Comparative Study of Different Respiratory Muscle Training Methods: Effects on Cardiopulmonary Indices and Athletic Performance in Elite Short-Track Speedskaters
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants’ Characteristics
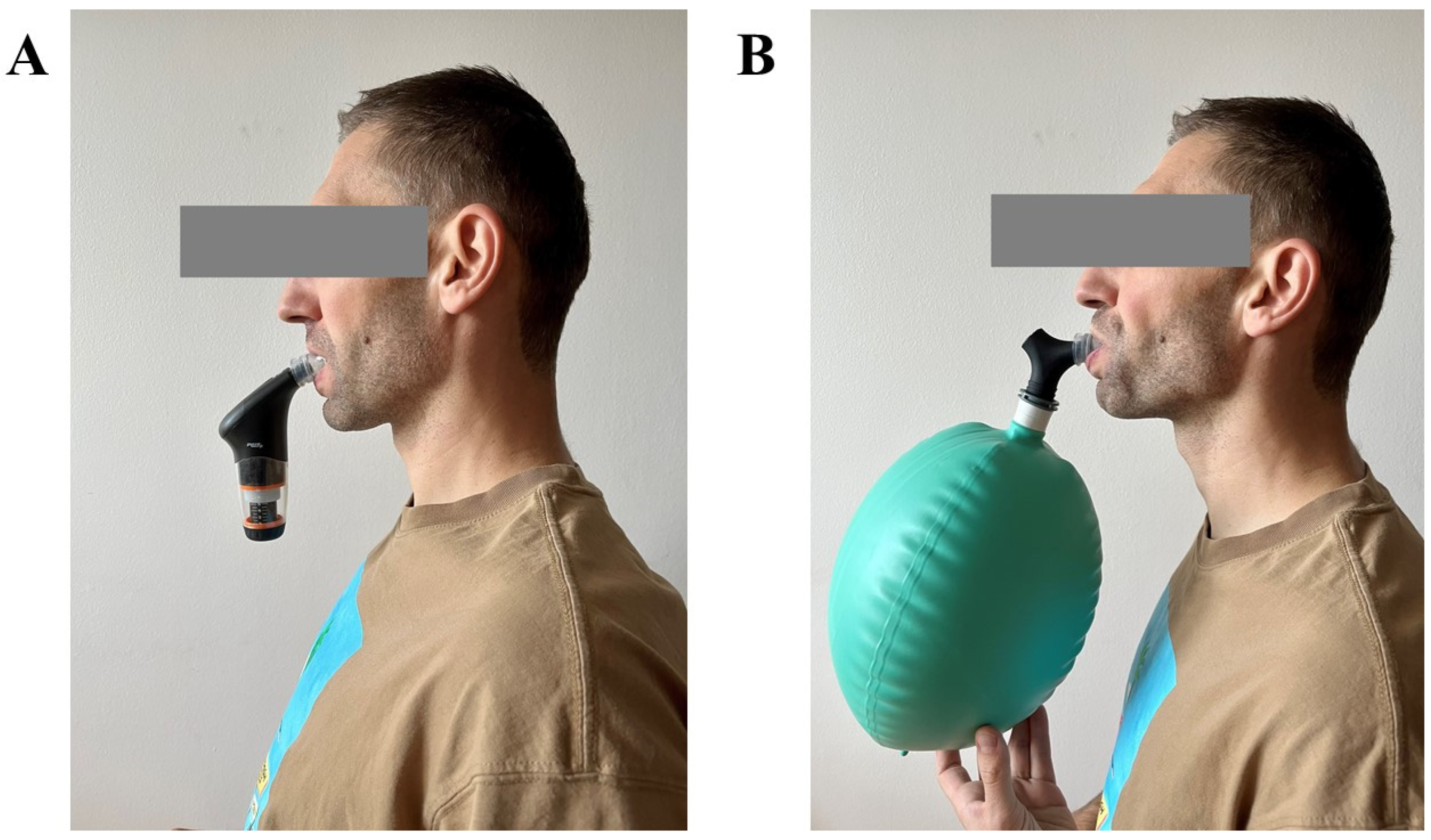
2.2. Respiratory Muscle Training Protocols
2.3. Data Collection
2.4. Statistical Analysis
3. Results
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boutellier, U.; Büchel, R.; Kundert, A.; Spengler, C. The Respiratory System as an Exercise Limiting Factor in Normal Trained Subjects. Eur. J. Appl. Physiol. Occup. Physiol. 1992, 65, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Volianitis, S.; Mcconnell, A.K.; Koutedakis, Y.; Mcnaughton, L.; Backx, K.; Jones, D.A. Inspiratory Muscle Training Improves Rowing Performance. Med. Sci. Sports Exerc. 2001, 33, 803–809. [Google Scholar] [CrossRef] [PubMed]
- Romer, L.M.; McConnell, A.K.; Jones, D.A. Effects of Inspiratory Muscle Training on Time-Trial Performance in Trained Cyclists. J. Sports Sci. 2002, 20, 547–562. [Google Scholar] [CrossRef] [PubMed]
- Klusiewicz, A.; Zubik, Ł.; Długołęcka, B.; Charmas, M.; Broniec, J.; Opaszowski, B.H.; Starczewski, M.; Ładyga, M. Effects of Endurance Training on Functional Status of the Respiratory Muscles in Healthy Men. Pol. J. Sport Tour. 2017, 24, 235–241. [Google Scholar] [CrossRef]
- Eastwood, P.R.; Hillman, D.R.; Finucane, K.E. Inspiratory Muscle Performance in Endurance Athletes and Sedentary Subjects. Respirology 2001, 6, 95–104. [Google Scholar] [CrossRef]
- Coast, J.R.; Clifford, P.S.; Henrich, T.W.; Stray-Gundersen, J.; Johnson, R.L., Jr. Maximal Inspiratory Pressure Following Maximal Exercise in Trained and Untrained Subjects. Med. Sci. Sports Exerc. 1990, 22, 811–815. [Google Scholar] [CrossRef]
- Leith, D.E.; Bradley, M. Ventilatory Muscle Strength and Endurance Training. J. Appl. Physiol. 1976, 41, 508–516. [Google Scholar] [CrossRef] [PubMed]
- HajGhanbari, B.; Yamabayashi, C.; Buna, T.R.; Coelho, J.D.; Freedman, K.D.; Morton, T.A.; Palmer, S.A.; Toy, M.A.; Walsh, C.; Sheel, A.W.; et al. Effects of Respiratory Muscle Training on Performance in Athletes: A Systematic Review with Meta-Analyses. J. Strength Cond. Res. 2013, 27, 1643–1663. [Google Scholar] [CrossRef]
- Illi, S.K.; Held, U.; Frank, I.; Spengler, C.M. Effect of Respiratory Muscle Training on Exercise Performance in Healthy Individuals: A Systematic Review and Meta-Analysis. Sports Med. 2012, 42, 707–724. [Google Scholar] [CrossRef]
