Efficacy and Challenges in the Treatment of Diastasis Recti Abdominis—A Scoping Review on the Current Trends and Future Perspectives
Abstract
:1. Introduction
- To analyze the different diagnostic and treatment procedures associated with DRA.
- To analyze the challenges involved in the assessment of treatment and rehabilitation procedures.
- To highlight the potential research gaps and future trends relating to the treatment of DRA.
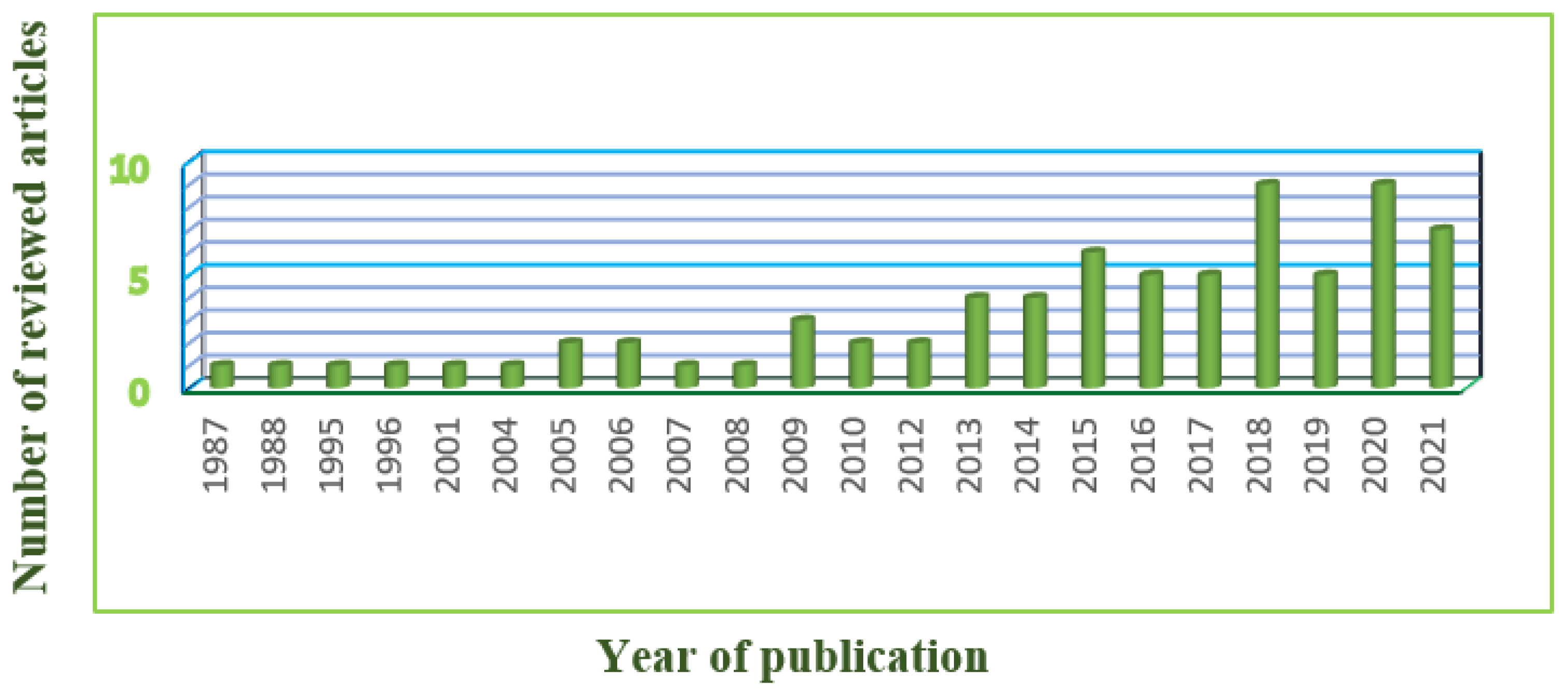
2. Search Strategy and Organization of the Review
3. DRA—A Walkthrough
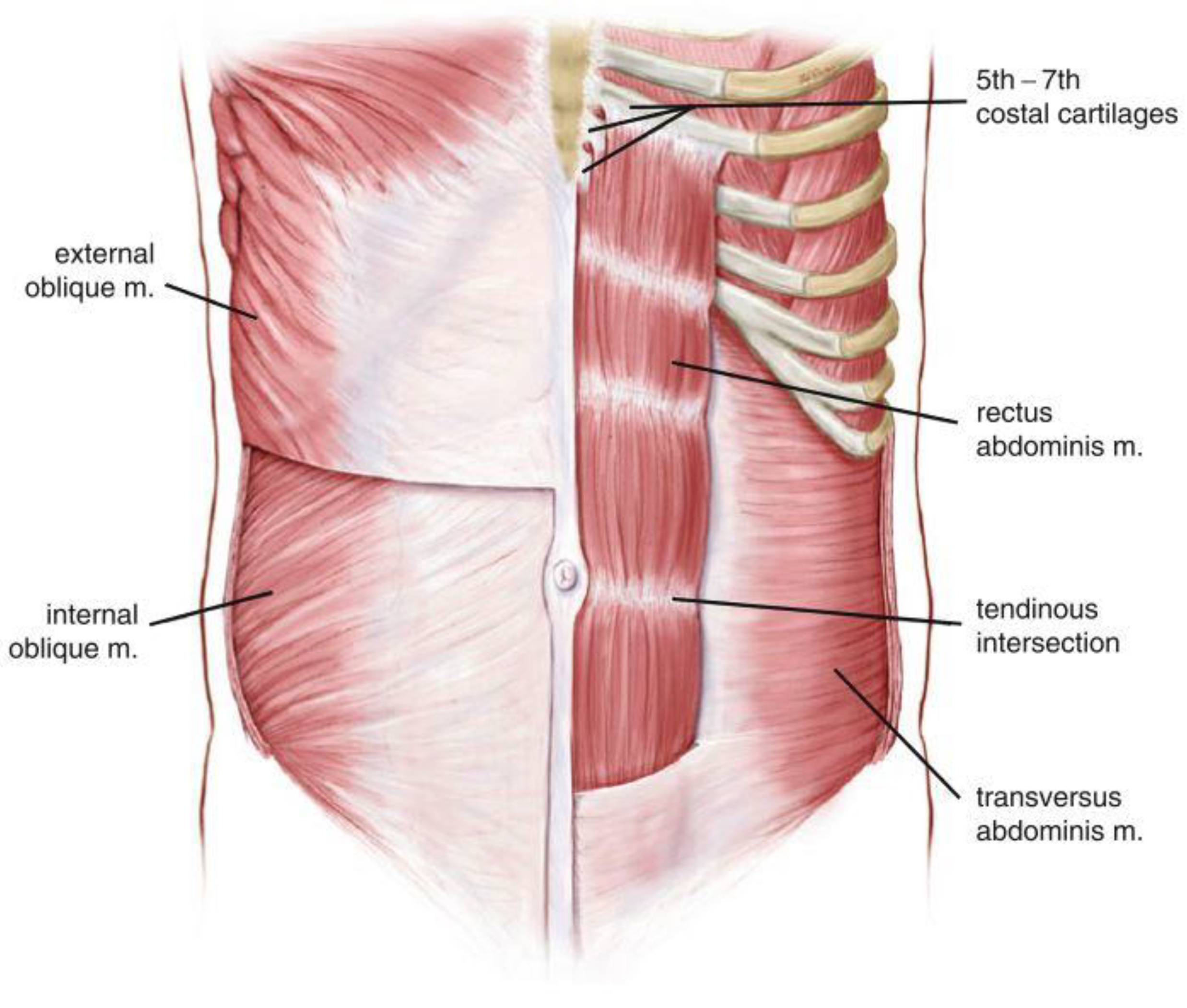
3.1. Anatomy of Rectus Abdominis Muscle
3.2. Morphological Changes in DRA
3.3. Width of the Linea Alba
3.4. Measurement Methods

4. Treatment
4.1. Conservative Treatment
4.1.1. Non-Exercise Physical Therapy
4.1.2. Physical Exercise Therapy
4.2. Surgery
4.2.1. Open Approach
4.2.2. Laparoscopic Approach
4.2.3. Endoscopic Approach
5. Diagnostic Techniques for the Rehabilitation of DRA
5.1. Electromyography
5.2. Ultrasound Imaging
6. Discussion
6.1. Impact of Exercises
6.2. Need for a Biofeedback Device
6.3. Scope of Automation
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Choo, H.J.; Hwang, S.K.; Hynes, C.K. Musculoskeletal Issues and Care for Pregnant and Postpartum Women. Curr. Phys. Med. Rehabil. Rep. 2020, 8, 493–500. [Google Scholar] [CrossRef]
- Campanelli, G. (Ed.) The Art of Hernia Surgery; Springer International Publishing: Cham, Switzerland, 2018. [Google Scholar] [CrossRef]
- Bø, K.; Hilde, G.; Tennfjord, M.; Sperstad, J.; Engh, M.E. Diastasis recti abdominis and pelvic floor muscle function. A cross sectional study of primiparous women during pregnancy and postpartum. Physiotherapy 2015, 101, e161–e162. [Google Scholar] [CrossRef] [Green Version]
- da Mota, P.G.F.; Pascoal, A.G.B.A.; Carita, A.I.; Bø, K. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man. Ther. 2015, 20, 200–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fei, H.; Liu, Y.; Li, M.; He, J.; Liu, L.; Li, J.; Wan, Y.; Li, T. The relationship of severity in diastasis recti abdominis and pelvic floor dysfunction: A retrospective cohort study. BMC Women’s Health 2021, 21, 68. [Google Scholar] [CrossRef]
