Current Trends in Surgical Management of Hepatocellular Carcinoma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Staging and Treatment Selection
3. Downstaging Therapy
3.1. Locoregional Therapies
3.2. Systemic Therapies
4. Surgical Management of HCC
4.1. Hepatic Resection
4.1.1. Expansion of Selection Criteria
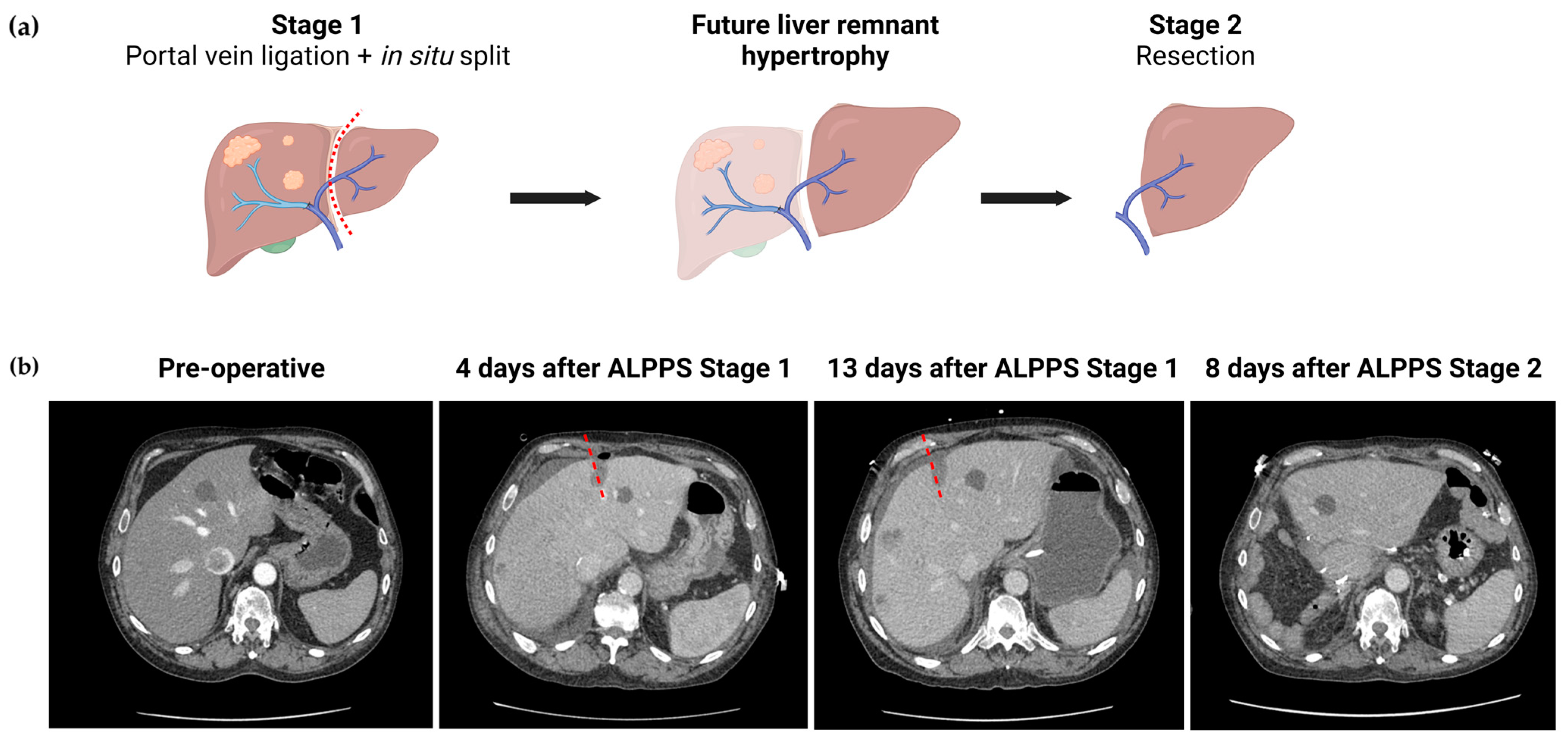
4.1.2. Optimizing Future Liver Remnant
4.1.3. Minimally Invasive Surgery
4.1.4. Visualization Techniques
4.1.5. Ex Vivo Resection
4.1.6. Hemorrhage Prevention and Control
4.2. Liver Transplantation
4.2.1. Inclusion Criteria
4.2.2. Bridging and Downstaging Therapy
4.3. Ablation
5. Future Directions and Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rumgay, H.; Arnold, M.; Ferlay, J.; Lesi, O.; Cabasag, C.J.; Vignat, J.; Laversanne, M.; McGlynn, K.A.; Soerjomataram, I. Global burden of primary liver cancer in 2020 and predictions to 2040. J. Hepatol. 2022, 77, 1598–1606. [Google Scholar] [CrossRef] [PubMed]
- Marrero, J.A.; Kulik, L.M.; Sirlin, C.B.; Zhu, A.X.; Finn, R.S.; Abecassis, M.M.; Roberts, L.R.; Heimbach, J.K. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the american association for the study of liver diseases. Hepatology 2018, 68, 723–750. [Google Scholar] [CrossRef] [PubMed]
- Rumgay, H.; Ferlay, J.; de Martel, C.; Georges, D.; Ibrahim, A.S.; Zheng, R.; Wei, W.; Lemmens, V.E.P.P.; Soerjomataram, I. Global, regional and national burden of primary liver cancer by subtype. Eur. J. Cancer 2022, 161, 108–118. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. Electronic address: [email protected]; European Association for the Study of the Liver EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef]
- Reig, M.; Forner, A.; Rimola, J.; Ferrer-Fàbrega, J.; Burrel, M.; Garcia-Criado, Á.; Kelley, R.K.; Galle, P.R.; Mazzaferro, V.; Salem, R.; et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J. Hepatol. 2022, 76, 681–693. [Google Scholar] [CrossRef]
- Llovet, J.M.; Kelley, R.K.; Villanueva, A.; Singal, A.G.; Pikarsky, E.; Roayaie, S.; Lencioni, R.; Koike, K.; Zucman-Rossi, J.; Finn, R.S. Hepatocellular carcinoma. Nat. Rev. Dis. Primers 2021, 7, 6. [Google Scholar] [CrossRef]
- Raoul, J.-L.; Forner, A.; Bolondi, L.; Cheung, T.T.; Kloeckner, R.; de Baere, T. Updated use of TACE for hepatocellular carcinoma treatment: How and when to use it based on clinical evidence. Cancer Treat. Rev. 2019, 72, 28–36. [Google Scholar] [CrossRef]
- Matsuo, Y. Stereotactic body radiotherapy for hepatocellular carcinoma: A brief overview. Curr. Oncol. 2023, 30, 2493–2500. [Google Scholar] [CrossRef]
- Sangro, B.; Iñarrairaegui, M.; Bilbao, J.I. Radioembolization for hepatocellular carcinoma. J. Hepatol. 2012, 56, 464–473. [Google Scholar] [CrossRef]
- Young, S.; Golzarian, J. Locoregional Therapies in the Treatment of 3- to 5-cm Hepatocellular Carcinoma: Critical Review of the Literature. AJR Am. J. Roentgenol. 2020, 215, 223–234. [Google Scholar] [CrossRef]
- Zhang, H.; Zhang, W.; Jiang, L.; Chen, Y. Recent advances in systemic therapy for hepatocellular carcinoma. Biomark. Res. 2022, 10, 3. [Google Scholar] [CrossRef]
- Wang, S.; Wang, Y.; Yu, J.; Wu, H.; Zhou, Y. Lenvatinib as First-Line Treatment for Unresectable Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 5525. [Google Scholar] [CrossRef]
- Bruix, J.; Qin, S.; Merle, P.; Granito, A.; Huang, Y.-H.; Bodoky, G.; Pracht, M.; Yokosuka, O.; Rosmorduc, O.; Breder, V.; et al. RESORCE Investigators Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017, 389, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Wilhelm, S.M.; Dumas, J.; Adnane, L.; Lynch, M.; Carter, C.A.; Schütz, G.; Thierauch, K.-H.; Zopf, D. Regorafenib (BAY 73-4506): A new oral multikinase inhibitor of angiogenic, stromal and oncogenic receptor tyrosine kinases with potent preclinical antitumor activity. Int. J. Cancer 2011, 129, 245–255. [Google Scholar] [CrossRef]
- Abou-Alfa, G.K.; Meyer, T.; Cheng, A.-L.; El-Khoueiry, A.B.; Rimassa, L.; Ryoo, B.-Y.; Cicin, I.; Merle, P.; Chen, Y.; Park, J.-W.; et al. Cabozantinib in Patients with Advanced and Progressing Hepatocellular Carcinoma. N. Engl. J. Med. 2018, 379, 54–63. [Google Scholar] [CrossRef]
- Zhu, A.X.; Kang, Y.-K.; Yen, C.-J.; Finn, R.S.; Galle, P.R.; Llovet, J.M.; Assenat, E.; Brandi, G.; Pracht, M.; Lim, H.Y.; et al. REACH-2 study investigators Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019, 20, 282–296. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Rong, D.; Zhang, B.; Zheng, W.; Wang, X.; Chen, Z.; Tang, W. Current perspectives on the immunosuppressive tumor microenvironment in hepatocellular carcinoma: Challenges and opportunities. Mol. Cancer 2019, 18, 130. [Google Scholar] [CrossRef]