- Kowalski, T.; Granda, D.; Klusiewicz, A. Practical Application of Respiratory Muscle Training in Endurance Sports. Strength Cond. J. 2024, 10-1519. [Google Scholar] [CrossRef]
- Sales, A.T.; Fregonezi, G.A.; Ramsook, A.H.; Guenette, J.A.; Lima, I.N.; Reid, W.D. Respiratory Muscle Endurance after Training in Athletes and Non-Athletes: A Systematic Review and Meta-Analysis. Phys. Ther. Sport 2016, 17, 76–86. [Google Scholar] [CrossRef]
- Álvarez-Herms, J.; Julià-Sánchez, S.; Corbi, F.; Odriozola-Martínez, A.; Burtscher, M. Putative Role of Respiratory Muscle Training to Improve Endurance Performance in Hypoxia: A Review. Front. Physiol. 2018, 9, 1970. [Google Scholar] [CrossRef]
- Wiecha, S.; Kasiak, P.S.; Szwed, P.; Kowalski, T.; Cieśliński, I.; Postuła, M.; Klusiewicz, A. VO2max Prediction Based on Submaximal Cardiorespiratory Relationships and Body Composition in Male Runners and Cyclists: A Population Study. Elife 2023, 12, e86291. [Google Scholar] [CrossRef]
- Dempsey, J.A.; Romer, L.; Rodman, J.; Miller, J.; Smith, C. Consequences of Exercise-Induced Respiratory Muscle Work. Respir. Physiol. Neurobiol. 2006, 151, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Illidi, C.R.; Romer, L.M.; Johnson, M.A.; Williams, N.C.; Rossiter, H.B.; Casaburi, R.; Tiller, N.B. Distinguishing Science from Pseudoscience in Commercial Respiratory Interventions: An Evidence-Based Guide for Health and Exercise Professionals. Eur. J. Appl. Physiol. 2023, 8, 1599–1625. [Google Scholar] [CrossRef] [PubMed]
- Witt, J.D.; Guenette, J.A.; Rupert, J.L.; McKenzie, D.C.; Sheel, A.W. Inspiratory Muscle Training Attenuates the Human Respiratory Muscle Metaboreflex. J. Physiol. 2007, 584, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Sheel, A.W.; Boushel, R.; Dempsey, J.A. Competition for Blood Flow Distribution between Respiratory and Locomotor Muscles: Implications for Muscle Fatigue. J. Appl. Physiol. 2018, 125, 820–831. [Google Scholar] [CrossRef]
- Aliverti, A. The Respiratory Muscles during Exercise. Breathe 2016, 12, 165–168. [Google Scholar] [CrossRef]
- Tong, T.K.; Wu, S.; Nie, J.; Baker, J.S.; Lin, H. The Occurrence of Core Muscle Fatigue during High-Intensity Running Exercise and Its Limitation to Performance: The Role of Respiratory Work. J. Sports Sci. Med. 2014, 13, 244–251. [Google Scholar]
- Sheikhhassani, S.; Rajabi, R.; Minoonejad, H. Effect of Core Muscle Fatigue on Measurements of Lower Extremity Functional Performance in Male Athletes. J. Res. Rehabil. Sci. 2013, 9, 4. [Google Scholar] [CrossRef]
