Exploring Prehospital Data for Pandemic Preparedness: A Western Brazilian Amazon Case Study on COVID-19
Abstract
:1. Introduction
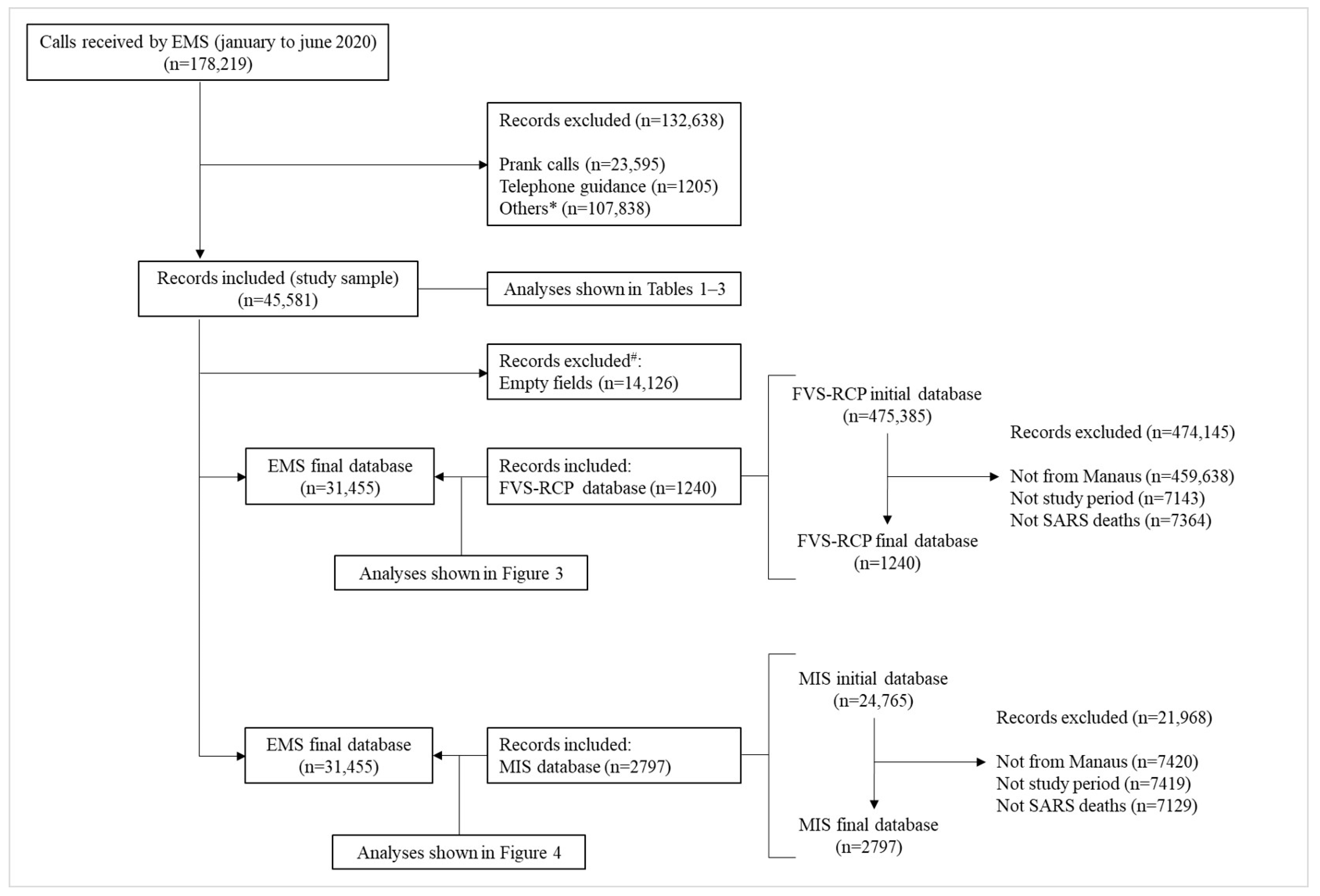
2. Materials and Methods
2.1. Study Settings and Patients
2.2. Data Collection
2.3. Data Analysis
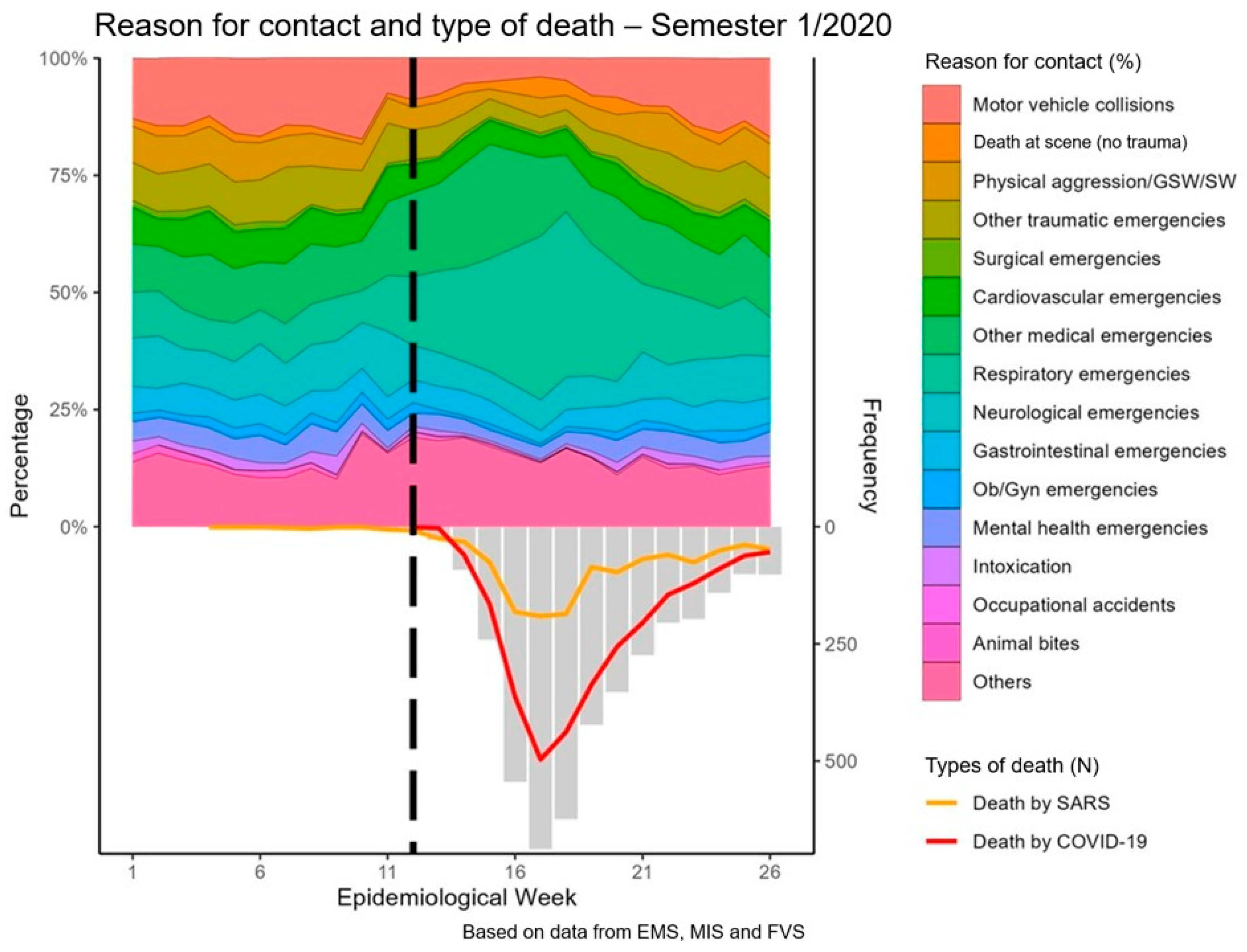
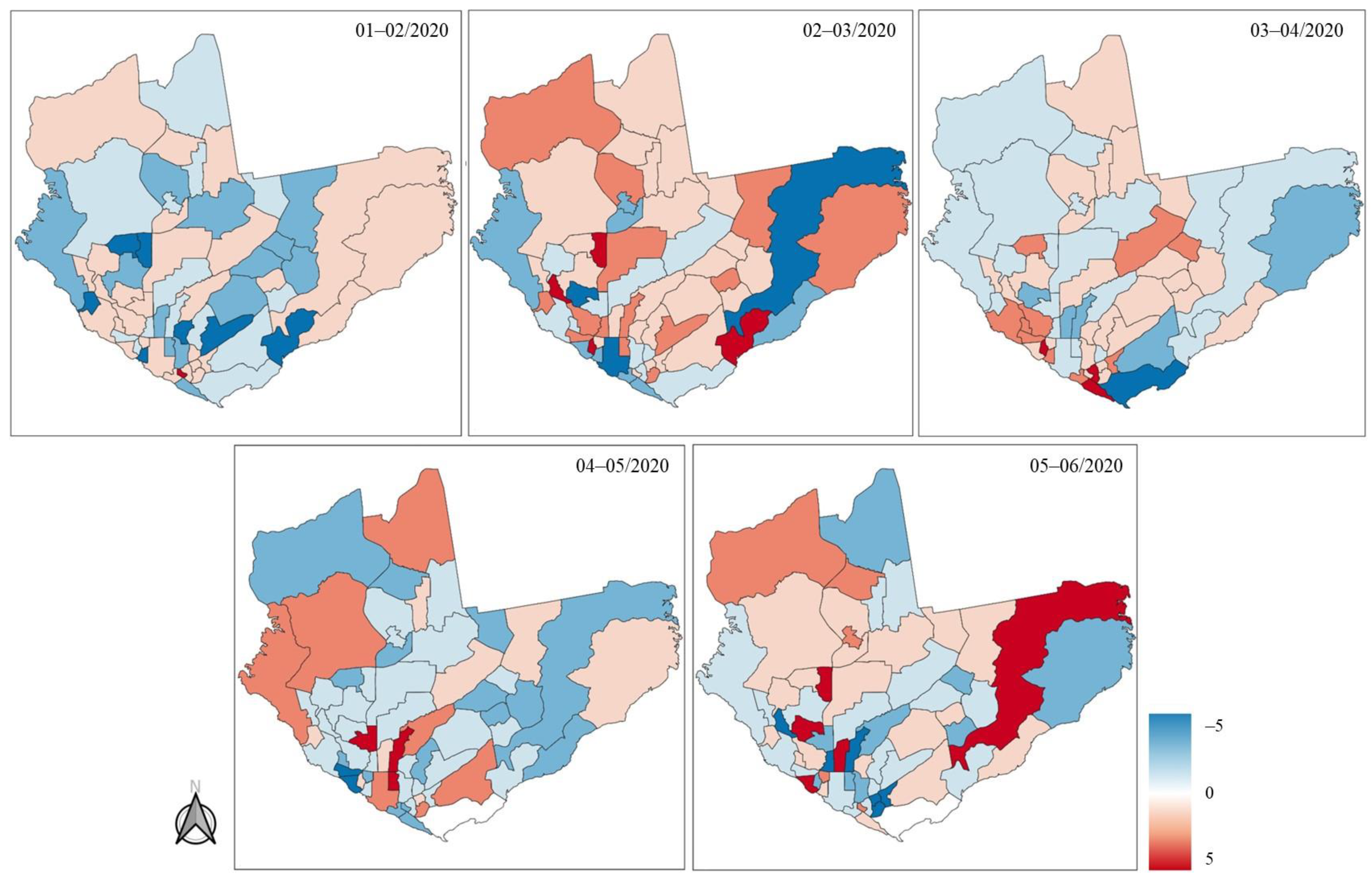
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ministério da Saúde. Relatório de Gestão; Ministério da Saúde: Brasília, Brazil, 2020.
- Ministério da Saúde, Brasília. Portaria No 2048, de 5 de Novembro de 2002. Reconhece a Urgência e Emergência Como Componente Importante de Assistência à Saúde; Ministério da Saúde: Brasília, Brazil, 2002.
- Desai, A.N.; Patel, P. Stopping the Spread of COVID-19. JAMA 2020, 323, 1516. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Ji, F.; Wang, L.; Wang, L.; Hao, J.; Dai, M.; Liu, Y.; Pan, X.; Fu, J.; Li, L.; et al. Asymptomatic and Human-to-Human Transmission of SARS-CoV-2 in a 2-Family Cluster, Xuzhou, China. Emerg. Infect. Dis. 2020, 26, 1626–1628. [Google Scholar] [CrossRef] [PubMed]