- Yau, T.; Park, J.-W.; Finn, R.S.; Cheng, A.-L.; Mathurin, P.; Edeline, J.; Kudo, M.; Harding, J.J.; Merle, P.; Rosmorduc, O.; et al. Nivolumab versus sorafenib in advanced hepatocellular carcinoma (CheckMate 459): A randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 2022, 23, 77–90. [Google Scholar] [CrossRef]
- Qin, S.; Chen, Z.; Fang, W.; Ren, Z.; Xu, R.; Ryoo, B.-Y.; Meng, Z.; Bai, Y.; Chen, X.; Liu, X.; et al. Pembrolizumab Versus Placebo as Second-Line Therapy in Patients From Asia with Advanced Hepatocellular Carcinoma: A Randomized, Double-Blind, Phase III Trial. J. Clin. Oncol. 2023, 41, 1434–1443. [Google Scholar] [CrossRef] [PubMed]
- Saung, M.T.; Pelosof, L.; Casak, S.; Donoghue, M.; Lemery, S.; Yuan, M.; Rodriguez, L.; Schotland, P.; Chuk, M.; Davis, G.; et al. FDA Approval Summary: Nivolumab Plus Ipilimumab for the Treatment of Patients with Hepatocellular Carcinoma Previously Treated with Sorafenib. Oncologist 2021, 26, 797–806. [Google Scholar] [CrossRef]
- Yau, T.; Kang, Y.-K.; Kim, T.-Y.; El-Khoueiry, A.B.; Santoro, A.; Sangro, B.; Melero, I.; Kudo, M.; Hou, M.-M.; Matilla, A.; et al. Efficacy and safety of nivolumab plus ipilimumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib: The checkmate 040 randomized clinical trial. JAMA Oncol. 2020, 6, e204564. [Google Scholar] [CrossRef] [PubMed]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. IMbrave150 Investigators Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef] [PubMed]
- Sinner, F.; Pinter, M.; Scheiner, B.; Ettrich, T.J.; Sturm, N.; Gonzalez-Carmona, M.A.; Waidmann, O.; Finkelmeier, F.; Himmelsbach, V.; De Toni, E.N.; et al. Atezolizumab Plus Bevacizumab in Patients with Advanced and Progressing Hepatocellular Carcinoma: Retrospective Multicenter Experience. Cancers 2022, 14, 5966. [Google Scholar] [CrossRef] [PubMed]
- Kelley, R.K.; Rimassa, L.; Cheng, A.-L.; Kaseb, A.; Qin, S.; Zhu, A.X.; Chan, S.L.; Melkadze, T.; Sukeepaisarnjaroen, W.; Breder, V.; et al. Cabozantinib plus atezolizumab versus sorafenib for advanced hepatocellular carcinoma (COSMIC-312): A multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2022, 23, 995–1008. [Google Scholar] [CrossRef] [PubMed]
- Abou-Alfa, G.K.; Lau, G.; Kudo, M.; Chan, S.L.; Kelley, R.K.; Furuse, J.; Sukeepaisarnjaroen, W.; Kang, Y.-K.; Van Dao, T.; De Toni, E.N.; et al. Tremelimumab plus Durvalumab in Unresectable Hepatocellular Carcinoma. NEJM Evid. 2022. [Google Scholar] [CrossRef]
- Kelley, R.K.; Sangro, B.; Harris, W.; Ikeda, M.; Okusaka, T.; Kang, Y.-K.; Qin, S.; Tai, D.W.-M.; Lim, H.Y.; Yau, T.; et al. Safety, efficacy, and pharmacodynamics of tremelimumab plus durvalumab for patients with unresectable hepatocellular carcinoma: Randomized expansion of a phase I/II study. J. Clin. Oncol. 2021, 39, 2991–3001. [Google Scholar] [CrossRef]
- Qin, S.; Chan, S.L.; Gu, S.; Bai, Y.; Ren, Z.; Lin, X.; Chen, Z.; Jia, W.; Jin, Y.; Guo, Y.; et al. CARES-310 Study Group Camrelizumab plus rivoceranib versus sorafenib as first-line therapy for unresectable hepatocellular carcinoma (CARES-310): A randomised, open-label, international phase 3 study. Lancet 2023, 402, 1133–1146. [Google Scholar] [CrossRef]
- Zhu, X.-D.; Huang, C.; Shen, Y.-H.; Ji, Y.; Ge, N.-L.; Qu, X.-D.; Chen, L.; Shi, W.-K.; Li, M.-L.; Zhu, J.-J.; et al. Downstaging and Resection of Initially Unresectable Hepatocellular Carcinoma with Tyrosine Kinase Inhibitor and Anti-PD-1 Antibody Combinations. Liver Cancer 2021, 10, 320–329. [Google Scholar] [CrossRef]
- Hoshino, T.; Naganuma, A.; Furusawa, A.; Suzuki, Y.; Hirai, K.; Sakamoto, I.; Ogawa, T.; Ogawa, A.; Hatanaka, T.; Kakizaki, S. A case of conversion hepatectomy for huge hepatocellular carcinoma with adrenal metastasis and vascular invasion after atezolizumab-bevacizumab treatment. Clin. J. Gastroenterol. 2022, 15, 776–783. [Google Scholar] [CrossRef]
- Fukunaga, A.; Takata, K.; Itoh, S.; Yamauchi, R.; Tanaka, T.; Yokoyama, K.; Shakado, S.; Kohashi, K.; Yoshizumi, T.; Hirai, F. Complete tumor necrosis confirmed by conversion hepatectomy after atezolizumab-bevacizumab treatment for advanced-stage hepatocellular carcinoma with lung metastasis. Clin. J. Gastroenterol. 2023, 16, 224–228. [Google Scholar] [CrossRef]
- Okuno, M.; Ishii, T.; Ichida, A.; Soyama, A.; Takemura, N.; Hirono, S.; Eguchi, S.; Hasegawa, K.; Sasaki, Y.; Uemura, K.; et al. Protocol of the RACB study: A multicenter, single-arm, prospective study to evaluate the efficacy of resection of initially unresectable hepatocellular carcinoma with atezolizumab combined with bevacizumab. BMC Cancer 2023, 23, 780. [Google Scholar] [CrossRef]
- Ozer, M.; Goksu, S.Y.; Akagunduz, B.; George, A.; Sahin, I. Adoptive cell therapy in hepatocellular carcinoma: A review of clinical trials. Cancers 2023, 15, 1808. [Google Scholar] [CrossRef]