- Willson, J.D.; Dougherty, C.P.; Ireland, M.L.; Davis, I.M. Core Stability and Its Relationship to Lower Extremity Function and Injury. J. Am. Acad. Orthop. Surg. 2005, 13, 316–325. [Google Scholar] [CrossRef] [PubMed]
- De Blaiser, C.; Roosen, P.; Willems, T.; Danneels, L.; Bossche, L.V.; De Ridder, R. Is Core Stability a Risk Factor for Lower Extremity Injuries in an Athletic Population? A Systematic Review. Phys. Ther. Sport 2018, 30, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.L.C.; Hall, E.; Maior, A.S. Inspiratory Muscle Training Improves Performance of a Repeated Sprints Ability Test in Professional Soccer Players. J. Bodyw. Mov. Ther. 2019, 23, 452–455. [Google Scholar] [CrossRef]
- Archiza, B.; Andaku, D.K.; Caruso, F.C.R.; Bonjorno, J.C.; de Oliveira, C.R.; Ricci, P.A.; do Amaral, A.C.; Mattiello, S.M.; Libardi, C.A.; Phillips, S.A.; et al. Effects of Inspiratory Muscle Training in Professional Women Football Players: A Randomized Sham-Controlled Trial. J. Sports Sci. 2018, 36, 771–780. [Google Scholar] [CrossRef]
- Brown, P.I.; Sharpe, G.R.; Johnson, M.A. Inspiratory Muscle Training Reduces Blood Lactate Concentration during Volitional Hyperpnoea. Eur. J. Appl. Physiol. 2008, 104, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Spengler, C.M.; Roos, M.; Laube, S.M.; Boutellier, U. Decreased Exercise Blood Lactate Concentrations after Respiratory Endurance Training in Humans. Eur. J. Appl. Physiol. Occup. Physiol. 1999, 79, 299–305. [Google Scholar] [CrossRef]
- Fregosi, R.F.; Dempsey, J.A. Effects of Exercise in Normoxia and Acute Hypoxia on Respiratory Muscle Metabolites. J. Appl. Physiol. 1986, 60, 1274–1283. [Google Scholar] [CrossRef] [PubMed]
- Rochester, D.F.; Briscoe, A.M. Metabolism of the Working Diaphragm. Am. Rev. Respir. Dis. 1979, 119, 101–106. [Google Scholar]
- Bernhardsen, G.P.; Stang, J.; Halvorsen, T.; Stensrud, T. Differences in Lung Function, Bronchial Hyperresponsiveness and Respiratory Health between Elite Athletes Competing in Different Sports. Eur. J. Sport Sci. 2023, 23, 1480–1489. [Google Scholar] [CrossRef]
- Martín-Valero, R.; Jimenez-Cebrian, A.M.; Moral-Munoz, J.A.; de-la-Casa-Almeida, M.; Rodriguez-Huguet, M.; Casuso-Holgado, M.J. The Efficacy of Therapeutic Respiratory Muscle Training Interventions in People with Bronchiectasis: A Systematic Review and Meta-Analysis. J. Clin. Med. Res. 2020, 9, 231. [Google Scholar] [CrossRef]
