A Multi-Level Analysis of Individual and Neighborhood Factors Associated with Patient Portal Use among Adult Emergency Department Patients with Multimorbidity
Abstract
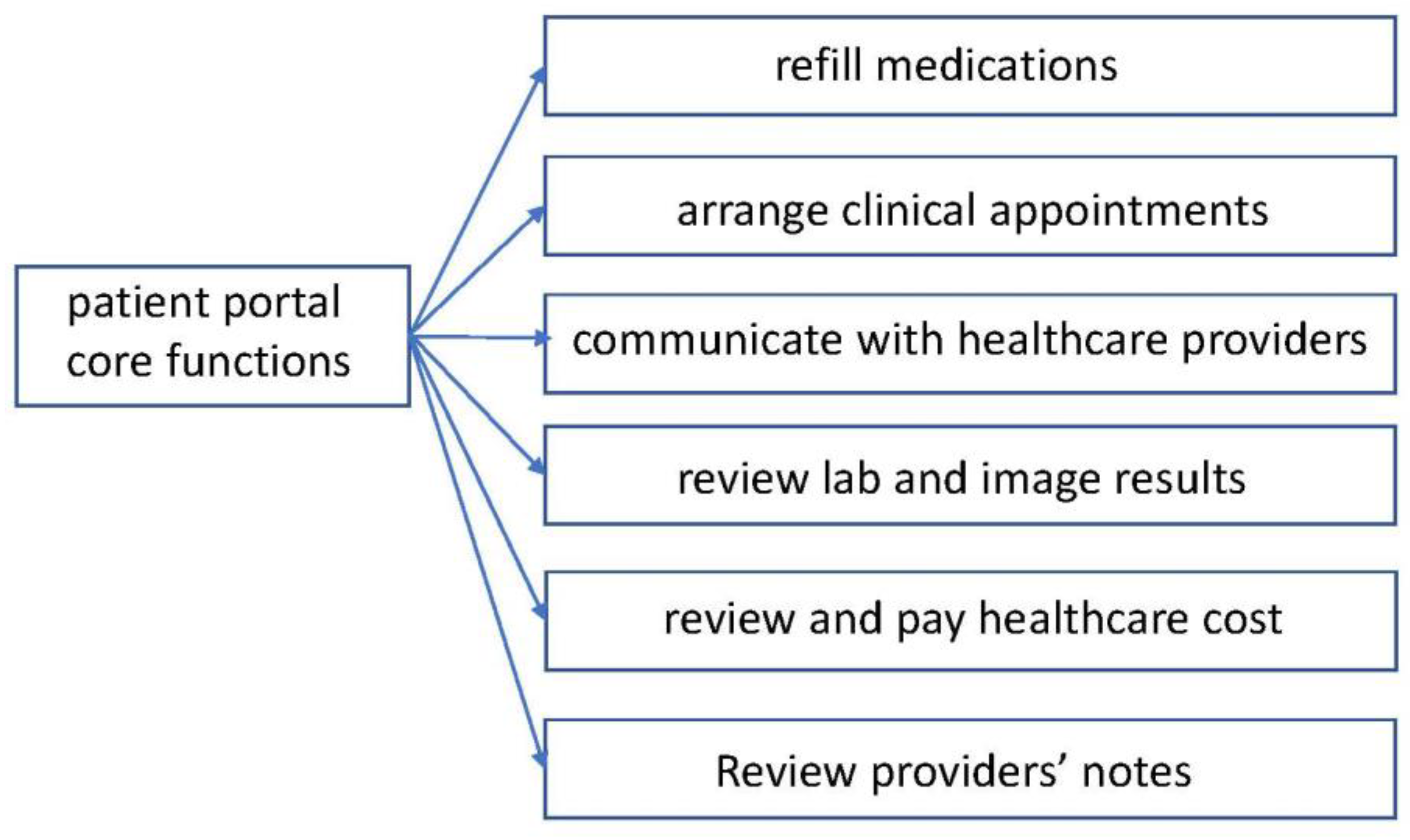
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Data Source
2.3. Study Population
2.4. Inclusion and Exclusion Criteria
2.5. Measures
2.6. Statistical Analyses
2.7. Reporting Guideline
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
Appendix A
References
- Tapuria, A.; Porat, T.; Kalra, D.; Dsouza, G.; Xiaohui, S.; Curcin, V. Impact of patient access to their electronic health record: Systematic review. Inform. Health Soc. Care 2021, 46, 192–204. [Google Scholar] [CrossRef] [PubMed]
- Assiri, G. The Impact of Patient Access to Their Electronic Health Record on Medication Management Safety: A Narrative Review. Saudi Pharm. J. 2022, 30, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Alturkistani, A.; Qavi, A.; Anyanwu, P.E.; Greenfield, G.; Greaves, F.; Costelloe, C. Patient Portal Functionalities and Patient Outcomes Among Patients with Diabetes: Systematic Review. J. Med. Internet Res. 2020, 22, e18976. [Google Scholar] [CrossRef] [PubMed]
- Apter, A.J.; Bryant-Stephens, T.; Perez, L.; Morales, K.H.; Howell, J.T.; Mullen, A.N.; Han, X.; Canales, M.; Rogers, M.; Klusaritz, H.; et al. Patient Portal Usage and Outcomes Among Adult Patients with Uncontrolled Asthma. J. Allergy Clin. Immunol. Pract 2020, 8, 965–970. [Google Scholar] [CrossRef] [PubMed]
- Fareed, N.; MacEwan, S.R.; Vink, S.; Jonnalagadda, P.; McAlearney, A.S. Relationships between patient portal activation and patient satisfaction scores among CG-CAHPS and HCAHPS respondents. Am. J. Manag. Care 2022, 28, 25–31. [Google Scholar]
- Campanella, P.; Lovato, E.; Marone, C.; Fallacara, L.; Mancuso, A.; Ricciardi, W.; Specchia, M.L. The impact of electronic health records on healthcare quality: A systematic review and meta-analysis. Eur. J. Public Health 2016, 26, 60–64. [Google Scholar] [CrossRef] [Green Version]
