Clampless In-Situ Immobilized Branching (CLIMB) to Reconstruct the Internal Iliac Artery
Abstract
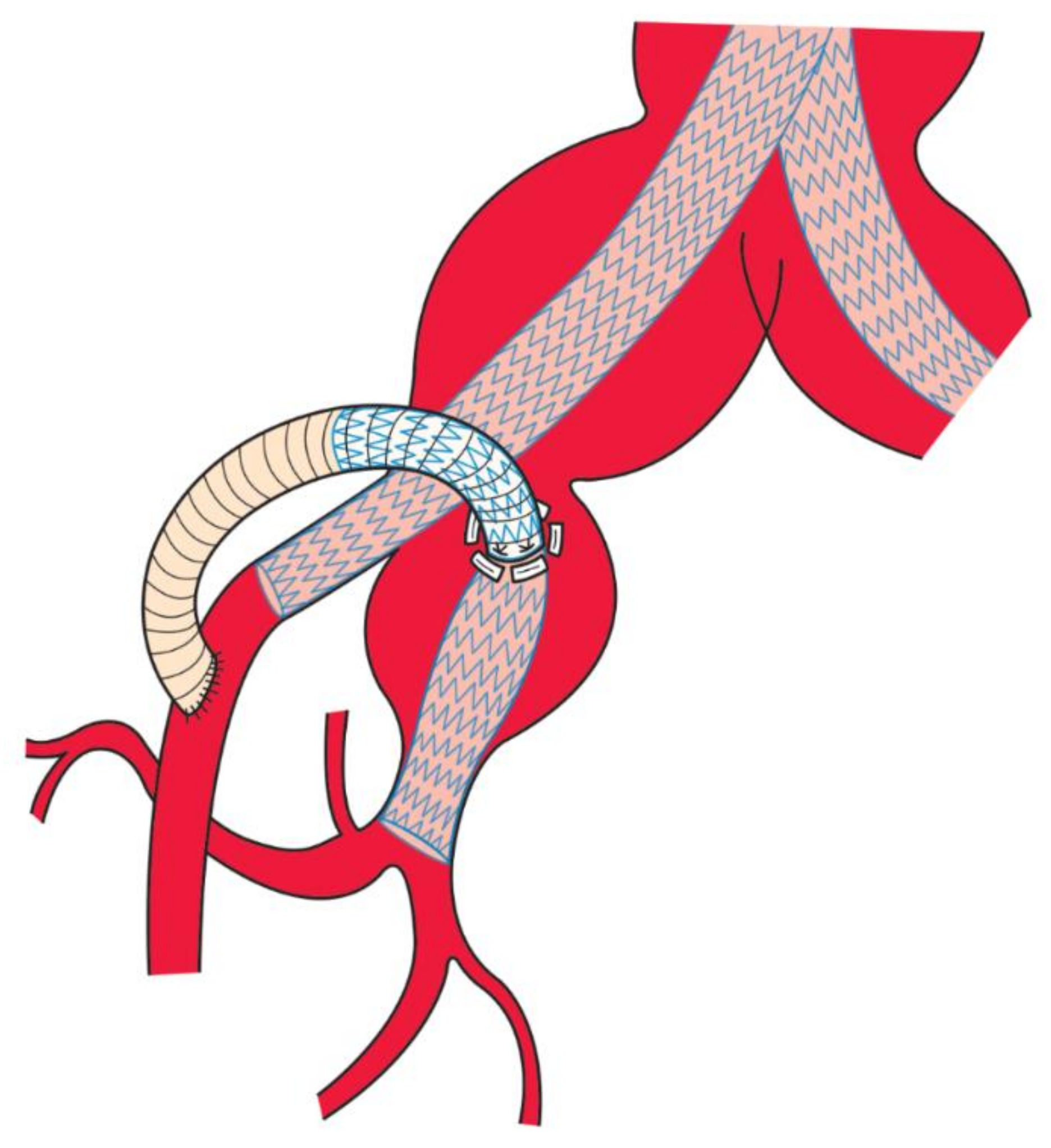
:1. Introduction
2. Patients and Methods
2.1. Perioperative Management
2.2. Surgical Procedures
2.3. Tips of the CLIMB Technique
2.4. Advantages of the CLIMB Technique over Other Alternatives at Planning
3. Results
3.1. Characteristics of the Eligible Patients
3.2. Details of Operation Procedures
3.3. Postoperative Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kouvelos, G.N.; Katsargyris, A.; Antoniou, G.A.; Oikonomou, K.; Verhoeven, E.L.G. Outcome after Interruption or Preservation of Internal Iliac Artery Flow During Endovascular Repair of Abdominal Aorto-iliac Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2016, 52, 621–634. [Google Scholar] [CrossRef] [Green Version]
- Jean-Baptiste, E.; Brizzi, S.; Bartoli, M.; Sadaghianloo, N.; Baqué, J.; Magnan, P.-E.; Hassen-Khodja, R. Pelvic ischemia and quality of life scores after interventional occlusion of the hypogastric artery in patients undergoing endovascular aortic aneurysm repair. J. Vasc. Surg. 2014, 60, 40–49.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosaka, A.; Kato, M.; Kato, I.; Isshiki, S.; Okubo, N. Outcome after concomitant unilateral embolization of the internal iliac artery and contralateral external-to-internal iliac artery bypass grafting during endovascular aneurysm repair. J. Vasc. Surg. 2011, 54, 960–964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wanhainen, A.; Verzini, F.; Van Herzeele, I.; Allaire, E.; Bown, M.; Cohnert, T.; Dick, F.; van Herwaarden, J.; Karkos, C.; Koelemay, M.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 8–93. [Google Scholar] [CrossRef] [Green Version]
- Chaikof, E.L.; Dalman, R.L.; Eskandari, M.K.; Jackson, B.M.; Lee, W.A.; Mansour, M.A.; Mastracci, T.M.; Mell, M.; Murad, M.H.; Nguyen, L.L.; et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J. Vasc. Surg. 2018, 67, 2–77.e2. [Google Scholar] [CrossRef] [Green Version]
- Schneider, D.B.; Matsumura, J.S.; Lee, J.T.; Peterson, B.G.; Chaer, R.A.; Oderich, G.S. Five-year outcomes from a prospective, multicenter study of endovascular repair of iliac artery aneurysms using an iliac branch device. J. Vasc. Surg. 2022, in press. [Google Scholar] [CrossRef]
