Blood–Brain Barrier Conquest in Glioblastoma Nanomedicine: Strategies, Clinical Advances, and Emerging Challenges
Abstract
:Simple Summary
Abstract
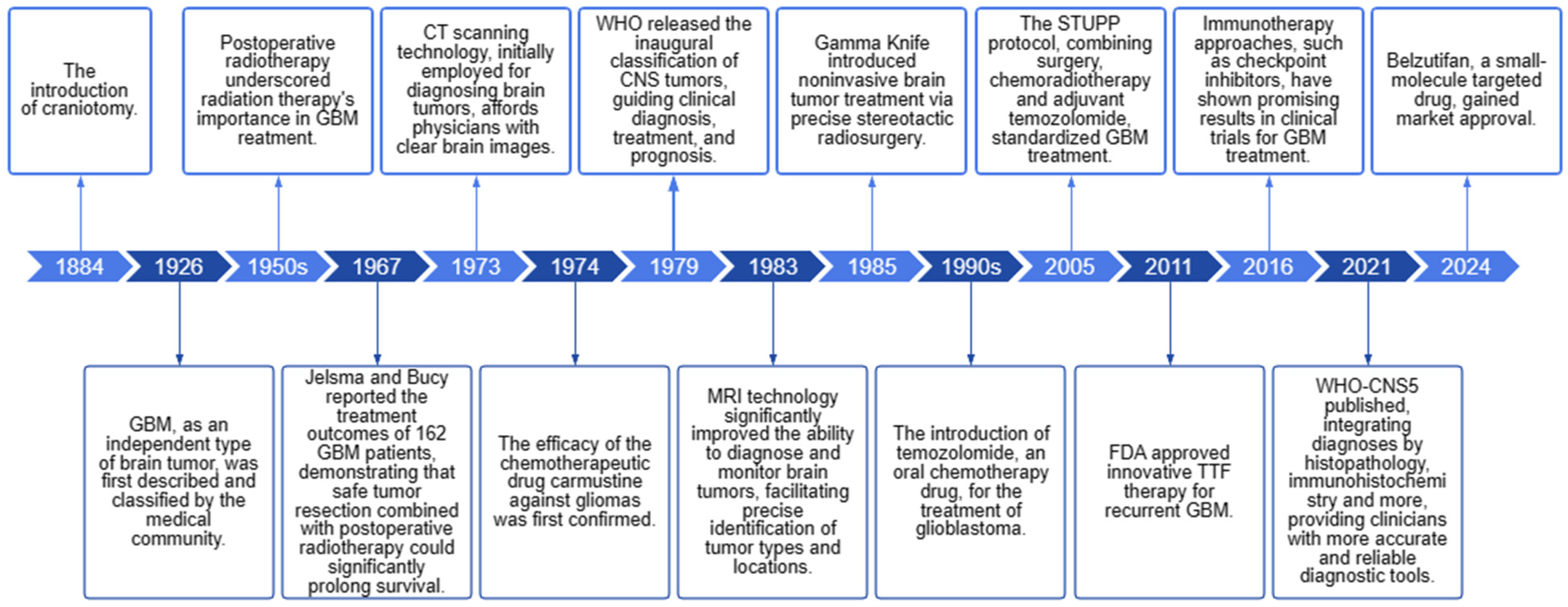
1. Introduction
2. NDDS Strategies for Crossing the BBB
2.1. Receptor-Mediated Transport
2.1.1. Transferrin and Lactoferrin Receptors
2.1.2. Acetylcholine Receptors
2.1.3. Folate Receptors
2.1.4. Low-Density Lipoprotein Receptors
2.1.5. Epidermal Growth Factor Receptors
2.1.6. Human Insulin-like Growth Factor-1 Receptors
2.1.7. Integrins
2.1.8. CD13
2.1.9. Neuropilin-1
2.1.10. Heat Shock Protein 70
2.2. Transporter-Mediated Transport
2.2.1. Glucose Transporters
2.2.2. Choline Transporters
2.2.3. Amino Acid Transporters
2.2.4. Vitamin Transporters
2.2.5. Organic Cation Transporters
2.2.6. Organic Anion Transporters
2.2.7. Monocarboxylate Transporters
2.3. Adsorptive-Mediated Transport
2.3.1. Cationic Albumin
2.3.2. Cell-Penetrating Peptides
2.4. Cell-Mediated Transport
2.4.1. Erythrocytes
2.4.2. Leukocytes
2.4.3. Stem Cells
2.5. Passive Diffusion
3. Alternative NDDS Strategies to Bypass the BBB
3.1. Intranasal Administration
3.2. Convection-Enhanced Delivery
3.3. Intracavitary/Intrathecal Drug Administration
4. Progress in Clinical Trials
5. Technical Challenges and New Strategies
- (1)
- The “physical barrier”: This barrier encompasses the anatomical and functional features of BBB endothelial cells, forming a vital anatomical gateway for targeted brain drug delivery. The lipid bilayer membranes of these cells exhibit lipophilicity and host receptors, carrier proteins, and other components that regulate molecular trafficking from the bloodstream to the brain tissue. High-molecular-weight drugs (>500 daltons) often fail to traverse this barrier [139]. The tight and adherens junctions between endothelial cells maintain the BBB’s integrity, preventing unrestricted substance exchange;
- (2)
- The “transportation barrier”: Functionally, the surfaces of BBB endothelial cells are negatively charged, impeding negatively charged compounds from entering neurons. Endothelial membranes express specific transporters that regulate substrate influx/efflux, preventing unauthorized bloodstream substances from crossing [141]. Pericytes and astrocytes encapsulate BBB endothelial cells, creating resistance that allows only small molecules (e.g., water, gases, lipids) to diffuse passively. Large, charged, polar, hydrophilic molecules (amino acids, glucose, drugs) rely on luminal membrane transport proteins/receptors [137]. ATP-driven efflux pumps (P-glycoprotein) limit toxin/drug permeability, reducing CNS exposure [103,142], impacting drug efficacy, exacerbating side effects, and challenging the drug action in brain tissue;
- (3)
- The “metabolic barrier”: Various drug-metabolizing enzymes, such as CYP450 enzymes, have been documented within the endothelial cells of the brain [103];
- (4)
- The “immune barrier”: Neurovascular units, comprising pericytes and astrocytes, regulate tight junctions, waste clearance, the vascular function, and neuroimmune responses, forming an “immune barrier” that constitutes the BBB.
6. Conclusions and Perspectives
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ostrom, Q.T.; Price, M.; Neff, C.; Cioffi, G.; Waite, K.A.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2016–2020. Neuro Oncol. 2023, 25 (Suppl. S2), iv1–iv99. [Google Scholar] [CrossRef] [PubMed]
- Liang, T.; Gu, L.; Kang, X.; Li, J.; Song, Y.; Wang, Y.; Ma, W. Programmed cell death disrupts inflammatory tumor microenvironment (TME) and promotes glioblastoma evolution. Cell Commun. Signal. 2024, 22, 333. [Google Scholar] [CrossRef]
- Horbinski, C.; Berger, T.; Packer, R.J.; Wen, P.Y. Clinical implications of the 2021 edition of the WHO classification of central nervous system tumours. Nat. Rev. Neurol. 2022, 18, 515–529. [Google Scholar] [CrossRef]
- Smerdi, D.; Moutafi, M.; Kotsantis, I.; Stavrinou, L.C.; Psyrri, A. Overcoming Resistance to Temozolomide in Glioblastoma: A Scoping Review of Preclinical and Clinical Data. Life 2024, 14, 673. [Google Scholar] [CrossRef]
- Banks, W.A. From blood-brain barrier to blood-brain interface: New opportunities for CNS drug delivery. Nat. Rev. Drug Discov. 2016, 15, 275–292. [Google Scholar] [CrossRef] [PubMed]
- Pardridge, W.M. Blood-brain barrier delivery. Drug Discov. Today 2007, 12, 54–61. [Google Scholar] [CrossRef]
- Pardridge, W.M. The blood-brain barrier: Bottleneck in brain drug development. NeuroRx 2005, 2, 3–14. [Google Scholar] [CrossRef]
- Tiwari, S.B.; Amiji, M.M. A review of nanocarrier-based CNS delivery systems. Curr. Drug Deliv. 2006, 3, 219–232. [Google Scholar] [CrossRef]
- Quader, S.; Kataoka, K.; Cabral, H. Nanomedicine for brain cancer. Adv. Drug Deliv. Rev. 2022, 182, 114115. [Google Scholar] [CrossRef]
- Song, X.; Qian, H.; Yu, Y. Nanoparticles Mediated the Diagnosis and Therapy of Glioblastoma: Bypass or Cross the Blood-Brain Barrier. Small 2023, 19, e2302613. [Google Scholar] [CrossRef]
- Khan, I.; Baig, M.H.; Mahfooz, S.; Imran, M.A.; Khan, M.I.; Dong, J.-J.; Cho, J.Y.; Hatiboglu, M.A. Nanomedicine for glioblastoma: Progress and future prospects. Semin. Cancer Biol. 2022, 86 Pt 2, 172–186. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Mu, N.; Jia, B.; Guo, Q.; Pan, L.; Zhu, M.; Zhang, W.; Zhang, K.; Li, W.; Li, M.; et al. Targeting radiation-tolerant persister cells as a strategy for inhibiting radioresistance and recurrence in glioblastoma. Neuro Oncol. 2022, 24, 1056–1070. [Google Scholar] [CrossRef] [PubMed]
- Lam, F.C.; Morton, S.W.; Wyckoff, J.; Han, T.-L.V.; Hwang, M.K.; Maffa, A.; Balkanska-Sinclair, E.; Yaffe, M.B.; Floyd, S.R.; Hammond, P.T. Enhanced efficacy of combined temozolomide and bromodomain inhibitor therapy for gliomas using targeted nanoparticles. Nat. Commun. 2018, 9, 1991. [Google Scholar] [CrossRef]
- Ji, B.; Maeda, J.; Higuchi, M.; Inoue, K.; Akita, H.; Harashima, H.; Suhara, T. Pharmacokinetics and brain uptake of lactoferrin in rats. Life Sci. 2006, 78, 851–855. [Google Scholar] [CrossRef]
- Dong, M.; Liu, Y.; Liu, B.; Peng, J.; Tang, Y.; Lu, G.; Shi, H.; Zhu, F. Enhanced anti-glioma efficacy of biodegradable periodic mesoporous organosilica nanoparticles through target delivery of chemotherapeutics. J. Mater. Sci. Mater. Med. 2023, 34, 48. [Google Scholar] [CrossRef]
- Janjua, T.I.; Cao, Y.; Ahmed-Cox, A.; Raza, A.; Moniruzzaman; Akhter, D.T.; Fletcher, N.L.; Kavallaris, M.; Thurecht, K.J.; Popat, A. Efficient delivery of Temozolomide using ultrasmall large-pore silica nanoparticles for glioblastoma. J. Control. Release 2023, 357, 161–174. [Google Scholar] [CrossRef]
- Chen, H.; Wang, Y.; Wang, H.; Zhang, K.; Liu, Y.; Li, Q.; Li, C.; Wen, Z.; Chen, Z. Biomimetic nanocarriers loaded with temozolomide by cloaking brain-targeting peptides for targeting drug delivery system to promote anticancer effects in glioblastoma cells. Heliyon 2024, 10, e28256. [Google Scholar] [CrossRef] [PubMed]
- Kuplennik, N.; Lang, K.; Steinfeld, R.; Sosnik, A. Folate Receptor α-Modified Nanoparticles for Targeting of the Central Nervous System. ACS Appl. Mater. Interfaces 2019, 11, 39633–39647. [Google Scholar] [CrossRef]
- Zhong, X.; Wei, G.; Liu, B.; Wang, C.; Wang, J.; Lu, Y.; Cui, W.; Guo, H. Polyhedral Oligomeric Silsesquioxane-Based Nanoparticles for Efficient Chemotherapy of Glioblastoma. Small 2023, 19, e2207248. [Google Scholar] [CrossRef] [PubMed]
- Neves, A.R.; Queiroz, J.F.; Weksler, B.; Romero, I.A.; Couraud, P.-O.; Reis, S. Solid lipid nanoparticles as a vehicle for brain-targeted drug delivery: Two new strategies of functionalization with apolipoprotein E. Nanotechnology 2015, 26, 495103. [Google Scholar] [CrossRef]
- Liang, J.; Li, L.; Tian, H.; Wang, Z.; Liu, G.; Duan, X.; Guo, M.; Liu, J.; Zhang, W.; Nice, E.C.; et al. Drug Repurposing-Based Brain-Targeting Self-Assembly Nanoplatform Using Enhanced Ferroptosis against Glioblastoma. Small 2023, 19, e2303073. [Google Scholar] [CrossRef] [PubMed]
- Thirumurugan, S.; Dash, P.; Liu, X.; Tseng, Y.-Y.; Huang, W.-J.; Li, Y.; Zhao, G.; Lin, C.; Murugan, K.; Dhawan, U.; et al. Angiopep-2-decorated titanium-alloy core-shell magnetic nanoparticles for nanotheranostics and medical imaging. Nanoscale 2022, 14, 14789–14800. [Google Scholar] [CrossRef] [PubMed]
- He, C.; Zhang, Z.; Ding, Y.; Xue, K.; Wang, X.; Yang, R.; An, Y.; Liu, D.; Hu, C.; Tang, Q. LRP1-mediated pH-sensitive polymersomes facilitate combination therapy of glioblastoma in vitro and in vivo. J. Nanobiotechnol. 2021, 19, 29. [Google Scholar] [CrossRef] [PubMed]
- Tashima, T. Brain Cancer Chemotherapy through a Delivery System across the Blood-Brain Barrier into the Brain Based on Receptor-Mediated Transcytosis Using Monoclonal Antibody Conjugates. Biomedicines 2022, 10, 1597. [Google Scholar] [CrossRef] [PubMed]
- Banstola, A.; Duwa, R.; Emami, F.; Jeong, J.H.; Yook, S. Enhanced Caspase-Mediated Abrogation of Autophagy by Temozolomide-Loaded and Panitumumab-Conjugated Poly(lactic-co-glycolic acid) Nanoparticles in Epidermal Growth Factor Receptor Overexpressing Glioblastoma Cells. Mol. Pharm. 2020, 17, 4386–4400. [Google Scholar] [CrossRef] [PubMed]
- Alata, W.; Yogi, A.; Brunette, E.; Delaney, C.E.; Faassen, H.; Hussack, G.; Iqbal, U.; Kemmerich, K.; Haqqani, A.S.; Moreno, M.J.; et al. Targeting insulin-like growth factor-1 receptor (IGF1R) for brain delivery of biologics. Faseb J. 2022, 36, e22208. [Google Scholar] [CrossRef]
- Yogi, A.; Hussack, G.; van Faassen, H.; Haqqani, A.S.; Delaney, C.E.; Brunette, E.; Sandhu, J.K.; Hewitt, M.; Sulea, T.; Kemmerich, K.; et al. Brain Delivery of IGF1R5, a Single-Domain Antibody Targeting Insulin-like Growth Factor-1 Receptor. Pharmaceutics 2022, 14, 1452. [Google Scholar] [CrossRef]
- Miura, Y.; Takenaka, T.; Toh, K.; Wu, S.; Nishihara, H.; Kano, M.R.; Ino, Y.; Nomoto, T.; Matsumoto, Y.; Koyama, H.; et al. Cyclic RGD-linked polymeric micelles for targeted delivery of platinum anticancer drugs to glioblastoma through the blood-brain tumor barrier. ACS Nano 2013, 7, 8583–8592. [Google Scholar] [CrossRef]
- Quader, S.; Liu, X.; Chen, Y.; Mi, P.; Chida, T.; Ishii, T.; Miura, Y.; Nishiyama, N.; Cabral, H.; Kataoka, K. cRGD peptide-installed epirubicin-loaded polymeric micelles for effective targeted therapy against brain tumors. J. Control. Release 2017, 258, 56–66. [Google Scholar] [CrossRef]
- Vangala, V.; Nimmu, N.V.; Khalid, S.; Kuncha, M.; Sistla, R.; Banerjee, R.; Chaudhuri, A. Combating Glioblastoma by Codelivering the Small-Molecule Inhibitor of STAT3 and STAT3siRNA with α5β1 Integrin Receptor-Selective Liposomes. Mol. Pharm. 2020, 17, 1859–1874. [Google Scholar] [CrossRef]