- Jeng, L.-B.; Liao, L.-Y.; Shih, F.-Y.; Teng, C.-F. Dendritic-Cell-Vaccine-Based Immunotherapy for Hepatocellular Carcinoma: Clinical Trials and Recent Preclinical Studies. Cancers 2022, 14, 4380. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Lei, Y.; Huang, J.; An, Y.; Ren, Y.; Chen, L.; Zhao, H.; Zheng, C. Recent advances in oncolytic virus therapy for hepatocellular carcinoma. Front. Oncol. 2023, 13, 1172292. [Google Scholar] [CrossRef]
- Cheng, S.; Chen, M.; Cai, J.; Sun, J.; Guo, R.; Bi, X.; Lau, W.Y.; Wu, M. Chinese Expert Consensus on Multidisciplinary Diagnosis and Treatment of Hepatocellular Carcinoma with Portal Vein Tumor Thrombus (2018 Edition). Liver Cancer 2020, 9, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Kokudo, T.; Hasegawa, K.; Matsuyama, Y.; Takayama, T.; Izumi, N.; Kadoya, M.; Kudo, M.; Ku, Y.; Sakamoto, M.; Nakashima, O.; et al. Liver Cancer Study Group of Japan Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. J. Hepatol. 2016, 65, 938–943. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Guo, W.X.; Chen, M.S.; Mao, Y.L.; Sun, B.C.; Shi, J.; Zhang, Y.J.; Meng, Y.; Yang, Y.F.; Cong, W.M.; et al. Multimodality Treatment for Hepatocellular Carcinoma with Portal Vein Tumor Thrombus: A Large-Scale, Multicenter, Propensity Mathching Score Analysis. Medicine 2016, 95, e3015. [Google Scholar] [CrossRef] [PubMed]
- Berzigotti, A.; Reig, M.; Abraldes, J.G.; Bosch, J.; Bruix, J. Portal hypertension and the outcome of surgery for hepatocellular carcinoma in compensated cirrhosis: A systematic review and meta-analysis. Hepatology 2015, 61, 526–536. [Google Scholar] [CrossRef]
- Molina, V.; Sampson-Dávila, J.; Ferrer, J.; Fondevila, C.; Díaz Del Gobbo, R.; Calatayud, D.; Bruix, J.; García-Valdecasas, J.C.; Fuster, J. Benefits of laparoscopic liver resection in patients with hepatocellular carcinoma and portal hypertension: A case-matched study. Surg. Endosc. 2018, 32, 2345–2354. [Google Scholar] [CrossRef]
- Del Basso, C.; Gaillard, M.; Lainas, P.; Zervaki, S.; Perlemuter, G.; Chagué, P.; Rocher, L.; Voican, C.S.; Dagher, I.; Tranchart, H. Current strategies to induce liver remnant hypertrophy before major liver resection. World J. Hepatol. 2021, 13, 1629–1641. [Google Scholar] [CrossRef]
- Kauffmann, R.; Fong, Y. Post-hepatectomy liver failure. Hepatobiliary Surg. Nutr. 2014, 3, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Adams, R.B.; Aloia, T.A.; Loyer, E.; Pawlik, T.M.; Taouli, B.; Vauthey, J.-N. Americas Hepato-Pancreato-Biliary Association; Society of Surgical Oncology; Society for Surgery of the Alimentary Tract Selection for hepatic resection of colorectal liver metastases: Expert consensus statement. HPB 2013, 15, 91–103. [Google Scholar] [CrossRef] [PubMed]
- van Lienden, K.P.; van den Esschert, J.W.; de Graaf, W.; Bipat, S.; Lameris, J.S.; van Gulik, T.M.; van Delden, O.M. Portal vein embolization before liver resection: A systematic review. Cardiovasc. Intervent. Radiol. 2013, 36, 25–34. [Google Scholar] [CrossRef]
- Buechter, M.; Gerken, G. Liver Function-How to Screen and to Diagnose: Insights from Personal Experiences, Controlled Clinical Studies and Future Perspectives. J. Pers. Med. 2022, 12, 1657. [Google Scholar] [CrossRef]
- de Lédinghen, V.; Vergniol, J. Transient elastography (FibroScan). Gastroenterol. Clin. Biol. 2008, 32, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.W.-S.; Chan, H.L.-Y. Transient elastography. J. Gastroenterol. Hepatol. 2010, 25, 1726–1731. [Google Scholar] [CrossRef] [PubMed]
- Mikolasevic, I.; Orlic, L.; Franjic, N.; Hauser, G.; Stimac, D.; Milic, S. Transient elastography (FibroScan(®)) with controlled attenuation parameter in the assessment of liver steatosis and fibrosis in patients with nonalcoholic fatty liver disease—Where do we stand? World J. Gastroenterol. 2016, 22, 7236–7251. [Google Scholar] [CrossRef] [PubMed]
- Gennisson, J.L.; Deffieux, T.; Fink, M.; Tanter, M. Ultrasound elastography: Principles and techniques. Diagn. Interv. Imaging 2013, 94, 487–495. [Google Scholar] [CrossRef]
- Lurie, Y.; Webb, M.; Cytter-Kuint, R.; Shteingart, S.; Lederkremer, G.Z. Non-invasive diagnosis of liver fibrosis and cirrhosis. World J. Gastroenterol. 2015, 21, 11567–11583. [Google Scholar] [CrossRef]
- Faria, S.C.; Ganesan, K.; Mwangi, I.; Shiehmorteza, M.; Viamonte, B.; Mazhar, S.; Peterson, M.; Kono, Y.; Santillan, C.; Casola, G.; et al. MR imaging of liver fibrosis: Current state of the art. Radiographics 2009, 29, 1615–1635. [Google Scholar] [CrossRef]
- Hussain, S.M.; Reinhold, C.; Mitchell, D.G. Cirrhosis and lesion characterization at MR imaging. Radiographics 2009, 29, 1637–1652. [Google Scholar] [CrossRef]