- Hills, N.F.; Graham, R.B.; McLean, L. Comparison of Trunk Muscle Function Between Women With and Without Diastasis Recti Abdominis at 1 Year Postpartum. Phys. Ther. 2018, 98, 891–901. [Google Scholar] [CrossRef] [Green Version]
- Parker, M.A.; Millar, L.A.; Dugan, S.A. Diastasis Rectus Abdominis and Lumbo-Pelvic Pain and Dysfunction-Are They Related? J. Women’s Health Phys. Ther. 2009, 33, 15–22. [Google Scholar] [CrossRef] [Green Version]
- Rath, A.M.; Attali, P.; Dumas, J.L.; Goldlust, D.; Zhang, J.; Chevrel, J.P. The abdominal linea alba: An anatomo-radiologic and biomechanical study. Surg. Radiol. Anat. 1996, 18, 281–288. [Google Scholar] [CrossRef]
- Nakip, G.; Akbayrak, T.; Çinar, G.N.; Üzelpasacı, E.; Baran, E.; Orhan, C.; Özgül, S.; Beksaç, M.S. AB1389-Hpr The Association Between the Amount of Diastasis Recti Abdominis and the Strength of Abdominal Muscles in Pregnant Women. In Proceedings of the Annual European Congress of Rheumatology, EULAR 2019, Madrid, Spain, 12–15 June 2019. [Google Scholar] [CrossRef] [Green Version]
- Sperstad, J.B.; Tennfjord, M.K.; Hilde, G.; Ellström-Engh, M.; Bø, K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: Prevalence, risk factors and report of lumbopelvic pain. Br. J. Sports Med. 2016, 50, 1092–1096. [Google Scholar] [CrossRef] [Green Version]
- Keshwani, N.; Mathur, S.; McLean, L. Relationship Between Interrectus Distance and Symptom Severity in Women with Diastasis Recti Abdominis in the Early Postpartum Period. Phys. Ther. 2017, 98, 182–190. [Google Scholar] [CrossRef] [Green Version]
- Spitznagle, T.M.; Leong, F.C.; Van Dillen, L.R. Prevalence of diastasis recti abdominis in a urogynecological patient population. Int. Urogynecology J. 2006, 18, 321–328. [Google Scholar] [CrossRef]
- Harada, B.S.; De Bortolli, T.T.; Carnaz, L.; De Conti, M.H.S.; Hijaz, A.; Driusso, P.; Marini, G. Diastasis recti abdominis and pelvic floor dysfunction in peri- and postmenopausal women: A cross-sectional study. Physiother. Theory Pract. 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Doubkova, L.; Andel, R.; Palascakova-Springrova, I.; Kolar, P.; Kriz, J.; Kobesova, A. Diastasis of rectus abdominis muscles in low back pain patients. J. Back Musculoskelet. Rehabil. 