- Majumder, J.; Minko, T. Recent Developments on Therapeutic and Diagnostic Approaches for COVID-19. AAPS J. 2021, 23, 14. [Google Scholar] [CrossRef]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Gralinski, L.E.; Menachery, V.D. Return of the Coronavirus: 2019-nCoV. Viruses 2020, 12, 135. [Google Scholar] [CrossRef]
- Yüce, M.; Filiztekin, E.; Özkaya, K.G. COVID-19 diagnosis—A review of current methods. Biosens. Bioelectron. 2021, 172, 112752. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Guo, Y.; Pan, Y.; Zhao, Z.J. Structure analysis of the receptor binding of 2019-nCoV. Biochem. Biophys. Res. Commun. 2020, 525, 135–140. [Google Scholar] [CrossRef]
- Cheng, Z.J.; Shan, J. 2019 Novel coronavirus: Where we are and what we know. Infection 2020, 48, 155–163. [Google Scholar] [CrossRef]
- WHO. Coronavirus Disease 2019 (COVID-19) Situation Report—44 [Internet]. 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200304-sitrep-44-covid-19.pdf?sfvrsn=783b4c9d_2 (accessed on 25 June 2024).
- Acosta, L.D. Capacidad de respuesta frente a la pandemia de COVID-19 en América Latina y el Caribe. Rev. Panam. Salud Pública 2020, 44, 1. [Google Scholar] [CrossRef]
- Borghi-Silva, A.; Back, G.D.; de Araújo, A.S.G.; Oliveira, M.R.; Goulart, C.d.L.; Silva, R.N.; Bassi, D.; Mendes, R.G.; Arena, R. COVID-19 seen from a syndemic perspective: Impact of unhealthy habits and future perspectives to combat these negative interactions in Latin America. Prog. Cardiovasc. Dis. 2022, 71, 72–78. [Google Scholar] [CrossRef]
- The Lancet. COVID-19 in Brazil: “So What?”. Lancet 2020, 395, 1461. [Google Scholar]
- MCR C for GIDA. Report 21—Estimating COVID-19 Cases and Reproduction Number in Brazil [Internet]. 2020. Available online: https://www.medrxiv.org/content/10.1101/2020.05.09.20096701v2 (accessed on 25 June 2024).