- Tout, R.; Tayara, L.; Halimi, M. The Effects of Respiratory Muscle Training on Improvement of the Internal and External Thoraco-Pulmonary Respiratory Mechanism in COPD Patients. Ann. Phys. Rehabil. Med. 2013, 56, 193–211. [Google Scholar] [CrossRef] [PubMed]
- Sandbakk, Ø.; Pyne, D.B.; McGawley, K.; Foster, C.; Talsnes, R.K.; Solli, G.S.; Millet, G.P.; Seiler, S.; Laursen, P.B.; Haugen, T.; et al. The Evolution of World-Class Endurance Training: The Scientist’s View on Current and Future Trends. Int. J. Sports Physiol. Perform. 2023, 18, 885–889. [Google Scholar] [CrossRef] [PubMed]
- ISU World Cup Speed Skating. Available online: https://www.isu.org/speed-skating/events/world-cup-speed-skating (accessed on 1 October 2023).
- Klusiewicz, A.; Borkowski, L.; Zdanowicz, R.; Boros, P.; Wesołowski, S. The Inspiratory Muscle Training in Elite Rowers. J. Sports Med. Phys. Fit. 2008, 48, 279–284. [Google Scholar]
- McConnell, A. Breathe Strong, Perform Better; Human Kinetics: Champaign, IL, USA, 2011; ISBN 9780736091695. [Google Scholar]
- Lukanova-Jakubowska, A.; Piechota, K.; Ozimek, M.; Borkowski, L.; Klusiewicz, A. Assessment of aerobic and anaerobic exercise capacity and sport level of Poland’s leading representative in a short track in a 4-year Olympic cycle. Acta Kinesiol. 2021, 15, 32–41. [Google Scholar] [CrossRef]
- Catunao, C. Performance-Related Characteristics of Elite Short Track Speed Skaters. In Proceedings of the Meeting of the Minds, Marshall, MN, USA, 16–17 May 2019. [Google Scholar]
- Deguire, S.; Sandford, G.N.; Bieuzen, F. Anaerobic Speed Reserve and Performance Relationships Between International and World-Class Short-Track Speed Skating. Int. J. Sports Physiol. Perform. 2023, 18, 1196–1205. [Google Scholar] [CrossRef]
- McKay, A.K.A.; Stellingwerff, T.; Smith, E.S.; Martin, D.T.; Mujika, I.; Goosey-Tolfrey, V.L.; Sheppard, J.; Burke, L.M. Defining Training and Performance Caliber: A Participant Classification Framework. Int. J. Sports Physiol. Perform. 2022, 17, 317–331. [Google Scholar] [CrossRef]
- Notter, D.A.; Verges, S.; Renggli, A.S.; Beltrami, F.G.; Spengler, C.M. Similar Effects on Exercise Performance Following Different Respiratory Muscle Training Programs in Healthy Young Men. Sci. Rep. 2023, 13, 16135. [Google Scholar] [CrossRef]
- Gaskill, S.E.; Ruby, B.C.; Walker, A.J.; Sanchez, O.A.; Serfass, R.C.; Leon, A.S. Validity and Reliability of Combining Three Methods to Determine Ventilatory Threshold. Med. Sci. Sports Exerc. 2001, 33, 1841–1848. [Google Scholar] [CrossRef]