- Ge, P.-L.; Du, S.-D.; Mao, Y.-L. Advances in preoperative assessment of liver function. Hepatobiliary Pancreat. Dis. Int. 2014, 13, 361–370. [Google Scholar] [CrossRef]
- Schneider, P.D. Preoperative assessment of liver function. Surg. Clin. N. Am. 2004, 84, 355–373. [Google Scholar] [CrossRef]
- De Gasperi, A.; Mazza, E.; Prosperi, M. Indocyanine green kinetics to assess liver function: Ready for a clinical dynamic assessment in major liver surgery? World J. Hepatol. 2016, 8, 355–367. [Google Scholar] [CrossRef] [PubMed]
- de Graaf, W.; Häusler, S.; Heger, M.; van Ginhoven, T.M.; van Cappellen, G.; Bennink, R.J.; Kullak-Ublick, G.A.; Hesselmann, R.; van Gulik, T.M.; Stieger, B. Transporters involved in the hepatic uptake of (99m)Tc-mebrofenin and indocyanine green. J. Hepatol. 2011, 54, 738–745. [Google Scholar] [CrossRef] [PubMed]
- Zarrinpar, A.; Lee, C.; Noguchi, E.; Yersiz, H.; Agopian, V.G.; Kaldas, F.M.; Farmer, D.G.; Busuttil, R.W. A rapid, reproducible, noninvasive predictor of liver graft survival. J. Surg. Res. 2015, 197, 183–190. [Google Scholar] [CrossRef]
- Mobley, C.M.; Zarrinpar, A. Portable device for the analysis of liver function: A boon to liver surgery and critical care. Expert. Rev. Med. Devices 2016, 13, 1–4. [Google Scholar] [CrossRef]
- Palmer, C.N.; Coates, P.J.; Davies, S.E.; Shephard, E.A.; Phillips, I.R. Localization of cytochrome P-450 gene expression in normal and diseased human liver by in situ hybridization of wax-embedded archival material. Hepatology 1992, 16, 682–687. [Google Scholar] [CrossRef]
- Stockmann, M.; Lock, J.F.; Riecke, B.; Heyne, K.; Martus, P.; Fricke, M.; Lehmann, S.; Niehues, S.M.; Schwabe, M.; Lemke, A.-J.; et al. Prediction of postoperative outcome after hepatectomy with a new bedside test for maximal liver function capacity. Ann. Surg. 2009, 250, 119–125. [Google Scholar] [CrossRef]
- Buechter, M.; Thimm, J.; Baba, H.A.; Bertram, S.; Willuweit, K.; Gerken, G.; Kahraman, A. Liver maximum capacity: A novel test to accurately diagnose different stages of liver fibrosis. Digestion 2019, 100, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.-H.; Miao, X.-Y.; Zou, H.; Xiong, L.; Wen, Y.; Chen, B.; Liu, X.; Zhou, J.-J. End-stage liver disease score and future liver remnant volume predict post-hepatectomy liver failure in hepatocellular carcinoma. World J. Clin. Cases 2019, 7, 3734–3741. [Google Scholar] [CrossRef]
- Zou, H.; Tao, Y.; Wang, Z.-M. Integration of Child-Pugh score with future liver remnant yields improved prediction of liver dysfunction risk for HBV-related hepatocellular carcinoma following hepatic resection. Oncol. Lett. 2017, 13, 3631–3637. [Google Scholar] [CrossRef]
- Gudowska, M.; Gruszewska, E.; Panasiuk, A.; Cylwik, B.; Flisiak, R.; Świderska, M.; Szmitkowski, M.; Chrostek, L. Hyaluronic acid concentration in liver diseases. Clin. Exp. Med. 2016, 16, 523–528. [Google Scholar] [CrossRef]
- Abdalla, E.K.; Hicks, M.E.; Vauthey, J.N. Portal vein embolization: Rationale, technique and future prospects. Br. J. Surg. 2001, 88, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Bertens, K.A.; Hawel, J.; Lung, K.; Buac, S.; Pineda-Solis, K.; Hernandez-Alejandro, R. ALPPS: Challenging the concept of unresectability--a systematic review. Int. J. Surg. 2015, 13, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Abulkhir, A.; Limongelli, P.; Healey, A.J.; Damrah, O.; Tait, P.; Jackson, J.; Habib, N.; Jiao, L.R. Preoperative portal vein embolization for major liver resection: A meta-analysis. Ann. Surg. 2008, 247, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.; Zhang, W.Y.; Chok, K.; Dai, J.; Ji, R.; Kwan, C.; Man, N.; Poon, R.; Lo, C.M. ALPPS Versus Portal Vein Embolization for Hepatitis-related Hepatocellular Carcinoma: A Changing Paradigm in Modulation of Future Liver Remnant Before Major Hepatectomy. Ann. Surg. 2021, 273, 957–965. [Google Scholar] [CrossRef]
- Sulieman, I.; Elmoghazy, W.; Ghali, M.S.; Mahfouz, A.; Elaffandi, A.; Khalaf, H. Associating liver partition and portal vein ligation for staged hepatectomy in Qatar: Initial experience with two case series and review of the literature. Int. J. Surg. Case Rep. 2019, 58, 108–116. [Google Scholar] [CrossRef]
- Cioffi, L.; Belli, G.; Izzo, F.; Fantini, C.; D’Agostino, A.; Russo, G.; Patrone, R.; Granata, V.; Belli, A. Minimally Invasive ALPPS Procedure: A Review of Feasibility and Short-Term Outcomes. Cancers 2023, 15, 1700. [Google Scholar] [CrossRef]
- Schlegel, A.; Lesurtel, M.; Melloul, E.; Limani, P.; Tschuor, C.; Graf, R.; Humar, B.; Clavien, P.A. ALPPS: From human to mice highlighting accelerated and novel mechanisms of liver regeneration. Ann. Surg. 2014, 260, 839–846, discussion 846. [Google Scholar] [CrossRef]