- Sorondo, B.; Allen, A.; Fathima, S.; Bayleran, J.; Sabbagh, I. Patient Portal as a Tool for Enhancing Patient Experience and Improving Quality of Care in Primary Care Practices. EGEMS 2016, 4, 1262. [Google Scholar] [CrossRef] [Green Version]
- Sieck, C.J.; Hefner, J.L.; McAlearney, A.S. Improving the patient experience through patient portals: Insights from experienced portal users. Patient Exp. J. 2018, 5, 47–54. [Google Scholar] [CrossRef]
- Sun, R.; Burke, L.E.; Korytkowski, M.T.; Saul, M.I.; Li, D.; Sereika, S.M. A longitudinal examination of patient portal use on glycemic control among patients with uncontrolled type 2 diabetes. Diabetes Res. Clin. Pract. 2020, 170, 108483. [Google Scholar] [CrossRef]
- Antonio, M.G.; Petrovskaya, O.; Lau, F. The State of Evidence in Patient Portals: Umbrella Review. J. Med. Internet Res. 2020, 22, e23851. [Google Scholar] [CrossRef]
- Apathy, N.C.; Holmgren, A.J.; Adler-Milstein, J. A decade post-HITECH: Critical access hospitals have electronic health records but struggle to keep up with other advanced functions. J. Am. Med. Inform. Assoc. 2021, 28, 1947–1954. [Google Scholar] [CrossRef] [PubMed]
- Wedd, J.; Basu, M.; Curtis, L.M.; Smith, K.; Lo, D.J.; Serper, M.; Wolf, M.S.; Parker, R.; Patzer, R.E. Racial, Ethnic, and Socioeconomic Disparities in Web-Based Patient Portal Usage Among Kidney and Liver Transplant Recipients: Cross-Sectional Study. J. Med. Internet Res. 2019, 21, e11864. [Google Scholar] [CrossRef]
- Clarke, M.A.; Lyden, E.R.; Ma, J.; King, K.M.; Siahpush, M.; Michaud, T.; Idoate, R.E.; Ramos, A.K. Sociodemographic Differences and Factors Affecting Patient Portal Utilization. J. Racial Ethn. Health Disparities 2021, 8, 879–891. [Google Scholar] [CrossRef]