- An, S.; Jiang, X.; Shi, J.; He, X.; Li, J.; Guo, Y.; Zhang, Y.; Ma, H.; Lu, Y.; Jiang, C. Single-component self-assembled RNAi nanoparticles functionalized with tumor-targeting iNGR delivering abundant siRNA for efficient glioma therapy. Biomaterials 2015, 53, 330–340. [Google Scholar] [CrossRef]
- Huang, N.; Cheng, S.; Zhang, X.; Tian, Q.; Pi, J.; Tang, J.; Huang, Q.; Wang, F.; Chen, J.; Xie, Z.; et al. Efficacy of NGR peptide-modified PEGylated quantum dots for crossing the blood-brain barrier and targeted fluorescence imaging of glioma and tumor vasculature. Nanomedicine 2017, 13, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lei, Y.; Xie, C.; Lu, W.; Wagner, E.; Xie, Z.; Gao, J.; Zhang, X.; Yan, Z.; Liu, M. Retro-inverso CendR peptide-mediated polyethyleneimine for intracranial glioblastoma-targeting gene therapy. Bioconjug. Chem. 2014, 25, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Zhao, X.; Fu, T.; Li, K.; He, Y.; Luo, Z.; Dai, L.; Zeng, R.; Cai, K. An iRGD-conjugated prodrug micelle with blood-brain-barrier penetrability for anti-glioma therapy. Biomaterials 2020, 230, 119666. [Google Scholar] [CrossRef]
- Xie, R.; Wang, Y.; Tong, F.; Yang, W.; Lei, T.; Du, Y.; Wang, X.; Yang, Z.; Gong, T.; Shevtsov, M.; et al. Hsp70-Targeting and Size-Tunable Nanoparticles Combine with PD-1 Checkpoint Blockade to Treat Glioma. Small 2023, 19, e2300570. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Meng, N.; Lu, L.; Lu, J.; Wu, S.; Ding, Y.; Wu, S.; Bao, Y.; Xu, Q.; Chen, R.; et al. A novel peptide-drug conjugate for glioma-targeted drug delivery. J. Control. Release 2024, 369, 722–733. [Google Scholar] [CrossRef] [PubMed]
- Enerson, B.E.; Drewes, L.R. The rat blood-brain barrier transcriptome. J. Cereb. Blood Flow Metab. 2006, 26, 959–973. [Google Scholar] [CrossRef] [PubMed]
- Gyimesi, G.; Hediger, M.A. Transporter-Mediated Drug Delivery. Molecules 2023, 28, 1151. [Google Scholar] [CrossRef]
- Zhang, Y.; Ren, Y.; Xu, H.; Li, L.; Qian, F.; Wang, L.; Quan, A.; Ma, H.; Liu, H.; Yu, R. Cascade-Responsive 2-DG Nanocapsules Encapsulate aV-siCPT1C Conjugates to Inhibit Glioblastoma through Multiple Inhibition of Energy Metabolism. ACS Appl. Mater. Interfaces 2023, 15, 10356–10370. [Google Scholar] [CrossRef]
- Min, H.S.; Kim, H.J.; Naito, M.; Ogura, S.; Toh, K.; Hayashi, K.; Kim, B.S.; Fukushima, S.; Anraku, Y.; Miyata, K.; et al. Systemic Brain Delivery of Antisense Oligonucleotides across the Blood-Brain Barrier with a Glucose-Coated Polymeric Nanocarrier. Angew. Chem. Int. Ed. Engl. 2020, 59, 8173–8180. [Google Scholar] [CrossRef]
- Anraku, Y.; Kuwahara, H.; Fukusato, Y.; Mizoguchi, A.; Ishii, T.; Nitta, K.; Matsumoto, Y.; Toh, K.; Miyata, K.; Uchida, S.; et al. Glycaemic control boosts glucosylated nanocarrier crossing the BBB into the brain. Nat. Commun. 2017, 8, 1001. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wang, X.; Xie, C.; Zhang, M.; Ruan, H.; Wang, S.; Jiang, K.; Wang, F.; Zhan, C.; Lu, W.; et al. Nanodisk-based glioma-targeted drug delivery enabled by a stable glycopeptide. J. Control. Release 2018, 284, 26–38. [Google Scholar] [CrossRef]
- Li, J.; Zhou, L.; Ye, D.; Huang, S.; Shao, K.; Huang, R.; Han, L.; Liu, Y.; Liu, S.; Ye, L.; et al. Choline-derivate-modified nanoparticles for brain-targeting gene delivery. Adv. Mater. 2011, 23, 4516–4520. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Guo, Y.; Kuang, Y.; An, S.; Ma, H.; Jiang, C. Choline transporter-targeting and co-delivery system for glioma therapy. Biomaterials 2013, 34, 9142–9148. [Google Scholar] [CrossRef]
- Jin, W.; Wu, Y.; Chen, N.; Wang, Q.; Wang, Y.; Li, Y.; Li, S.; Han, X.; Yang, E.; Tong, F.; et al. Early administration of MPC-n(IVIg) selectively accumulates in ischemic areas to protect inflammation-induced brain damage from ischemic stroke. Theranostics 2021, 11, 8197–8217. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Chao, Y.; Zhao, H.; Zhou, X.; Zhang, F.; Zhang, Z.; Li, Z.; Pan, J.; Wang, J.; Chen, Q.; et al. Smart Nanomedicine to Enable Crossing Blood-Brain Barrier Delivery of Checkpoint Blockade Antibody for Immunotherapy of Glioma. ACS Nano 2022, 16, 664–674. [Google Scholar] [CrossRef]
- Puris, E.; Gynther, M.; Auriola, S.; Huttunen, K.M. L-Type amino acid transporter 1 as a target for drug delivery. Pharm. Res. 2020, 37, 88. [Google Scholar] [CrossRef] [PubMed]
- Montaser, A.B.; Järvinen, J.; Löffler, S.; Huttunen, J.; Auriola, S.; Lehtonen, M.; Jalkanen, A.; Huttunen, K.M. L-Type Amino Acid Transporter 1 Enables the Efficient Brain Delivery of Small-Sized Prodrug across the Blood-Brain Barrier and into Human and Mouse Brain Parenchymal Cells. ACS Chem. Neurosci. 2020, 11, 4301–4315. [Google Scholar] [CrossRef]
- Wei, Z.Y.; Feng, M.M.; Yang, B.; Yan, Z.Y.; Wang, B.Q.; Bu, X.Y. Methylmercury-l-Cysteine targeting L-type amino acid transporter conjugate cytotoxicity on C6 glioma cells. J. Biol. Regul. Homeost. Agents 2018, 32, 147–151. [Google Scholar]
- Bhunia, S.; Vangala, V.; Bhattacharya, D.; Ravuri, H.G.; Kuncha, M.; Chakravarty, S.; Sistla, R.; Chaudhuri, A. Large Amino Acid Transporter 1 Selective Liposomes of l-DOPA Functionalized Amphiphile for Combating Glioblastoma. Mol. Pharm. 2017, 14, 3834–3847. [Google Scholar] [CrossRef]
- Salmaso, S.; Pappalardo, J.S.; Sawant, R.R.; Musacchio, T.; Rockwell, K.; Caliceti, P.; Torchilin, V.P. Targeting glioma cells in vitro with ascorbate-conjugated pharmaceutical nanocarriers. Bioconjug. Chem. 2009, 20, 2348–2355. [Google Scholar] [CrossRef] [PubMed]
- Quéléver, G.; Kachidian, P.; Melon, C.; Garino, C.; Laras, Y.; Pietrancosta, N.; Shehac, M.; Kraus, J.L. Enhanced delivery of gamma-secretase inhibitor DAPT into the brain via an ascorbic acid mediated strategy. Org. Biomol. Chem. 2005, 3, 2450–2457. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Zhao, Y.; Chen, Y.; Yang, Z.; Zhang, L.; Xiao, W.; Yang, J.; Guo, L.; Wu, Y. Dual-targeting for brain-specific liposomes drug delivery system: Synthesis and preliminary evaluation. Bioorg. Med. Chem. 2018, 26, 4677–4686. [Google Scholar] [CrossRef] [PubMed]
- Kou, L.; Sun, R.; Ganapathy, V.; Yao, Q.; Chen, R. Recent advances in drug delivery via the organic cation/carnitine transporter 2 (OCTN2/SLC22A5). Expert Opin. Ther. Targets 2018, 22, 715–726. [Google Scholar] [CrossRef]
- Fink, M.A.; Paland, H.; Herzog, S.; Grube, M.; Vogelgesang, S.; Weitmann, K.; Bialke, A.; Hoffmann, W.; Rauch, B.H.; Schroeder, H.W.S.; et al. L-Carnitine-Mediated Tumor Cell Protection and Poor Patient Survival Associated with OCTN2 Overexpression in Glioblastoma Multiforme. Clin. Cancer Res. 2019, 25, 2874–2886. [Google Scholar] [CrossRef] [PubMed]
- Kou, L.; Hou, Y.; Yao, Q.; Guo, W.; Wang, G.; Wang, M.; Fu, Q.; He, Z.; Ganapathy, V.; Sun, J. L-Carnitine-conjugated nanoparticles to promote permeation across blood-brain barrier and to target glioma cells for drug delivery via the novel organic cation/carnitine transporter OCTN2. Artif. Cells Nanomed. Biotechnol. 2018, 46, 1605–1616. [Google Scholar] [CrossRef]
- Bakos, É.; Német, O.; Patik, I.; Kucsma, N.; Várady, G.; Szakács, G.; Özvegy-Laczka, C. A novel fluorescence-based functional assay for human OATP1A2 and OATP1C1 identifies interaction between third-generation P-gp inhibitors and OATP1A2. FEBS J. 2020, 287, 2468–2485. [Google Scholar] [CrossRef]
- Baklaushev, V.P.; Nukolova, N.N.; Khalansky, A.S.; Gurina, O.I.; Yusubalieva, G.M.; Grinenko, N.P.; Gubskiy, I.L.; Melnikov, P.A.; Kardashova, K.S.; Kabanov, A.V.; et al. Treatment of glioma by cisplatin-loaded nanogels conjugated with monoclonal antibodies against Cx43 and BSAT1. Drug Deliv. 2015, 22, 276–285. [Google Scholar] [CrossRef]
- Higuchi, K.; Sivaprakasam, S.; Sennoune, S.R.; Ogura, J.; Bhutia, Y.D.; Rueda, R.; Pereira, S.L.; Ganapathy, V. A Proton-Coupled Transport System for β-Hydroxy-β-Methylbutyrate (HMB) in Blood-Brain Barrier Endothelial Cell Line hCMEC/D3. Nutrients 2021, 13, 3220. [Google Scholar] [CrossRef]
- Sadeghzadeh, M.; Wenzel, B.; Gündel, D.; Deuther-Conrad, W.; Toussaint, M.; Moldovan, R.-P.; Fischer, S.; Ludwig, F.-A.; Teodoro, R.; Jonnalagadda, S.; et al. Development of Novel Analogs of the Monocarboxylate Transporter Ligand FACH and Biological Validation of One Potential Radiotracer for Positron Emission Tomography (PET) Imaging. Molecules 2020, 25, 2309. [Google Scholar] [CrossRef]
- Huber, I.; Pandur, E.; Sipos, K.; Barna, L.; Harazin, A.; Deli, M.A.; Tyukodi, L.; Gulyás-Fekete, G.; Kulcsár, G.; Rozmer, Z. Novel cyclic C(5)-curcuminoids penetrating the blood-brain barrier: Design, synthesis and antiproliferative activity against astrocytoma and neuroblastoma cells. Eur. J. Pharm. Sci. 2022, 173, 106184. [Google Scholar] [CrossRef] [PubMed]
- Klibanov, A.L.; Maruyama, K.; Torchilin, V.P.; Huang, L. Amphipathic polyethyleneglycols effectively prolong the circulation time of liposomes. FEBS Lett. 1990, 268, 235–237. [Google Scholar] [CrossRef] [PubMed]
- Sim, T.M.; Tarini, D.; Dheen, S.T.; Bay, B.H.; Srinivasan, D.K. Nanoparticle-Based Technology Approaches to the Management of Neurological Disorders. Int. J. Mol. Sci. 2020, 21, 6070. [Google Scholar] [CrossRef] [PubMed]
- Herce, H.D.; Rajan, M.; Lättig-Tünnemann, G.; Fillies, M.; Cardoso, M.C. Cell-permeable nanobodies for targeted immunolabelling and antigen manipulation in living cells. Nat. Chem. 2017, 9, 762–771. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Wang, L.; Zhao, L.; Liao, J.; Zhao, C.; Xu, X.; Wang, F.; Zhang, X. A Novel Blood-Brain Barrier-Penetrating and Vascular-Targeting Chimeric Peptide Inhibits Glioma Angiogenesis. Int. J. Mol. Sci. 2023, 24, 8753. [Google Scholar] [CrossRef]
- Hervé, F.; Ghinea, N.; Scherrmann, J.M. CNS delivery via adsorptive transcytosis. AAPS J. 2008, 10, 455–472. [Google Scholar] [CrossRef]
- Lu, W.; Sun, Q.; Wan, J.; She, Z.; Jiang, X.-G. Cationic albumin-conjugated pegylated nanoparticles allow gene delivery into brain tumors via intravenous administration. Cancer Res. 2006, 66, 11878–11887. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, W.; Sun, Y.; Dong, X. Transthyretin-Penetratin: A Potent Fusion Protein Inhibitor against Alzheimer’s Amyloid-β Fibrillogenesis with High Blood Brain Barrier Crossing Capability. Bioconjug. Chem. 2024, 35, 419–431. [Google Scholar] [CrossRef]
- Zhang, Y.; Guo, P.; Ma, Z.; Lu, P.; Kebebe, D.; Liu, Z. Combination of cell-penetrating peptides with nanomaterials for the potential therapeutics of central nervous system disorders: A review. J. Nanobiotechnol. 2021, 19, 255. [Google Scholar] [CrossRef]
