 133–144. [Google Scholar] [CrossRef]
- Cash, T. The Situational Inventory of Body-Image Dysphoria: Contextual assessment of a negative body image. Behav. Ther. 1994, 17, 133. [Google Scholar]
- Henderson, M.; Freeman, C. A self-rating scale for bulimia the ‘BITE’. Br. J. Psychiatry 1987, 150, 18–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garner, D.M.; Garfinkel, P.E. The Eating Attitudes Test: An index of the symptoms of anorexia nervosa. Psychol. Med. 1979, 9, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Perpiñá, C.; Botella, C.; Baños, R. Virtual reality in eating disorders. Eur. Eat. Disord. Rev. Prof. J. Eat. Disord. Assoc. 2003, 11, 261–278. [Google Scholar] [CrossRef]
- Mantovani, E.; Zucchella, C.; Bottiroli, S.; Federico, A.; Giugno, R.; Sandrini, G.; Chiamulera, C.; Tamburin, S. Telemedicine and Virtual Reality for Cognitive Rehabilitation: A Roadmap for the COVID-19 Pandemic. Front. Neurol. 2020, 11, 926. [Google Scholar] [CrossRef]
- Smits, M.; Staal, J.B.; Van Goor, H. Could Virtual Reality play a role in the rehabilitation after COVID-19 infection? BMJ Open Sport Exerc. Med. 2020, 6, e000943. [Google Scholar] [CrossRef]
- Carter, J.C.; McFarlane, T.L.; Bewell, C.; Olmsted, M.P.; Woodside, D.B.; Kaplan, A.S.; Crosby, R.D. Maintenance treatment for anorexia nervosa: A comparison of cognitive behavior therapy and treatment as usual. Int. J. Eat. Disord. 2009, 42, 202–207. [Google Scholar] [CrossRef]
- Pike, K.M.; Walsh, B.T.; Vitousek, K.; Wilson, G.T.; Bauer, J. Cognitive behavior therapy in the posthospitalization treatment of anorexia nervosa. Am. J. Psychiatry 2003, 160, 2046–2049. [Google Scholar] [CrossRef]
- Dalle Grave, R.; Calugi, S.; Conti, M.; Doll, H.; Fairburn, C.G. Inpatient cognitive behaviour therapy for anorexia nervosa: A randomized controlled trial. Psychother. Psychosom. 2013, 82, 390–398. [Google Scholar] [CrossRef] [Green Version]
- Grange, D.L.; Hughes, E.K.; Court, A.; Yeo, M.; Crosby, R.D.; Sawyer, S.M. Randomized Clinical Trial of Parent-Focused Treatment and Family-Based Treatment for Adolescent Anorexia Nervosa. J. Am. Acad. Child. Adolesc. Psychiatry 2016, 55, 683–692. [Google Scholar] [CrossRef] [PubMed]
- Von Brachel, R.; Hötzel, K.; Hirschfeld, G.; Rieger, E.; Schmidt, U.; Kosfelder, J.; Hechler, T.; Schulte, D.; Vocks, S. Internet-Based Motivation Program for Women with Eating Disorders: Eating Disorder Pathology and Depressive Mood Predict Dropout. J. Med. Internet Res. 2014, 16, e92. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.C.; Jeng, Y.; Wu, W.T.; Wang, T.G.; Han, D.S.; Ozcakar, L.; Chang, K.V. Sarcopenic Dysphagia: A Narrative Review from Diagnosis to Intervention. Nutrients 2021, 13, 4043. [Google Scholar] [CrossRef] [PubMed]
- Westmoreland, P.; Krantz, M.J.; Mehler, P.S. Medical Complications of Anorexia Nervosa and Bulimia. Am. J. Med. 2016, 129, 30–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, A.; Burford, S.; Wyles, C.L.; Mundy, H.; Sainsbury, R. Evaluation of strategies to improve nutrition in people with dementia in an assessment unit. J. Nutr. Health Aging 2008, 12, 309–312. [Google Scholar] [CrossRef] [PubMed]
- Dunne, T.E.; Neargarder, S.A.; Cipolloni, P.B.; Cronin-Golomb, A. Visual contrast enhances food and liquid intake in advanced Alzheimer’s dis’ase. Clin. Nutr. 2004, 23, 533–538. [Google Scholar] [CrossRef] [PubMed]