- Naveca, F.G.; Nascimento, V.; de Souza, V.C.; Corado, A.d.L.; Nascimento, F.; Silva, G.; Costa, Á.; Duarte, D.; Pessoa, K.; Mejía, M.; et al. COVID-19 in Amazonas, Brazil, was driven by the persistence of endemic lineages and P.1 emergence. Nat. Med. 2021, 27, 1230–1238. [Google Scholar] [CrossRef]
- Ferrante, L.; Steinmetz, W.A.; Almeida, A.C.L.; Leão, J.; Vassão, R.C.; Tupinambás, U.; Fearnside, P.M.; Duczmal, L.H. Brazil’s policies condemn Amazonia to a second wave of COVID-19. Nat. Med. 2020, 26, 1315. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística. IBGE: Panorama Manaus, Amazonas [Internet]. 2022. Available online: https://cidades.ibge.gov.br/brasil/am/manaus/panorama (accessed on 20 November 2023).
- Fundação de Vigilância em Saúde do Amazonas. Painel COVID-19 Amazonas; Fundação de Vigilância em Saúde do Amazonas: Manaus, Brazil, 2022. [Google Scholar]
- Goldberg, S.A.; Cash, R.E.; Peters, G.; Weiner, S.G.; Greenough, P.G.; Seethala, R. The impact of COVID-19 on statewide EMS use for cardiac emergencies and stroke in Massachusetts. J. Am. Coll. Emerg. Physicians Open 2021, 2, e12351. [Google Scholar] [CrossRef] [PubMed]
- Satty, T.; Ramgopal, S.; Elmer, J.; Mosesso, V.N.; Martin-Gill, C. EMS responses and non-transports during the COVID-19 pandemic. Am. J. Emerg. Med. 2021, 42, 1–8. [Google Scholar] [CrossRef]
- Friedman, J.; Calderón-Villarreal, A.; Bojorquez, I.; Vera Hernández, C.; Schriger, D.L.; Tovar Hirashima, E. Excess Out-of-Hospital Mortality and Declining Oxygen Saturation: The Sentinel Role of Emergency Medical Services Data in the COVID-19 Crisis in Tijuana, Mexico. Ann. Emerg. Med. 2020, 76, 413–426. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization (PAHO). Epidemiological Calendar 2016: A Basic Element for the Use of the Time Variable in Health Surveillance [Internet]. 2016. Available online: https://www.paho.org/en/documents/epidemiological-calendar-2016-basic-element-use-time-variable-health-surveillance (accessed on 19 November 2023).
- Yang, B.Y.; Barnard, L.M.; Emert, J.M.; Drucker, C.; Schwarcz, L.; Counts, C.R.; Murphy, D.L.; Guan, S.; Kume, K.; Rodriquez, K.; et al. Clinical Characteristics of Patients with Coronavirus Disease 2019 (COVID-19) Receiving Emergency Medical Services in King County, Washington. JAMA Netw. Open 2020, 3, e2014549. [Google Scholar] [CrossRef]
- Jain, N.; Berkenbush, M.; Feldman, D.C.; Eskin, B.; Allegra, J.R. Effect of COVID19 on prehospital pronouncements and ED visits for stroke and myocardial infarction. Am. J. Emerg. Med. 2021, 43, 46–49. [Google Scholar] [CrossRef]
- Ministério da Saúde. Portaria 1.010, de 21 de Maio de 2012; Ministério da Saúde: Brasilia, Brazil, 2012.