- Sarkar, U.; Karter, A.J.; Liu, J.Y.; Adler, N.E.; Nguyen, R.; López, A.; Schillinger, D. Social disparities in internet patient portal use in diabetes: Evidence that the digital divide extends beyond access. J. Am. Med. Inform. Assoc. 2011, 18, 318–321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goel, M.S.; Brown, T.L.; Williams, A.; Hasnain-Wynia, R.; Thompson, J.A.; Baker, D.W. Disparities in enrollment and use of an electronic patient portal. J. Gen. Intern. Med. 2011, 26, 1112–1116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garrido, T.; Kanter, M.; Meng, D.; Turley, M.; Wang, J.; Sue, V.; Scott, L. Race/ethnicity, personal health record access, and quality of care. Am. J. Manag. Care 2015, 21, e103–e113. [Google Scholar]
- Hagglund, M.; Blease, C.; Scandurra, I. Mobile Access and Adoption of the Swedish National Patient Portal. Stud. Health Technol. Inform. 2020, 275, 82–86. [Google Scholar] [PubMed]
- Wang, H.; Manning, S.E.; Ho, A.F.; Sambamoorthi, U. Factors Associated with Reducing Disparities in Electronic Personal Heath Records Use Among Non-Hispanic White and Hispanic Adults. J. Racial Ethn. Health Disparities 2022. [Google Scholar] [CrossRef]
- Localio, A.M.; Klusaritz, H.; Morales, K.H.; Ruggieri, D.G.; Han, X.; Apter, A.J. Primary language and the electronic health record patient portal: Barriers to use among Spanish-speaking adults with asthma. J. Asthma 2021, 59, 2081–2090. [Google Scholar] [CrossRef]
- Powell, K.R. Patient-Perceived Facilitators of and Barriers to Electronic Portal Use: A Systematic Review. Comput. Inform. Nurs. 2017, 35, 565–573. [Google Scholar] [CrossRef]
- El-Toukhy, S.; Mendez, A.; Collins, S.; Perez-Stable, E.J. Barriers to Patient Portal Access and Use: Evidence from the Health Information National Trends Survey. J. Am. Board Fam. Med. 2020, 33, 953–968. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.Y.; Song, B.; Anand, E.; Schwartz, D.; Panesar, M.; Jackson, G.P.; Elkin, P.L. Barriers, Facilitators, and Solutions to Optimal Patient Portal and Personal Health Record Use: A Systematic Review of the Literature. AMIA Annu. Symp. Proc. 2017, 2017, 1913–1922. [Google Scholar]
- From a National Survey and Policy Implications. Am. J. Health Promot. 2020, 34, 677–680.
