Cardiac Adaptation and Preferential Streaming in Fetuses with Multiple Nuchal Cords
Abstract
:1. Introduction
2. Materials and Methods
2.1. Exclusions and Final Sample Number
2.2. Statistical Analysis
3. Results
4. Discussion
- HA/CA (heart area/chest area ratio);
- GSI (global sphericity index);
- 4CV analysis;
- 3VV analysis.
- FHR;
- PI MCA, PS MCA;
- PI UMBA;
- Cerebroplacental ratio—CPR;
- PI DV, PS DV;
- PS UV;
- PS PA;
- PS Ao;
- PS AOI;
- PS DA, PI DA.
- SF LV, SF RV, IVS;
- RV myocardial width.
- assessment of the cardiac contractility and GLS—global longitudinal sphericity index.

5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bhalgat, P.; Kulkarni, D.; Lovhale, P. Tetralogy of Fallot and aortopulmonary window: Diagnosis and management. IHJ Cardiovasc. Case Rep. 2020, 4, 77–79. [Google Scholar] [CrossRef]
- Hammad, I.A.; Blue, N.R.; Allshouse, A.A.; Silver, R.M.; Gibbins, K.J.; Page, J.M.; Goldenberg, R.L.; Reddy, U.M.; Saade, G.R.; Dudley, D.J.; et al. Umbilical Cord Abnormalities and Stillbirth. Obstet. Gynecol. 2020, 135, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Vasa, R.; Dimitrov, R.; Patel, S. Nuchal cord at delivery and perinatal outcomes: Single-center retrospective study, with emphasis on fetal acid-base balance. Pediatr. Neonatol. 2018, 59, 439–447. [Google Scholar] [CrossRef] [PubMed]
- Hayes, D.J.L.; Warland, J.; Parast, M.M.; Bendon, R.W.; Hasegawa, J.; Banks, J.; Clapham, L.; Heazell, A.E.P. Umbilical cord characteristics and their association with adverse pregnancy outcomes: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0239630. [Google Scholar] [CrossRef] [PubMed]
- Młodawska, M.; Młodawski, J.; Świercz, G.; Zieliński, R. The Relationship between Nuchal Cord and Adverse Obstetric and Neonatal Outcomes: Retrospective Cohort Study. Pediatr. Rep. 2022, 14, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Yan, Y.; Yang, Z.; Li, Y.; Xue, X.; Zhang, X.; Pei, Q. Analysis of ultrasound clinical early warning system in hyper-coiling umbilical cord. Chin. Med. J. 2023, 136, 2516–2517. [Google Scholar] [CrossRef] [PubMed]
- Crispi, F.; Sepúlveda-Martínez, Á.; Crovetto, F.; Gómez, O.; Bijnens, B.; Gratacós, E. Main Patterns of Fetal Cardiac Remodeling. Fetal. Diagn Ther. 2020, 47, 337–344. [Google Scholar] [CrossRef]
- Więckowska, K.; Zych-Krekora, K.; Słodki, M.; Respondek-Liberska, M. Do umbilical cord wrapped around the fetal body can mimic signs of aortal coarctation? Prenat Cardio 2016, 6, 82–86. [Google Scholar] [CrossRef]
- Leo, I.; Sabatino, J.; Avesani, M.; Moscatelli, S.; Bianco, F.; Borrelli, N.; De Sarro, R.; Leonardi, B.; Calcaterra, G.; Surkova, E.; et al. Non-Invasive Imaging Assessment in Patients with Aortic Coarctation: A Contemporary Review. J. Clin. Med. 2024, 13, 28. [Google Scholar] [CrossRef]
- Raza, S.; Aggarwal, S.; Jenkins, P.; Kharabish, A.; Anwer, S.; Cullington, D.; Jones, J.; Dua, J.; Papaioannou, V.; Ashrafi, R.; et al. Coarctation of the Aorta: Diagnosis and Management. Diagnostics 2023, 13, 2189. [Google Scholar] [CrossRef]
- Idilman, I.S.; Ipek, A.; Balaban, M.; Keskin, H.L.; Aypar, E.; Ozkutlu, S. Fetal aorta larger than the main pulmonary artery on the three-vessel view: Correlation with postnatal echocardiographic findings. J. Clin. Ultrasound 2016, 44, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Respondek-Liberska, M. WS06-05 Disproportion of the four chamber view of the fetal heart: What does it mean? Ultrasound Obstet. Gynecol. 2000, 16, 14. [Google Scholar] [CrossRef]
- Sherer, D.M.; Roach, C.; Soyemi, S.; Dalloul, M. Current Perspectives of Prenatal Sonographic Diagnosis and Clinical Management Challenges of Complex Umbilical Cord Entanglement. Int. J. Womens Health 2021, 13, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Battarbee, A.N.; Palatnik, A.; Ernst, L.M.; Grobman, W.A. Association of Isolated Single Umbilical Artery with Small for Gestational Age and Preterm Birth. Obstet. Gynecol. 2015, 126, 760–764. [Google Scholar] [CrossRef]