- Lepidi, S.; Piazza, M.; Scrivere, P.; Menegolo, M.; Antonello, M.; Grego, F.; Frigatti, P. Parallel Endografts in the Treatment of Distal Aortic and Common Iliac Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2014, 48, 29–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kritpracha, B.; Pigott, J.P.; Russell, T.E.; Corbey, M.J.; Whalen, R.C.; DiSalle, R.S.; Price, C.I.; Sproat, I.A.; Beebe, H.G. Bell-bottom aortoiliac endografts: An alternative that preserves pelvic blood flow. J. Vasc. Surg. 2002, 35, 874–881. [Google Scholar] [CrossRef] [Green Version]
- Muzepper, M.; Zhou, M. Anatomic Suitability of Iliac Branched Devices for Chinese Patients with Abdominal-Iliac Aortic Aneurysm. Ann. Vasc. Surg. 2020, 67, 178–184. [Google Scholar] [CrossRef]
- Rouby, A.-F.; Kuntz, S.; Delay, C.; Thaveau, F.; Georg, Y.; Lejay, A.; Chakfe, N. Volume Change after Endovascular Treatment of Common Iliac Arteries ≥ 17 mm Diameter: Assessment of Type 1b Endoleak Risk Factors. Eur. J. Vasc. Endovasc. Surg. 2020, 59, 51–58. [Google Scholar] [CrossRef]
- Gray, D.; Shahverdyan, R.; Reifferscheid, V.; Gawenda, M.; Brunkwall, J. EVAR with Flared Iliac Limbs has a High Risk of Late Type 1b Endoleak. Eur. J. Vasc. Endovasc. Surg. 2017, 54, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Kagaya, H.; Kubo, Y.; Banno, H.; Ohkubo, N. Real chimney technique for total debranching of supra-aortic trunks. J. Vasc. Surg. 2014, 61, 542–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Oria, M.; Tenorio, E.R.; Oderich, G.S.; Mendes, B.C.; Kalra, M.; Shuja, F.; Colglazier, J.J.; DeMartino, R.R. Outcomes of the Gore Excluder Iliac Branch Endoprosthesis Using Division Branches of the Internal Iliac Artery as Distal Landing Zones. J. Endovasc. Ther. 2020, 27, 316–327. [Google Scholar] [CrossRef] [PubMed]
- Faries, P.L.; Morrissey, N.; Burks, J.A.; Gravereaux, E.; Kerstein, M.D.; Teodorescu, V.J.; Hollier, L.H.; Marin, M.L. Internal iliac artery revascularization as an adjunct to endovascular repair of aortoiliac aneurysms. J. Vasc. Surg. 2001, 34, 892–899. [Google Scholar] [CrossRef] [Green Version]
- Kobayashi, Y.; Sakaki, M.; Yasuoka, T.; Iida, O.; Dohi, T.; Uematsu, M. Endovascular repair with contralateral external-to-internal iliac artery bypass grafting: A case series. BMC Res. Notes 2015, 8, 183. [Google Scholar] [CrossRef] [Green Version]
- Mansukhani, N.A.; Havelka, G.E.; Helenowski, I.B.; Rodriguez, H.E.; Hoel, A.W.; Eskandari, M.K. Hybrid Endovascular Aortic Aneurysm Repair: Preservation of Pelvic Perfusion with External to Internal Iliac Artery Bypass. Ann. Vasc. Surg. 2017, 42, 162–168. [Google Scholar] [CrossRef]