2018, 31, 107–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crommert, M.E.; Fieril, K.P.; Gustavsson, C. Women’s experiences of living with increased inter-recti distance after childbirth: An interview study. BMC Women’s Health 2020, 20, 260. [Google Scholar] [CrossRef]
- Fiori, F.; Ferrara, F.; Gobatti, D.; Gentile, D.; Stella, M. Surgical treatment of diastasis recti: The importance of an overall view of the problem. Hernia 2020, 25, 871–882. [Google Scholar] [CrossRef]
- Emanuelsson, P.; Gunnarsson, U.; Strigård, K.; Stark, B. Early complications, pain, and quality of life after reconstructive surgery for abdominal rectus muscle diastasis: A 3-month follow-up. J. Plast. Reconstr. Aesthetic Surg. 2014, 67, 1082–1088. [Google Scholar] [CrossRef] [Green Version]
- Kulhanek, J.; Mestak, O. Treatment of umbilical hernia and recti muscles diastasis without a periumbilical incision. Hernia 2013, 17, 527–530. [Google Scholar] [CrossRef]
- Gandhi, J.A.; Shinde, P.; Kothari, B.; Churiwala, J.J.; Banker, A. Endoscopic Pre-aponeurotic Repair (EPAR) Technique with Meshplasty for Treatment of Ventral Hernia and Rectus Abdominis Diastasis. Indian J. Surg. 2020, 1–5. [Google Scholar] [CrossRef]
- Claus, C.M.P.; Malcher, F.; Cavazzola, L.T.; Furtado, M.; Morrell, A.; Azevedo, M.; Meirelles, L.G.; Santos, H.; Garcia, R. Subcutaneous Onlay Laparoscopic Approach (Scola) for Ventral Hernia and Rectus Abdominis Diastasis Repair: Technical Description and Initial Results. Arq. Bras. Cir. Dig. 2018, 31, e1399. [Google Scholar] [CrossRef] [Green Version]
- Nahas, F.X.; Ferreira, L.M.; Mendes, J.D.A. An Efficient Way to Correct Recurrent Rectus Diastasis. Aesthetic Plast. Surg. 2004, 28, 189–196. [Google Scholar] [CrossRef]
- Draghi, F.; Cocco, G.; Richelmi, F.M.; Schiavone, C. Abdominal wall sonography: A pictorial review. J. Ultrasound 2020, 23, 265–278. [Google Scholar] [CrossRef]
- Shiffman, M.A.; di Giuseppe, A. (Eds.) Cosmetic Surgery; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar] [CrossRef]