- Masuda, Y.; Teoh, S.E.; Yeo, J.W.; Tan, D.J.; Jimian, D.L.; Lim, S.L.; Ong, M.E.; Blewer, A.L.; Ho, A.F. Variation in community and ambulance care processes for out-of-hospital cardiac arrest during the COVID-19 pandemic: A systematic review and meta-analysis. Sci. Rep. 2022, 12, 800. [Google Scholar] [CrossRef]
- Jaffe, E.; Sonkin, R.; Alpert, E.A.; Magid, A.; Knobler, H.Y. Flattening the COVID-19 Curve: The Unique Role of Emergency Medical Services in Containing a Global Pandemic. Isr. Med. Assoc. J. 2020, 22, 476–482. [Google Scholar]
- Malvestio, M.A.A.; de Sousa, R.M.C. Inequality in pre-hospital care in Brazil: Analysis of the efficiency and sufficiency of SAMU 192 coverage. Cienc. Saude Coletiva 2022, 27, 2921–2934. [Google Scholar] [CrossRef] [PubMed]
- Musso, M.; Tatum, D.; Hamer, D.; Hammarlund, R.; Son, L.; McMahon, P. The Relationship Between Grit and Resilience in Emergency Medical Service Personnel. Ochsner. J. 2019, 19, 199–203. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Streb, M.; Häller, P.; Michael, T. PTSD in paramedics: Resilience and sense of coherence. Behav. Cogn. Psychother. 2014, 42, 452–463. [Google Scholar] [CrossRef] [PubMed]


| Categories | Main Associated Terms |
|---|---|
| Motor vehicle collisions | Collision, run over, rollover, motorcycle, car, bus, bike, truck |
| Death at scene (nontraumatic) | Death without assistance, death, sudden death |
| Aggresion/stab wound/gunshot wound | Firearm, stab wound, aggression against women, aggression against elderly, sexual assault |
| Other trauma | Building collapse, landslide, explosion, drowning, burn, electric shock |
| Surgical emergencies | Acute abdominal pain, postoperative complication |
| Cardiac emergencies | Syncope, chest pain, tachycardia, hypotension, hypertensive emergency |
| Other medical emergencies | Pain, edema, epistaxis, hemorrhage, hyperglycemia, hypothermia, infection, eye complaints, neoplasm, hypoactivity, bleeding |
| Respiratory emergencies | Respiratory failure, respiratory arrest, flu, suspected COVID-19, dyspnea, asthma, pneumonia, SARS |
| Neurological emergencies | Facial asymmetry, coma, stroke, headache, paralysis, seizure, hemiplegia, hemiparesis, altered mental status |
| Obstetric/gynecology emergencies | Miscarriage, amniorrhexis, eclampsia, preeclampsia, hyperemesis, out-of-hospital delivery, labor, vaginal bleeding |
| Mental health emergencies | Psychomotor agitation, hallucination, delirium, psychosis, panic attack, suicide attempt, hanging, self-harm |
| Intoxication | Alcohol, drugs, exogenous intoxication, toxic |
| Occupational accident | Work-related accident |
| Animal bites | Venomous animal accident, animal bite |
| Total | Weeks 1–5 | Weeks 6–9 | Weeks 10–14 | Weeks 15–18 | Weeks 19–22 | Weeks 23–27 | p-Value | |
|---|---|---|---|---|---|---|---|---|
| n = 45,581 | n = 6016 | n = 5697 | n = 7333 | n = 12,600 | n = 7960 | n = 5975 | ||
| Gender | 0.002 | |||||||
| Female | 17,354/45,581 (38.1%) | 2233/6016 (37.1%) | 2056/5697 (36.1%) | 2785/7333 (38.0%) | 4876/12,600 (38.7%) | 3197/7960 (40.2%) | 2207/5975 (36.9%) | |
| Male | 28,227/45,581 (61.9%) | 3783/6016 (62.9%) | 3641/5697 (63.9%) | 4548/7333 (62.0%) | 7724/12,600 (61.3%) | 4763/7960 (59.8%) | 3768/5975 (63.1%) | |
| Age (years) | 47.0 (30.0–67.0) | 45.0 (28.0–67.0) | 44.0 (27.0–67.0) | 43.0 (26.0–64.0) | 52.0 (35.0–70.0) | 47.0 (30.0–67.0) | 43.0 (27.0–65.0) | <0.001 |