- Young, K.W.H.; Greenwood, C.E.; van Reekum, R.; Binns, M.A. Providing nutrition supplements to institutionalized seniors with probable Alzheimer’s disease is least beneficial to those with low body weight status. J. Am. Geriatr. Soc. 2004, 52, 1305–1312. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Torres, M.; Planas, M.; Altimir, S.; Pagan, C.; Gonzalez, M.E.; Johnston, S.; Puiggros, C.; Bonada, A.; García-Lorda, P. Effect of oral administration of a whole formula diet on nutritional and cognitive status in patients with Alzheimer’s disease. Clin. Nutr. 2005, 24, 390–397. [Google Scholar] [CrossRef]
- Keller, H.H.; Gibbs, A.J.; Boudreau, L.D.; Goy, R.E.; Pattillo, M.S.; Brown, H.M. Prevention of weight loss in dementia with comprehensive nutritional treatment. J. Am. Geriatr. Soc. 2003, 51, 945–952. [Google Scholar] [CrossRef]
- Perivolaris, A.; Leclerc, C.M.; Wilkinson, K.; Buchanan, S. An Enhanced Dining Program for Persons with Dementia. Alzheimer’s Care Today 2006, 7, 258–267. [Google Scholar]
- Suominen, M.H.; Kivisto, S.M.; Pitkala, K.H. The effects of nutrition education on professionals’ practice and on the nutrition of aged residents in dementia wards. Eur J. Clin. Nutr. 2007, 61, 1226–1232. [Google Scholar] [CrossRef] [PubMed]
- Mamhidir, A.-G.; Karlsson, I.; Norberg, A.; Mona, K. Weight increase in patients with dementia, and alteration in meal routines and meal environment after integrity promoting care. J. Clin. Nurs. 2007, 16, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Clarfield, A.M. The Decreasing Prevalence of Reversible Dementias: An Updated Meta-analysis. Arch. Intern. Med. 2003, 163, 2219–2229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cotman, C.W.; Su, J.H. Mechanisms of Neuronal Death in Alzheimer’s Disease. Brain Pathol. 1996, 6, 493–506. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Sui, Y.; Shen, Y.; Zhu, Y.; Ali, N.; Guo, C.; Wang, T. Effects of Virtual Reality Intervention on Cognition and Motor Function in Older Adults with Mild Cognitive Impairment or Dementia: A Systematic Review and Meta-Analysis. Front. Aging Neurosci. 2021, 13, 586999. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef] [Green Version]
- Menotti, A.; Puddu, P.E. Can we still learn from the seven countries study? Curr. Opin. Lipidol. 2018, 29, 313–317. [Google Scholar] [CrossRef]
- Mumford, D.B. Eating disorders in different cultures. Int. Rev. Psychiatry 1993, 5, 109–114. [Google Scholar] [CrossRef]
- Keel, P.K.; Klump, K.L. Are eating disorders culture-bound syndromes? Implications for conceptualizing their etiology. Psychol. Bull. 2003, 129, 747. [Google Scholar] [CrossRef]
- Bertoli, S.; Spadafranca, A.; Bes-Rastrollo, M.; Martinez-Gonzalez, M.A.; Ponissi, V.; Beggio, V.; Leone, A.; Battezzati, A. Adherence to the Mediterranean diet is inversely related to binge eating disorder in patients seeking a weight loss program. Clin. Nutr. 2015, 34, 107–114. [Google Scholar] [CrossRef]
| Theme | Component |
|---|---|
| Recipients and Providers | Patients Healthcare Providers Researchers VR Designers |
| Virtual Environment | 3D Tacking System Augmented Reality System Cave System Active Video Game Haptic Interface Simulators |
| Applications in Health Care | Physical Rehabilitation Cognitive Training Psychosocial Rehabilitation Surgical Simulation Physical Literacy Development |
| Social Engagement | Accessibility Changing Attitude Cost Cultural Sensitivity Safety Concern |
| Author | Year | Group | Sample Size (M/F) | Age (Mean, SD) | BMI (Mean, SD) | Providers/Trainers |
|---|---|---|---|---|---|---|
| Cesa et al. [30] | 2013 | VR | 0/27 | 32.9, 8.8 | 39.2, 5.3 | Clinical psy. and psy.ther |
| CBT | 0/20 | 29.9, 7.95 | 41.1, 3.3 | |||
| Ctrl | 0/19 | 32.2, 6.36 | 41.8, 6.3 | |||