- Mota, P.; Pascoal, A.G.; Vaz, C.; João, F.; Veloso, A.; Bø, K. Diastasis Recti During Pregnancy and Postpartum. In Women’s Health and Biomechanics; Springer International Publishing: Cham, Switzerland, 2018; pp. 121–132. [Google Scholar] [CrossRef]
- Puri, J.; Sharma, S.; Samuel, A.J.; Chahal, A. Investigate Correlation between Diastasis of Rectus Abdominis Muscle and Low Back Pain in Obese Women. J. Lifestyle Med. 2021, 11, 38–42. [Google Scholar] [CrossRef]
- Cardaillac, C.; Vieillefosse, S.; Oppenheimer, A.; Joueidi, Y.; Thubert, T.; Deffieux, X. Diastasis of the rectus abdominis muscles in postpartum: Concordance of patient and clinician evaluations, prevalence, associated pelvic floor symptoms and quality of life. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 252, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Beer, G.M.; Schuster, A.; Seifert, B.; Manestar, M.; Mihic-Probst, D.; Weber, S.A. The normal width of the linea alba in nulliparous women. Clin. Anat. 2009, 22, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Mota, P.; Gil Pascoal, A.; Carita, A.I.; Bø, K. Normal width of the inter-recti distance in pregnant and postpartum primiparous women. Musculoskelet. Sci. Pract. 2018, 35, 34–37. [Google Scholar] [CrossRef] [PubMed]
- Bursch, S.G. Interrater Reliability of Diastasis Recti Abdominis Measurement. Phys. Ther. 1987, 67, 1077–1079. [Google Scholar] [CrossRef]
- Boissonnault, J.S.; Blaschak, M.J. Incidence of Diastasis Recti Abdominis During the Childbearing Year. Phys. Ther. 1988, 68, 1082–1086. [Google Scholar] [CrossRef]
- Mota, P.; Gil Pascoal, A.; Sancho, F.; Carita, A.I.; Bø, K. Reliability of the inter-rectus distance measured by palpation. Comparison of palpation and ultrasound measurements. Man. Ther. 2013, 18, 294–298. [Google Scholar] [CrossRef] [Green Version]
- Qu, E.; Wu, J.; Zhang, M.; Wu, L.; Zhang, T.; Xu, J.; Zhang, X. The ultrasound diagnostic criteria for diastasis recti and its correlation with pelvic floor dysfunction in early postpartum women. Quant. Imaging Med. Surg. 2021, 11, 706–713. [Google Scholar] [CrossRef]
- Available online: https://dreamplasticsurgery.com/medical-surgery/diastasis-recti/ (accessed on 10 January 2022).