- Crouch, E.; Gordon, N.P. Prevalence and Factors Influencing Use of Internet and Electronic Health Resources by Middle-Aged and Older Adults in a US Health Plan Population: Cross-Sectional Survey Study. JMIR Aging 2019, 2, e11451. [Google Scholar] [CrossRef]
- Schultz, C.L.; McCahan, S.M.; Lewis, A.M.; Bunnell, H.T.; Alderfer, M.A. Online patient portal use by caregivers in pediatric oncology: Are we widening sociodemographic disparities? Pediatr Blood Cancer 2021, 68, e29373. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.A.; Volkman, J.E.; Leveille, S.G.; Amante, D.J. Predictors of Online Patient Portal Use Among a Diverse Sample of Emerging Adults: Cross-sectional Survey. JMIR Form. Res. 2022, 6, e33356. [Google Scholar] [CrossRef] [PubMed]
- Gordon, W.J.; Bates, D.W.; Fuchs, D.; Pappas, J.; Silacci, S.; Landman, A. Comparing Characteristics of Patients Who Connect Their iPhones to an Electronic Health Records System Versus Patients Who Connect Without Personal Devices: Cohort Study. J. Med. Internet Res. 2019, 21, e14871. [Google Scholar] [CrossRef]
- Balthazar, P.; Narayan, A.K.; Reid, N.; Miles, R.; Flores, E. Effect of Sociodemographic Factors on Utilization of an Online Patient Portal to Self-Schedule Screening Mammography: A Cross-Sectional Study. J. Am. Coll. Radiol. 2022, 19, 866–873. [Google Scholar] [CrossRef] [PubMed]
- Riippa, I.; Linna, M.; Ronkko, I. The effect of a patient portal with electronic messaging on patient activation among chronically ill patients: Controlled before-and-after study. J. Med. Internet Res. 2014, 16, e257. [Google Scholar] [CrossRef] [Green Version]
- Goldzweig, C.L.; Orshansky, G.; Paige, N.M.; Towfigh, A.A.; Haggstrom, D.A.; Miake-Lye, I.; Beroes, J.M.; Shekelle, P.G. Electronic patient portals: Evidence on health outcomes, satisfaction, efficiency, and attitudes: A systematic review. Ann. Intern. Med. 2013, 159, 677–687. [Google Scholar] [CrossRef]
- Liu, S.K.; Osborn, A.E.; Bell, S.; Mecchella, J.N.; Hort, S.; Batsis, J.A. Patient characteristics and utilization of an online patient portal in a rural academic general internal medicine practice. BMC Med. Inform. Decis. Mak. 2022, 22, 42. [Google Scholar] [CrossRef]
- Wang, H.; Ho, A.F.; Wiener, R.C.; Sambamoorthi, U. The Association of Mobile Health Applications with Self-Management Behaviors among Adults with Chronic Conditions in the United States. Int. J. Environ. Res. Public Health 2021, 18, 10351. [Google Scholar] [CrossRef]
- Jackson, B.M.; Gutierrez, M.L.; Relyea, G.E.; Carlton, E.L.; Ahn, S.; Binkley, B.L.; Bailey, J.E. Unmet primary care needs in diabetic patients with multimorbidity in a medically underserved area. Health Serv. Res. Manag. Epidemiol. 2017, 4, 2333392817702760. [Google Scholar] [CrossRef]
- Alhussain, K.; Meraya, A.M.; Sambamoorthi, U. Serious psychological distress and emergency room use among adults with multimorbidity in the United States. Psychiatry J. 2017, 2017, 8565186. [Google Scholar] [CrossRef]
- McCusker, J.; Karp, I.; Cardin, S.; Durand, P.; Morin, J. Determinants of emergency department visits by older adults: A systematic review. Acad. Emerg. Med. 2003, 10, 1362–1370. [Google Scholar] [CrossRef]
- Goodman, R.A.; Posner, S.F.; Huang, E.S.; Parekh, A.K.; Koh, H.K. Defining and measuring chronic conditions: Imperatives for research, policy, program, and practice. Prev. Chronic Dis. 2013, 10, E66. [Google Scholar] [CrossRef] [Green Version]
- Mass, C.J.M.; Hox, J.J. Sufficient sample sizes for multilevel modeling. Methodology 2005, 1, 86–92. [Google Scholar] [CrossRef] [Green Version]
- Liang, Z.; Nau, C.; Xie, F.; Vogel, R.; Chen, W. The Application of Community-Based Information from the American Community Survey in a Large Integrated Health Care Organization. Perm J. 2020, 25, 1–3. [Google Scholar] [CrossRef]
