Impact of Multiple COVID-19 Waves on Gynaecological Cancer Services in the UK
Abstract
:Simple Summary
Abstract
1. Introduction
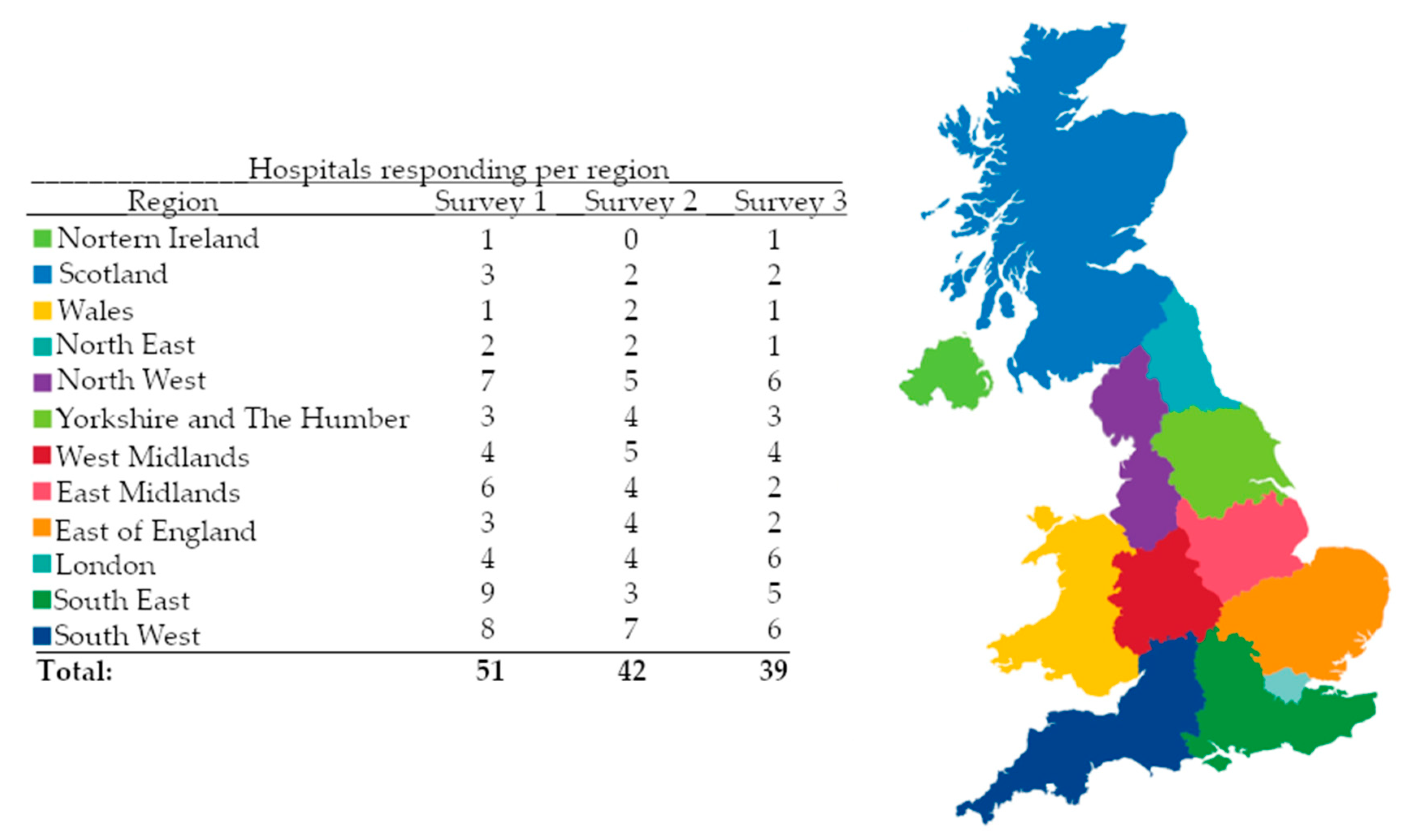
2. Materials and Methods
2.1. Patient Public Involvement
2.2. Ethics
3. Results
3.1. Staffing
3.2. Gynaecological Cancer Referrals, MDT Workload, and Meetings
3.3. Virtual Clinics
3.4. Service Provision
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
4.3. Comparison with Other Literature
4.4. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhou, M.; Kan, M.-Y. The varying impacts of COVID-19 and its related measures in the UK: A year in review. PLoS ONE 2021, 16, e0257286. [Google Scholar] [CrossRef]
- NERVTAG. COVID-19 Variant of Concern B.1.1.7. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/961037/NERVTAG_note_on_B.1.1.7_severity_for_SAGE_77__1_.pdf (accessed on 27 January 2023).