- El-Mekawy, H.S.; Eldeeb, A.M.; Lythy, M.A.E.; El-Begawy, A.F. Effect Of Abdominal Exercises Versus Abdominal Supporting Belt On Post-Partum Abdominal Efficiency And Rectus Separation. Int. J. Med. Health Sci. 2013, 7, 75–79. [Google Scholar] [CrossRef]
- Keshwani, N.; Mathur, S.; McLean, L. The impact of exercise therapy and abdominal binding in the management of diastasis recti abdominis in the early post-partum period: A pilot randomized controlled trial. Physiother. Theory Pract. 2019, 37, 1018–1033. [Google Scholar] [CrossRef]
- Tuttle, L.J.; Fasching, J.; Keller, A.; Patel, M.; Saville, C.; Schlaff, R.; Walker, A.; Mason, M.; Gombatto, S.P. Noninvasive Treatment of Postpartum Diastasis Recti Abdominis: A Pilot Study. J. Women’s Health Phys. Ther. 2018, 42, 65–75. [Google Scholar] [CrossRef]
- Kamel, D.M.; Yousif, A.M. Neuromuscular Electrical Stimulation and Strength Recovery of Postnatal Diastasis Recti Abdominis Muscles. Ann. Rehabil. Med. 2017, 41, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y. EP36.10: High-frequency ultrasonography for the evaluation of changes in postpartum rectus abdominis diastasis treated with electrical stimulation. Ultrasound Obstet. Gynecol. 2019, 54, 457. [Google Scholar] [CrossRef] [Green Version]
- Kirk, B.; Elliott-Burke, T. The effect of visceral manipulation on Diastasis Recti Abdominis (DRA): A case series. J. Bodyw. Mov. Ther. 2020, 26, 471–480. [Google Scholar] [CrossRef]
- Sancho, F.; Gil Pascoal, A.; Mota, P. An Ultrasound Study on the Effect of Exercise on Postpartum Women Inter-Rectus Abdominis Distance. J. Biomech. 2012, 45, S493. [Google Scholar] [CrossRef]
- Sancho, M.; Pascoal, A.; Mota, P.; Bø, K. Abdominal exercises affect inter-rectus distance in postpartum women: A two-dimensional ultrasound study. Physiotherapy 2015, 101, 286–291. [Google Scholar] [CrossRef] [Green Version]
- Gil Pascoal, A.; Dionisio, S.; Cordeiro, F.; Mota, P. Inter-rectus distance in postpartum women can be reduced by isometric contraction of the abdominal muscles: A preliminary case–control study. Physiotherapy 2014, 100, 344–348. [Google Scholar] [CrossRef]
- Mota, P.; Pascoal, A.; Carita, A.; Bø, K. Inter-recti distance at rest, during abdominal crunch and drawing in exercises during pregnancy and postpartum. Physiotherapy 2015, 101, e1050–e1051. [Google Scholar] [CrossRef] [Green Version]
- Mota, P.; Gil Pascoal, A.; Carita, A.I.; Bø, K. The Immediate Effects on Inter-rectus Distance of Abdominal Crunch and Drawing-in Exercises During Pregnancy and the Postpartum Period. J. Orthop. Sports Phys. Ther. 2015, 45, 781–788. [Google Scholar] [CrossRef]
- Da Cuña-Carrera, I.; Soto-González, M.; Alonso-Calvete, A.; González-González, Y.; Lantarón-Caeiro, E.M. Immediate effects of different types of abdominal exercises on the inter-rectus distance. Isokinet. Exerc. Sci. 2021, 29, 31–37. [Google Scholar] [CrossRef]
- Lee, D.; Hodges, P. Behaviour of the linea alba during a curl-up task in diastasis rectus abdominis: A new interpretation with clinical implications. Physiotherapy 2015, 101, e580–e581. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.; Hodges, P. Diastasis rectus abdominis—Should we open or close the gap? Musculoskelet. Sci. Pract. 2017, 28, e16. [Google Scholar] [CrossRef]