| Dispatched unit | 0.82 | |||||||
| Boat ambulance | 63/23,343 (0.3%) | 15/3909 (0.4%) | 7/3640 (0.2%) | 4/3274 (0.1%) | 17/4869 (0.3%) | 13/4093 (0.3%) | 7/3558 (0.2%) | |
| Motorcycle ambulance | 69/23,343 (0.3%) | 15/3909 (0.4%) | 9/3640 (0.2%) | 33/3274 (1.0%) | 12/4869 (0.2%) | 0/4093 (0.0%) | 0/3558 (0.0%) | |
| ALS ambulance | 2226/23,343 (9.5%) | 369/3909 (9.4%) | 304/3640 (8.4%) | 269/3274 (8.2%) | 586/4869 (12.0%) | 410/4093 (10.0%) | 288/3558 (8.1%) | |
| BLS ambulance | 20,979/23,343 (89.9%) | 3510/3909 (89.8%) | 3318/3640 (91.2%) | 2966/3274 (90.6%) | 4254/4869 (87.4%) | 3669/4093 (89.6%) | 3262/3558 (91.7%) | |
| Rapid intervention vehicle | 6/23,343 (0.0%) | 0/3909 (0.0%) | 2/3640 (0.1%) | 2/3274 (0.1%) | 0/4869 (0.0%) | 1/4093 (0.0%) | 1/3558 (0.0%) | |
| Reason for EMS call | <0.001 | |||||||
| Motor vehicle collisions | 3521/31,455 (11.2%) | 691/5114 (13.5%) | 759/4903 (15.5%) | 608/5385 (11.3%) | 262/5346 (4.9%) | 446/5612 (7.9%) | 755/5095 (14.8%) | |
| Dead at scene | 616/31,455 (2.0%) | 105/5114 (2.1%) | 84/4903 (1.7%) | 77/5385 (1.4%) | 120/5346 (2.2%) | 142/5612 (2.5%) | 88/5095 (1.7%) | |
| Aggression/SW/GSW | 1862/31,455 (5.9%) | 392/5114 (7.7%) | 364/4903 (7.4%) | 285/5385 (5.3%) | 170/5346 (3.2%) | 305/5612 (5.4%) | 346/5095 (6.8%) | |
| Other Trauma | 2211/31,455 (7.0%) | 431/5114 (8.4%) | 479/4903 (9.8%) | 379/5385 (7.0%) | 207/5346 (3.9%) | 291/5612 (5.2%) | 424/5095 (8.3%) | |
| Surgical | 343/31,455 (1.1%) | 75/5114 (1.5%) | 63/4903 (1.3%) | 39/5385 (0.7%) | 47/5346 (0.9%) | 54/5612 (1.0%) | 65/5095 (1.3%) | |
| Cardiac emergencies | 2063/31,455 (6.6%) | 395/5114 (7.7%) | 359/4903 (7.3%) | 323/5385 (6.0%) | 268/5346 (5.0%) | 363/5612 (6.5%) | 355/5095 (7.0%) | |
| Other medical emergencies * | 4505/31,455 (14.3%) | 582/5114 (11.4%) | 572/4903 (11.7%) | 840/5385 (15.6%) | 1171/5346 (21.9%) | 688/5612 (12.3%) | 652/5095 (12.8%) | |
| Respiratory emergencies | 4935/31,455 (15.7%) | 447/5114 (8.7%) | 398/4903 (8.1%) | 709/5385 (13.2%) | 1335/5346 (25.0%) | 1464/5612 (26.1%) | 582/5095 (11.4%) | |
| Neurological emergencies | 2611/31,455 (8.3%) | 472/5114 (9.2%) | 475/4903 (9.7%) | 458/5385 (8.5%) | 346/5346 (6.5%) | 380/5612 (6.8%) | 480/5095 (9.4%) | |
| Gastrointestinal emergencies | 1669/31,455 (5.3%) | 299/5114 (5.8%) | 286/4903 (5.8%) | 279/5385 (5.2%) | 253/5346 (4.7%) | 262/5612 (4.7%) | 290/5095 (5.7%) | |
| Ob/Gyn emergencies | 525/31,455 (1.7%) | 101/5114 (2.0%) | 105/4903 (2.1%) | 97/5385 (1.8%) | 51/5346 (1.0%) | 75/5612 (1.3%) | 96/5095 (1.9%) | |
| Mental health emergencies | 1243/31,455 (4.0%) | 227/5114 (4.4%) | 255/4903 (5.2%) | 190/5385 (3.5%) | 136/5346 (2.5%) | 219/5612 (3.9%) | 216/5095 (4.2%) | |
| Intoxication | 494/31,455 (1.6%) | 105/5114 (2.1%) | 110/4903 (2.2%) | 80/5385 (1.5%) | 31/5346 (0.6%) | 84/5612 (1.5%) | 84/5095 (1.6%) | |
| Occupational accidents | 8/31,455 (0.0%) | 3/5114 (0.1%) | 1/4903 (0.0%) | 0/5385 (0.0%) | 0/5346 (0.0%) | 2/5612 (0.0%) | 2/5095 (0.0%) | |
| Animal bites | 262/31,455 (0.8%) | 75/5114 (1.5%) | 62/4903 (1.3%) | 46/5385 (0.9%) | 19/5346 (0.4%) | 23/5612 (0.4%) | 37/5095 (0.7%) | |
| Others | 4587/31,455 (14.6%) | 714/5114 (14.0%) | 531/4903 (10.8%) | 975/5385 (18.1%) | 930/5346 (17.4%) | 814/5612 (14.5%) | 623/5095 (12.2%) | |
| Type of call | <0.001 | |||||||
| External causes | 7929/34,979 (22.7%) | 1612/5714 (28.2%) | 1681/5415 (31.0%) | 1337/6006 (22.3%) | 651/6057 (10.7%) | 1083/6101 (17.8%) | 1565/5686 (27.5%) | |