- Office, U.C. COVID-19 Response—Spring 2021 (Summary). Available online: https://www.gov.uk/government/publications/covid-19-response-spring-2021/covid-19-response-spring-2021-summary#step-2---not-before-12-april (accessed on 27 January 2023).
- Elliott, P.; Bodinier, B.; Eales, O.; Wang, H.; Haw, D.; Elliott, J.; Whitaker, M.; Jonnerby, J.; Tang, D.; Walters, C.E. Rapid increase in Omicron infections in England during December 2021: REACT-1 study. Science 2022, 375, 1406–1411. [Google Scholar] [CrossRef]
- Kirsebom, F.C.; Andrews, N.; Stowe, J.; Toffa, S.; Sachdeva, R.; Gallagher, E.; Groves, N.; O’Connell, A.-M.; Chand, M.; Ramsay, M. COVID-19 vaccine effectiveness against the omicron (BA. 2) variant in England. Lancet Infect. Dis. 2022, 22, 931–933. [Google Scholar] [CrossRef]
- Manchanda, R.; Oxley, S.; Ghaem-Maghami, S.; Sundar, S. COVID-19 and the impact on gynecologic cancer care. Int. J. Gynaecol. Obstet. 2021, 155, 94–101. [Google Scholar] [CrossRef]
- Liang, W.; Guan, W.; Chen, R.; Wang, W.; Li, J.; Xu, K.; Li, C.; Ai, Q.; Lu, W.; Liang, H.; et al. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020, 21, 335–337. [Google Scholar] [CrossRef]
- The Expert Advisory Group on Cancer to the Chief Medical Officers of England and Wales. A Policy Framework for Commissioning Cancer Services. Available online: https://webarchive.nationalarchives.gov.uk/ukgwa/20080817211349mp_/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4071083?IdcService=GET_FILE&dID=17110&Rendition=Web (accessed on 27 January 2023).
- NHS England. Communique 001559. Guidance for Trusts on the Management of Non-Coronavirus Patients Requiring Acute Treatment: Cancer. 2020. Available online: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/2003/specialty-guide-acute-treatment-cancer-2023-march-2020.pdf (accessed on 13 April 2021).
- BGCS. BGCS Framework for Care of Patients with Gynaecological Cancer during the COVID-19 Pandemic. 2020. Available online: https://www.bgcs.org.uk/wp-content/uploads/2020/2004/BGCS-covid-guidance-v2022.-2013.2004.2020.pdf (accessed on 27 January 2023).
- NICE. COVID-19 Rapid Guideline: Delivery of Radiotherapy (NG162). 2020. Available online: www.nice.org.uk/guidance/ng162 (accessed on 13 April 2021).
- NICE. COVID-19 Rapid Guideline: Delivery of Systemic Anticancer Treatments (NG161). 2020. Available online: www.nice.org.uk/guidance/ng161 (accessed on 13 April 2021).