- Qin, Y.; Zhang, Q.; Chen, H.; Yuan, W.; Kuai, R.; Xie, F.; Zhang, L.; Wang, X.; Zhang, Z.; Liu, J.; et al. Comparison of four different peptides to enhance accumulation of liposomes into the brain. J. Drug Target. 2012, 20, 235–245. [Google Scholar] [CrossRef]
- Liu, L.; Guo, K.; Lu, J.; Venkatraman, S.S.; Luo, D.; Ng, K.C.; Ling, E.-A.; Moochhala, S.; Yang, Y.-Y. Biologically active core/shell nanoparticles self-assembled from cholesterol-terminated PEG-TAT for drug delivery across the blood-brain barrier. Biomaterials 2008, 29, 1509–1517. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Z.; Yu, Z.; Xu, T.; Wang, L.; Meng, N.; Jin, H.; Xu, B. Novel Nano-Drug Delivery System for Brain Tumor Treatment. Cells 2022, 11, 3761. [Google Scholar] [CrossRef] [PubMed]
- Ayer, M.; Klok, H.A. Cell-mediated delivery of synthetic nano- and microparticles. J. Control. Release 2017, 259, 92–104. [Google Scholar] [CrossRef] [PubMed]
- Choi, A.; Javius-Jones, K.; Hong, S.; Park, H. Cell-Based Drug Delivery Systems with Innate Homing Capability as a Novel Nanocarrier Platform. Int. J. Nanomed. 2023, 18, 509–525. [Google Scholar] [CrossRef]
- Xiao, T.; He, M.; Xu, F.; Fan, Y.; Jia, B.; Shen, M.; Wang, H.; Shi, X. Macrophage Membrane-Camouflaged Responsive Polymer Nanogels Enable Magnetic Resonance Imaging-Guided Chemotherapy/Chemodynamic Therapy of Orthotopic Glioma. ACS Nano 2021, 15, 20377–20390. [Google Scholar] [CrossRef] [PubMed]
- Stephan, M.T.; Irvine, D.J. Enhancing Cell therapies from the Outside In: Cell Surface Engineering Using Synthetic Nanomaterials. Nano Today 2011, 6, 309–325. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Yang, Z.; Li, F.; Xu, L.; Sun, Y. Cell-mediated targeting drugs delivery systems. Drug Deliv. 2020, 27, 1425–1437. [Google Scholar] [CrossRef] [PubMed]
- He, H.; Ye, J.; Wang, Y.; Liu, Q.; Chung, H.S.; Kwon, Y.M.; Shin, M.C.; Lee, K.; Yang, V.C. Cell-penetrating peptides meditated encapsulation of protein therapeutics into intact red blood cells and its application. J. Control. Release 2014, 176, 123–132. [Google Scholar] [CrossRef]
- Wu, H.; Ye, J.; Wang, Y.; Liu, Q.; Chung, H.S.; Kwon, Y.M.; Shin, M.C.; Lee, K.; Yang, V.C. Cell membrane-based biomimetic vehicles for effective central nervous system target delivery: Insights and challenges. J. Control. Release 2023, 360, 169–184. [Google Scholar] [CrossRef]
- Chai, Z.; Ran, D.; Lu, L.; Zhan, C.; Ruan, H.; Hu, X.; Xie, C.; Jiang, K.; Li, J.; Zhou, J.; et al. Ligand-Modified Cell Membrane Enables the Targeted Delivery of Drug Nanocrystals to Glioma. ACS Nano 2019, 13, 5591–5601. [Google Scholar] [CrossRef]
- Zou, Y.; Liu, Y.; Yang, Z.; Zhang, D.; Lu, Y.; Zheng, M.; Xue, X.; Geng, J.; Chung, R.; Shi, B. Effective and Targeted Human Orthotopic Glioblastoma Xenograft Therapy via a Multifunctional Biomimetic Nanomedicine. Adv. Mater. 2018, 30, e1803717. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Chen, Z.; Peng, Y.; Liu, C. IRGD-modified erythrocyte membrane biomimetic temozolomide nanodots for the treatment of glioblastoma. Nanotechnology 2024, 35, 245701. [Google Scholar] [CrossRef]
- Song, M.; Tian, J.; Wang, L.; Dong, S.; Fu, K.; Chen, S.; Liu, C. Efficient Delivery of Lomitapide using Hybrid Membrane-Coated Tetrahedral DNA Nanostructures for Glioblastoma Therapy. Adv. Mater. 2024, 36, e2311760. [Google Scholar] [CrossRef] [PubMed]
- Karp, J.M.; Teo, G.S.L. Mesenchymal stem cell homing: The devil is in the details. Cell Stem Cell 2009, 4, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Elmadany, N.; Alhalabi, O.T.; Platten, M.; Bunse, L. Site-Specific Considerations on Engineered T Cells for Malignant Gliomas. Biomedicines 2022, 10, 1738. [Google Scholar] [CrossRef]
- Wang, D.; Starr, R.; Chang, W.-C.; Aguilar, B.; Alizadeh, D.; Wright, S.L.; Yang, X.; Brito, A.; Sarkissian, A.; Ostberg, J.R.; et al. Chlorotoxin-directed CAR T cells for specific and effective targeting of glioblastoma. Sci. Transl. Med. 2020, 12, eaaw2672. [Google Scholar] [CrossRef]
- Sabbagh, A.; Beccaria, K.; Ling, X.; Marisetty, A.; Ott, M.; Caruso, H.; Barton, E.; Kong, L.-Y.; Fang, D.; Latha, K.; et al. Opening of the Blood-Brain Barrier Using Low-Intensity Pulsed Ultrasound Enhances Responses to Immunotherapy in Preclinical Glioma Models. Clin. Cancer Res. 2021, 27, 4325–4337. [Google Scholar] [CrossRef]
- Kim, G.B.; Aragon-Sanabria, V.; Randolph, L.; Jiang, H.; Reynolds, J.A.; Webb, B.S.; Madhankumar, A.; Lian, X.; Connor, J.R.; Yang, J.; et al. High-affinity mutant Interleukin-13 targeted CAR T cells enhance delivery of clickable biodegradable fluorescent nanoparticles to glioblastoma. Bioact. Mater. 2020, 5, 624–635. [Google Scholar] [CrossRef]
- Wang, J.; Tang, W.; Yang, M.; Yin, Y.; Li, H.; Hu, F.; Tang, L.; Ma, X.; Zhang, Y.; Wang, Y. Inflammatory tumor microenvironment responsive neutrophil exosomes-based drug delivery system for targeted glioma therapy. Biomaterials 2021, 273, 120784. [Google Scholar] [CrossRef]
- Chang, Y.; Cai, X.; Syahirah, R.; Yao, Y.; Xu, Y.; Jin, G.; Bhute, V.J.; Torregrosa-Allen, S.; Elzey, B.D.; Won, Y.-Y.; et al. CAR-neutrophil mediated delivery of tumor-microenvironment responsive nanodrugs for glioblastoma chemo-immunotherapy. Nat. Commun. 2023, 14, 2266. [Google Scholar] [CrossRef]
- Chen, H.; Ji, J.; Zhang, L.; Chen, T.; Zhang, Y.; Zhang, F.; Wang, J.; Ke, Y. Inflammatory responsive neutrophil-like membrane-based drug delivery system for post-surgical glioblastoma therapy. J. Control. Release 2023, 362, 479–488. [Google Scholar] [CrossRef] [PubMed]
- Tong, H.I.; Kang, W.; Shi, Y.; Zhou, G.; Lu, Y. Physiological function and inflamed-brain migration of mouse monocyte-derived macrophages following cellular uptake of superparamagnetic iron oxide nanoparticles-Implication of macrophage-based drug delivery into the central nervous system. Int. J. Pharm. 2016, 505, 271–282. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Xiang, Y.; Liu, S.; Zhang, Y.; Wan, J.; Ci, Z.; Cui, M.; Shen, L.; Li, N.; Guan, Y. Macrophage membrane modified baicalin liposomes improve brain targeting for alleviating cerebral ischemia reperfusion injury. Nanomedicine 2022, 43, 102547. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Kuang, L.; Yin, Y.; Tang, L.; Zhang, Y.; Fan, Q.; Wang, B.; Dong, Z.; Wang, W.; Yin, T.; et al. Tumor-Antigen Activated Dendritic Cell Membrane-Coated Biomimetic Nanoparticles with Orchestrating Immune Responses Promote Therapeutic Efficacy against Glioma. ACS Nano 2023, 17, 2341–2355. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.; Hu, J.; Belladonna, M.L.; Black, K.L.; Yu, J.S. Interleukin-23-expressing bone marrow-derived neural stem-like cells exhibit antitumor activity against intracranial glioma. Cancer Res. 2006, 66, 2630–2638. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Sun, S.; Dangelmajer, S.; Zhang, Q.; Wang, J.; Hu, F.; Dong, F.; Kahlert, U.D.; Zhu, M.; Lei, T. Exploiting tumor-intrinsic signals to induce mesenchymal stem cell-mediated suicide gene therapy to fight malignant glioma. Stem Cell Res. Ther. 2019, 10, 88. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Fitch, S.; Wang, C.; Wilson, C.; Li, J.; Grant, G.A.; Yang, F. Nanoparticle engineered TRAIL-overexpressing adipose-derived stem cells target and eradicate glioblastoma via intracranial delivery. Proc. Natl. Acad. Sci. USA 2016, 113, 13857–13862. [Google Scholar] [CrossRef]
- Mangraviti, A.; Tzeng, S.Y.; Gullotti, D.; Kozielski, K.L.; Kim, J.E.; Seng, M.; Abbadi, S.; Schiapparelli, P.; Sarabia-Estrada, R.; Vescovi, A.; et al. Non-virally engineered human adipose mesenchymal stem cells produce BMP4, target brain tumors, and extend survival. Biomaterials 2016, 100, 53–66. [Google Scholar] [CrossRef]
- Malik, Y.S.; Sheikh, M.A.; Xing, Z.; Guo, Z.; Zhu, X.; Tian, H.; Chen, X. Polylysine-modified polyethylenimine polymer can generate genetically engineered mesenchymal stem cells for combinational suicidal gene therapy in glioblastoma. Acta Biomater. 2018, 80, 144–153. [Google Scholar] [CrossRef]
- Mooney, R.; Weng, Y.; Tirughana-Sambandan, R.; Valenzuela, V.; Aramburo, S.; Garcia, E.; Li, Z.; Gutova, M.; Annala, A.J.; Berlin, J.M.; et al. Neural stem cells improve intracranial nanoparticle retention and tumor-selective distribution. Future Oncol. 2014, 10, 401–415. [Google Scholar] [CrossRef]
- Pavon, L.F.; Sibov, T.T.; de Souza, A.V.; da Cruz, E.F.; Malheiros, S.M.F.; Cabral, F.R.; de Souza, J.G.; Boufleur, P.; de Oliveira, D.M.; de Toledo, S.R.C.; et al. Tropism of mesenchymal stem cell toward CD133(+) stem cell of glioblastoma in vitro and promote tumor proliferation in vivo. Stem Cell Res. Ther. 2018, 9, 310. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Tu, M.; Kelly, R.S.; Chen, C.; Smith, B.J. Development of a computational approach to predict blood-brain barrier permeability. Drug Metab. Dispos. 2004, 32, 132–139. [Google Scholar] [CrossRef]
- Kadry, H.; Noorani, B.; Cucullo, L. A blood-brain barrier overview on structure, function, impairment, and biomarkers of integrity. Fluids Barriers CNS 2020, 17, 69. [Google Scholar] [CrossRef] [PubMed]
- Haumann, R.; Videira, J.C.; Kaspers, G.J.L.; van Vuurden, D.G.; Hulleman, E. Overview of Current Drug Delivery Methods Across the Blood-Brain Barrier for the Treatment of Primary Brain Tumors. CNS Drugs 2020, 34, 1121–1131. [Google Scholar] [CrossRef]
- Radaram, B.; Pisaneschi, F.; Rao, Y.; Yang, P.; Piwnica-Worms, D.; Alauddin, M.M. Novel derivatives of anaplastic lymphoma kinase inhibitors: Synthesis, radiolabeling, and preliminary biological studies of fluoroethyl analogues of crizotinib, alectinib, and ceritinib. Eur. J. Med. Chem. 2019, 182, 111571. [Google Scholar] [CrossRef] [PubMed]
- Ismail, M.; Yang, W.; Li, Y.; Chai, T.; Zhang, D.; Du, Q.; Muhammad, P.; Hanif, S.; Zheng, M.; Shi, B. Targeted liposomes for combined delivery of artesunate and temozolomide to resistant glioblastoma. Biomaterials 2022, 287, 121608. [Google Scholar] [CrossRef]
- Fulton, M.D.; Najahi-Missaoui, W. Liposomes in Cancer Therapy: How Did We Start and Where Are We Now. Int. J. Mol. Sci. 2023, 24, 6615. [Google Scholar] [CrossRef]
- Ye, D.; Zhang, X.; Yue, Y.; Raliya, R.; Biswas, P.; Taylor, S.; Tai, Y.-C.; Rubin, J.B.; Liu, Y.; Chen, H. Focused ultrasound combined with microbubble-mediated intranasal delivery of gold nanoclusters to the brain. J. Control. Release 2018, 286, 145–153. [Google Scholar] [CrossRef]
- Burgess, A.; Hynynen, K. Noninvasive and targeted drug delivery to the brain using focused ultrasound. ACS Chem. Neurosci. 2013, 4, 519–526. [Google Scholar] [CrossRef]