- Chen, H.; Wang, X.; Zhu, W.; Li, Y.; Yu, Z.; Li, H.; Yang, Y.; Zhu, S.; Chen, X.; Wang, G. Application of associating liver partition and portal vein ligation for staged hepatectomy for initially unresectable hepatocellular carcinoma. BMC Surg. 2022, 22, 407. [Google Scholar] [CrossRef] [PubMed]
- Berardi, G.; Guglielmo, N.; Colasanti, M.; Meniconi, R.L.; Ferretti, S.; Mariano, G.; Usai, S.; Angrisani, M.; Pecoraro, A.; Lucarini, A.; et al. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) for advanced hepatocellular carcinoma with macrovascular invasion. Updates Surg. 2022, 74, 927–936. [Google Scholar] [CrossRef] [PubMed]
- Serenari, M.; Ratti, F.; Guglielmo, N.; Zanello, M.; Mocchegiani, F.; Lenzi, J.; Colledan, M.; Mazzaferro, V.; Cillo, U.; Ferrero, A.; et al. ALPPS Italian Registry Evolution of minimally invasive techniques and surgical outcomes of ALPPS in Italy: A comprehensive trend analysis over 10 years from a national prospective registry. Surg. Endosc. 2023, 37, 5285–5294. [Google Scholar] [CrossRef]
- Kazaryan, A.M.; Pavlik Marangos, I.; Rosseland, A.R.; Røsok, B.I.; Mala, T.; Villanger, O.; Mathisen, O.; Giercksky, K.-E.; Edwin, B. Laparoscopic liver resection for malignant and benign lesions: Ten-year Norwegian single-center experience. Arch. Surg. 2010, 145, 34–40. [Google Scholar] [CrossRef]
- Yoon, Y.-I.; Kim, K.-H.; Kang, S.-H.; Kim, W.-J.; Shin, M.-H.; Lee, S.-K.; Jung, D.-H.; Park, G.-C.; Ahn, C.-S.; Moon, D.-B.; et al. Pure laparoscopic versus open right hepatectomy for hepatocellular carcinoma in patients with cirrhosis: A propensity score matched analysis. Ann. Surg. 2017, 265, 856–863. [Google Scholar] [CrossRef]
- Peng, Y.; Yang, Y.; Chen, K.; Li, B.; Zhang, Y.; Xu, H.; Guo, S.; Wei, Y.; Liu, F. Hemihepatic versus total hepatic inflow occlusion for laparoscopic hepatectomy: A randomized controlled trial. Int. J. Surg. 2022, 107, 106961. [Google Scholar] [CrossRef]
- Witowski, J.; Rubinkiewicz, M.; Mizera, M.; Wysocki, M.; Gajewska, N.; Sitkowski, M.; Małczak, P.; Major, P.; Budzyński, A.; Pędziwiatr, M. Meta-analysis of short- and long-term outcomes after pure laparoscopic versus open liver surgery in hepatocellular carcinoma patients. Surg. Endosc. 2019, 33, 1491–1507. [Google Scholar] [CrossRef] [PubMed]
- Andreou, A.; Struecker, B.; Raschzok, N.; Krenzien, F.; Haber, P.; Wabitsch, S.; Waldbaur, C.; Touet, E.-M.; Eichelberg, A.-C.; Atanasov, G.; et al. Minimal-invasive versus open hepatectomy for hepatocellular carcinoma: Comparison of postoperative outcomes and long-term survivals using propensity score matching analysis. Surg. Oncol. 2018, 27, 751–758. [Google Scholar] [CrossRef]
- El-Gendi, A.; El-Shafei, M.; El-Gendi, S.; Shawky, A. Laparoscopic versus open hepatic resection for solitary hepatocellular carcinoma less than 5 cm in cirrhotic patients: A randomized controlled study. J. Laparoendosc. Adv. Surg. Tech. A 2018, 28, 302–310. [Google Scholar] [CrossRef]
- Ruzzenente, A.; Bagante, F.; Ratti, F.; Alaimo, L.; Marques, H.P.; Silva, S.; Soubrane, O.; Endo, I.; Sahara, K.; Beal, E.W.; et al. Minimally Invasive Versus Open Liver Resection for Hepatocellular Carcinoma in the Setting of Portal Vein Hypertension: Results of an International Multi-institutional Analysis. Ann. Surg. Oncol. 2020, 27, 3360–3371. [Google Scholar] [CrossRef]
- Ng, K.K.C.; Chong, C.C.N.; Lee, K.-F.; Lai, P.B.S.; Cheng, T.K.C.; Chen, H.-W.; Yi, B.; Huang, J.-W. Asia-Pacific multicentre randomized trial of laparoscopic versus open major hepatectomy for hepatocellular carcinoma (AP-LAPO trial). BJS Open. 2023, 7, zrac166. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.-B.; Lin, J.-M.; Chen, Y.-P.; Ye, X.-X. Surgical site wound infection and pain after laparoscopic repeat hepatectomy for recurrent hepatocellular carcinoma. Int. Wound J. 2023. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Yuan, Q.; Xu, Y.; Wang, W. Comparative clinical outcomes of robot-assisted liver resection versus laparoscopic liver resection: A meta-analysis. PLoS ONE 2020, 15, e0240593. [Google Scholar] [CrossRef]
- Feldbrügge, L.; Wabitsch, S.; Benzing, C.; Krenzien, F.; Kästner, A.; Haber, P.K.; Atanasov, G.; Andreou, A.; Öllinger, R.; Pratschke, J.; et al. Safety and feasibility of laparoscopic liver resection in patients with a history of abdominal surgeries. HPB 2020, 22, 1191–1196. [Google Scholar] [CrossRef] [PubMed]
- Feldbrügge, L.; Ortiz Galindo, S.A.; Frisch, O.; Benzing, C.; Krenzien, F.; Riddermann, A.; Kästner, A.; Nevermann, N.F.; Malinka, T.; Schöning, W.; et al. Safety and feasibility of robotic liver resection after previous abdominal surgeries. Surg. Endosc. 2022, 36, 2842–2849. [Google Scholar] [CrossRef]