| Macro et al. [31] | 2013 | SEDT | 0/9 | 21.82, 5.75 | 21.5, 4.28 | Eating disorder therapist & co-therapist |
| SEDTBI (Ctrl) | 0/9 | |||||
| Nameth et al. [32] | 2021 | VR | 1/10 | 40.9, 5.7 | 31.8, 8.1 | Therapist recruited from outpatient university clinic |
| Perpiñá et al. [33] | 1999 | VR | 8 * | 18.38, 2.9 | 21.5, 3.2 | - |
| SBIT (Ctrl) | 5 | 16.6, 1.3 | 22.4, 3 | |||
| Porras-Garcia et al. [34] | 2020 | - | 0/1 | 15 | 18.14 | Health psy. |
| Porras-Garcia et al. [38] | 2021 | VR | 2/14 | 18.25, 1.30 | 17.39, 1.06 | Psy. & co-therapists |
| Ctrl | 2/17 | 19.21, 1.78 | 17.54, 1.27 | |||
| Riva et al. [39] | 1998 | - | 0/1 | 22 | 16.8 | Clinical psy. & psy.ther. |
| Riva et al. [35] | 2000 | BED | 0/25 | Range: 18 to 45 | 41.82, 7.81 | Clinical psy. & psy.ther. |
| Obese | 0/18 | 42.11, 5.43 | ||||
| Riva et al. [36] | 2003 | VR CBT Nutritional | 0/36 | 33.07, 8.08 | 39.80, 6.10 | Clinical psy. & psy.ther. |
| Riva et al. [37] | 2004 | VR | 0/30 | 33.63, 8.29 | 39.59, 6.20 | Clinical psy. & psy.ther. |
| CBT | 0/30 | 32.20, 7.95 | 41.14, 5.70 | |||
| Nutritional | 0/30 | 33.50, 8.17 | 39.95, 6.40 | |||
| No action (Ctrl) | 0/30 | 33.16, 8.25 | 38.59, 6.09 |
| Author | Software | Head-Mounted Display | Controller | Tracker/Sensor |
|---|---|---|---|---|
| Cesa et al. (2013) [30] | Neuro VR open-source software | - | - | - |
| Macro et al. (2013) [31] | WorldUp, Sense8 | V6, Virtual Research | 2D mouse | - |
| Nameth et al. (2021) [32] | Unity, StreamVR | Oculus Rift | Oculus Controllers | Oculus Sensor |
| Perpiñá et al. (1999) [33] | WorldUp, Sense8 | V6, Virtual Research | 2D mouse | - |
| Porras-Garcia et al. (2020) [34] | Unity, Blender | HMD-HTC-VIVE | HMD-HTC-VIVE | HMD FOVE Eye Tracking |
| Porras-Garcia et al. (2021) [38] | Unity, Blender | HMD-HTC-VIVE | - | FOVE VR-HMD Eye Tracking |
| Riva et al. (1998) [39] | VEBIM 2 | Thunder 400/C VR system | ||
| Riva et al. (2000) [35] | VEBIM 2 | Thunder 500/C VR system | Joystick-type input device | - |
| Riva et al. (2003) [36] | VREDIM | - | - | - |
| Riva et al. (2004) [37] | VREDIM | Glasstron | Joystick-type input device | Joystick-type input device |
| Author | Env. Design | Object/Avatar Design | Interaction/Game Design | Training Context |
|---|---|---|---|---|
| Cesa et al. (2013) [30] | 14 env., including Home, supermarket, pub, restaurant, swimming pool, beach, Gym | 2 body images | Practice eating, emotional, relational management, decision-making, problem-solving | Expectation & emotions related to food & weight; Strategies used to cope with difficult interpersonal & potential maintenance situations; Body experience of the subject. |
| Macro et al. (2013) [31] | 5 env. in stage 1 Kitchen in stage 2 Mirror room in stage 3 | Virtual scale in stage 2 Mirror and a 3D avatar in stage 3 | Distinguish and estimate real, subjective, desired, & healthy weight. Manipulate body areas in the avatar | Psychosocial education on body image distortion, consequences of negative body image, exaggeration in media, cultural factors for body dissatisfaction |
| Nameth et al. (2021) [32] | 4 env., including kitchen, dining room, bedroom, restaurant | 30 common binge foods | Access eliciting craving & anxiety about losing control overeating on food & environment | Changing physical state of body; Increase behavioral alternative to eating; Changing the attentional Focus;Enhancing motivation to resist cues. |
| Perpiñá et al. (1999) [33] | Food area, Exhibition room Mirror room | Virtual scale Posters with different body builds 3D avatar | Estimate body weight after eating a virtual food. Manipulate body areas in the avatar | Education, exposure & cognitive discussion; Learn to correct estimate weight after eating; understand weight as a relative concept |