- Costa, C.P.; Barreiro, S.; Moreira, J.N.; Silva, R.; Almeida, H.; Lobo, J.M.S.; Silva, A.C. In Vitro Studies on Nasal Formulations of Nanostructured Lipid Carriers (NLC) and Solid Lipid Nanoparticles (SLN). Pharmaceuticals 2021, 14, 711. [Google Scholar] [CrossRef]
- Van Woensel, M.; Wauthoz, N.; Rosière, R.; Mathieu, V.; Kiss, R.; Lefranc, F.; Steelant, B.; Dilissen, E.; Van Gool, S.W.; Mathivet, T.; et al. Development of siRNA-loaded chitosan nanoparticles targeting Galectin-1 for the treatment of glioblastoma multiforme via intranasal administration. J. Control. Release 2016, 227, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.R.; Liu, M.; Khan, M.W.; Zhai, G. Progress in brain targeting drug delivery system by nasal route. J. Control. Release 2017, 268, 364–389. [Google Scholar] [CrossRef] [PubMed]
- Van Woensel, M.; Mathivet, T.; Wauthoz, N.; Rosière, R.; Garg, A.D.; Agostinis, P.; Mathieu, V.; Kiss, R.; Lefranc, F.; Boon, L.; et al. Sensitization of glioblastoma tumor micro-environment to chemo- and immunotherapy by Galectin-1 intranasal knock-down strategy. Sci. Rep. 2017, 7, 1217. [Google Scholar] [CrossRef] [PubMed]
- Chu, L.; Wang, A.; Ni, L.; Yan, X.; Song, Y.; Zhao, M.; Sun, K.; Mu, H.; Liu, S.; Wu, Z. Nose-to-brain delivery of temozolomide-loaded PLGA nanoparticles functionalized with anti-EPHA3 for glioblastoma targeting. Drug Deliv. 2018, 25, 1634–1641. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Ramos, J.; Song, S.; Kong, X.; Foroutan, P.; Martinez, G.; Dominguez-Viqueria, W.; Mohapatra, S.; Mohapatra, S.; Haraszti, R.A.; Khvorova, A.; et al. Chitosan-Mangafodipir nanoparticles designed for intranasal delivery of siRNA and DNA to brain. J. Drug Deliv. Sci. Technol. 2018, 43, 453–460. [Google Scholar] [CrossRef]
- Jahangiri, A.; Chin, A.T.; Flanigan, P.M.; Chen, R.; Bankiewicz, K.; Aghi, M.K. Convection-enhanced delivery in glioblastoma: A review of preclinical and clinical studies. J. Neurosurg. 2017, 126, 191–200. [Google Scholar] [CrossRef]
- Mehta, A.M.; Sonabend, A.M.; Bruce, J.N. Convection-Enhanced Delivery. Neurotherapeutics 2017, 14, 358–371. [Google Scholar] [CrossRef]
- Desjardins, A.; Gromeier, M.; Herndon, J.E.; Beaubier, N.; Bolognesi, D.P.; Friedman, A.H.; Friedman, H.S.; McSherry, F.; Muscat, A.M.; Nair, S.; et al. Recurrent Glioblastoma Treated with Recombinant Poliovirus. N. Engl. J. Med. 2018, 379, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Séhédic, D.; Chourpa, I.; Tétaud, C.; Griveau, A.; Loussouarn, C.; Avril, S.; Legendre, C.; Lepareur, N.; Wion, D.; Hindré, F.; et al. Locoregional Confinement and Major Clinical Benefit of (188)Re-Loaded CXCR4-Targeted Nanocarriers in an Orthotopic Human to Mouse Model of Glioblastoma. Theranostics 2017, 7, 4517–4536. [Google Scholar] [CrossRef]
- Wang, J.L.; Barth, R.F.; Cavaliere, R.; Puduvalli, V.K.; Giglio, P.; Lonser, R.R.; Elder, J.B. Phase I trial of intracerebral convection-enhanced delivery of carboplatin for treatment of recurrent high-grade gliomas. PLoS ONE 2020, 15, e0244383. [Google Scholar] [CrossRef]
- Kunwar, S.; Chang, S.; Westphal, M.; Vogelbaum, M.; Sampson, J.; Barnett, G.; Shaffrey, M.; Ram, Z.; Piepmeier, J.; Prados, M.; et al. Phase III randomized trial of CED of IL13-PE38QQR vs Gliadel wafers for recurrent glioblastoma. Neuro Oncol. 2010, 12, 871–881. [Google Scholar] [CrossRef] [PubMed]
- Fowler, M.J.; Cotter, J.D.; Knight, B.E.; Sevick-Muraca, E.M.; Sandberg, D.I.; Sirianni, R.W. Intrathecal drug delivery in the era of nanomedicine. Adv. Drug Deliv. Rev. 2020, 165–166, 77–95. [Google Scholar] [CrossRef] [PubMed]
- Zheng, F.; Pang, Y.; Li, L.; Pang, Y.; Zhang, J.; Wang, X.; Raes, G. Applications of nanobodies in brain diseases. Front. Immunol. 2022, 13, 978513. [Google Scholar] [CrossRef] [PubMed]
- Calias, P.; Banks, W.A.; Begley, D.; Scarpa, M.; Dickson, P. Intrathecal delivery of protein therapeutics to the brain: A critical reassessment. Pharmacol. Ther. 2014, 144, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Barenholz, Y. Doxil®—The first FDA-approved nano-drug: Lessons learned. J. Control. Release 2012, 160, 117–134. [Google Scholar] [CrossRef]
- Elinzano, H.; McMahon, J.B.; Mohler, A.B.; Robison, J.B.; Carcieri, A.B.; Toms, S.A.; Cielo, D.B.; Turchetti, W.B.; Vatkevich, J.; Wood, R.; et al. Nanoliposomal Irinotecan and Metronomic Temozolomide for Patients with Recurrent Glioblastoma: BrUOG329, A Phase I Brown University Oncology Research Group Trial. Am. J. Clin. Oncol. 2021, 44, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Clarke, J.L.; Molinaro, A.M.; Cabrera, J.R.; DeSilva, A.A.; Rabbitt, J.E.; Prey, J.; Drummond, D.C.; Kim, J.; Noble, C.; Fitzgerald, J.B.; et al. A phase 1 trial of intravenous liposomal irinotecan in patients with recurrent high-grade glioma. Cancer Chemother. Pharmacol. 2017, 79, 603–610. [Google Scholar] [CrossRef]
- Beier, C.P.; Schmid, C.; Gorlia, T.; Kleinletzenberger, C.; Beier, D.; Grauer, O.; Steinbrecher, A.; Hirschmann, B.; Brawanski, A.; Dietmaier, C.; et al. RNOP-09: Pegylated liposomal doxorubicine and prolonged temozolomide in addition to radiotherapy in newly diagnosed glioblastoma--a phase II study. BMC Cancer 2009, 9, 308. [Google Scholar] [CrossRef]
- Maier-Hauff, K.; Ulrich, F.; Nestler, D.; Niehoff, H.; Wust, P.; Thiesen, B.; Orawa, H.; Budach, V.; Jordan, A. Efficacy and safety of intratumoral thermotherapy using magnetic iron-oxide nanoparticles combined with external beam radiotherapy on patients with recurrent glioblastoma multiforme. J. Neurooncol. 2011, 103, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Kumthekar, P.; Ko, C.H.; Paunesku, T.; Dixit, K.; Sonabend, A.M.; Bloch, O.; Tate, M.; Schwartz, M.; Zuckerman, L.; Lezon, R.; et al. A first-in-human phase 0 clinical study of RNA interference-based spherical nucleic acids in patients with recurrent glioblastoma. Sci. Transl. Med. 2021, 13, eabb3945. [Google Scholar] [CrossRef]
- Kasenda, B.; König, D.; Manni, M.; Ritschard, R.; Duthaler, U.; Bartoszek, E.; Bärenwaldt, A.; Deuster, S.; Hutter, G.; Cordier, D.; et al. Targeting immunoliposomes to EGFR-positive glioblastoma. ESMO Open 2022, 7, 100365. [Google Scholar] [CrossRef]
- Thivat, E.; Casile, M.; Moreau, J.; Molnar, I.; Dufort, S.; Seddik, K.; Le Duc, G.; De Beaumont, O.; Loeffler, M.; Durando, X.; et al. Phase I/II study testing the combination of AGuIX nanoparticles with radiochemotherapy and concomitant temozolomide in patients with newly diagnosed glioblastoma (NANO-GBM trial protocol). BMC Cancer 2023, 23, 344. [Google Scholar] [CrossRef]
- Evans, L.; Walker, R.; MacDiarmid, J.; Brahmbhatt, H.; Anazodo, A.; McCowage, G.; Gifford, A.J.; Kavallaris, M.; Trahair, T.; Ziegler, D.S. A Phase 1 Study of Intravenous EGFR-ErbituxEDVsMIT in Children with Solid or CNS Tumours Expressing Epidermal Growth Factor Receptor. Target. Oncol. 2024, 19, 333–342. [Google Scholar] [CrossRef]
- Portnow, J.; Synold, T.W.; Badie, B.; Tirughana, R.; Lacey, S.F.; D’Apuzzo, M.; Metz, M.Z.; Najbauer, J.; Bedell, V.; Vo, T.; et al. Neural Stem Cell-Based Anticancer Gene Therapy: A First-in-Human Study in Recurrent High-Grade Glioma Patients. Clin. Cancer Res. 2017, 23, 2951–2960. [Google Scholar] [CrossRef] [PubMed]
- Portnow, J.; Badie, B.; Blanchard, M.S.; Kilpatrick, J.; Tirughana, R.; Metz, M.; Mi, S.; Tran, V.; Ressler, J.; D’apuzzo, M.; et al. Feasibility of intracerebrally administering multiple doses of genetically modified neural stem cells to locally produce chemotherapy in glioma patients. Cancer Gene Ther. 2021, 28, 294–306. [Google Scholar] [CrossRef]
- Fares, J.; Ahmed, A.U.; Ulasov, I.V.; Sonabend, A.M.; Miska, J.; Lee-Chang, C.; Balyasnikova, I.V.; Chandler, J.P.; Portnow, J.; Tate, M.C.; et al. Neural stem cell delivery of an oncolytic adenovirus in newly diagnosed malignant glioma: A first-in-human, phase 1, dose-escalation trial. Lancet Oncol. 2021, 22, 1103–1114. [Google Scholar] [CrossRef]
- Wu, D.; Chen, Q.; Chen, X.; Han, F.; Chen, Z.; Wang, Y. The blood-brain barrier: Structure, regulation, and drug delivery. Signal Transduct. Target. Ther. 2023, 8, 217. [Google Scholar] [CrossRef]
- Pardridge, W.M. CNS drug design based on principles of blood-brain barrier transport. J. Neurochem. 1998, 70, 1781–1792. [Google Scholar] [CrossRef]
- Gao, H. Progress and perspectives on targeting nanoparticles for brain drug delivery. Acta Pharm. Sin. B 2016, 6, 268–286. [Google Scholar] [CrossRef]
- van Tellingen, O.; Yetkin-Arik, B.; de Gooijer, M.; Wesseling, P.; Wurdinger, T.; de Vries, H.; De Lange, E. Overcoming the blood-brain tumor barrier for effective glioblastoma treatment. Drug Resist. Updat. 2015, 19, 1–12. [Google Scholar] [CrossRef]
- Chu, C.; Li, J.Y.; Boado, R.J.; Pardridge, W.M. Blood-brain barrier genomics and cloning of a novel organic anion transporter. J. Cereb. Blood Flow Metab. 2008, 28, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Fromm, M.F. Importance of P-glycoprotein at blood-tissue barriers. Trends Pharmacol. Sci. 2004, 25, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Peer, D.; Karp, J.M.; Hong, S.; Farokhzad, O.C.; Margalit, R.; Langer, R. Nanocarriers as an emerging platform for cancer therapy. Nat. Nanotechnol. 2007, 2, 751–760. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, V.; Liu, Z.; Hirvonen, J.; Santos, H.A. Bridging the Knowledge of Different Worlds to Understand the Big Picture of Cancer Nanomedicines. Adv. Healthc. Mater. 2018, 7, 1700432. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Zhang, X.; Huang, J.; Feng, K.; Zhang, Y.; Wu, J.; Ma, L.; Zhu, A.; Di, L. Bio-fabricated nanodrugs with chemo-immunotherapy to inhibit glioma proliferation and recurrence. J. Control. Release 2023, 354, 572–587. [Google Scholar] [CrossRef]
- Zhan, Q.; Yi, K.; Cui, X.; Li, X.; Yang, S.; Wang, Q.; Fang, C.; Tan, Y.; Li, L.; Xu, C.; et al. Blood exosomes-based targeted delivery of cPLA2 siRNA and metformin to modulate glioblastoma energy metabolism for tailoring personalized therapy. Neuro Oncol. 2022, 24, 1871–1883. [Google Scholar] [CrossRef]


| BBB-Crossing Strategy | Targeting | NDDSs | Drug | Combination Therapy (If Any) | Administration Route | Administration Model | Safety Evaluation | Pharmacokinetics (PK) | Pharmacodynamics | Ref. |
|---|---|---|---|---|---|---|---|---|---|---|
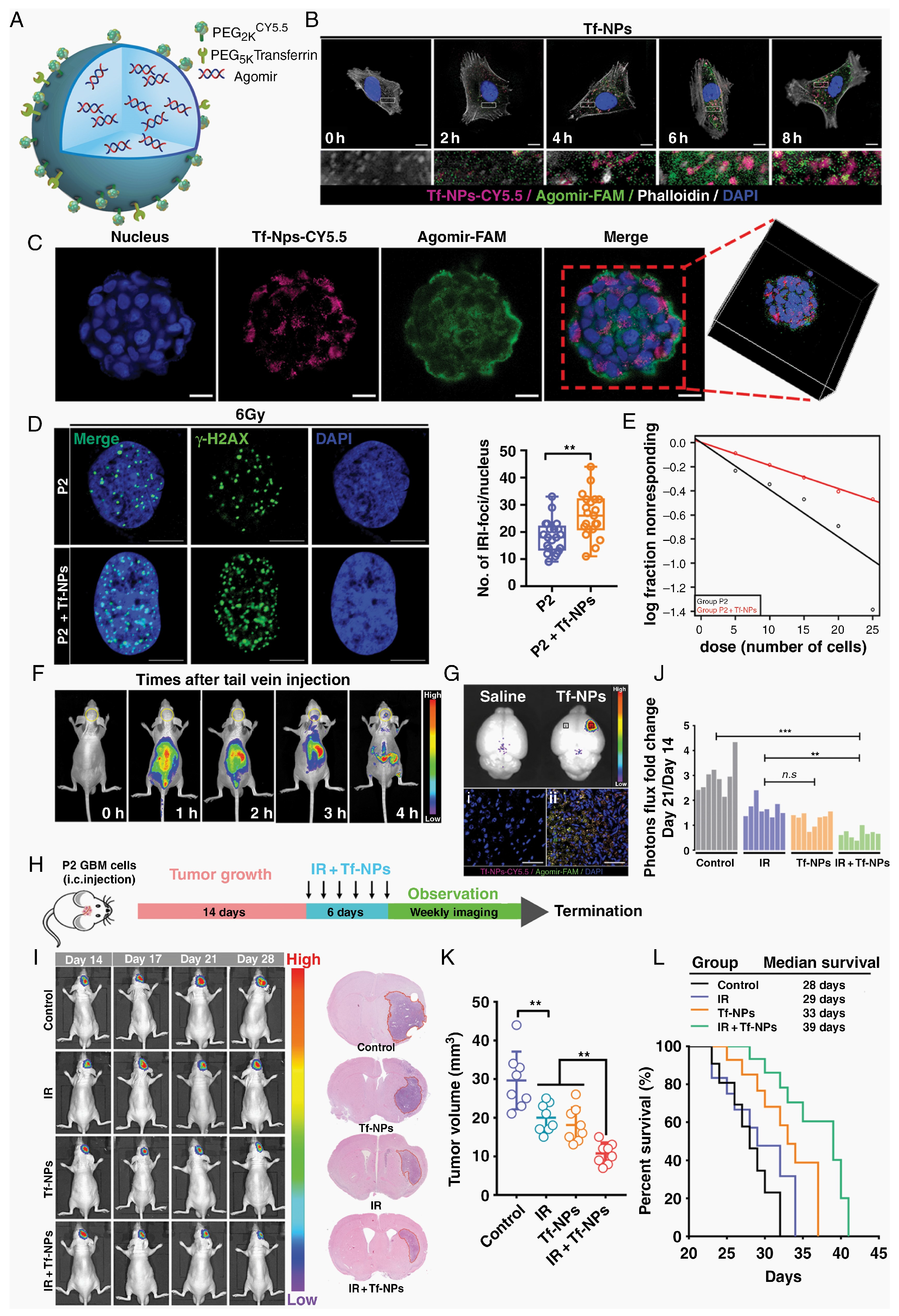