- Kobayashi, K.; Kawaguchi, Y.; Kobayashi, Y.; Matsumura, M.; Ishizawa, T.; Akamatsu, N.; Kaneko, J.; Arita, J.; Sakamoto, Y.; Kokudo, N.; et al. Identification of liver lesions using fluorescence imaging: Comparison of methods for administering indocyanine green. HPB 2021, 23, 262–269. [Google Scholar] [CrossRef]
- Ishizawa, T.; Fukushima, N.; Shibahara, J.; Masuda, K.; Tamura, S.; Aoki, T.; Hasegawa, K.; Beck, Y.; Fukayama, M.; Kokudo, N. Real-time identification of liver cancers by using indocyanine green fluorescent imaging. Cancer 2009, 115, 2491–2504. [Google Scholar] [CrossRef]
- Ladd, A.D.; Zarate Rodriguez, J.; Lewis, D.; Warren, C.; Duarte, S.; Loftus, T.J.; Nassour, I.; Soma, D.; Hughes, S.J.; Hammill, C.W.; et al. Low vs Standard-Dose Indocyanine Green in the Identification of Biliary Anatomy Using Near-Infrared Fluorescence Imaging: A Multicenter Randomized Controlled Trial. J. Am. Coll. Surg. 2023, 236, 711–717. [Google Scholar] [CrossRef]
- Barbier, L.; Souche, R.; Slim, K.; Ah-Soune, P. Long-term consequences of bile duct injury after cholecystectomy. J. Visc. Surg. 2014, 151, 269–279. [Google Scholar] [CrossRef]
- Fang, C.; An, J.; Bruno, A.; Cai, X.; Fan, J.; Fujimoto, J.; Golfieri, R.; Hao, X.; Jiang, H.; Jiao, L.R.; et al. Consensus recommendations of three-dimensional visualization for diagnosis and management of liver diseases. Hepatol. Int. 2020, 14, 437–453. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Zeng, X.; Hu, H.; Xiang, N.; Zeng, N.; Wen, S.; Tian, J.; Yang, J.; Fang, C. Perioperative and Disease-Free Survival Outcomes after Hepatectomy for Centrally Located Hepatocellular Carcinoma Guided by Augmented Reality and Indocyanine Green Fluorescence Imaging: A Single-Center Experience. J. Am. Coll. Surg. 2023, 236, 328–337. [Google Scholar] [CrossRef]
- Zhang, W.; Zhu, W.; Yang, J.; Xiang, N.; Zeng, N.; Hu, H.; Jia, F.; Fang, C. Augmented reality navigation for stereoscopic laparoscopic anatomical hepatectomy of primary liver cancer: Preliminary experience. Front. Oncol. 2021, 11, 663236. [Google Scholar] [CrossRef]
- Zawistowski, M.; Nowaczyk, J.; Jakubczyk, M.; Domagała, P. Outcomes of ex vivo liver resection and autotransplantation: A systematic review and meta-analysis. Surgery 2020, 168, 631–642. [Google Scholar] [CrossRef]
- Baimas-George, M.R.; Levi, D.M.; Vrochides, D. Three Possible Variations in Ex Vivo Hepatectomy: Achieving R0 Resection by Auto-transplantation. J. Gastrointest. Surg. 2019, 23, 2294–2297. [Google Scholar] [CrossRef]
- Hemming, A.W.; Reed, A.I.; Langham, M.R.; Fujita, S.; Howard, R.J. Combined resection of the liver and inferior vena cava for hepatic malignancy. Ann. Surg. 2004, 239, 712, discussion 719. [Google Scholar] [CrossRef] [PubMed]
- Pichlmayr, R.; Bretschneider, H.J.; Kirchner, E.; Ringe, B.; Lamesch, P.; Gubernatis, G.; Hauss, J.; Niehaus, K.J.; Kaukemüller, J. Ex situ operation on the liver. A new possibility in liver surgery. Langenbecks Arch. Chir. 1988, 373, 122–126. [Google Scholar] [CrossRef] [PubMed]
- Weiner, J.; Hemming, A.; Levi, D.; Beduschi, T.; Matsumoto, R.; Mathur, A.; Liou, P.; Griesemer, A.; Samstein, B.; Cherqui, D.; et al. Ex vivo liver resection and autotransplantation: Should it be used more frequently? Ann. Surg. 2022, 276, 854–859. [Google Scholar] [CrossRef] [PubMed]
- Shen, S.; Kong, J.; Qiu, Y.; Zhang, S.; Qin, Y.; Wang, W. Ex vivo liver resection and autotransplantation versus allotransplantation for end-stage hepatic alveolar echinococcosis. Int. J. Infect. Dis. 2019, 79, 87–93. [Google Scholar] [CrossRef]
- Qiu, Y.; Huang, B.; Yang, X.; Wang, T.; Shen, S.; Yang, Y.; Wang, W. Evaluating the Benefits and Risks of Ex Vivo Liver Resection and Autotransplantation in Treating Hepatic End-stage Alveolar Echinococcosis. Clin. Infect. Dis. 2022, 75, 1289–1296. [Google Scholar] [CrossRef]
- Ozsoy, M.; Ozsoy, Z.; Yilmaz, S.; Arikan, Y. Ex situ Liver Resection and Partial Liver Autotransplantation for Advanced Cholangiocarcinoma. Niger. J. Surg. 2019, 25, 97–100. [Google Scholar] [CrossRef]
- Li, J.; Chen, S.; Zhang, T.; Ma, K. Intermittent Pringle maneuver combined with controlled low Central venous pressure prolongs hepatic hilum occlusion time in patients with hepatocellular carcinoma complicated by post hepatitis B cirrhosis: A randomized controlled trial. Scand. J. Gastroenterol. 2023, 58, 497–504. [Google Scholar] [CrossRef]
- Liu, T.-S.; Shen, Q.-H.; Zhou, X.-Y.; Shen, X.-; Lai, L.; Hou, X.-M.; Liu, K. Application of controlled low central venous pressure during hepatectomy: A systematic review and meta-analysis. J. Clin. Anesth. 2021, 75, 110467. [Google Scholar] [CrossRef]
- Yang, P.; Gao, S.; Chen, X.; Xiong, W.; Hai, B.; Huang, X. Milrinone is better choice for controlled low central venous pressure during hepatectomy: A randomized, controlled trial comparing with nitroglycerin. Int. J. Surg. 2021, 94, 106080. [Google Scholar] [CrossRef]