- Boone, J.; Bourgois, J. The Oxygen Uptake Response to Incremental Ramp Exercise: Methodogical and Physiological Issues. Sports Med. 2012, 42, 511–526. [Google Scholar] [CrossRef]
- Graham, B.L.; Steenbruggen, I.; Miller, M.R.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, e70–e88. [Google Scholar] [CrossRef]
- Kowalski, T.; Klusiewicz, A. POWERbreathe® S-Index Test—Guidelines and Recommendations for Practitioners. Biomed. Hum. Kinet. 2023, 15, 225–228. [Google Scholar] [CrossRef]
- Klusiewicz, A.; Starczewski, M.; Sadowska, D.; Ładyga, M. Effect of High- and Low-Resistance Inspiratory Muscle Training on Physiological Response to Exercise in Cross-Country Skiers. J. Sports Med. Phys. Fit. 2019, 59, 1156–1161. [Google Scholar] [CrossRef] [PubMed]
- Mueller, G.; Hopman, M.T.E.; Perret, C. Comparison of Respiratory Muscle Training Methods in Individuals with Motor and Sensory Complete Tetraplegia: A Randomized Controlled Trial. J. Rehabil. Med. 2013, 45, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Journal of Physical Education and Sport; Physical Education and Sport Faculty: Abiko, Japan, 2018; Volume 2018.
- Coyle, E.F. Physiological Determinants of Endurance Exercise Performance. J. Sci. Med. Sport 1999, 2, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Cordain, L.; Stager, J. Pulmonary Structure and Function in Swimmers. Sports Med. 1988, 6, 271–278. [Google Scholar] [CrossRef]
- Faghy, M.A.; Brown, P.I. Training the Inspiratory Muscles Improves Running Performance When Carrying a 25 Kg Thoracic Load in a Backpack. Eur. J. Sport Sci. 2016, 16, 585–594. [Google Scholar] [CrossRef]
- Kowalski, T.; Kasiak, P.; Rebis, K.; Klusiewicz, A.; Granda, D.; Wiecha, S. Respiratory Muscle Training Induces Additional Stress and Training Load in Well-Trained Triathletes-Randomized Controlled Trial. Front. Physiol. 2023, 14, 1264265. [Google Scholar] [CrossRef]
- Griffiths, L.A.; McConnell, A.K. The Influence of Inspiratory and Expiratory Muscle Training upon Rowing Performance. Eur. J. Appl. Physiol. 2007, 99, 457–466. [Google Scholar] [CrossRef]
- Shei, R.-J.; Chapman, R.F.; Gruber, A.H.; Mickleborough, T.D. Inspiratory Muscle Training Improves Exercise Capacity with Thoracic Load Carriage. Physiol. Rep. 2018, 6, e13558. [Google Scholar] [CrossRef]
- Shei, R.-J.; Paris, H.L.; Sogard, A.S.; Mickleborough, T.D. Time to Move Beyond a “One-Size Fits All” Approach to Inspiratory Muscle Training. Front. Physiol. 2022, 12, 766346. [Google Scholar] [CrossRef]