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Weisel, K.C.; Morgner-Miehlke, A.; Petersen, C.; Fiedler, W.; Block, A.; Schafhausen, P.; Knobloch, J.K.; Bokemeyer, C. Implications of SARS-CoV-2 infection and COVID-19 crisis on clinical cancer care: Report of the University Cancer Center Hamburg. Oncol. Res. Treat. 2020, 43, 307–313. [Google Scholar] [CrossRef]
- Bhandoria, G.; Shylasree, T.S.; Bhandarkar, P.; Ahuja, V.; Maheshwari, A.; Sekhon, R.; Somashekhar, S.P. Impact of COVID-19 Pandemic on Gynecological Oncology Care: Glimpse into Association of Gynecological Oncologists of India (AGOI) Perspective. Indian J. Gynecol. Oncol. 2020, 18, 71. [Google Scholar] [CrossRef]
- Bogani, G.; Apolone, G.; Ditto, A.; Scambia, G.; Panici, P.B.; Angioli, R.; Pignata, S.; Greggi, S.; Scollo, P.; Delia, M.; et al. Impact of COVID-19 in gynecologic oncology: A Nationwide Italian Survey of the SIGO and MITO groups. J. Gynecol. Oncol. 2020, 31, e92. [Google Scholar] [CrossRef]
- Nogami, Y.; Komatsu, H.; Makabe, T.; Hasegawa, Y.; Yokoyama, Y.; Kawana, K.; Okamoto, A.; Mikami, M.; Katabuchi, H.; Oncology, C.-T.F.o.t.J.S.o.G. Impact of COVID-19 on gynecologic cancer treatment in Japan: A nationwide survey by the Japan Society of Gynecologic Oncology (JSGO). J. Gynecol. Oncol. 2022, 33, e8. [Google Scholar] [CrossRef]
- Bruce, S.F.; Huysman, B.; Bharucha, J.; Massad, L.S.; Mullen, M.M.; Hagemann, A.R.; Fuh, K.C.; McCourt, C.K.; Thaker, P.H.; Khabele, D.; et al. Impact of the COVID-19 pandemic on referral to and delivery of gynecologic oncology care. Gynecol. Oncol. Rep. 2022, 39, 100928. [Google Scholar] [CrossRef]
- Davies, J.M.; Spencer, A.; Macdonald, S.; Dobson, L.; Haydock, E.; Burton, H.; Angelopoulos, G.; Martin-Hirsch, P.; Wood, N.J.; Thangavelu, A.; et al. Cervical cancer and COVID-an assessment of the initial effect of the pandemic and subsequent projection of impact for women in England: A cohort study. BJOG 2022, 129, 1133–1139. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, B.D.; Ordóñez-Mena, J.M.; Lay-Flurrie, S.; Sheppard, J.P.; Liyanage, H.; McGagh, D.; Sherlock, J.; Williams, J.; Smith, M.; Drakesmith, C.W.; et al. Consultations for clinical features of possible cancer and associated urgent referrals before and during the COVID-19 pandemic: An observational cohort study from English primary care. Br. J. Cancer 2022, 126, 948–956. [Google Scholar] [CrossRef] [PubMed]
- Spencer, K.; Jones, C.M.; Girdler, R.; Roe, C.; Sharpe, M.; Lawton, S.; Miller, L.; Lewis, P.; Evans, M.; Sebag-Montefiore, D.; et al. The impact of the COVID-19 pandemic on radiotherapy services in England, UK: A population-based study. Lancet Oncol. 2021, 22, 309–320. [Google Scholar] [CrossRef] [PubMed]
- Fotopoulou, C.; Khan, T.; Bracinik, J.; Glasbey, J.; Abu-Rustum, N.; Chiva, L.; Fagotti, A.; Fujiwara, K.; Ghebre, R.; Gutelkin, M.; et al. Outcomes of gynecologic cancer surgery during the COVID-19 pandemic: An international, multicenter, prospective CovidSurg-Gynecologic Oncology Cancer study. Am. J. Obstet. Gynecol. 2022, 227, 735.e1–735.e25. [Google Scholar] [CrossRef]
- Gaba, F.; Blyuss, O.; Rodriguez, I.; Dilley, J.; Wan, Y.L.; Saiz, A.; Razumova, Z.; Zalewski, K.; Nikolova, T.; Selcuk, I.; et al. Impact of SARS-CoV-2 on training and mental well-being of surgical gynecological oncology trainees. Int. J. Gynecol. Cancer 2021, 31, 1268–1277. [Google Scholar] [CrossRef]