| Porras-Garcia et al. (2020) [34] | Simple room w/large mirror on the front wall | - | Asked to observe & focus different part of her virtual body in the mirror | The Virtual body start with the same BMI of the patient and change with progressive increase of BMI until targeted healthy BMI |
| Porras-Garcia et al. (2021) [38] | Unique room w/o furniture except a large mirror | - | Exposed a silhouette to patients. The patients orally report their throughs & feeling about most of the body parts of their virtual body | Patient exposed to their real silhouette, & processingly increased the BMI of silhouette until a healthy BMI |
| Riva et al. (1998) [39] | Different rooms of a virtual office | Virtual weighing machine; 7 avatars from underweight to overweight; Panels of model pictures. | Different questions (hypothetical, inverse, & third-person ones) to help patients synthesize information & reach conclusions on their own. | Access & modify patients’ symptoms of anxiety related to food exposure & their body experience |
| Riva et al. (2000) [35] | Kitchen, closet, bedroom; 4 working env.; Room w/5 doors of different dimensions | Virtual weighing machine; 7 avatars from underweight to overweight; Panels of model pictures; Large mirror showing patients’ real body. | Different questions (hypothetical, inverse, & third-person ones) to help patients synthesize information & reach conclusions on their own. | Access & modify patients’ symptoms of anxiety related to food exposure & their body experience |
| Riva et al. (2003) [36] | - | - | Different questions (hypothetical, inverse, & third-person ones) to help patients synthesize information & reach conclusions on their own. | Access & modify patients’ symptoms of anxiety related to food exposure & their body experience |
| Riva et al. (2004) [37] | 14 virtual env. including kitchen, bathroom, bedroom, 9 doors room, Shopping mall, Swimming pool & beach) | Body Image VR Scale (BIVRS) | Different questions (hypothetical, inverse, & third-person ones) to help patients synthesize information & reach conclusions on their own. | Access & modify patients’ symptoms of anxiety related to food exposure & their body experience |
| Author | Disorder | VR Therapy | Study Design | Protocol |
|---|---|---|---|---|
| Cesa et al. (2013) [30] | BED | ECT | RCT | VR: 1 × Inpatient program; 5 × group sessions, 1 per week; 10 × 1-h VR sessions, 2 per week. CBT: 1 × Inpatient program; 5 × group sessions, 1 per week; 10 × CBT sessions, 2 per week. Control: Inpatient program |
| Macro et al. (2013) [31] | AN, BN, EDNOS | ECT + BET | RCT | 15 ECT sessions & 8 individual psychotherapy sessions |
| Nameth et al. (2021) [32] | BED, BN | CET | CS | 8 × 1-h session, 1 per week |
| Perpiñá et al. (1999) [33] | AN, BN | BET | RCT | 6 × 1-h session, 1 per week |
| Porras-Garcia et al. (2020) [34] | BED, BN | BET | CR | 5 × 1-h session, 1 per week |
| Porras-Garcia et al. (2021) [38] | Restrictive AN | BET | RCT | 5 × 45-min session, 1 per week |
| Riva et al. (1998) [39] | AN | ECT | CR | Individual psy. talks for a month, 1 a week; Group sessions, 2 per week; 5 × VR session. |
| Riva et al. (2000) [35] | BED | ECT | CS | Individual work: Psychometric tests; Weekly supportive psy. talks; 5 × VR sessions. Group work: Psycho-nutritional groups held by nutritionists, 2 per week (for patients eat 1200 kcal per day) |