- Oliveira-Pinto, J.; Martins, P.; Mansilha, A. Endovascular treatment of iliac aneurysmal disease with internal iliac artery preservation: A review of two different approaches. Int. Angiol. 2019, 38, 494–501. [Google Scholar] [CrossRef]
- Massière, B.; Leão, R.; Vescovi, A.; Leal, D.; Vivas, P.; Vasconcelos, A.; von Ristow, A. Outcomes of bell-bottom technique compared to standard endovascular aneurysm repair. Vascular 2021, 29, 817–821. [Google Scholar] [CrossRef]
- Pini, R.; Faggioli, G.; Indelicato, G.; Gallitto, E.; Mascoli, C.; Abualhin, M.; Stella, A.; Gargiulo, M. Anatomical Predictors of Flared Limb Complications in Endovascular Aneurysm Repair. J. Endovasc. Ther. 2019, 26, 550–555. [Google Scholar] [CrossRef]
- Pickney, C.C.; Rowse, J.; Quatromoni, J.; Kirksey, L.; Caputo, F.J.; Lyden, S.P.; Smolock, C.J. Outcomes of Gore iliac branch endoprosthesis with internal iliac component versus Gore Viabahn VBX. J. Vasc. Surg. 2022, 76, 733–740.e2. [Google Scholar] [CrossRef]
- Qazi, E.; Wilting, J.; Patel, N.R.; Alenezi, A.O.; Kennedy, S.A.; Tan, K.T.; Jaberi, A.; Mafeld, S. Arteries of the Lower Limb—Embryology, Variations, and Clinical Significance. Can. Assoc. Radiol. J. 2022, 73, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.K.; Campbell, W.B.; Earnshaw, J.J. Survey of management of common iliac artery aneurysms by members of the Vascular Society of Great Britain and Ireland. Ann. R. Coll. Surg. Engl. 2014, 96, 116–120. [Google Scholar] [CrossRef] [PubMed]

| Pt No. | Age | Sex | Diagnosis | Contralateral IIA Occlusion | Prior Aortic Procedure | Bridging Stentgraft (Size) | Distal Landing | IIA Branch Embolization | Concomitant Aortic Procedures | Other Procedures | Operative Time, Min | Estimated Blood Loss, mL |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 79 | M | Bil CIAA, bil IIAA s/p OAR | + | OAR | Iliac leg (12–100) | IIA | - | EVAR, contralateral IIA embolization | None | 370 | 275 |
| 2 | 75 | M | AAA, bil CIAA, bil IIAA | + | - | Iliac leg (12–100) | IIA | - | EVAR, contralateral IIA embolization | None | 475 | 440 |
| 3 | 69 | M | AAA, bil CIAA, bil IIAA | + | - | Covered stents (SGA, 10–80; IGA, 8–80) | SGA, IGA | - | EVAR, contralateral IIA embolization | FAA repair | 622 | 520 |
| 4 | 39 | M | DAA, Chronic TBAD | - | - | Iliac leg (12–70) | IIA | - | EVAR | None | 485 | 130 |