- Forthman, K.L.; Colaizzi, J.M.; Yeh, H.W.; Kuplicki, R.; Paulus, M.P. Latent Variables Quantifying Neighborhood Characteristics and Their Associations with Poor Mental Health. Int. J. Environ. Res. Public Health 2021, 18, 1202. [Google Scholar] [CrossRef]
- Austin, P.C.; Wagner, P.; Merlo, J. The median hazard ratio: A useful measure of variance and general contextual effects in multilevel survival analysis. Stat. Med. 2017, 36, 928–938. [Google Scholar] [CrossRef]
- Austin, P.C.; Merlo, J. Intermediate and advanced topics in multilevel logistic regression analysis. Stat. Med. 2017, 36, 3257–3277. [Google Scholar] [CrossRef] [Green Version]
- Merlo, J.; Wagner, P.; Ghith, N.; Leckie, G. An Original Stepwise Multilevel Logistic Regression Analysis of Discriminatory Accuracy: The Case of Neighbourhoods and Health. PLoS ONE 2016, 11, e0153778. [Google Scholar] [CrossRef] [Green Version]
- Merlo, J.; Chaix, B.; Ohlsson, H.; Beckman, A.; Johnell, K.; Hjerpe, P.; Råstam, L.; Larsen, K. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J. Epidemiol. Community Health 2006, 60, 290–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Epidemiology 2007, 18, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Reed, M.E.; Huang, J.; Brand, R.J.; Neugebauer, R.; Graetz, I.; Hsu, J.; Ballard, D.W.; Grant, R. Patients with complex chronic conditions: Health care use and clinical events associated with access to a patient portal. PLoS ONE 2019, 14, e0217636. [Google Scholar] [CrossRef] [Green Version]
- Manard, W.; Scherrer, J.F.; Salas, J.; Schneider, F.D. Patient Portal Use and Blood Pressure Control in Newly Diagnosed Hypertension. J. Am. Board Fam. Med. 2016, 29, 452–459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weppner, W.G.; Ralston, J.D.; Koepsell, T.D.; Grothaus, L.C.; Reid, R.J.; Jordan, L.; Larson, E.B. Use of a shared medical record with secure messaging by older patients with diabetes. Diabetes Care 2010, 33, 2314–2319. [Google Scholar] [CrossRef] [Green Version]
- Anthony, D.L.; Campos-Castillo, C.; Lim, P.S. Who Isn’t Using Patient Portals and Why? Evidence and Implications from a National Sample OF US Adults. Health Aff 2018, 37, 1948–1954. [Google Scholar] [CrossRef] [PubMed]
- Shimada, S.L.; Allison, J.J.; Rosen, A.K.; Feng, H.; Houston, T.K. Sustained Use of Patient Portal Features and Improvements in Diabetes Physiological Measures. J. Med. Internet Res. 2016, 18, e179. [Google Scholar] [CrossRef]
- LeLaurin, J.H.; Nguyen, O.T.; Thompson, L.A.; Hall, J.; Bian, J.; Cho, H.D.; Acharya, R.; Harle, C.A.; Salloum, R.G. Disparities in Pediatric Patient Portal Activation and Feature Use. JAMIA Open 2021, 4, ooab086. [Google Scholar] [CrossRef]
- Kim, H.S.; Kim, H.J.; Juon, H.S. Racial/Ethnic Disparities in Patient-Provider Communication and the Role of E-Health Use. J. Health Commun. 2021, 26, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Schofield, E.; Hay, J.L.; Waters, E.A.; Kiviniemi, M.T.; Orom, H. Race/Ethnicity, Nativity Status, and Patient Portal Access and Use. J. Health Care Poor Underserved 2021, 32, 700–711. [Google Scholar] [CrossRef]
- Moqbel, M.; Hewitt, B.; Nah, F.F.; McLean, R.M. Sustaining Patient Portal Continuous Use Intention and Enhancing Deep Structure Usage: Cognitive Dissonance Effects of Health Professional Encouragement and Security Concerns. Inf. Syst. Front. 2021, 24, 1483–1496. [Google Scholar] [CrossRef]
- Perzynski, A.T.; Roach, M.J.; Shick, S.; Callahan, B.; Gunzler, D.; Cebul, R.; Kaelber, D.C.; Huml, A.; Thornton, J.D.; Einstadter, D. Patient portals and broadband internet inequality. J. Am. Med. Inform. Assoc. 2017, 24, 927–932. [Google Scholar] [CrossRef]
- Moiduddin, A.; Moore, J. The Underserved and Health Information Technology: Issues and Opportunities. Available online: https://aspe.hhs.gov/sites/default/files/migrated_legacy_files//101521/report.pdf (accessed on 30 December 2022).