- Cheng, H.; Clymer, J.W.; Po-Han Chen, B.; Sadeghirad, B.; Ferko, N.C.; Cameron, C.G.; Hinoul, P. Prolonged operative duration is associated with complications: A systematic review and meta-analysis. J. Surg. Res. 2018, 229, 134–144. [Google Scholar] [CrossRef]
- Ortiz Galindo, S.A.; Haber, P.K.; Benzing, C.; Krenzien, F.; Riddermann, A.; Frisch, O.; Schöning, W.; Schmelzle, M.; Pratschke, J.; Feldbrügge, L. Safety of intermittent Pringle maneuver during minimally invasive liver resection in patients with hepatocellular carcinoma with and without cirrhosis. Langenbecks Arch. Surg. 2022, 407, 235–244. [Google Scholar] [CrossRef]
- Wang, H.-Q.; Yang, J.-Y.; Yan, L.-N. Hemihepatic versus total hepatic inflow occlusion during hepatectomy: A systematic review and meta-analysis. World J. Gastroenterol. 2011, 17, 3158–3164. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Lu, D.; Ling, Q.; Wei, X.; Wu, J.; Zhou, L.; Yan, S.; Wu, L.; Geng, L.; Ke, Q.; et al. Liver transplantation for hepatocellular carcinoma beyond the Milan criteria. Gut 2016, 65, 1035–1041. [Google Scholar] [CrossRef]
- Commander, S.J.; Shaw, B.; Washburn, L.; Yoeli, D.; Rana, A.; Goss, J.A. A long-term experience with expansion of Milan criteria for liver transplant recipients. Clin. Transplant. 2018, 32, e13254. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.; Dodge, J.L.; Roberts, J.P.; Hirose, R.; Yao, F.Y. Alpha-Fetoprotein Decrease from > 1000 to < 500 ng/mL in Patients with Hepatocellular Carcinoma Leads to Improved Posttransplant Outcomes. Hepatology 2019, 69, 1193–1205. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.; Bhangui, P.; Yao, F.Y.; Mazzaferro, V.; Toso, C.; Akamatsu, N.; Durand, F.; Ijzermans, J.; Polak, W.; Zheng, S.; et al. Liver Transplantation for Hepatocellular Carcinoma. Working Group Report from the ILTS Transplant Oncology Consensus Conference. Transplantation 2020, 104, 1136–1142. [Google Scholar] [CrossRef]
- Mazzaferro, V.; Citterio, D.; Bhoori, S.; Bongini, M.; Miceli, R.; De Carlis, L.; Colledan, M.; Salizzoni, M.; Romagnoli, R.; Antonelli, B.; et al. Liver transplantation in hepatocellular carcinoma after tumour downstaging (XXL): A randomised, controlled, phase 2b/3 trial. Lancet Oncol. 2020, 21, 947–956. [Google Scholar] [CrossRef] [PubMed]
- Sapisochin, G.; Barry, A.; Doherty, M.; Fischer, S.; Goldaracena, N.; Rosales, R.; Russo, M.; Beecroft, R.; Ghanekar, A.; Bhat, M.; et al. Stereotactic body radiotherapy vs. TACE or RFA as a bridge to transplant in patients with hepatocellular carcinoma. An intention-to-treat analysis. J. Hepatol. 2017, 67, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Vitale, A.; Scolari, F.; Bertacco, A.; Gringeri, E.; D’Amico, F.; Bassi, D.; D’Amico, F.E.; Angeli, P.; Burra, P.; Lai, Q.; et al. Sustained Complete Response after Biological Downstaging in Patients with Hepatocellular Carcinoma: XXL-Like Prioritization for Liver Transplantation or “Wait and See” Strategy? Cancers 2021, 13, 2406. [Google Scholar] [CrossRef]
- Takayama, T.; Hasegawa, K.; Izumi, N.; Kudo, M.; Shimada, M.; Yamanaka, N.; Inomata, M.; Kaneko, S.; Nakayama, H.; Kawaguchi, Y.; et al. Surgery versus Radiofrequency Ablation for Small Hepatocellular Carcinoma: A Randomized Controlled Trial (SURF Trial). Liver Cancer 2022, 11, 209–218. [Google Scholar] [CrossRef]
- Shiina, S.; Teratani, T.; Obi, S.; Sato, S.; Tateishi, R.; Fujishima, T.; Ishikawa, T.; Koike, Y.; Yoshida, H.; Kawabe, T.; et al. A randomized controlled trial of radiofrequency ablation with ethanol injection for small hepatocellular carcinoma. Gastroenterology 2005, 129, 122–130. [Google Scholar] [CrossRef]
- Yu, J.; Yu, X.-L.; Han, Z.-Y.; Cheng, Z.-G.; Liu, F.-Y.; Zhai, H.-Y.; Mu, M.-J.; Liu, Y.-M.; Liang, P. Percutaneous cooled-probe microwave versus radiofrequency ablation in early-stage hepatocellular carcinoma: A phase III randomised controlled trial. Gut 2017, 66, 1172–1173. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, X.; Ding, X.; Wang, Z.; Fan, Y.; Chen, G.; Hu, X.; Zheng, J.; Xue, Z.; He, X.; et al. Novel irreversible electroporation ablation (Nano-knife) versus radiofrequency ablation for the treatment of solid liver tumors: A comparative, randomized, multicenter clinical study. Front. Oncol. 2022, 12, 945123. [Google Scholar] [CrossRef] [PubMed]


| Reference | Year | Study Population | Findings |
|---|---|---|---|
| Section 4.1 Resection: Section 4.1.1 Expansion of selection criteria | |||
| Kokudo et al. [36] | 2016 | 6474 (LR n = 2093 and non-LR n = 4381) | Patients with PVTT confined to a first-order branch had improved survival with surgical intervention. |