| RMT | Tf | Tf-NPs | TMZ | Bromodomain inhibitor | Tail vein injection | Human U87MG and murine GL261 glioma models | Mice treated with drug-loaded Tf-NPs maintained their body weights and body conditioning scores and had significantly more stable WBC and PLT levels over the treatment course compared with the control group. | The 24 h absorption efficiency was higher (13% vs. >1%). Tf-NPs accumulated and were retained on the tumor surface, while non-functional NPs were not. NPs loaded with TMZ demonstrated an attenuated release profile with ~90% release by 48 h. | Tf-NPs bind to GBM tumors, enhance DNA damage and apoptosis, reduce tumor burden, improve survival, and protect against systemic toxicity. | [13] |
| RMT | Lf | PMO-Lf@Dox | DOX | - | Co-incubation | C6 cells | PMO concentration was 200 μg/mL, cell survival rate was 90%, and hemolysis rate was <2%. One week after tail vein injection of 60 mg/kg PMO, no obvious changes were seen in heart, liver, spleen, lungs, or kidneys. | PMO-Lf@Dox-treated C6 cells showed a significantly higher uptake after 24 h than PMO@Dox-treated cells. | Lf-modified PMO enhances the inhibitory effect of Dox on C6 cells. | [15] |
| RMT | Lf | USLP-NH2-PEG-TMZ-Lf | TMZ | - | Tail vein injection | Transwell model with hCMEC/D3 cells; Balb/C mice | Safety was evaluated via H&E staining of mouse organs (brain, kidneys, lungs, liver) post-nano-formulation IV injection, with no toxicity observed in 24 h. | USLP-NH2-Cy5-PEG-Lf accumulated rapidly in the brain and reached its peak at 1 h post-administration, and the USLP formula significantly reduced the external alignment. | In vitro apoptosis studies on GBM cell lines U87 and GL261 showed improved TMZ-induced apoptosis with USLP formulations compared to pure TMZ. | [16] |
| RMT | Acetylcholine receptor | TMZ@RVG-Zein NPs | TMZ | - | Co-incubation | U87 cell lines; BBB model with bEnd.3 cells | TMZ@RVG-Zein NPs exhibited excellent stability, without causing significant side effects. | The TMZ@RVG-Zein NPs had an encapsulation efficiency (EE) of 77.9 ± 4.7% and a loading efficiency (LE) of 66.7 ± 2.9 mg/g. | TMZ@RVG-Zein NPs had cytotoxic effects on U87 cells and induced apoptosis and showed enhanced cellular uptake compared to TMZ alone. | [17] |
| RMT | FR | iRPPFFA@TMZ | TMZ | - | Tail vein injection | Subcutaneous and orthotopic xenograft tumor models | The biocompatibility of POSS nanoparticles was evaluated via a CCK-8 assay, hemolysis rate tests, and fluorescence imaging, showing a low toxicity and effective cellular uptake for biomedical applications. | The multifunctional POSS nanoparticles demonstrated high stability with no significant fluorescence intensity change over 8 weeks, while the iRPPFFA nanoparticle half-life was estimated at approximately 16 weeks. | In vivo studies showed that TMZ-loaded POSS nanoparticles significantly improved the survival of GBM-bearing mice, indicating an enhanced therapeutic efficacy compared to monotherapy. | [19] |
| RMT | LRP-1 receptors | Ti@FeAu–Ang nanoparticles | Magnetic nanoparticles as therapeutic agents | - | Tail vein injection | Rat GBM model | Preliminary safety analysis highlighted no toxicity to the hematological system after Ti@FeAu–Ang nanoparticle-induced hyperthermia treatment. Immunohistochemical analysis showed no significant organ damage or biological changes in vital organs such as the heart, liver, spleen, lungs, and kidneys. | The paper does not provide detailed pharmacokinetic data, but it does mention that the nanoparticles were prepared at various concentrations for the temperature elevation test and in vivo tumor growth assessment. | The Ti@FeAu–Ang nanoparticles demonstrated a temperature elevation of up to 12 °C upon magnetic stimulation, indicating potential applications in MRI- and hyperthermia-based cancer therapy. The nanoparticles showed improved cytotoxicity up to 85% in vitro due to hyperthermia produced by a magnetic field. In vivo findings showed a 10-fold decrement in tumor volume compared to that of the control group. | [22] |
| RMT | LRP-1 receptors | Au-DOX@PO-ANG | DOX | Radiotherapy | Tail vein injection | U87-MG human GBM xenografts in nude mice | Blood biochemical indicators (CK-MB, AST, and Scr) were measured in vivo, and no significant pathological changes were observed in the main organs (heart, liver, spleen, lungs, or kidneys) of the Au-DOX@PO-ANG group compared to the PBS group. The cytotoxicity of the modified AuNPs was evaluated in vitro using CCK-8 assays, showing more than 80% cell viability at concentrations up to 10 mg/L, indicating non-toxicity to GBM cells. | The storage stability of the modified AuNPs in PBS (pH 7.4) at 4 °C showed little particle size change over 4 weeks, indicating good storage ability and potential stability. | The antitumor activity of Au-DOX@PO-ANG was evaluated in vitro using the CCK-8 assay, showing significant antitumor effects when combined with radiotherapy. The therapeutic effect was observed in vivo through MRI, with the tumor volume rate of increase slowing in the Au-DOX@PO-ANG + RT group, and a significant increase in cell apoptosis was observed in this group, consistent with the MRI data. | [23] |
| RMT | EGFR | PmAb-TMZ-PLGA-NPs | TMZ | Panitumumab | Co-incubation | U-87MG and LN229 GBM cell lines | In vitro cytotoxicity assessed using the Live/Dead assay kit and fluorescence-activated cell sorting (FACS). Immunoreactivity evaluated using EGFR-overexpressed U-87MG cells. | In vitro drug release was studied using phosphate-buffered saline (PBS) under acidic (pH 5.0) and neutral (pH 7.4) conditions. Release profile determined via UV–Vis spectroscopy at various time points. | In vitro cytotoxicity/drug release was enhanced in U-87MG cells due to high EGFR expression compared to LN229 cells. | [25] |
| RMT | IGF1R | IGF1R4-mFc | Galanin peptide | - | ISBP | Rat model; Hargreaves pain model | No specific safety evaluation was described in detail. However, the use of sdAbs, which are known for their low immunogenicity and high solubility/stability, suggests potential safety advantages. | IGF1R4-mFc showed significant brain uptake compared to the negative control A20.1-mFc, with ~25% of the total amount accumulating in the brain parenchymal fraction post-ISBP. The concentration curve for IGF1R4-mFc demonstrated a linear accumulation plateauing at approximately 400 µg (~1 µM), suggesting a saturable transport mechanism. | The systemic administration of IGF1R4-mFc fused with galanin induced a dose-dependent suppression of thermal hyperalgesia in the Hargreaves pain model, indicating the pharmacological effectiveness of the brain-delivered cargo. | [26] |
| RMT | α5β1 integrin receptor | RGEK-lipopeptide containing coencapsulated STAT3siRNA and WP1066 | WP1066; STAT3siRNA | Tail vein injection | Intracranial orthotopic GL261 GBM model in C57BL/6J male mice | The document does not provide direct safety evaluation data. However, the use of integrin receptor-selective liposomes and their preferential accumulation in tumor tissue suggests the potential for reduced systemic toxicity. | NIR dye-labeled α5β1 integrin receptor-selective liposomes were found to accumulate preferentially in mouse brain tumor tissue after intravenous administration. Encapsulation efficiency: entrapment efficiency (%EE) for WP1066 was measured using analytical HPLC. | The coadministration of WP1066 and STAT3siRNA within RGDK-lipopeptide-based liposomes led to significant inhibition (>350% compared to the untreated mouse group) of orthotopically growing mouse GBM. | [30] | |
| RMT | αv β integrin and NRP-1 | CPT-S-S-PEG-iRGD@IR780 micelles | Camptothecin (CPT) | Photodynamic therapy | Tail vein injection | Intracranial orthotopic U87MG glioma tumor model in Balb/c nude mice | The micelles were shown to be stable with controlled drug release under physiological conditions. Toxicity studies in vivo assessed the mice’s survival, body weights, and histopathologies. | Information on the pharmacokinetic behavior of the micelles is not explicitly detailed in the Abstract. However, the micelle design enabled sustained CPT release upon exposure to high glutathione levels in glioma cells. | The CPT-S-S-PEG-iRGD@IR780 micelles displayed significantly enhanced antitumor effects with laser irradiation, as compared to controls. Micelles with iRGD demonstrated favorable targeting ability to glioma cells and deep tumor penetration. | [34] |
| RMT | Hsp70 | D-A-DA/TPP | DOX | PD-1 checkpoint blockade | Tail vein injection | C6-luc tumor-bearing mice | In vivo toxicity assessment: safety evaluation likely conducted by monitoring animal health, blood chemistry, and tissue histology post-treatment. However, specific details are not provided. | The biodistribution and clearance of D-A-DA/TPP nanoparticles in vivo are not explicitly discussed in the excerpt. These would typically involve measuring nanoparticle concentrations in blood, tumors, and other organs over time. | The efficacy of D-A-DA/TPP nanoparticles at inducing glioma apoptosis and prolonging the median survival time was demonstrated through in vivo studies. Combination with PD-1 checkpoint blockade was shown to further activate T cells and provoke an antitumor immune response. | [35] |
| RMT | Dopamine and GRP78 receptors | pHA-AOHX-VAP-DOX | DOX | - | Tail vein injection | Intracranial U87 glioma-bearing nude mice model | The maximum tolerated dose (MTD) was determined in healthy BALB/c mice. Hematoxylin–eosin (H&E) stains of major organs and blood samples were collected to measure blood routine and biochemical parameters. | The conjugate biodistribution in tumor and normal tissues was evaluated. The DOX accumulation at the tumor site was assessed, and the conjugation with peptides reduced the DOX accumulation in normal tissues. | The anti-GBM efficacy was evaluated by the prolonged survival time of mice and assessing the tumor cell apoptosis through TUNEL staining. The inhibition of tumor angiogenesis was evaluated using CD31 immunofluorescence staining. | [36] |
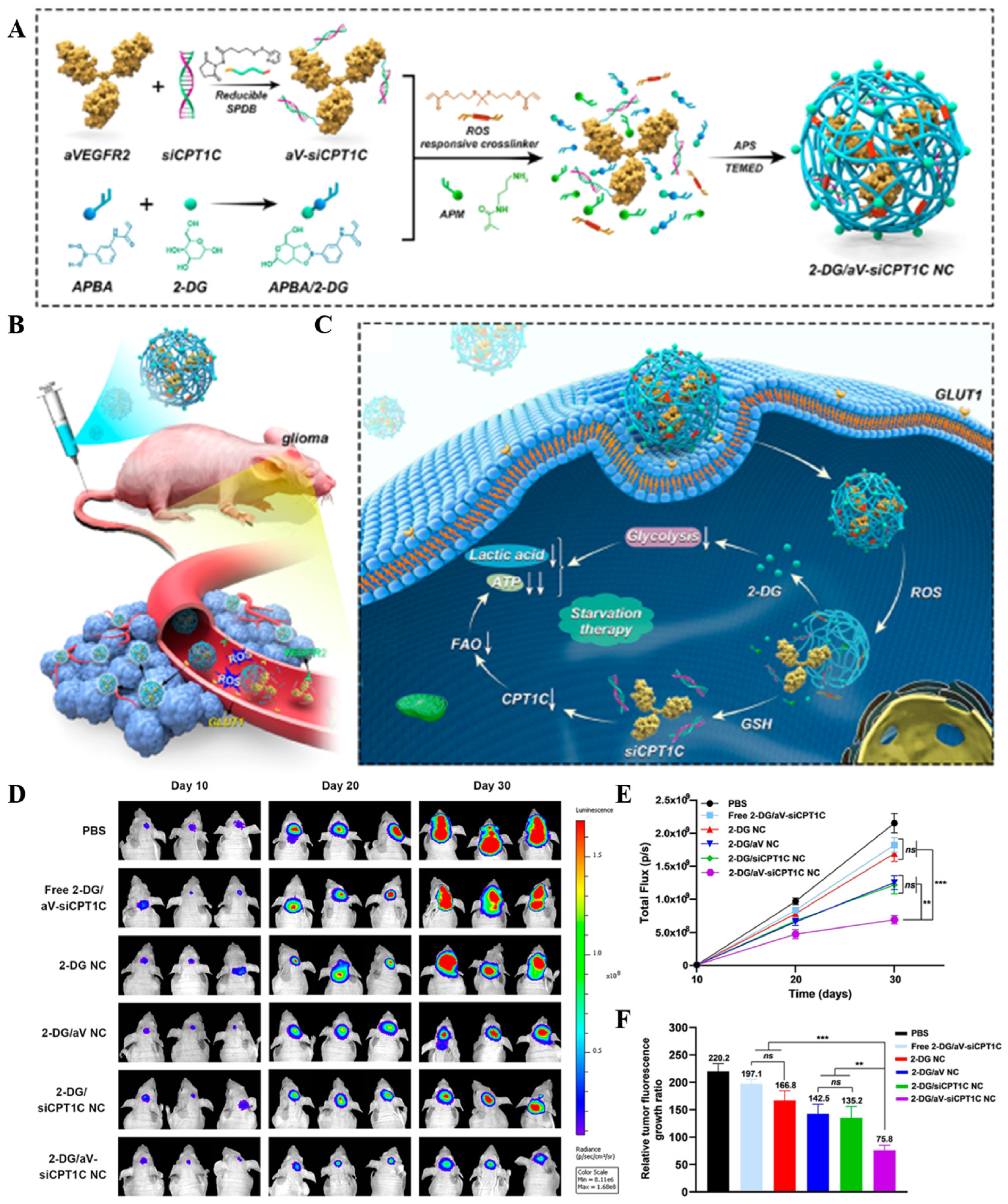
| TMT | GLUT1 | 2-DG/aV-siCPT1C NC | 2-DG | siCPT1C | Tail vein injection | Orthotopic U87-Luci cell xenograft tumor model in BALB/c nude mice | The nanocapsule safety was evaluated through histopathologic studies and blood biochemical tests, including ALT, AST, BUN, and CREA levels. No significant toxicity or side effects were observed on normal cells and tissues. | The nanocapsules showed an extended half-life compared to free siRNA, with the 2-DG/aV-Cy5-siCPT1C NC having an elimination half-life (t1/2) of approximately 1.2 h. | The nanocapsules effectively targeted GBM, inhibited energy metabolism, and showed a significant inhibitory effect on GBM growth. The combination of 2-DG, aV, and siCPT1C resulted in decreased lactic acid levels and reduced ATP production in tumor tissues, indicating effective metabolic pathway inhibition. | [39] |