- Carr, C.; Layne, T.; Tomita, S.; Wang, K.; Saleh, M.; Zeligs, K.; Papatla, K.; Prasad-Hayes, M.; Blank, S. We Can’t Just Wait This Out: Burnout and Fulfillment among SGO Members over the First Two Waves of the COVID-19 Pandemic (051). Gynecol. Oncol. 2022, 166, S34–S35. [Google Scholar] [CrossRef]
- Burki, T.K. Burnout among cancer professionals during COVID-19. Lancet Oncol. 2020, 21, 1402. [Google Scholar] [CrossRef]
- Burns, M.L.; Saager, L.; Cassidy, R.B.; Mentz, G.; Mashour, G.A.; Kheterpal, S. Association of anesthesiologist staffing ratio with surgical patient morbidity and mortality. JAMA Surg. 2022, 157, 807–815. [Google Scholar] [CrossRef]
- Needleman, J.; Buerhaus, P.; Pankratz, V.S.; Leibson, C.L.; Stevens, S.R.; Harris, M. Nurse staffing and inpatient hospital mortality. N. Engl. J. Med. 2011, 364, 1037–1045. [Google Scholar] [CrossRef] [Green Version]
- Wild, J.; McKinnon, A.; Wilkins, A.; Browne, H. Post-traumatic stress disorder and major depression among frontline healthcare staff working during the COVID-19 pandemic. Br. J. Clin. Psychol. 2022, 61, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Sirois, F.M.; Owens, J. Factors associated with psychological distress in health-care workers during an infectious disease outbreak: A rapid systematic review of the evidence. Front. Psychiatry 2021, 11, 589545. [Google Scholar] [CrossRef]
- Hlubocky, F.J.; Taylor, L.P.; Marron, J.M.; Spence, R.A.; McGinnis, M.M.; Brown, R.F.; McFarland, D.C.; Tetzlaff, E.D.; Gallagher, C.M.; Rosenberg, A.R. A call to action: Ethics committee roundtable recommendations for addressing burnout and moral distress in oncology. JCO Oncol. Pract. 2020, 16, 191–199. [Google Scholar] [CrossRef] [PubMed]
- BGCS. BGCS Workforce Survey 2022. Available online: https://www.bgcs.org.uk/wp-content/uploads/2022/11/BGCS-Workforce-Summary.pdf (accessed on 2 November 2022).
- Wood, E.; King, R.; Senek, M.; Robertson, S.; Taylor, B.; Tod, A.; Ryan, A. UK advanced practice nurses’ experiences of the COVID-19 pandemic: A mixed-methods cross-sectional study. BMJ Open 2021, 11, e044139. [Google Scholar] [CrossRef]
- Glasbey, J.C.; Nepogodiev, D.; Simoes, J.F.F.; Omar, O.; Li, E.; Venn, M.L.; Pgdme; Abou Chaar, M.K.; Capizzi, V.; Chaudhry, D.; et al. Elective Cancer Surgery in COVID-19-Free Surgical Pathways During the SARS-CoV-2 Pandemic: An International, Multicenter, Comparative Cohort Study. J. Clin. Oncol. 2021, 39, 66–78. [Google Scholar] [CrossRef] [PubMed]
- Fox, L.; Monroy-Iglesias, M.J.; Aggarwal, A.; Haire, K.; Purushotham, A.; Spicer, J.; Papa, S.; Rigg, A.; Dolly, S.; Sullivan, R.; et al. Association between COVID-19 burden and delays to diagnosis and treatment of cancer patients in England. J. Cancer Policy 2022, 31, 100316. [Google Scholar] [CrossRef] [PubMed]
- Purushotham, A.; Roberts, G.; Haire, K.; Dodkins, J.; Harvey-Jones, E.; Han, L.; Rigg, A.; Twinn, C.; Pramesh, C.; Ranganathan, P.; et al. The impact of national non-pharmaceutical interventions (‘lockdowns’) on the presentation of cancer patients. Ecancermedicalscience 2021, 15, 1180. [Google Scholar] [CrossRef]
- BGCS. British Gynaecological Cancer Society Recommendations for Management of Women with Gynaecological Cancer Who Have Received Non-Standard Care during the COVID-19 Pandemic. Available online: https://www.bgcs.org.uk/wp-content/uploads/2021/07/BGCS-Website-Post-Covid-Recommendations_July-2021.pdf (accessed on 14 July 2022).