| 5 | 68 | M | AAA, Lt CIAA, bil IIAA | + | - | IIC (10–70) | IIA | - | EVAR, contralateral IIA embolization | PTRA | 316 | 420 |
| 6 | 76 | M | AAA, lt CIAA s/p Rt iliac EVAR | + | Iliac EVAR | Iliac leg (12–100) | IIA | - | EVAR | PTRA | 262 | 585 |
| 7 | 80 | M | Lt IIAA | + * | - | VBX ×2 (8L–79) | SGA | - † | None | None | 171 | 310 |
| 8 | 80 | M | T1bEL after EVAR, IIAA | + | EVAR | Iliac leg (12–100) + IIC (10–70) | SGA | + | IIA branch embolization | None | 181 | 220 |
| 9 | 67 | M | T1bEL after EVAR | + | EVAR | IIC ×2 (10–70) | IIA | - | EVAR | None | 166 | 670 |
| 10 | 56 | M | Lt CIAA, IIAA s/p OAR | + | OAR | Iliac leg (10–70) + IIC (10–70) | SGA | + | IIA branch embolization | Graft interposition | 479 | 1610 |
| 11 | 71 | M | T1bEL after EVAR | + | EVAR | Iliac leg (12–120) + IIC (12–70) | IIA | - | None | None | 196 | 285 |
| Pt No. | BC, Ipsilateral | BC, Contralateral | LOS | IIA Patency | Other Complications | Survival | Follow-Up Period, mo |
|---|---|---|---|---|---|---|---|
| 1 | - | + | 14 | + | EL- | Dead, pneumoniae | 8.9 |
| 2 | - | - | 14 | + | T2EL | Dead, colon cancer | 101.0 |
| 3 | - | - | 11 | SGA+ IGA- * | T2EL | Dead, lung cancer | 111.9 |
| 4 | - | - | 26 | + | EL- | Dead, heart failure | 64.6 |
| 5 | - | - | 11 | + | EL- | Alive | 45.2 |
| 6 | - | - | 20 | + | T2EL | Alive | 13.2 |
| 7 | - | - | 14 | + | T2EL | Alive | 33.2 |
| 8 | - | - | 8 | + | T2EL | Alive | 19.8 |
| 9 | - | - | 8 | + | EL- | Alive | 12.9 |
| 10 | - | + | 9 | + | EL- | Alive | 4.2 |
| 11 | - | - | 14 | + | EL- | Alive | 0.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shirasu, T.; Akai, A.; Motoki, M.; Kato, M. Clampless In-Situ Immobilized Branching (CLIMB) to Reconstruct the Internal Iliac Artery. Life 2022, 12, 1928. https://doi.org/10.3390/life12111928
Shirasu T, Akai A, Motoki M, Kato M. Clampless In-Situ Immobilized Branching (CLIMB) to Reconstruct the Internal Iliac Artery. Life. 2022; 12(11):1928. https://doi.org/10.3390/life12111928
Chicago/Turabian StyleShirasu, Takuro, Atsushi Akai, Manabu Motoki, and Masaaki Kato. 2022. "Clampless In-Situ Immobilized Branching (CLIMB) to Reconstruct the Internal Iliac Artery" Life 12, no. 11: 1928. https://doi.org/10.3390/life12111928
APA StyleShirasu, T., Akai, A., Motoki, M., & Kato, M. (2022). Clampless In-Situ Immobilized Branching (CLIMB) to Reconstruct the Internal Iliac Artery. Life, 12(11), 1928. https://doi.org/10.3390/life12111928