| TMT | ChTs | pMPC-co-(anti-PD-L1-pPEGMA) | Anti-PD-L1 | - | Intravenous injection | LCPN orthotopic glioma tumor model | The safety and biocompatibility of the delivery system were evaluated through in vitro cytotoxicity studies using bEnd.3 and LCPN cells, as well as via a histological examination of major organs from mice. | The PK of the Cy5.5-labeled IgG in the anti-PD-L1-MP-3 formulation was studied, showing a prolonged blood circulation time compared to that of non-choline-containing controls. | The system demonstrated pH-responsive protein release in vitro, with accelerated release at pH 6.0 simulating the acidic tumor microenvironment. In vivo studies showed significant tumor growth suppression and prolonged animal survival, indicating the activation of antitumor immune responses. | [46] |
| TMT | LAT1 | WP1066-loaded liposomes of Amphi-DOPA | wp1066 | DNA vaccine | Tail vein injection | Orthotopic GL261 tumor model in female C57BL/6J mice | The safety and toxicity of the liposomal formulation were evaluated through in vivo serum toxicity profiles. No significant changes in the biochemical or hematological parameters suggest that the system is well tolerated. | Intravenously administered NIR dye-labeled Amphi-DOPA liposomes showed a preferential accumulation of the dye in brain tissue, indicating successful BBB penetration. | WP1066-loaded Amphi-DOPA liposomes alone showed an enhanced overall survivability of C57BL/6J mice bearing orthotopically established mouse GBMs by ~60% compared to untreated mice. Combination therapy further enhanced the overall survivability (>300% compared to untreated mice) when combining WP1066-loaded Amphi-DOPA liposomes with in vivo DC-targeted DNA vaccination using a survivin-encoded DNA vaccine. | [50] |
| TMT | SVCT2 | PTX-Glu-Vc-Lip | PTX | - | Tail vein injection | Intracranial C6 glioma-bearing mice | The safety of the ligand-modified liposomes was demonstrated through hemolysis assays, showing no significant increase in hemocompatibility even at high phospholipid concentrations. | The study evaluated the plasma concentration–time profiles and brain distribution of paclitaxel after the intravenous injection of different liposome formulations. The pharmacokinetic parameters, including the AUC(0-t), MRT, Tmax, Cmax, and t1/2, are reported for each formulation. | The cellular uptake of the liposomes was evaluated in GLUT1- and SVCT2-overexpressed C6 cells, showing higher uptake for the Glu-Vc-Lip compared to other formulations. The in vivo imaging of DiD-loaded liposomes demonstrated the targeting efficiency to the brain tumor site. | [53] |
| TMT | OCTN2 | LC-1000-PLGA NPs | PTX | - | Tail vein injection | 2D and 3D tumor growth models using glioma cell line T98G | The specific dose is not explicitly mentioned in the provided text. However, the studies involved the use of different paclitaxel concentrations in the in vitro cytotoxicity assays and varying PEG spacer lengths in the nanoparticles. | LC-PLGA NPs showed high accumulation in the brain as indicated by biodistribution and imaging assays in mice. Paclitaxel-loaded LC-PLGA NPs showed the sustained release of paclitaxel compared to Taxol. | The pharmacodynamic evaluation included in vitro cytotoxicity assays in T98G cells, demonstrating increased toxicity with LC-PLGA NPs compared to Taxol- and paclitaxel-loaded PLGA NPs. In vivo biodistribution studies showed an enhanced brain accumulation of paclitaxel with LC-1000-PLGA NPs. | [56] |
| TMT | Cx43 and BSAT1 | Cx43-NG/CDDP and BSAT1-NG/CDDP | Cisplatin | - | Tail vein injection | Intracranial implantation of rat GBM 101/8 in female Wistar rats | Safety was evaluated by monitoring body weight changes and the general condition of the animals, and by comparing the median survival rates of the different treatment groups. | The nanogel PK was assessed by monitoring the tumor volume changes over time using MRI and comparing the median survival times of the treated groups with those of the control group. | The antitumor efficacy of the targeted nanogels was evaluated by comparing the glioma volume and the survival rate of rats treated with targeted nanogels conjugated with specific mAbs against Cx43 and BSAT1 to those treated with non-targeted nanogels or free cisplatin. The study demonstrated a significantly reduced tumor growth and increased lifespans in animals treated with targeted nanogels. | [58] |
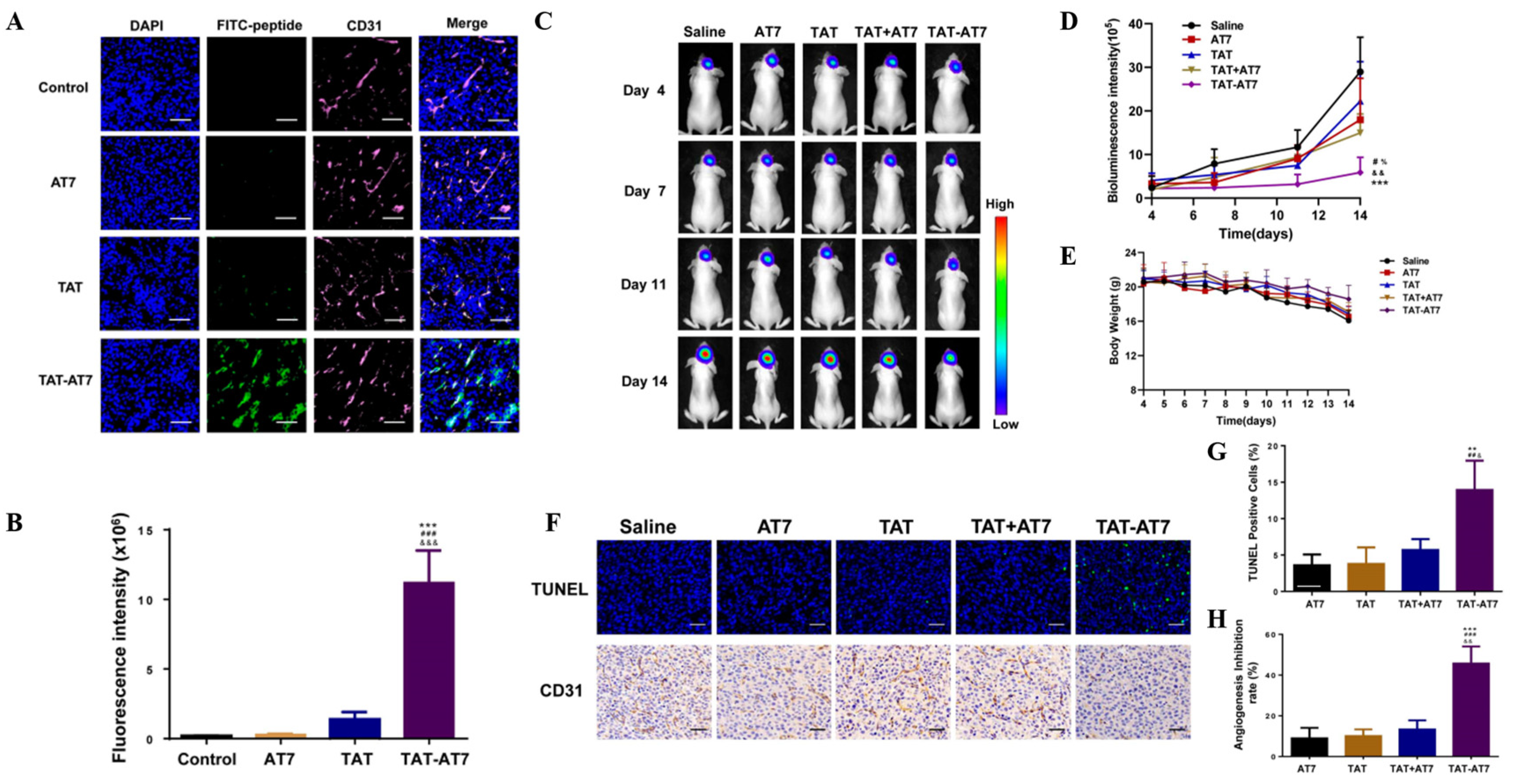
| AMT | TAT | TAT-AT7-modified PEI nanocomplex | Secretory endostatin gene | - | Intravenous injection | Orthotopic U87 glioma-bearing nude mice model | TAT-AT7 showed no obvious hemolysis at concentrations ranging from 2.5 to 640 µmol/L, indicating good biosafety. | The cellular uptake of TAT-AT7 in bEnd.3 cells (mouse brain microvascular endothelial cells) and its distribution in an intracranial glioma model were evaluated, demonstrating a high uptake efficiency and penetration capability. | TAT-AT7 exhibited significant inhibitory effects on HUVEC proliferation, migration, invasion, and tubular structure formation and also promoted apoptosis in HUVECs and inhibited zebrafish embryo angiogenesis. In vivo, TAT-AT7 significantly suppressed glioma growth, induced glioma cell apoptosis, and inhibited angiogenesis. | [65] |
| CMT+ RMT | RF + active targeting | LMP tFNA NPs | LMP | - | Tail vein injection | Orthotopic U87 glioma-bearing nude mice model | In vitro and in vivo safety evaluations showed that RFA NPs had no significant cytotoxic effects on primary hepatocytes, astrocytes, or GBM cells, and no obvious immune side effects were observed in vivo. | Biomimetic NPs encapsulated with natural cell membranes prolonged the circulation time of the drug in vivo. The hybrid membrane coating facilitated the efficient crossing of the BBB. | Inhibition of GBM growth: LMP-loaded RFA NPs exhibited superior and specific anti-GBM activities in vitro and in vivo. LMP induced apoptosis and pyroptosis in GBM cells, reducing tumor growth. The RFA NPs demonstrated reduced off-target drug delivery, ensuring specificity. | [83] |
| CMT | Active targeting | Ang-RBCm@NM-(Dox/Lex) | Dox | Lexiscan (Lex) | Intravenous injection | Orthotopic U87MG human GBM tumor-bearing nude mice | The nanomedicine was evaluated for cytotoxicity using in vitro cell viability assays. While specific toxicity data are not detailed in the Abstract, in vivo studies assessed the therapeutic efficacy and survival outcomes, which indirectly reflect safety. | The nanomedicine demonstrated a prolonged blood circulation time, with an elimination half-life (t1/2,β) of 9.3 h for Ang-RBCm@NM-(Dox/Lex), which is longer than its RBCm@NM-(Dox/Lex) counterpart (t1/2,β = 7.8 h). | Superior BBB penetration: the angiopep-2 functionalization and Lex-mediated BBB opening facilitated superb penetration across the BBB Treatment with Ang-RBCm@NM-(Dox/Lex) resulted in effective tumor growth suppression and significantly improved median survival time in orthotopic U87MG human GBM tumor-bearing nude mice. | [81] |
| CMT | Active targeting | iRGD-EM:TNDs | TMZ | - | Tail vein injection | Orthotopic U87MG human GBM tumor-bearing nude mice | Safety was evaluated through the hematoxylin and eosin (H&E) pathological staining of major organs, the monitoring of body weight, and the detection of IgE levels associated with hypersensitivity reactions. The results suggest the low systemic toxicity and good biocompatibility of the iRGD-EM:TNDs. | The EM-coated nanodots demonstrated a longer elimination half-life, suggesting reduced degradation in vivo compared to traditional PEG stealth motifs. | iRGD-EM:TNDs showed enhanced cellular uptake, improved penetration in multicellular tumor spheroids, and increased transport ratios across the BBB in vitro and in vivo. The treatment with iRGD-EM:TNDs resulted in a 100% survival rate after 30 days post-tumor implantation and induced the highest cell apoptosis level. | [82] |
| CMT | IL13Rα2 | T cells + BPLP-PLA-NPs (clicked) | DOX | CAR T-cell therapy | Tail vein injection | Intracranial xenograft model using female immunodeficient nude mice | The safety evaluation included assessing the cytotoxic effects of the nanoparticles and T cells on GBM cells in vitro and observing the behavior of T cells in vivo without them causing observable side effects. | The study evaluated the retention of nanoparticles on T cells for at least 8 days, indicating the stability of the linkage for a suitable time window for in vivo delivery. | The system demonstrated enhanced cytotoxic effects in vitro with T cells clicked with doxorubicin-loaded nanoparticles compared to bare T cells. In vivo, T cells expressing TQM-13 served as delivery shuttles for nanoparticles, significantly increasing the number of nanoparticles reaching brain tumors compared to nanoparticles alone. | [88] |
| CMT | Inflammatory tumor microenvironment | NEs-Exos/DOX | DOX | - | Intravenous injection | C6-Luc glioma-bearing mice models | The safety evaluation of the NEs-Exos/DOX system is not detailed in the provided text. The focus is on the efficacy of the system in crossing the BBB and targeting glioma cells. | The study does not provide specific pharmacokinetic data for the NEs-Exos/DOX system. However, it does mention that NEs-Exos can rapidly penetrate the BBB and migrate into the brain, suggesting favorable pharmacokinetic properties for brain tumor targeting. | The pharmacodynamics of the NEs-Exos/DOX system were demonstrated through in vitro and in vivo assays, showing that the system can improve the anticancer efficacy of DOX, reduce mortality, and effectively suppress tumor growth while prolonging the survival time in a glioma mouse model. | [89] |
| CMT | Domain CLTX and IgG4 hinge | CAR-neutrophils@RSiO2-TPZ | Tirapazamine (TPZ) | - | Intravenous injection | Mouse xenograft model of GBM | CAR neutrophils exhibited high biocompatibility with normal cells (SVG p12 glial cells, hPSCs, and hPSC-derived cells). Necrosis was not observed in major organs of experimental mice. However, concerns regarding off-target tissue toxicity or systemic toxicity are mentioned. | CAR neutrophils delivered >20% of administered nanodrugs to brain tumors compared to 1% via free nanodrugs. | CAR neutrophils presented enhanced antitumor cytotoxicity compared to peripheral blood (PB) neutrophils. In vivo tumor growth inhibition: CAR-neutrophils loaded with TPZ-loaded SiO2 nanoparticles significantly inhibited tumor growth and prolonged animal survival in GBM xenograft models. Mechanism: combination of CAR-enhanced direct cytolysis and chemotherapeutic-mediated tumor killing via cellular uptake and glutathione (GSH)-induced degradation of nanoparticles within tumor cells. | [90] |