| Surgical | 125/34,979 (0.4%) | 15/5714 (0.3%) | 25/5415 (0.5%) | 16/6006 (0.3%) | 13/6057 (0.2%) | 17/6101 (0.3%) | 39/5686 (0.7%) | |
| Medical | 19,540/34,979 (55.9%) | 2883/5714 (50.5%) | 2645/5415 (48.8%) | 3186/6006 (53.0%) | 4143/6057 (68.4%) | 3725/6101 (61.1%) | 2958/5686 (52.0%) | |
| Ob/Gyn | 848/34,979 (2.4%) | 166/5714 (2.9%) | 163/5415 (3.0%) | 150/6006 (2.5%) | 96/6057 (1.6%) | 124/6101 (2.0%) | 149/5686 (2.6%) | |
| Not evaluated | 4501/34,979 (12.9%) | 703/5714 (12.3%) | 522/5415 (9.6%) | 952/6006 (15.9%) | 918/6057 (15.2%) | 799/6101 (13.1%) | 607/5686 (10.7%) | |
| Pediatrics | 705/34,979 (2.0%) | 82/5714 (1.4%) | 107/5415 (2.0%) | 160/6006 (2.7%) | 100/6057 (1.7%) | 124/6101 (2.0%) | 132/5686 (2.3%) | |
| Mental health | 1331/34,979 (3.8%) | 253/5714 (4.4%) | 272/5415 (5.0%) | 205/6006 (3.4%) | 136/6057 (2.2%) | 229/6101 (3.8%) | 236/5686 (4.2%) | |
| Response time (minutes) | 35.0 (24.0–54.6) | 32.8 (21.8–48.1) | 32.8 (21.8–48.1) | 32.8 (21.8–48.1) | 45.9 (30.6–67.7) | 43.7 (28.4–63.4) | 35.0 (24.0–50.2) | <0.001 |
| City zones | 0.88 | |||||||
| West central | 2423/33,670 (7.2%) | 390/5455 (7.1%) | 361/5208 (6.9%) | 406/5789 (7.0%) | 407/5866 (6.9%) | 448/5896 (7.6%) | 411/5456 (7.5%) | |
| South central | 2945/33,670 (8.7%) | 470/5455 (8.6%) | 509/5208 (9.8%) | 587/5789 (10.1%) | 474/5866 (8.1%) | 435/5896 (7.4%) | 470/5456 (8.6%) | |
| East | 7498/33,670 (22.3%) | 1249/5455 (22.9%) | 1096/5208 (21.0%) | 1321/5789 (22.8%) | 1325/5866 (22.6%) | 1332/5896 (22.6%) | 1175/5456 (21.5%) | |
| North | 9706/33,670 (28.8%) | 1578/5455 (28.9%) | 1487/5208 (28.6%) | 1596/5789 (27.6%) | 1647/5866 (28.1%) | 1786/5896 (30.3%) | 1612/5456 (29.5%) | |
| West | 4544/33,670 (13.5%) | 681/5455 (12.5%) | 673/5208 (12.9%) | 755/5789 (13.0%) | 849/5866 (14.5%) | 833/5896 (14.1%) | 753/5456 (13.8%) | |
| South | 6385/33,670 (19.0%) | 1068/5455 (19.6%) | 1068/5208 (20.5%) | 1101/5789 (19.0%) | 1135/5866 (19.3%) | 1017/5896 (17.2%) | 996/5456 (18.3%) | |
| Riverine communities | 169/33,670 (0.5%) | 19/5455 (0.3%) | 14/5208 (0.3%) | 23/5789 (0.4%) | 29/5866 (0.5%) | 45/5896 (0.8%) | 39/5456 (0.7%) |
| Total | Pre-Pandemic | Pandemic | p-Value | |
|---|---|---|---|---|
| n = 45,581 | n = 14,133 | n = 31,448 | ||
| Age (years) | 47.0 (30.0–67.0) | 44.0 (27.0–66.0) | 48.0 (30.0–68.0) | <0.001 |
| Dispatched unit | 0.0007 | |||
| Boat ambulance | 63/23,343 (0.3%) | 25/8888 (0.3%) | 38/14,455 (0.3%) | |
| Motorcycle ambulance | 69/23,343 (0.3%) | 34/8888 (0.4%) | 35/14,455 (0.2%) | |
| ALS ambulance | 2226/23,343 (9.5%) | 762/8888 (8.6%) | 1464/14,455 (10.1%) | |
| BLS ambulance | 20,979/23,343 (89.9%) | 8064/8888 (90.7%) | 12,915/14,455 (89.3%) | |
| Rapid intervention vehicle | 6/23,343 (0.0%) | 3/8888 (0.0%) | 3/14,455 (0.0%) | |
| Reason for EMS call | <0.001 | |||
| Motor vehicle collision | 3521/31,455 (11.2%) | 1770/11,887 (14.9%) | 1751/19,568 (8.9%) | |
| Death at scene (non-traumatic) | 616/31,455 (2.0%) | 208/11,887 (1.7%) | 408/19,568 (2.1%) | |
| Physical aggression/GSW/SW | 1862/31,455 (5.9%) | 867/11,887 (7.3%) | 995/19,568 (5.1%) | |
| Other traumatic emergencies | 2211/31,455 (7.0%) | 1055/11,887 (8.9%) | 1156/19,568 (5.9%) | |
| Surgical emergencies | 343/31,455 (1.1%) | 152/11,887 (1.3%) | 191/19,568 (1.0%) | |
| Cardiac emergencies | 2063/31,455 (6.6%) | 878/11,887 (7.4%) | 1185/19,568 (6.1%) | |