| Hospitals with Significant Staffing Reduction | All | Units | Centres | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Survey 1 | 25/51 (49%) | 8/19 (42%) | 17/32 (53%) | ||||||
| Survey 2 | 7/42 (17%) | 0/13 (0%) | 7/29 (24%) | ||||||
| Survey 3 | 17/39 (44%) | 5/9 (56%) | 12/30 (40%) | ||||||
| Staff Category | Number of Hospitals Reporting Staff Reduction Due to COVID-19- Related Sickness 1 | Number of Hospitals Reporting Staff Reduction Due to Redeployment 2 | Proportion of Staff Reduction in Affected Hospitals (%) 3 | Number of Hospitals Reporting Staff Reduction Due to COVID-19-Related Sickness 1 | Number of Hospitals Reporting Staff Reduction Due to Redeployment 2 | Proportion of Staff Reduction in Affected Hospitals (%)3 | Number of Hospitals Reporting Staff Reduction Due to COVID-19-Related Sickness 1 | Number of Hospitals Reporting Staff Reduction Due to Redeployment 2 | Proportion of Staff Reduction in Affected hospitals (%) 3 |
| Non-subspecialty trainee doctor staff numbers | |||||||||
| Survey 1 | 14/25 (56%) | 14/25 (56%) | 40% (25–100) [1] | 5/8 (62%) | 4/8 (50%) | 30% (25–40) [1] | 9/17 (53%) | 10/17 (59%) | 45% (24–100) [0] |
| Survey 2 | 4/7 (57%) | 4/7 (57%) | 25% (5–75%) | 4/7 (57%) | 4/7 (57%) | 25% (5–75%) | |||
| Survey 3 | 15/39 (38%) | 2/39 (5%) | 25% (5–35%) | 5/9 (56%) | 1/9 (11%) | 25% (25–35%) | 10/30 (33%) | 1/30 (3%) | 30% (5–30%) |
| Gynaecological oncology subspecialty trainee numbers (hospitals where applicable) | |||||||||
| Survey 1 | 2/25 (8%) | 6/25 (24%) | 100% (100–100) [0] | 0/8 (0%) | 1/8 (12%) | 30% (30–30) [0] | 2/17 (12%) | 5/17 (29%) | 100% (100–100) [0] |
| Survey 2 | 1/7 (14%) | 0/7 (0%) | 45% | 1/7 (14%) | 0/7 (0%) | 45% | |||
| Survey 3 | 7/39 (18%) | 1/39 (3%) | 0% (0–35%) | 3/9 (33%) | 1/9 (11%) | 15% (8–50%) | 4/30 (13%) | 0/30 (0%) | 0% (0–15%) |
| Consultant staff numbers | |||||||||
| Survey 1 | 17/25 (68%) | 2/25 (8%) | 28% (20–38) [1] | 6/8 (75%) | 0/8 (0%) | 30% (30–33) [1] | 11/17 (65%) | 2/17 (12%) | 25% (20–50) [0] |
| Survey 2 | 5/7 (71%) | 0/7 (0%) | 5% (5–25%) | 5/7 (71%) | 0/7 (0%) | 5% (5–25%) | |||
| Survey 3 | 9/39 (23%) | 1/39 (3%) | 15% (3–30%) | 4/9 (44%) | 0/9 (0%) | 15% (5–15%) | 5/30 (17%) | 1/30 (3%) | 10% (3–30%) |
| Clinical nurse specialist staff numbers | |||||||||