| CMT | Active targeting | MPM@P NGs | Cisplatin | Chemodynamic therapy (CDT) | Intravenous injection | Orthotopic C6 glioma in a mouse model | The nanogel safety was evaluated using in vitro hemolysis assays, in vivo hematological indices, blood biochemical analysis, and a histopathological examination of major organs. | The nanogel PK was assessed by tracking the platinum (Pt) content in blood after intravenous injection. The MPM@P NG half-life was determined to be longer than that of PM@P NGs without a membrane coating, indicating an improved blood circulation time. | The in vivo antitumor activity of the nanogels was evaluated by monitoring tumor volume changes using T1-weighted MR imaging. The MPM@P NGs demonstrated the smallest tumor size and most efficient therapeutic effect among all the groups due to the combination of enhanced CDT and chemotherapy, as well as an improved BBB-crossing and glioma-targeting ability. | [75] |
| CMT | Active targeting | aDCM@PLGA/RAPA | RAPA | Immunotherapeutic activation | Tail vein injection | Orthotopic C6 tumor model | Studies investigating the biocompatibility and potential toxicity of aDCM@PLGA/RAPA in vivo and in vitro are mentioned but specific details are not provided. | Stability studies on aDCM@PLGA/RAPA demonstrated good colloidal stability in PBS and plasma, suggesting the potential for a prolonged circulation time in the blood. | aDCM@PLGA/RAPA effectively activated T cells and NK cells, modifying the tumor microenvironment to an immune-supportive state. Antitumor efficacy: the combined immunotherapeutic and chemotherapeutic effects led to the significant inhibition of glioma growth and induced glial differentiation. | [94] |
| CMT | Active targeting | Nanoparticle-engineered TRAIL-expressing hADSCs | TRAIL | - | Local intracranial delivery | Mouse intracranial xenograft model of patient-derived GBM cells | MTS assay revealed no significant change in cell viability of hADSCs transfected with nanoparticle-laden TRAIL DNA compared to controls, indicating safety. The in vivo safety was assessed by monitoring the survival and weight changes of the mice. | The TRAIL-overexpressing hADSC PK was evaluated by observing the migration and infiltration of the cells towards GBM tumors in vivo and measuring the TRAIL protein expression levels in vivo. | The study demonstrated that TRAIL-overexpressing hADSCs induce significant apoptosis in GBM cells in vitro and in vivo, with negligible apoptotic activity in normal brain cells. The therapeutic effects included tumor growth inhibition, the extension of animal survival, and reductions in the tumor mass and microsatellite occurrence. | [97] |
| CMT | Active targeting | PEI-PLL-transfected MSCs | Suicidal genes, namely, HSV-TK and TRAIL | Ganciclovir | Intratumoral injection | SD rats used with C6 glioma cells injected intracranially | Cell viability of MSCs transfected with the PEI-PLL copolymer was evaluated using the MTT assay. Cell viability was more than 90% at a pDNA/polymer ratio of 1:1.5 for the PEI-PLL copolymer. In vivo toxicity: while not explicitly stated in the Abstract or Methods sections, the use of nonviral vectors such as PEI-PLL copolymers is generally considered safer than viral vectors due to their low immunogenicity and reduced oncogenicity risk. | The PK of the system was assessed by monitoring the survival rates and tumor growth in the animal model after treatment with PEI-PLL-transfected MSCs. | The study demonstrated that the combination of HSV-TK and TRAIL genes in MSCs leads to a significant decrease in cell viability and an increase in apoptosis in glioma cells, both in vitro and in vivo. The reduction in the cell proliferation marker Ki67 and angiogenesis marker VEGF, along with the TUNEL assay results, indicate the therapeutic effectiveness of the MSCs at inducing apoptosis in GBM cells. | [99] |
| CMT | Active targeting | ApoE-ARTPC@TMZ | ART | TMZ | Tail vein injection | Orthotopic U251-TR GBM mouse model | In vivo experiments were conducted to assess the nanoplatform safety, including an examination of body weights, blood cell counts (RBCs, WBCs, PLTs), and histological examinations of major organs and brain tissue. | The circulation time of the liposomes in the bloodstream was evaluated using FITC-Dex as a marker, showing prolonged circulation times for ApoE-ARTPC@FITC-Dex and ARTPC@FITC-Dex compared to those of free FITC-Dex. | The induction of apoptosis, DNA damage, and inhibition of MGMT expression and Wnt/β-catenin signaling were assessed. The combination therapy showed an enhanced cytotoxicity, increased ROS generation, and significant apoptosis induction in vivo. | [106] |
| Methods to Overcome the BBB | Drug | Combination Therapy (If Any) | Research Phases | NDDSs | Administration Route | Safety Evaluation | PK | Primary Efficacy Endpoints | ClinicalTrials.Gov Identifier | Ref. |
|---|---|---|---|---|---|---|---|---|---|---|
| Passive diffusion | DOX | TMZ + radiotherapy | Phase II | Caelyx™, PEG-Dox | Intravenous infusion + oral administration | The treatment was well tolerated, with most AEs classified as grade 1–2. However, some grade 3–4 AEs were also reported. | The PK of PEG-Dox and temozolomide were not specifically detailed in the document summary provided. However, the improved BBB penetration of PEG-Dox suggests an enhanced PK compared to conventional doxorubicin. | Progression-free survival after intravenous infusion at 12 months (PFS-12): 30.2% in all patients. Median overall survival (mOS): 17.6 months in all patients including those from Phase I. Comparison to historical control: the endpoints did not differ significantly from the EORTC26981/NCIC-CE.3 data in a post hoc statistical comparison. | NCT00944801 | [128] |
| Intratumoral injection | Magnetic iron oxide nanoparticles | Fractionated stereotactic radiotherapy | Phase II | Magnetic iron oxide nanoparticles | Intratumoral injection | Side effects: acute side effects during thermotherapy were classified according to the Common Toxicity Criteria (CTC) version 2.0. Common side effects included sweating (50.0%), a general sensation of warmth (47.0%), and thermal stress with body temperatures exceeding 38° C in 6 patients (9.1%). No serious complications were observed. | The study does not provide specific pharmacokinetic data. However, it mentions that no indication of iron release from the intratumoral deposits or iron metabolization was observed, suggesting that the nanoparticles remained stable post-administration. | Overall survival after first tumor recurrence (OS-2): the median OS-2 was 13.4 months (95% CI: 10.6–16.2 months) among the 59 patients with recurrent glioblastoma. Only the tumor volume at study entry was significantly correlated with ensuing survival (p < 0.01). Overall survival after primary tumor diagnosis (OS-1): the median OS-1 was 23.2 months, with a 95% confidence interval of 17.2–29.2 months. | - | [129] |
| EPR | Irinotecan | - | Phase I | nal-IRI | Intravenous infusion | The maximum tolerated dose (MTD) was determined for both WT and HT cohorts. Dose-limiting toxicities included diarrhea, dehydration, and fatigue. The study concluded that nal-IRI had no unexpected toxicities and that the UGT1A1 genotype did not correlate with toxicity. | PK results were comparable to those seen in other PK studies of nal-IRI. PK parameters were analyzed, including maximum plasma concentrations (Cmax), areas under plasma concentration–time curve (AUC0−t), and terminal half-life (t1/2) for total irinotecan, SN-38, and SN-38G. UGT1A1*28 genotype did not affect PK parameters. | The primary efficacy endpoint was PFS-6. The study reported PFS-6 as 2.9% for the intent-to-treat cohort, with a median PFS of 42 days and a median overall survival of 107 days. | - | [127] |
| Passive diffusion | Irinotecan | TMZ | Phase I | nal-IRI | Intravenous infusion + oral administration | The study evaluated safety by monitoring dose-limiting toxicities (DLTs), which included grade 4 neutropenia, grade 3 diarrhea, hypokalemia, fatigue, anorexia, and other grade 3 or 4 nonhematologic toxicities. The MTD for nal-IRI was determined to be 50 mg/m2 every 2 weeks with TMZ. | The study does not provide specific pharmacokinetic data. Enhanced BBB penetration: the nanoliposomal encapsulation of irinotecan improved its ability to cross the BBB, as demonstrated in preclinical animal models. Tissue analysis: in preclinical studies, nal-IRI showed a 10.9-fold increase in tumor area under the curve compared to free irinotecan and a 35-fold selectivity for tumor versus normal tissue exposure. | The primary efficacy endpoints were the assessment of the response rate (complete or partial response as defined by Macdonald criteria) and PFS. The study was terminated after an interim analysis showed no activity (0% response rate) and a median PFS of 2 months. | NCT03119064 | [126] |
| EPR + active transport | NU-0129 | - | Phase 0 | siBcl2L12-SNAs | Intravenous infusion | The safety assessment revealed no significant treatment-related toxicities. The study monitored vital signs, blood chemistry, and adverse events in patients, with only two treatment-related severe adverse events (lymphopenia and hypophosphatemia) noted, which were considered “possibly” related to the treatment. | PK analysis showed that siRNA was rapidly eliminated from plasma with a mean half-life of 0.09 h, while gold (Au), used as a marker for the SNAs, had a much slower elimination with a mean half-life of 17 h. The study also details the clearance rates and volume of distribution for both siRNA and Au. | The primary efficacy endpoints were the intratumoral accumulation of SNAs and the suppression of the Bcl2L12 gene. The study reported that NU-0129 uptake into glioma cells correlated with a significant reduction in tumor-associated Bcl2L12 protein expression. Additionally, the presence of Au in the tumor tissue was confirmed, indicating that the SNAs reached the patient tumors. | NCT03020017 | [130] |