- Manetti, G.; Lolli, M.G.; Belloni, E.; Nigri, G. A new minimally invasive technique for the repair of diastasis recti: A pilot study. Surg. Endosc. 2021, 35, 4028–4034. [Google Scholar] [CrossRef]
- Wilhelmsson, S.; Olsén, M.F.; Staalesen, T.; Elander, A.; Nygren-Bonnier, M. Abdominal plasty with and without plication-effects on trunk muscles, lung function, and self-rated physical function. J. Plast. Surg. Hand Surg. 2016, 51, 199–204. [Google Scholar] [CrossRef]
- Nahas, F.X.; Augusto, S.M.; Ghelfond, C. Nylon versus Polydioxanone in the Correction of Rectus Diastasis. Plast. Reconstr. Surg. 2001, 107, 700–706. [Google Scholar] [CrossRef]
- Nahas, F.X.; Ferreira, L.M.; Augusto, S.M.; Ghelfond, C. Long-Term Follow-Up of Correction of Rectus Diastasis. Plast. Reconstr. Surg. 2005, 115, 1736–1741. [Google Scholar] [CrossRef]
- Nahas, F.X.; Ferreira, L.M.; Ely, P.B.; Ghelfond, C. Rectus Diastasis Corrected with Absorbable Suture: A Long-Term Evaluation. Aesthetic Plast. Surg. 2010, 35, 43–48. [Google Scholar] [CrossRef]
- Mestak, O.; Kullac, R.; Mestak, J.; Nosek, A.; Krajcova, A.; Sukop, A. Evaluation of the Long-Term Stability of Sheath Plication Using Absorbable Sutures in 51 Patients with Diastasis of the Recti Muscles. Plast. Reconstr. Surg. 2012, 130, 714e–719e. [Google Scholar] [CrossRef] [PubMed]
- Veríssimo, P.; Nahas, F.X.; Barbosa, M.V.J.; Gomes, H.F.D.C.; Ferreira, L.M. Is it Possible to Repair Diastasis Recti and Shorten the Aponeurosis at the Same Time? Aesthetic Plast. Surg. 2014, 38, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Mabrouk, A.A.; Helal, H.; Mahmoud, N.A. Abstract. Plast. Reconstr. Surg.-Glob. Open 2016, 4, 204–205. [Google Scholar] [CrossRef]
- Gama, L.J.M.; Barbosa, M.V.J.; Czapkowski, A.; Ajzen, S.; Ferreira, L.M.; Nahas, F.X. Single-Layer Plication for Repair of Diastasis Recti: The Most Rapid and Efficient Technique. Aesthetic Surg. J. 2017, 37, 698–705. [Google Scholar] [CrossRef] [Green Version]
- Köhler, G.; Fischer, I.; Kaltenböck, R.; Schrittwieser, R. Minimal Invasive Linea Alba Reconstruction for the Treatment of Umbilical and Epigastric Hernias with Coexisting Rectus Abdominis Diastasis. J. Laparoendosc. Adv. Surg. Tech. 2018, 28, 1223–1228. [Google Scholar] [CrossRef] [PubMed]
- Olsson, A.; Kiwanuka, O.; Wilhelmsson, S.; Sandblom, G.; Stackelberg, O. Cohort study of the effect of surgical repair of symptomatic diastasis recti abdominis on abdominal trunk function and quality of life. BJS Open 2019, 3, 750–758. [Google Scholar] [CrossRef] [PubMed]
- Swedenhammar, E.; Strigård, K.; Emanuelsson, P.; Gunnarsson, U.; Stark, B. Long-term follow-up after surgical repair of abdominal rectus diastasis: A Prospective Randomized Study. Scand. J. Surg. 2020, 110, 283–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emanuelsson, P.; Gunnarsson, U.; Dahlstrand, U.; Strigård, K.; Stark, B. Operative correction of abdominal rectus diastasis (ARD) reduces pain and improves abdominal wall muscle strength: A randomized, prospective trial comparing retromuscular mesh repair to double-row, self-retaining sutures. Surgery 2016, 160, 1367–1375. [Google Scholar] [CrossRef] [Green Version]
- Çintesun, E.; Çintesun, F.N.İ.; Aydoğdu, M.; Bayramoğlu, D.; Çelik, Ç. Effect of re-approximation of the rectus muscles on Diastasis Recti abdominis at cesarean section—A prospective cross-sectional study. Ginekol. Pol. 2021, 92, 132–136. [Google Scholar] [CrossRef]