| Survey 1 | 9/25 (36%) | 14/25 (56%) | 30% (20–50) [2] | 4/8 (50%) | 6/8 (75%) | 40% (20–50) [2] | 5/17 (29%) | 8/17 (47%) | 30% (20–50) [0] |
| Survey 2 | 3/7 (43%) | 3/7 (43%) | 35% (25–45%) | 3/7 (43%) | 3/7 (43%) | 35% (25–45%) | |||
| Survey 3 | 9/39 (23%) | 1/39 (3%) | 15% (0–30%) | 4/9 (44%) | 0/9 (0%) | 50% (20–80%) | 5/30 (17%) | 1/30 (3%) | 10% (0–30%) |
| Survey 1 | Survey 2 | Survey 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| All | Unit | Centre | All | Unit | Centre | All | Unit | Centre | |
| (a) MDT meeting functioning | |||||||||
| Change to MDT functioning | 51/51 (100%) | 19/19 (100%) | 32/32 (100%) | 35/42 (83%) | 10/13 (77%) | 25/29 (87%) | 33/39 (85%) | 6/9 (66%) | 27/30 (90%) |
| Moved to virtual meetings | 20/51 (39%) | 5/19 (26%) | 15/32 (47%) | 16/42 (38%) | 6/13 (46%) | 10/29 (34%) | 17/39 (44%) | 5/9 (56%) | 12/30 (40%) |
| Mixed virtual/F2F meetings | 33/51 (65%) | 13/19 (68%) | 20/32 (62%) | 21/42 (50%) | 5/13 (38%) | 16/29 (55%) | 18/39 (46%) | 1/9 (11%) | 17/30 (57%) |
| Reduced meeting frequency | 0/51 (0%) | 0/19 (0%) | 0/32 (0%) | ||||||
| Meetings Suspended | 0/51 (0%) | 0/19 (0%) | 0/32 (0%) | ||||||
| Meetings Less Attended | 21/51 (41%) | 6/19 (32%) | 15/32 (47%) | 7/42 (17%) | 2/13 (15%) | 5/29 (17%) | 5/39 (13%) | 1/9 (11%) | 4/30 (13%) |
| % reduction * | 40% (17–50) [2] | 50% (16–52) [1] | 25% (20–40) [1] | 25% (5–35) | 25% (25–25) | 25% (5–60) | 25% (25–25) | 25% (25–25) | 25% (25–40) |
| % of remote consultations * | 75% (50–88) [2] | 75% (50–85) [0] | 74% (50–87) [2] | 25% (5–35) [1] | 15% (5–35) | 25% (10–45) [1] | 0% (0–25) | 0% (0–15) | 0% (0–25) |
| (b) Capacity reductions in services * | |||||||||
| Theatre time | 40% (20–70) [6] | 60% (32–88) [1] | 30% (12–55) | 10% (0–25) | 15% (0–35) | 5% (0–25) | 0% (0–5) | 0% (0–30) | 0% (0–0) |
| Surgical cases postponed | 30% (16–57) [9] | 35% (16–72) [3] | 30% (16–50) [6] | 5% (0–15) | 5% (5–15) | 5%(0–15) | 5% (0–5) | 5% (5–15) | 5% (0–5) |
| Medical-oncology | 0% (0–0) [28] | 0% (0–0) [9] | 0% (0–13) [19] | 0% (0–5) [7] | 5% (0–25) [2] | 0% (0–5) | 0% (0–5) [4] | 0% (0–3) [2] | 0% (0–5) [2] |
| Clinical-oncology | 0% (0–8) [27] | 0% (0–0) [8] | 0% (0–10) [19] | 0% (0–5) [8] | 0% (0–5) [2] | 0% (0–5) [6] | 0% (0–5) [3] | 3% (0–5) [1] | 0% (0–3) [2] |
| Radiology | 0% (0–10) [19] | 0% (0–0) [6] | 0% (0–18) [13] | 0% (0–5) [4] | 3% (0–5) [1] | 0% (0–5) [3] | 0% (0–10) [4] | 3% (0–15) [1] | 0% (0–10) [3] |