| Number | Percentage | ||
|---|---|---|---|
| Sex | |||
| Female | 20,234 | 49.9 | |
| Male | 20,310 | 50.1 | |
| Race, Ethnicity, and Preferred Language | |||
| Non-Hispanic White and English | 14,385 | 35.5 | |
| Non-Hispanic Black and English | 13,609 | 33.6 | |
| Latino/Hispanic and English | 6011 | 14.8 | |
| Latino/Hispanic and Spanish | 4603 | 11.4 | |
| Other race and English | 1084 | 2.7 | |
| Other race and Other language | 852 | 2.1 | |
| Age Groups | |||
| 18–34 years | 6619 | 16.3 | |
| 35–49 years | 10,183 | 25.1 | |
| 50–64 years | 16,416 | 40.5 | |
| 65–74 years | 5046 | 12.5 | |
| 75 years+ | 2280 | 5.6 | |
| Marital Status | |||
| Single | 19,163 | 47.3 | |
| Married | 10,185 | 25.1 | |
| Divorced | 5432 | 13.4 | |
| Other | 5764 | 14.2 | |
| PCP Visit | |||
| Yes | 28,046 | 69.2 | |
| No | 12,498 | 30.8 | |
| Health Insurance | |||
| Yes | 30,165 | 74.4 | |
| No | 10,379 | 25.6 | |
| Mean | STD | Median | Min | Max | IQR | |
|---|---|---|---|---|---|---|
| Unemployment | 5.6 | 1.4 | 5.5 | 1.5 | 9.2 | [4.7–6.9] |
| Median family income in US $ | 63,390 | 22,304 | 60,284 | 36,300 | 177,393 | [43,042–80,040] |
| Below poverty level | 18.3 | 8.7 | 18.7 | 2.7 | 33.9 | [10.6–25.8] |
| Hispanic residents | 38.5 | 19.7 | 36.3 | 4.0 | 93.9 | [23.7–47.8] |
| Residents reporting two or more races | 2.7 | 1.0 | 2.6 | 0.6 | 5.4 | [2.0–3.6] |
| People speaking other languages | 36.3 | 18.0 | 30 | 6.3 | 81.6 | [21.4–46.2] |
| Bachelor or higher degrees | 22.6 | 13.3 | 20.6 | 4.2 | 72.3 | [12.0–31.9] |
| No health insurance | 21.9 | 8.3 | 22.3 | 3.0 | 41.0 | [14.9–28.1] |
| Married couples | 43.7 | 11.4 | 42.2 | 24.8 | 77.8 | [34.3–51.6] |
| Access to Internet | 79.1 | 11.1 | 81.2 | 56.8 | 98.8 | [68.8–87.1] |
| Non-US citizen | 66.0 | 14.4 | 71.6 | 24.3 | 81.5 | [54.0–77.0] |
| No vehicle in family | 6.6 | 3.7 | 6.8 | 0.4 | 14.4 | [3.4–9.3] |
| Patient Portal Users | Non-Users | ||||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | Chi2 Value | p-Value | ||
| Patient-Level Characteristics | |||||||
| ALL | 7757 | 19.1 | 32,787 | 80.9 | |||
| Sex | 712.1 | <0.001 | |||||
| Female | 4928 | 24.4 | 15,306 | 75.6 | |||
| Male | 2829 | 13.9 | 17,481 | 86.1 | |||
| Race, Ethnicity, and Preferred Language | 468.9 | <0.001 | |||||
| Non-Hispanic White and English | 3191 | 22.2 | 11,194 | 77.8 | |||
| Non-Hispanic African American and English | 2121 | 15.6 | 11,488 | 84.4 | |||
| Latino/Hispanic and English | 1258 | 20.9 | 4753 | 79.1 | |||