| Riva et al. (2003) [36] | BED | ECT | RCT | 5 × group sessions aimed at improving assertiveness & motivation to change, 1 per week; 10 × VR sessions, 2 per week. |
| Riva et al. (2004) [37] | BED, Obese, BN, EDNOS | ECT | RCT | 5 × group psy. sessions; 10 × individual VR sessions w/psy. (ECT); 1 × individual diet session. 4 or 6 × group diet sessions;Physical activity |
| Author | Evaluation Timepoint | Endpoint | Instruments | Treatment Findings |
|---|---|---|---|---|
| Cesa et al. (2013) [30] | Bf-Aft, 1-year FU | Binge Eating Epi. | EDI BSS BIAQ Weight No. of epi. | CBT + VR: - Only effective on weight loss at 1 year. Recurrence: - Occurs in all groups 1-year FU; - Maintains a low rate in VR & CBT. |
| Macro et al. (2013) [31] | Bf-Aft, 1-year FU | Body Image | BAT, BIATQ, BASS, SIBID, BITE, EAT | SEDTBI: ↑ BAT, BIATQ, BASS, SIBID after treatment and follow-up; and better than SEDT group but not significant. |
| Nameth et al. (2021) [32] | Bf-Aft | Preliminary Signal of Effectiveness | OBE SBE | ↓ Binge epi. (Perceived & Referenced) |
| Perpiñá et al. (1999) [33] | Bf-Aft | General Psychopathology Measures General Eating Disorder Measures Body Image | BDI, PANAS; EAT, RS, BITE, EDI; BSQ, BIAQ, BAT, BES, BIATQ, ASI, SIBID, BASS, Body Inference, Fear of putting weight | For both groups: ↑ BDI, PANAS, SIBID, BIAQ, BIATQ, BSQ ↓ Fear of putting weight For VR group ↓ Fear of putting weight, ↑ Accuracy in estimating their body weight, closer desired weight to healthy weight; compared to control |
| Porras-Garcia et al. (2020) [34] | Bf-Aft, 5 months FU | Symptomatology Body Anxiety Body Image Disturbance FBI FGW | BMI EDI PASTAS TSA Body-Related Attentional Bias VAS | After treatment: - ↓ Body anxiety, FGB, VAS; - ↓ Levels of body anxiety & FGW (VAS); - ↑ Patient’s BMI; - ↓ Body dissat., PASTAS, TSA, Complete fixation time & No. of fixations. 5 months FU: - BMI slightly increased; - Body dissat., body image distortion & body anxiety slightly reduced; - ↑ FGW (VAS). |
| Porras-Garcia et al. (2021) [38] | Bf-Aft, 3 months FU | FBI, FGW Anxiety Level | VAS | ↑ FBI, ↓ FGW |
| Body Anxiety Attentional Bias | PASTAS | ↓ Attentional Bias | ||
| Riva et al. (1998) [39] | Bf-Aft | Body dissat. | BSS CDRS FRS | ↓ BSS, CDRS, FRS |
| Avoidance behav. Grooming habits associated with negative body image | BIAQs | ↓ Avoidance behav. & grooming habits associated with negative body image | ||
| Riva et al. (2000) [35] | Bf-Aft | Body dissat. | BSS CDRS FRS | BED group: - ↓ Body dissat. (BSS, FRS, CDRS). Obese group: - ↓ Body dissat., better representation of their members. |
| Social activities Concealing behav. | BIAQs | Both group: - ↑ Social activities; - ↓ Concealing behav. | ||
| Riva et al. (2003) [36] | Bf-Aft, 6 months FU | Anxiety Depressive mood Body Image | STAI BDI EDI 2 BSS CDRS FRS | After treatment: - ↓ Anxiety (STAI) in VR & dietetic groups; - ↓ Depressive mood (BDI) in VR & CBT; - VR amended depressive symptoms; - ↑ BSS, BIAQ, CDRS (VR more effective). 6 months FU: - VR had better efficacy on EDI2, BSS, BIAQ, CDRS. |
| Eating control | DIET WELSQ | After treatment: - ↑ DIET, WELSQ except control; - Best results in VR. | ||
| Weight | Weight | After treatment: - ↓ Weight except control. 6 months FU: - ⊗ Weight loss. | ||
| Self-esteem Social skills | RSEQ RAS | ↑ RAS in VR; ↑ DIET, except control; Best results in VR. | ||
| Riva et al. (2004) [37] | Bf-Aft | Anxiety Depressive mood Body Image | STAI BDI BSS CDRS FRS | Both BED & obese patients: - ↓ STAI in VR & dietetic; - ↓ BDI in VR & CBT; - VR amended depressive symptoms; - ↑ BSS, BIAQ, CDRS more effective in VR. |