| Other medical emergencies | 4505/31,455 (14.3%) | 1356/11,887 (11.4%) | 3149/19,568 (16.1%) | |
| Respiratory emergencies | 4935/31,455 (15.7%) | 991/11,887 (8.3%) | 3944/19,568 (20.2%) | |
| Neurological emergencies | 2611/31,455 (8.3%) | 1138/11,887 (9.6%) | 1473/19,568 (7.5%) | |
| Gastrointestinal emergencies | 1669/31,455 (5.3%) | 689/11,887 (5.8%) | 980/19,568 (5.0%) | |
| Ob/Gyn emergencies | 525/31,455 (1.7%) | 248/11,887 (2.1%) | 277/19,568 (1.4%) | |
| Mental health emergencies | 1243/31,455 (4.0%) | 559/11,887 (4.7%) | 684/19,568 (3.5%) | |
| Intoxication | 494/31,455 (1.6%) | 255/11,887 (2.1%) | 239/19,568 (1.2%) | |
| Occupational accidents | 8/31,455 (0.0%) | 4/11,887 (0.0%) | 4/19,568 (0.0%) | |
| Animal bites | 262/31,455 (0.8%) | 149/11,887 (1.3%) | 113/19,568 (0.6%) | |
| Others | 4587/31,455 (14.6%) | 1568/11,887 (13.2%) | 3019/19,568 (15.4%) | |
| Type of call | <0.001 | |||
| External cause | 7929/34,979 (22.7%) | 3892/13,197 (29.5%) | 4037/21,782 (18.5%) | |
| Surgical | 125/34,979 (0.4%) | 46/13,197 (0.3%) | 79/21,782 (0.4%) | |
| Medical | 19,540/34,979 (55.9%) | 6497/13,197 (49.2%) | 13,043/21,782 (59.9%) | |
| Ob/Gyn | 848/34,979 (2.4%) | 392/13,197 (3.0%) | 456/21,782 (2.1%) | |
| Not evaluated | 4501/34,979 (12.9%) | 1534/13,197 (11.6%) | 2967/21,782 (13.6%) | |
| Pediatrics | 705/34,979 (2.0%) | 231/13,197 (1.8%) | 474/21,782 (2.2%) | |
| Mental health | 1331/34,979 (3.8%) | 605/13,197 (4.6%) | 726/21,782 (3.3%) | |
| Response time (minutes) | 35.0 (24.0–54.6) | 32.8 (21.8–48.1) | 39.3 (26.2–59.0) | <0.001 |
| City zones | 0.80 | |||
| West central | 2423/33,670 (7.2%) | 889/12,637 (7.0%) | 1534/21,033 (7.3%) | |
| South central | 2945/33,670 (8.7%) | 1170/12,637 (9.3%) | 1775/21,033 (8.4%) | |
| East | 7498/33,670 (22.3%) | 2784/12,637 (22.0%) | 4714/21,033 (22.4%) | |
| North | 9706/33,670 (28.8%) | 3632/12,637 (28.7%) | 6074/21,033 (28.9%) | |
| West | 4544/33,670 (13.5%) | 1594/12,637 (12.6%) | 2950/21,033 (14.0%) | |
| South | 6385/33,670 (19.0%) | 2522/12,637 (20.0%) | 3863/21,033 (18.4%) | |
| Riverine communities | 169/33,670 (0.5%) | 46/12,637 (0.4%) | 123/21,033 (0.6%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, E.; Silva, B.M.d.; Goulart, C.d.L.; Valente, J.; Cubas-Vega, N.; Sato, C.; Rezende, A.G.; Almeida, T.V.R.; de Amorim, R.L.O.; Salinas, J.L.; et al. Exploring Prehospital Data for Pandemic Preparedness: A Western Brazilian Amazon Case Study on COVID-19. Int. J. Environ. Res. Public Health 2024, 21, 1229. https://doi.org/10.3390/ijerph21091229
Fernandes E, Silva BMd, Goulart CdL, Valente J, Cubas-Vega N, Sato C, Rezende AG, Almeida TVR, de Amorim RLO, Salinas JL, et al. Exploring Prehospital Data for Pandemic Preparedness: A Western Brazilian Amazon Case Study on COVID-19. International Journal of Environmental Research and Public Health. 2024; 21(9):1229. https://doi.org/10.3390/ijerph21091229
Chicago/Turabian StyleFernandes, Eduardo, Bernardo Maia da Silva, Cássia da Luz Goulart, Jefferson Valente, Nádia Cubas-Vega, Camila Sato, Anna Gabriela Rezende, Taynna Vernalha Rocha Almeida, Robson Luís Oliveira de Amorim, Jorge Luis Salinas, and et al. 2024. "Exploring Prehospital Data for Pandemic Preparedness: A Western Brazilian Amazon Case Study on COVID-19" International Journal of Environmental Research and Public Health 21, no. 9: 1229. https://doi.org/10.3390/ijerph21091229