| Latino/Hispanic and Spanish | 605 | 13.1 | 3998 | 86.9 | |||
| Other race and English | 311 | 28.7 | 773 | 71.3 | |||
| Other race and Other language | 271 | 31.8 | 581 | 68.2 | |||
| Age Groups | 183.9 | <0.001 | |||||
| 18–34 years | 971 | 14.7 | 5648 | 85.3 | |||
| 35–49 years | 2085 | 20.5 | 8098 | 79.5 | |||
| 50–64 years | 3462 | 21.1 | 12,954 | 78.9 | |||
| 65–74 years | 928 | 18.4 | 4118 | 81.6 | |||
| 75 years or older | 311 | 13.6 | 1969 | 86.4 | |||
| Marital Status | 326.1 | <0.001 | |||||
| Single | 2975 | 15.5 | 16,188 | 84.5 | |||
| Married | 2346 | 23.0 | 7839 | 77.0 | |||
| Divorced | 1262 | 23.2 | 4170 | 76.8 | |||
| Other | 1174 | 20.4 | 4590 | 79.6 | |||
| PCP | >2400 | <0.001 | |||||
| Yes | 7158 | 25.5 | 20,888 | 74.5 | |||
| No | 599 | 4.8 | 11,899 | 95.2 | |||
| Health Insurance | 977.6 | <0.001 | |||||
| Yes | 6852 | 22.7 | 23,313 | 77.3 | |||
| No | 905 | 8.7 | 9474 | 91.3 | |||
| Community-Level Characteristics | |||||||
| Mean | SE | Mean | SE | t-Value | p-Value | ||
| Married couple (%) | 45.90 | 0.13 | 43.16 | 0.06 | 19.10 | <0.001 | |
| None US citizen (%) | 62.39 | 0.17 | 66.87 | 0.08 | 24.89 | <0.001 | |
| Unemployment (%) | 5.36 | 0.02 | 5.67 | 0.01 | 18.63 | <0.001 | |
| Median family income ($) | 67,468.99 | 260.19 | 62,425.30 | 121.76 | 17.98 | <0.001 | |
| No insurance (%) | 20.22 | 0.09 | 22.24 | 0.05 | 19.43 | <0.001 | |
| Below poverty level (%) | 16.15 | 0.09 | 18.84 | 0.05 | 24.72 | <0.001 | |
| No vehicle in family (%) | 5.64 | 0.04 | 6.77 | 0.02 | 24.60 | <0.001 | |
| Multiracial communities (%) | 2.89 | 0.01 | 2.67 | 0.01 | 17.75 | <0.001 | |
| Hispanic residents (%) | 35.66 | 0.22 | 39.18 | 0.11 | 14.20 | <0.001 | |
| People speaking other languages (%) | 34.26 | 0.20 | 36.80 | 0.10 | 11.17 | <0.001 | |
| Bachelor or higher degrees (%) | 24.39 | 0.15 | 22.18 | 0.07 | 13.17 | <0.001 | |
| Access to Internet (%) | 81.61 | 0.12 | 78.44 | 0.06 | 22.82 | <0.001 | |
| Random Effects | Estimate of Variance of the Random Intercept | Variation Partition Coefficient (%) |
|---|---|---|
| Model 1: Null model | 0.25 | 7.16 |
| Model 2: Adjusted for patient-level factors | 0.21 | 6.10 |
| Model 3: Adjusted for both patient-level and neighborhood-level factors | 0.14 | 4.12 |
| Model 2 AOR (95%CI) | Model 3 AOR (95% CI) | |
| Sex (Reference Group—Male) Female | 1.77 [1.68–1.87] | 1.77 [1.68–1.87] |