| Eating control | DIET WELSQ | Both BED & obese patients: - ↑ DIET, WELSQ except control; - Best results in VR. | ||
| Weight | Weight | Both BED & obese patients: - ↓ Weight except control | ||
| Self-esteem Social skills | RSEQ RAS | Both BED & obese patients: - ↑ RSEQ except control; - ↑ RAS in VR. |
| Author | Construct | Instrument | Finding |
|---|---|---|---|
| Cesa et al. (2013) [30] | Acceptability | Nonrespondent rate | Medium to High (33.4%) |
| Macro et al. (2013) [31] | - | - | - |
| Nameth et al. (2021) [32] | Feasibility | No. of therapist attended training after information session & enrolled after the training session; % of participant enrolled; Attendance; % completion; % completed questionnaires by patients & therapists. | High attend & complete rate for both patients & therapists. |
| Acceptability | SSQ PQ CSQ-R | SSQ, PQ & CSQ-R indicated general acceptance | |
| Perpiñá et al. (1999) [33] | Acceptability | Patient Feedback | VR system provided an objective judgement that was less resisted by patients. They accepted that they had a body distortion belief |
| Attribute | Interview and Patient Feedback | All patients reported 7 to 9 points out of ten for the realism of VR. They felt the stress when ate virtually | |
| Porras-Garcia et al. (2020) [34] | Attribute | Patient Feedback | Motivated, Helpful, Entertaining, Progressively more relaxing Not look realistic enough, clothes look bland, prefer no swimming cap |
| Porras-Garcia et al. (2021) [38] | Acceptability | Drop-out rates Patient Feedback Author Comment | Low drop-out rates cannot simulate important feature of general appearance Virtual body seemed too young |
| Riva et al. (1998) [39] | Affordability | Cost | About $12,000 High |
| Riva et al. (2000) [35] | Safety | Side effects Simulation sickness | Comment that VR had minimum side effects or simulation sickness was found |
| Riva et al. (2003) [36] | - | - | - |
| Riva et al. (2004) [37] | Safety | Side effects Simulation sickness | Comment that VR had minimum side effects or simulation sickness was found |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
So, B.P.-H.; Lai, D.K.-H.; Cheung, D.S.-K.; Lam, W.-K.; Cheung, J.C.-W.; Wong, D.W.-C. Virtual Reality-Based Immersive Rehabilitation for Cognitive- and Behavioral-Impairment-Related Eating Disorders: A VREHAB Framework Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 5821. https://doi.org/10.3390/ijerph19105821
So BP-H, Lai DK-H, Cheung DS-K, Lam W-K, Cheung JC-W, Wong DW-C. Virtual Reality-Based Immersive Rehabilitation for Cognitive- and Behavioral-Impairment-Related Eating Disorders: A VREHAB Framework Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(10):5821. https://doi.org/10.3390/ijerph19105821
Chicago/Turabian StyleSo, Bryan Pak-Hei, Derek Ka-Hei Lai, Daphne Sze-Ki Cheung, Wing-Kai Lam, James Chung-Wai Cheung, and Duo Wai-Chi Wong. 2022. "Virtual Reality-Based Immersive Rehabilitation for Cognitive- and Behavioral-Impairment-Related Eating Disorders: A VREHAB Framework Scoping Review" International Journal of Environmental Research and Public Health 19, no. 10: 5821. https://doi.org/10.3390/ijerph19105821
APA StyleSo, B. P. -H., Lai, D. K. -H., Cheung, D. S. -K., Lam, W. -K., Cheung, J. C. -W., & Wong, D. W. -C. (2022). Virtual Reality-Based Immersive Rehabilitation for Cognitive- and Behavioral-Impairment-Related Eating Disorders: A VREHAB Framework Scoping Review. International Journal of Environmental Research and Public Health, 19(10), 5821. https://doi.org/10.3390/ijerph19105821