- Millet, G.P.; Brocherie, F.; Burtscher, J. Olympic Sports Science—Bibliometric Analysis of All Summer and Winter Olympic Sports Research. Front. Sports Act. Living 2021, 3, 772140. [Google Scholar] [CrossRef] [PubMed]
| Variable/Group | IPTL (n = 8) | VIH (n = 8) |
|---|---|---|
| Age (years) | 23.06 ± 2.36 | 22.18 ± 2.64 |
| Body mass (kg) | 67.96 ± 8.78 | 69.0 ± 9.70 |
| Body height (cm) | 172.88 ± 6.49 | 175.12 ± 7.90 |
| Body fat (%) | 11.15 ± 4.43 | 13.66 ± 5.49 |
| VO2max (mL·min−1·kg−1) | 56.88 ± 6.36 | 53.13 ± 7.64 |
| Training experience (years) | 11.92 ± 3.06 | 12.1 ± 3.43 |
| Session Number | Session Length (Minutes) | Breathing Frequency (Breaths per Minute) | Session Number | Session Length (Minutes) | Breathing Frequency (Breaths per Minute) |
|---|---|---|---|---|---|
| 1 | 3 | 20 | 12 | 13 | 22 |
| 2 | 4 | 20 | 13 | 14 | 24 |
| 3 | 5 | 20 | 14 | 15 | 24 |
| 4 | 5 | 20 | 15 | 16 | 24 |
| 5 | 6 | 22 | 16 | 17 | 24 |
| 6 | 7 | 22 | 17 | 18 | 44 |
| 7 | 8 | 22 | 18 | 18 | 26 |
| 8 | 9 | 22 | 19 | 19 | 26 |
| 9 | 10 | 22 | 20 | 20 | 26 |
| 10 | 11 | 22 | 21 | 20 | 26 |
| 11 | 12 | 22 |
| Variables/Group | IPTL (n = 7) | VIH (n = 7) | p-Value | ||
|---|---|---|---|---|---|
| Before | After | Before | After | ||
| PmaxWAnT (W·kg−1) | 13.56 ± 1.70 | 13.04 ± 1.56 | 12.98 ± 1.23 | 13.11 ± 0.81 | 0.068 |
| TW-AnC (kJ·kg−1) | 4.68 ± 0.48 | 4.57 ± 0.34 | 4.41 ± 0.45 | 4.52 ± 0.24 | 0.101 |
| bLaWAnT (mmol·L−1) | 16.59 ± 2.73 | 13.30 ± 2.10 | 15.94 ± 1.60 | 14.88 ± 1.12 | 0.861 |
| Variables/Group | IPTL (n = 7) | VIH (n = 8) | p-Value | ||
|---|---|---|---|---|---|
| Before | After | Before | After | ||
| PmaxCPET (W·kg−1) | 4.82 ± 0.59 | 4.78 ± 0.62 | 4.47 ± 0.61 | 4.03 ± 1.68 | 0.302 |
| VO2max (mL·min−1·kg−1) | 56.88 ± 6.34 | 56.375 ± 7.50 | 54.43 ± 7.23 | 54.71 ± 5.91 | 0.510 |
| HRmax (bpm) | 196.62 ± 8.23 | 191.00 ± 13.75 | 192.25 ± 6.84 | 188.43 ± 6.58 | 0.560 |
| VEmax (L·min−1) | 162.82 ± 33.73 | 157.60 ± 32.41 | 153.77 ± 39.50 | 164.27 ± 31.53 | 0.274 |
| BFmax (brpm) | 61.13 ± 6.20 | 55.00 ± 5.93 | 55.43 ± 6.13 | 58.43 ± 8.67 | 0.009 |
| TVmax | 2.88 ± 0.47 | 2.86 ± 0.48 | 2.80 ± 0.77 | 2.92 ± 0.69 | 0.965 |
| RERmax | 1.15 ± 0.04 | 1.18 ± 0.05 | 1.15 ± 0.04 | 1.21 ± 0.03 | 0.318 |
| bLaMaxCPET (mmol·L−1) | 14.30 ± 2.87 | 11.92 ± 2.40 | 12.99 ± 3.69 | 13.20 ± 2.29 | 0.180 |
| Variables/Group | IPTL (n = 8) | VIH (n = 8) | p-Value | ||
|---|---|---|---|---|---|
| Before | After | Before | After | ||
| FVC (L) | 5.61 ± 1.06 | 5.38 ± 0.84 | 5.31 ± 1.03 | 5.21 ± 1.06 | 0.604 |
| FEV1 (L) | 4.44 ± 0.71 | 4.42 ± 0.65 | 4.65 ± 1.03 | 4.54 ± 1.06 | 0.591 |