| Race/ethnicity and preferred language (Reference group—NHW speaking English) Non-Hispanic Black and English Hispanic/Latino and English Hispanic/Latino and Spanish Other races and English Other races and other languages | 0.66 [0.61–0.70] 0.94 [0.86–1.02] 0.50 [0.45–0.56] 1.02 [0.87–1.18] 0.88 [0.74–1.04] | 0.66 [0.61–0.71] 0.94 [0.86–1.02] 0.50 [0.45–0.56] 1.01 [0.87–1.18] 0.87 [0.73–1.02] |
| Age Groups (Reference Group = 18–34 years) 35–49 years 50–64 years 65–74 years 75 years + | 1.15 [1.05–1.27] 0.95 [0.87–1.04] 0.74 [0.66–0.83] 0.53 [0.45–0.61] | 1.16 [1.05–1.27] 0.9 [0.87–1.04] 0.74 [0.66–0.83] 0.53 [0.45–0.61] |
| Marital Status (Reference Group = Single) Married Divorced Others | 1.47 [1.37–1.57] 1.29 [1.19–1.40] 1.23 [1.13–1.33] | 1.47 [1.37–1.57] 1.29 [1.19–1.40] 1.22 [1.13–1.33] |
| PCP Visit (Reference Group = No) Yes | 5.55 [5.07–6.07] | 5.54 [5.06–6.06] |
| Health Insurance (Reference Group = No) Yes | 2.41 [2.23–2.61] | 2.41 [2.22–2.61] |
| Neighborhood Factors | ||
| Measure of neighborhood variation MOR | 1.55 [1.43–1.68] | 1.43 [1.33–1.53] |
| Neighborhood factors (Associations) Percent residents below federal poverty level AOR (95%, p) IOR-80% POOR (%) Percent with no health insurance AOR (95%, p) IOR-80% POOR (%) Percent speaking other languages AOR (95%, p) IOR-80% POOR (%) | 0.99 [0.97–1.02] 1.00 [0.50–1.97] 50 0.94 [0.91–0.97] 0.94 [0.48–1.86] 45 1.02 [1.01–1.04] 1.02 [0.52–2.02] 48 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Shen, C.; Barbaro, M.; Ho, A.F.; Pathak, M.; Dunn, C.; Sambamoorthi, U. A Multi-Level Analysis of Individual and Neighborhood Factors Associated with Patient Portal Use among Adult Emergency Department Patients with Multimorbidity. Int. J. Environ. Res. Public Health 2023, 20, 1231. https://doi.org/10.3390/ijerph20021231
Wang H, Shen C, Barbaro M, Ho AF, Pathak M, Dunn C, Sambamoorthi U. A Multi-Level Analysis of Individual and Neighborhood Factors Associated with Patient Portal Use among Adult Emergency Department Patients with Multimorbidity. International Journal of Environmental Research and Public Health. 2023; 20(2):1231. https://doi.org/10.3390/ijerph20021231
Chicago/Turabian StyleWang, Hao, Chan Shen, Michael Barbaro, Amy F. Ho, Mona Pathak, Cita Dunn, and Usha Sambamoorthi. 2023. "A Multi-Level Analysis of Individual and Neighborhood Factors Associated with Patient Portal Use among Adult Emergency Department Patients with Multimorbidity" International Journal of Environmental Research and Public Health 20, no. 2: 1231. https://doi.org/10.3390/ijerph20021231