| RMT | DOX | - | Phase I | Anti-EGFR ILs-dox | Intravenous infusion | The study reports safety data from the application of anti-EGFR ILs-dox in patients with relapsed glioblastoma. No grade 4 or 5 adverse events occurred. One case of severe pneumonitis was reported, which resolved with treatment. Other adverse events included febrile neutropenia in two patients, which was managed without sequelae. | The pharmacokinetic analysis showed that the mean plasma concentration of doxorubicin 24 h after administration was 15,805 ng/mL. DOX concentrations in CSF were below 1 ng/mL in all patients, indicating that anti-EGFR ILs-dox does not cross the BBB at clinically relevant levels. However, significant doxorubicin levels were detected in glioblastoma tissue 24 h after application, suggesting that the disrupted BBB in high-grade gliomas may enable liposome delivery into tumor tissue. | The primary efficacy endpoints were the anti-EGFR ILs-dox concentrations in plasma, CSF, and glioblastoma tissue. The median PFS was 1.5 months, and the median OS was 8 months. One patient had a very long remission, suggesting that neoadjuvant administration may positively affect the outcome. | NCT03603379 | [131] |
| EPR | AGuIX nanoparticles | Standard of care for glioblastoma | Phase I/II | AGuIX nanoparticles | Intravenous infusion | Toxicity assessment: DLT defined as any grade 3–4 NCI Common Terminology Criteria for Adverse Events (CTCAE) toxicity, except for alopecia, nausea, vomiting, or fever. Adverse event reporting: according to CTCAE (version 5.0). Neurological status evaluation: clinical assessment and Mini-Mental State Examination (MMSE). | PK parameters of AGuIX nanoparticles, including AUC, Tmax, and Cmax, were measured on blood samples and urinary excretion during Phase I of the study. | For Phase I, the primary endpoint is the RP2D of AGuIX nanoparticles, with DLT defined as any grade 3–4 toxicity. For Phase II, the primary endpoint is the 6-month progression-free survival rate, which will be estimated using the Kaplan–Meier method. | NCT04881032 | [132] |
| EPR + RMT | Mitoxantrone | - | Phase I | EGFR-Erbitux EDVsMIT | Intravenous infusion | The safety evaluation of EEDVsMit showed that it was well tolerated, with no dose-limiting toxicities observed. The most common drug-related adverse events were grade 1–2 fever, nausea, vomiting, rash, lymphopenia, and mildly deranged liver function tests. | The study does not provide detailed pharmacokinetic data within the summary. However, it mentions that the EDV selectively targets the cancer cell via the bispecific antibody and releases the cytotoxic drug into the tumor cell after macropinocytosis and a breakdown in lysosomes. | The primary efficacy endpoints were safety and tolerability, with the study also aiming to preliminarily define the antitumor activity of mitoxantrone-containing EDVs. The best antitumor response observed was a mixed response in one patient, and all other patients had progressive disease. | NCT02687386 | [133] |
| CED | Irinotecan | - | Phase I | nal-IRI | Intratumoral injection | Safety was evaluated via monitoring adverse events, scheduled laboratory assessments, vital sign measurements, and physical examinations. Toxicities were graded according to the NCI CTCAE v. 4.0. | The study assesses the distribution of gadolinium, used in conjunction with real-time imaging, to model the drug distribution and evaluate the effectiveness of CED at delivering nal-IRI to the tumor site. | The primary efficacy endpoint is OS at 12 months (OS12), which will be considered evaluable for clinical efficacy. | NCT03086616 | - |
| CED | Irinotecan | - | Phase I | Liposomal irinotecan | Intratumoral injection | Safety was evaluated by monitoring DLTs within 30 days post-infusion, as well as any neurological or systemic grade 3 or higher toxicities. | PK measurements were taken at pre-dose, 1 day after drug administration, and 1 week post-op to estimate the drug distribution and concentration in the brain. | The primary efficacy endpoints include the determination of the maximum tolerated dose and the assessment of the PFS at 6 months and 10 years, as well as the OS at 12 months and 10 years. | NCT 02022644 | - |
| Active targeting | MT-201-GBM | Standard radiation therapy and TMZ chemotherapy | Phase I | MT-201-GBM | Intravenous administration | The study aimed to assess the safety and tolerability of MT-201-GBM by measuring the primary safety endpoint: the percentage of patients with a DLT during the DLT observation period within each dose level. Other safety measures: changes in laboratory parameters (e.g., hemoglobin, creatinine, AST, and bilirubin) and monitoring for adverse events. | The study does not provide specific details on pharmacokinetic assessments. However, it does include immune response measurements, such as changes from baseline in IFN gamma, granzyme-B, and fluorospot, which may provide insights into the vaccine’s biological activity. | The primary efficacy endpoints include the MTD of MT-201-GBM and immune response measurements after the second and third infusions compared to baseline. Secondary outcome measures include OS, PFS, and changes in immune response indicators. | NCT04741984 | - |
| Active targeting and bypassing of the BBB | 5-FC | - | Phase I | CD-NSCs | Intracranial injection + oral administration | The study evaluated safety through the monitoring of adverse events, an assessment of possible NSC migration into the systemic circulation, and testing for the presence of replication-competent retrovirus (RCR). No DLTs were observed due to the CD-NSCs, and there was no development of anti-CD-NSC antibodies. | Intracerebral microdialysis was used to measure brain levels of 5-FC and 5-FU, showing CD-NSCs produced 5-FU locally in a 5-FC dose-dependent manner. Blood samples were collected to assess systemic drug concentrations and perform immunologic correlative studies. | The primary efficacy endpoints included assessing the feasibility of treating recurrent high-grade glioma patients with intracranially administered CD-NSCs followed by oral 5-FC. Secondary objectives included assessing possible CDNSC immunogenicity and secondary tumorigenicity and evaluating the proof-of-concept regarding CD-NSC migration to tumor foci and the localized conversion of 5-FC to 5-FU. | NCT01172964 | [134] |
| Active targeting and bypassing of the BBB | 5-FC | Leucovorin | Phase I | CD-NSCs | Intracranial injection | Safety was evaluated by monitoring adverse events, an assessment of possible NSC migration into the systemic circulation using qPCR, and testing for the presence of replication-competent retrovirus (RCR). No clinical signs of immunogenicity were observed, and only three patients developed anti-NSC antibodies. | Neuropharmacokinetic data were collected using intracerebral microdialysis to confirm continuous production of 5-FU in the brain during the course of 5-FC administration. The primary pharmacokinetic parameters of interest were the Cmax and AUC of 5-FC and 5-FU, measured in both dialysate samples and plasma. | The primary efficacy endpoints included assessing the feasibility of serially administering CD-NSCs and determining the recommended dosing for Phase II testing. Secondary objectives included characterizing the relationship between intracerebral and systemic concentrations of 5-FC and 5-FU, assessing CD-NSC immunogenicity, and describing clinical activity. The best response observed was stable disease in three participants, with a range of 4 to 5 months. | NCT02015819 | [135] |
| Active targeting and bypassing of the BBB | Irinotecan Hydrochloride | - | Phase I | hCE1m6-NSCs | Intracranial administration + intravenous administration | Safety was evaluated by grading toxicities using the NCI CTCAE version 4.0, with specific attention to DLTs during the first treatment cycle. | PK data were collected via intracerebral microdialysis to measure SN-38 concentrations in the brain interstitium and plasma levels of irinotecan and SN-38. | The primary efficacy endpoints included the assessment of clinical benefit, defined as stable disease, partial response, or complete response, as measured by RANO criteria, for up to 6 months. | NCT02192359 | - |
| Active targeting and bypassing of the BBB | Oncolytic Adenovirus (CRAd-S-pk7) | Standard temozolomide chemotherapy and radiotherapy | Phase I | NSC-CRAd-S-pk7 | Intracranial injection | The trial demonstrated that the treatment was safe, with no formal dose-limiting toxicity reached. One patient developed viral meningitis (grade 3) due to an inadvertent injection into the lateral ventricle. | PK assessments were performed through medical history, imaging, blood samples, and chemistry values collected at screening and follow-up. The study does not detail specific pharmacokinetic parameters but focuses on the safety and presence of the treatment. | The primary endpoints were safety and tolerability. Secondary endpoints included the estimation of survival outcomes and evaluation of immune response correlation with clinical outcomes. The median progression-free survival was 9.05 months, and the overall survival was 18.4 months. | NCT03072134 | [136] |
| CMT | Survivin DC cell injection | Radiotherapy and TMZ chemotherapy | Phase I | Survivin-loaded dendritic cell injection | Intradermal injection + intravenous infusion | Safety was evaluated by monitoring adverse events that occurred within 28 days after the first to the third dose, as judged by the investigator to be related to the study drug. DLT was a primary outcome measure. | Not specifically detailed in the document. However, the administration schedule (days 0, 14, and 28) and route of administration (ID and IV) indicate that the PK is influenced by the absorption, distribution, metabolism, and excretion of the survivin-loaded dendritic cells. | The primary efficacy endpoints include the PFS and OS measured over 2 years. Secondary outcome measures include immune effect assessments such as an anti-survivin antibody test, cytokine detection, and specific T-cell responses, as well as DC cell activity and in vivo processes, measured at specific time points. | NCT06524063 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duan, M.; Cao, R.; Yang, Y.; Chen, X.; Liu, L.; Ren, B.; Wang, L.; Goh, B.-C. Blood–Brain Barrier Conquest in Glioblastoma Nanomedicine: Strategies, Clinical Advances, and Emerging Challenges. Cancers 2024, 16, 3300. https://doi.org/10.3390/cancers16193300
Duan M, Cao R, Yang Y, Chen X, Liu L, Ren B, Wang L, Goh B-C. Blood–Brain Barrier Conquest in Glioblastoma Nanomedicine: Strategies, Clinical Advances, and Emerging Challenges. Cancers. 2024; 16(19):3300. https://doi.org/10.3390/cancers16193300
Chicago/Turabian StyleDuan, Mengyun, Ruina Cao, Yuan Yang, Xiaoguang Chen, Lian Liu, Boxu Ren, Lingzhi Wang, and Boon-Cher Goh. 2024. "Blood–Brain Barrier Conquest in Glioblastoma Nanomedicine: Strategies, Clinical Advances, and Emerging Challenges" Cancers 16, no. 19: 3300. https://doi.org/10.3390/cancers16193300