| FEV1/FVC | 79.98 ± 9.61 | 82.68 ± 6.26 | 87.14 ± 6.55 | 86.76 ± 8.87 | 0.326 |
| PEF (L·min−1) | 6.62 ± 2.09 | 7.97 ± 2.71 | 8.77 ± 2.93 | 8.88 ± 3.22 | 0.323 |
| S-Index Test Score (cmH2O) | 142.39 ± 26.96 | 141.64 ± 22.84 | 137.83 ± 29.57 | 152.00 ± 29.53 | 0.065 |
| Variables/Group | IPTL (n = 7) | VIH (n = 8) | p-Value | ||
|---|---|---|---|---|---|
| Before | After | Before | After | ||
| VT1-HR (bpm) | 163.50 ± 13.89 | 164.38 ± 17.57 | 153.00 ± 11.55 | 156.43 ± 4.83 | 0.455 |
| VT1-P (W·kg−1) | 2.81 ± 0.77 | 3.06 ± 0.68 | 2.52 ± 1.04 | 2.85 ± 0.65 | 0.564 |
| VT1-VE (L·min−1) | 63.51 ± 16.95 | 73.575 ± 14.69 | 59.94 ± 22.04 | 67.70 ± 14.94 | 0.876 |
| VT1-BF (brpm) | 29.75 ± 6.089 | 32.38 ± 5.50 | 27.75 ± 4.39 | 30.09 ± 5.08 | 0.618 |
| VT1-TV (L) | 2.13 ± 0.29 | 2.28 ± 0.39 | 2.16 ± 0.65 | 2.25 ± 0.46 | 0.703 |
| VT2-HR (bpm) | 182.66 ± 10.34 | 178.63 ± 16.13 | 174.75 ± 12.209 | 174.57 ± 5.41 | 0.263 |
| VT2-P (W·kg−1) | 3.90 ± 0.83 | 4.50 ± 0.85 | 3.36 ± 1.06 | 3.69 ± 0.77 | 0.124 |
| VT2-VE (L·min−1) | 92.93 ± 17.85 | 98.76 ± 16.95 | 85.80 ± 25.79 | 101.53 ± 18.40 | 0.579 |
| VT2-BF (brpm) | 38.13 ± 5.64 | 39.50 ± 4.18 | 35.75 ± 4.95 | 40.71 ± 4.99 | 0.216 |
| VT2-TV (L) | 2.44 ± 0.38 | 2.51 ± 0.36 | 2.41 ± 0.76 | 2.49 ± 0.60 | 0.945 |
| Variables/Group | IPTL (n = 7) | VIH (n = 8) | p-Value | ||
|---|---|---|---|---|---|
| Before | After | Before | After | ||
| FLT (s/lap) | 8.83 ± 0.47 | 8.62 ± 0.22 | 9.03 ± 0.68 | 8.70 ± 0.35 | 0.394 |
| RS-ALT (s/lap) | 9.27 ± 0.09 | 9.21 ± 0.27 | 9.49 ± 0.32 | 9.29 ± 0.33 | 0.334 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kowalski, T.; Klusiewicz, A.; Rębiś, K.; Wilk, A.; Starczewski, M. Comparative Study of Different Respiratory Muscle Training Methods: Effects on Cardiopulmonary Indices and Athletic Performance in Elite Short-Track Speedskaters. Life 2024, 14, 1159. https://doi.org/10.3390/life14091159
Kowalski T, Klusiewicz A, Rębiś K, Wilk A, Starczewski M. Comparative Study of Different Respiratory Muscle Training Methods: Effects on Cardiopulmonary Indices and Athletic Performance in Elite Short-Track Speedskaters. Life. 2024; 14(9):1159. https://doi.org/10.3390/life14091159
Chicago/Turabian StyleKowalski, Tomasz, Andrzej Klusiewicz, Kinga Rębiś, Adrian Wilk, and Michał Starczewski. 2024. "Comparative Study of Different Respiratory Muscle Training Methods: Effects on Cardiopulmonary Indices and Athletic Performance in Elite Short-Track Speedskaters" Life 14, no. 9: 1159. https://doi.org/10.3390/life14091159