- Palanivelu, C.; Rangarajan, M.; Jategaonkar, P.A.; Amar, V.; Gokul, K.S.; Srikanth, B. Laparoscopic repair of diastasis recti using the ‘Venetian blinds’ technique of plication with prosthetic reinforcement: A retrospective study. Hernia 2009, 13, 287–292. [Google Scholar] [CrossRef]
- Siddiky, A.H.; Kapadia, C.R. Laparoscopic plication of the linea alba as a repair for diastasis recti—A mesh free approach. J. Surg. Case Rep. 2010, 2010, 3. [Google Scholar] [CrossRef] [Green Version]
- Core, G.B.; Mizgala, C.L.; Bowen, J.C.; Vasconez, L.O. Endoscopic Abdominoplasty with Repair of Diastasis Recti and Abdominal Wall Hernia. Clin. Plast. Surg. 1995, 22, 707–722. [Google Scholar] [CrossRef]
- Luque, J.B.; Luque, A.B.; Valdivia, J.; Gráu, J.M.S.; Menchero, J.G.; Moreno, J.G.; Jurado, J.G. Totally endoscopic surgery on diastasis recti associated with midline hernias. The advantages of a minimally invasive approach. Prospective cohort study. Hernia 2014, 19, 493–501. [Google Scholar] [CrossRef]
- Köckerling, F.; Botsinis, M.D.; Rohde, C.; Reinpold, W. Endoscopic-Assisted Linea Alba Reconstruction plus Mesh Augmentation for Treatment of Umbilical and/or Epigastric Hernias and Rectus Abdominis Diastasis—Early Results. Front. Surg. 2016, 3, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carrara, A.; Catarci, M.; Fabris, L.; Zuolo, M.; Pellecchia, L.; Moscatelli, P.; Dorna, A.; Motter, M.; Pertile, R.; Tirone, G. Prospective observational study of abdominal wall reconstruction with THT technique in primary midline defects with diastasis recti: Clinical and functional outcomes in 110 consecutive patients. Surg. Endosc. 2020, 35, 5104–5114. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.; Lees, A.; Barton, G. An electromyographic investigation of abdominal exercises and the effects of fatigue. Ergonomics 2005, 48, 1604–1612. [Google Scholar] [CrossRef] [PubMed]
- Hwang, Y.-I.; Park, D.-J. Comparison of abdominal muscle activity during abdominal drawing-in maneuver combined with irradiation variations. J. Exerc. Rehabil. 2017, 13, 335–339. [Google Scholar] [CrossRef] [Green Version]
- Escamilla, R.F.; Babb, E.; DeWitt, R.; Jew, P.; Kelleher, P.; Burnham, T.; Busch, J.; D’Anna, K.; Mowbray, R.; Imamura, R.T. Electromyographic Analysis of Traditional and Nontraditional Abdominal Exercises: Implications for Rehabilitation and Training. Phys. Ther. 2006, 86, 656–671. [Google Scholar] [CrossRef]
- Hides, J.A.; Miokovic, T.; Belavý, D.L.; Stanton, W.R.; Richardson, C.A. Ultrasound Imaging Assessment of Abdominal Muscle Function During Drawing-in of the Abdominal Wall: An Intrarater Reliability Study. J. Orthop. Sports Phys. Ther. 2007, 37, 480–486. [Google Scholar] [CrossRef] [Green Version]
- Teyhen, D.S.; Rieger, J.L.; Westrick, R.B.; Miller, A.C.; Molloy, J.M.; Childs, J.D. Changes in Deep Abdominal Muscle Thickness During Common Trunk-Strengthening Exercises Using Ultrasound Imaging. J. Orthop. Sports Phys. Ther. 2008, 38, 596–605. [Google Scholar] [CrossRef] [Green Version]
- Larivière, C.; Pt, S.M.H.; Pt, D.H.G.; Pt, R.P.; Pt, J.D.; Dumas, J.-P. Ultrasound Measures of the Abdominal Wall in Patients with Low Back Pain Before and After an 8-week Lumbar Stabilization Exercise Program, and Their Association with Clinical Outcomes. PM&R 2018, 11, 710–721. [Google Scholar] [CrossRef]