| Molina et al. [39] | 2018 | 45 (CSPH n = 15 and w/o CSPH n = 30) | Laparoscopic resection could be safely performed in well-selected patients with CSPH. |
| Section 4.1 Resection: Section 4.1.2 Optimizing future liver remnant | |||
| Buechter et al. [60] | 2019 | 102 | The LiMAx test is a non-invasive tool capable of providing real-time measurements of liver function with higher accuracy than TE and serum biomarker. |
| Chan et al. [67] | 2021 | 148 (ALPPS n = 46 and PVE n = 102) | ALPPS allowed more patients to undergo resection, promoting faster and greater FLR hypertrophy, while maintaining comparable postoperative and oncological outcomes. |
| Cioffi et al. [69] | 2023 | 119 | Minimally invasive ALPPS demonstrated FLR augmentation of nearly 88%, suggesting to be a feasible and effective approach with the potential of improving the morbidity related to this procedure. |
| Serenari et al. [73] | 2023 | 268 | From 2012 to 2021, the minimally invasive approach to ALPPS increased by 43% in Stage 1, and 27% in Stage 2. This approach was associated with reduced morbidity. |
| Section 4.1 Resection: Section 4.1.3 Minimally invasive surgery | |||
| El-Genti et al. [79] | 2018 | 50 (OLR n = 25 and LLR n = 25) | LLR provides shorter operative time and length of hospital stay with similar complication rate and oncological outcomes. |
| Wang et al. [82] | 2023 | 4380 (LLR n = 1108 and OLR n = 3289) | LLR reduces wound infection, wound pain, and bile leakage when compared to OLR. |
| Zhang et al. [83] | 2020 | 3544 (RLR n = 1312 and LLR n = 2232) | RLR was associated with decreased conversion rate, but increased total cost, operative time, and transfusion rate when compared to LLR. |
| Section 4.1 Resection: Section 4.1.4 Visalization techniques | |||
| Zhu et al. [91] | 2023 | 76 (ARN-FI n = 42 and non-ARN-FI n = 34) | The use of a combination of ARN and fluorescence imaging (FI) in laparoscopic resections was associated with reduced rates of blood loss, conversion to laparotomy, postoperative complications, and hospital stay. |
| Section 4.1 Resection: Section 4.1.5 Ex vivo resection | |||
| Weiner et al. [97] | 2022 | 35 | Favorable outcomes for overall survival at 1, 3, and 5 years for patients with low-grade to highly aggressive malignancies suggest that the more liberal use of this technique could benefit selected patients. |
| Section 4.1 Resection: Section 4.1.6 Hemorrhage prevention and control | |||
| Li et al. [101] | 2023 | 151 (Group 20 n = 75 and Group 15 n = 76) | In resections using IPM combined with CLCVP, extending the hepatic hilum occlusion time from 15 to 20 min resulted in significantly shorter operative times with similar bleeding and postoperative aminotransferase levels. |
| Section 4.2 Liver transplantation: Section 4.2.1 Inclusion criteria | |||
| Xu et al. [107] | 2016 | 6012 | The Milan criteria excluded 56% of LT candidates. Meanwhile, 4 alternatives, more included crtieria, expanded the pool of eligible patients from 12.4 to 51.5%, and maintained similar outcomes. |
| Commander et al. [108] | 2018 | 2068 (Region 4 Criteria n = 180 and Milan Criteria n = 1888) | 10 years after the implementation of expanded LT criteria for HCC patients within UNOS Region 4, there was a 9% rise in LT-eligible patients, with no difference in overall, recurrence-free, or allograft survivals when compared to the Milan criteria group. |
| Section 4.3 Ablation | |||
| Takayama et al. [114] | 2022 | 308 (RFA n = 151 and Surgery n = 150) | Among patients with small (≤3 cm) and few (≤3) tumors, RFA showed comparable recurrence-free survival, but higher local recurrence rate. RFA was associated with shorter operative time and hospital stay. |
| Yu et al. [116] | 2017 | 454 (RFA n = 251 and MWA n = 203) | MWA was associated with lower hospitalization costs, shorter duration, with similar complication and tumor progression rates when compared to RFA. |
| Zhang et al. [70,117] | 2022 | 152 (RFA n = 74 and IRE n = 78) | IRE procedures were significantly longer, but demonstrated comparable rates of success, recurrence, and adverse effects to RFA. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angeli-Pahim, I.; Chambers, A.; Duarte, S.; Zarrinpar, A. Current Trends in Surgical Management of Hepatocellular Carcinoma. Cancers 2023, 15, 5378. https://doi.org/10.3390/cancers15225378
Angeli-Pahim I, Chambers A, Duarte S, Zarrinpar A. Current Trends in Surgical Management of Hepatocellular Carcinoma. Cancers. 2023; 15(22):5378. https://doi.org/10.3390/cancers15225378
Chicago/Turabian StyleAngeli-Pahim, Isabella, Anastasia Chambers, Sergio Duarte, and Ali Zarrinpar. 2023. "Current Trends in Surgical Management of Hepatocellular Carcinoma" Cancers 15, no. 22: 5378. https://doi.org/10.3390/cancers15225378