| Pathology | 0% (0–0) [15] | 0% (0–0) [4] | 0% (0–0) [11] | 0% (0–5) [2] | 0% (0–5) | 0% (0–5) [2] | 0% (0–15) [2] | 0% (0–15) | 0% (0–30) [2] |
| Palliative care | 0% (0–0) [28] | 0% (0–0) [11] | 0% (0–0) [17] | 0% (0–5) [1] | 0% (0–5) | 0% (0–0) [1] | 0% (0–0) [4] | 0% (0–3) | 0% (0–0) [4] |
| Urgent referrals | 50% (25–70) [10] | 45% (18–62) [3] | 50% (30–70) [7] | 0% (0–15) [2] | 0% (0–5%) | 0% (0–15) [2] | 0% (0–3) [3] | 0% (0–3) | 0% (0–10%) [3] |
| Weekly MDT meeting list | 22% (2–48) | 20% (0–30) [1] | 28% (14–50) [4] | 0% (0–0) | 0% (0–0) | 0% (0–3%) | 0% (0–0) | 0% (0–0) | 0% (0–0) |
| (c) Move of activity off-site (another hospital) | |||||||||
| Moved operation lists | 23/41 (56%) | 9/19 (47%) | 14/22 (64%) | 17/42 (40%) | 5/13 (38%) | 12/29 (41%) | 4/39 (10%) | 1/9 (11%) | 3/30 (10%) |
| Moved clinic | 6/40 (15%) | 2/19 (11%) | 4/21 (19%) | 2/42 (5%) | 1/13 (8%) | 1/29 (3%) | 1/39 (3%) | 0/9 (0%) | 1/30 (3%) |
| Not yet moved | 3/29 (10%) | 2/16 (12%) | 1/13 (8%) | 0/32 (0%) | 0/6 (0%) | 0/26 (0%) | 1/39 (3%) | 1/9 (11%) | 0/30 (0%) |
| Central hub for surgical cases | 15/39 (38%) | 5/18 (28%) | 10/21 (48%) | 14/37 (38%) | 5/10 (50%) | 9/27 (33%) | 5/39 (13%) | 1/9 (11%) | 4/30 (13%) |
| MAS undertaken | 30/41 (73%) | 11/19 (58%) | 19/22 (86%) | 41/41 (100%) | 13/13 (100%) | 28/28 (100%) [1] | 39/39 (100%) | 9/9 (100%) | 30/30 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oxley, S.; Kalra, A.; Sideris, M.; Itzkowitz, N.; Evans, O.; Atakpa, E.C.; Brentnall, A.R.; Dworschak, N.; Gaba, F.; Gabe, R.; et al. Impact of Multiple COVID-19 Waves on Gynaecological Cancer Services in the UK. Cancers 2023, 15, 1273. https://doi.org/10.3390/cancers15041273
Oxley S, Kalra A, Sideris M, Itzkowitz N, Evans O, Atakpa EC, Brentnall AR, Dworschak N, Gaba F, Gabe R, et al. Impact of Multiple COVID-19 Waves on Gynaecological Cancer Services in the UK. Cancers. 2023; 15(4):1273. https://doi.org/10.3390/cancers15041273
Chicago/Turabian StyleOxley, Samuel, Ashwin Kalra, Michail Sideris, Nicole Itzkowitz, Olivia Evans, Emma Christine Atakpa, Adam R. Brentnall, Nina Dworschak, Faiza Gaba, Rhian Gabe, and et al. 2023. "Impact of Multiple COVID-19 Waves on Gynaecological Cancer Services in the UK" Cancers 15, no. 4: 1273. https://doi.org/10.3390/cancers15041273