- Aboufazeli, M.; Afshar-Mohajer, N. Within-day and between-day reliability of thickness measurements of abdominal muscles using ultrasound during abdominal hollowing and bracing maneuvers. J. Bodyw. Mov. Ther. 2017, 22, 122–128. [Google Scholar] [CrossRef]
- Pirri, C.; Todros, S.; Fede, C.; Pianigiani, S.; Fan, C.; Foti, C.; Stecco, C.; Pavan, P. Inter-rater reliability and variability of ultrasound measurements of abdominal muscles and fasciae thickness. Clin. Anat. 2019, 32, 948–960. [Google Scholar] [CrossRef]
- Fan, C.; Guidolin, D.; Ragazzo, S.; Fede, C.; Pirri, C.; Gaudreault, N.; Porzionato, A.; Macchi, V.; De Caro, R.; Stecco, C. Effects of Cesarean Section and Vaginal Delivery on Abdominal Muscles and Fasciae. Medicina 2020, 56, 260. [Google Scholar] [CrossRef] [PubMed]
- Michalska, A.; Rokita, W.; Wolder, D.; Pogorzelska, J.; Kaczmarczyk, K. Diastasis recti abdominis—A review of treatment methods. Ginekol. Polska 2018, 89, 97–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Factor | Inclusion | Exclusion |
|---|---|---|
| Research outcome |
|
|
| Study design and Methodology |
|
|
| S.No | Name of the Exercise | Description |
|---|---|---|
| 1. | Sit-Up | The exercise is performed by the subject lying with arms straight, knees bent and feet in a flat position. The abdominal muscles are then engaged, while a slight lift of the head, neck and shoulders is performed. The position is held for 10 s and then a return to the starting position. |
| 2. | Curl-up | The exercise is performed by the subject lying with arms straight, knees bent and feet in a flat position. The abdominal muscles are then engaged, while a major lift of the head, neck and shoulders is performed. The position is held for 10 s and then a return to the starting position. |
| 3. | TA Sit-up | The transverse abdominis muscle contraction is done along with sit-up. |
| 4. | TA Curl-up | Transverse abdominis muscle contraction is done along with curl-up. |
| 5. | TAPFM Curl-up | The transverse abdominis muscle and pelvic floor muscle contraction is done along with curl-up. |
| 6. | TASLR | The transverse abdominis muscle contraction is done along with straight leg raise. In the straight leg raise, the subject lies flat initially. One leg is raised above and the position held for 10 s and then relax back to the starting position. |
| 7. | Reverse Curl-up | In a reverse curl up, the subject initially lies flat. Then both legs are curled up together with knees towards chest. Hold the position for 10 s and then relax back to the starting position. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radhakrishnan, M.; Ramamurthy, K. Efficacy and Challenges in the Treatment of Diastasis Recti Abdominis—A Scoping Review on the Current Trends and Future Perspectives. Diagnostics 2022, 12, 2044. https://doi.org/10.3390/diagnostics12092044
Radhakrishnan M, Ramamurthy K. Efficacy and Challenges in the Treatment of Diastasis Recti Abdominis—A Scoping Review on the Current Trends and Future Perspectives. Diagnostics. 2022; 12(9):2044. https://doi.org/10.3390/diagnostics12092044
Chicago/Turabian StyleRadhakrishnan, Menaka, and Karthik Ramamurthy. 2022. "Efficacy and Challenges in the Treatment of Diastasis Recti Abdominis—A Scoping Review on the Current Trends and Future Perspectives" Diagnostics 12, no. 9: 2044. https://doi.org/10.3390/diagnostics12092044