- Ebbing, C.; Kessler, J.; Moster, D.; Rasmussen, S. Single umbilical artery and risk of congenital malformation: Population-based study in Norway. Ultrasound Obstet. Gynecol. 2020, 55, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, R.; Miao, J.H.; Rehman, A. Physiology, Cardiovascular; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Skrobich, P.; Tchorzewska-Skrobich, M. Dlaczego krew nie płynie przez by-pass? Prawa fizyczne warunkujące przepływ w by-passach. Kardiol. W Prakt. 2017, 10, 21–26. [Google Scholar]
- Tchirikov, M.; Eisermann, K.; Rybakowski, C.; Schröder, H.J. Doppler ultrasound evaluation of ductus venosus blood flow during acute hypoxemia in fetal lambs. Ultrasound Obstet Gynecol. 1998, 11, 426–431. [Google Scholar] [CrossRef]
- Murlewska, J.; Sylwestrzak, O.; Poszwa, P.; Respondek-Liberska, M. The effect of nuchal umbilical cord on fetal cardiac and cerebral circulation-cross-sectional study. J. Perinat. Med. 2021, 49, 590–595. [Google Scholar] [CrossRef]
- Shin, J.A.; Lee, J.Y.; Yum, S.K. Echocardiographic assessment of brain sparing in small-for-gestational age infants and association with neonatal outcomes. Sci. Rep. 2023, 13, 10248. [Google Scholar] [CrossRef]
- Giussani, D.A. The fetal brain sparing response to hypoxia: Physiological mechanisms. J. Physiol. 2016, 594, 1215–1230. [Google Scholar] [CrossRef]
- Quaresima, P.; Fesslova, V.; Farina, A.; Kagan, K.O.; Candiani, M.; Morelli, M.; Crispi, F.; Cavoretto, P.I. How to do a fetal cardiac scan. Arch. Gynecol. Obstet. 2023, 307, 1269–1276. [Google Scholar] [CrossRef] [PubMed]
- Braga, M.; Moleiro, M.L.; Guedes-Martins, L. Clinical Significance of Ductus Venosus Waveform as Generated by Pressure- volume Changes in the Fetal Heart. Curr. Cardiol. Rev. 2019, 15, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Luzi, G.; Bori, S.; Iammarino, G.; Taddei, F.; Martines, G.; Piatti, P.; Di Renzo, G.C. Aspetti funzionali dell’apparato urinario fetale in rapporto all’ accrescimento [Functional aspects of the fetal urinary apparatus in relation to growth]. Arch. Ital. Urol. Androl. 1996, 68 (Suppl. S5), 9–12. (In Italian) [Google Scholar]
- van Asselt, K.; Gudmundsson, S.; Lindqvist, P.; Marsal, K. Uterine and umbilical artery velocimetry in pre-eclampsia. Acta Obstet. Gynecol. Scand. 1998, 77, 614–619. [Google Scholar] [CrossRef] [PubMed]











| Parameter | Group A | Group B | Group C |
|---|---|---|---|
| GA (biometry) | 32.54 ± 3.1 | 33.14 ± 2.9 | 33.45 ± 2.9 |
| UmbA PI | 0.974 ± 0.2 | 1.101 ± 0.2 | 0.889 ± 0.3 |
| MCA PI | 1.825 ± 0.5 | 1.862 ± 0.5 | 1.788 ± 0.5 |
| AFI | 14.18 ± 3.7 | 15.57 ± 4.3 | 15.64 ± 3.6 |
| CTAR | 0.31 ± 0.03 | 0.31 ± 0.04 | 0.33 ± 0.04 |
| EFW | 2071.75 ± 653 | 2179.54 ± 647 | 2240.22 ± 677 |
| Parameter | Group A (n = 716) vs. Group B (n = 102) | Group A (n = 716) vs. Group C (n = 32) |
|---|---|---|
| UmbA PI | p > 0.05 | p = 0.04 * |
| MCA PI | p > 0.05 | p > 0.05 |
| AFI | p < 0.05 (p = 0.0004) | p < 0.05 (p = 0.009) |
| CTAR | p > 0.05 | p < 0.05 (p = 0.006) |
| EFW | p > 0.05 | p > 0.05 |
| Parameter | PA [mm] | AO [mm] | PA/AO Ratio |
|---|---|---|---|
| 0 nuchal cords, n = 716 (group A), vs. 1 nuchal cord, n = 102 (group B) | 7.4 ± 1.4 vs. 7.8 ± 1.5 (p = 0.009) | 6.1 ± 1.1 vs. 6.2 ± 1.1 (p = 0.35) | 1.2 ± 0.2 vs. 1.3 ± 0.2 (p = 0.01) |
| 0 nuchal cords, n = 716 (group A), vs. 2 nuchal cords, n = 32 (group C) | 7.4 ± 1.4 vs. 8.3 ± 1.7 (p = 0.002) | 6.1 ± 1.1 vs. 6.4 ± 1.0 (p = 0.07) | 1.2 ± 0.2 vs. 1.3 ± 0.2 (p = 0.01) |
| 1 nuchal cord, n = 102 (group B), vs. 2 nuchal cords, n = 32 (group C) | 7.8 ± 1.5 vs. 8.3 ± 1.7 (p = 0.1) | 6.2 ± 1.1 vs. 6.3 ± 1.0 (p = 0.3) | 1.3 ± 0.2 vs. 1.3 ± 0.2 (p = 0.2) |
| 2D |
|
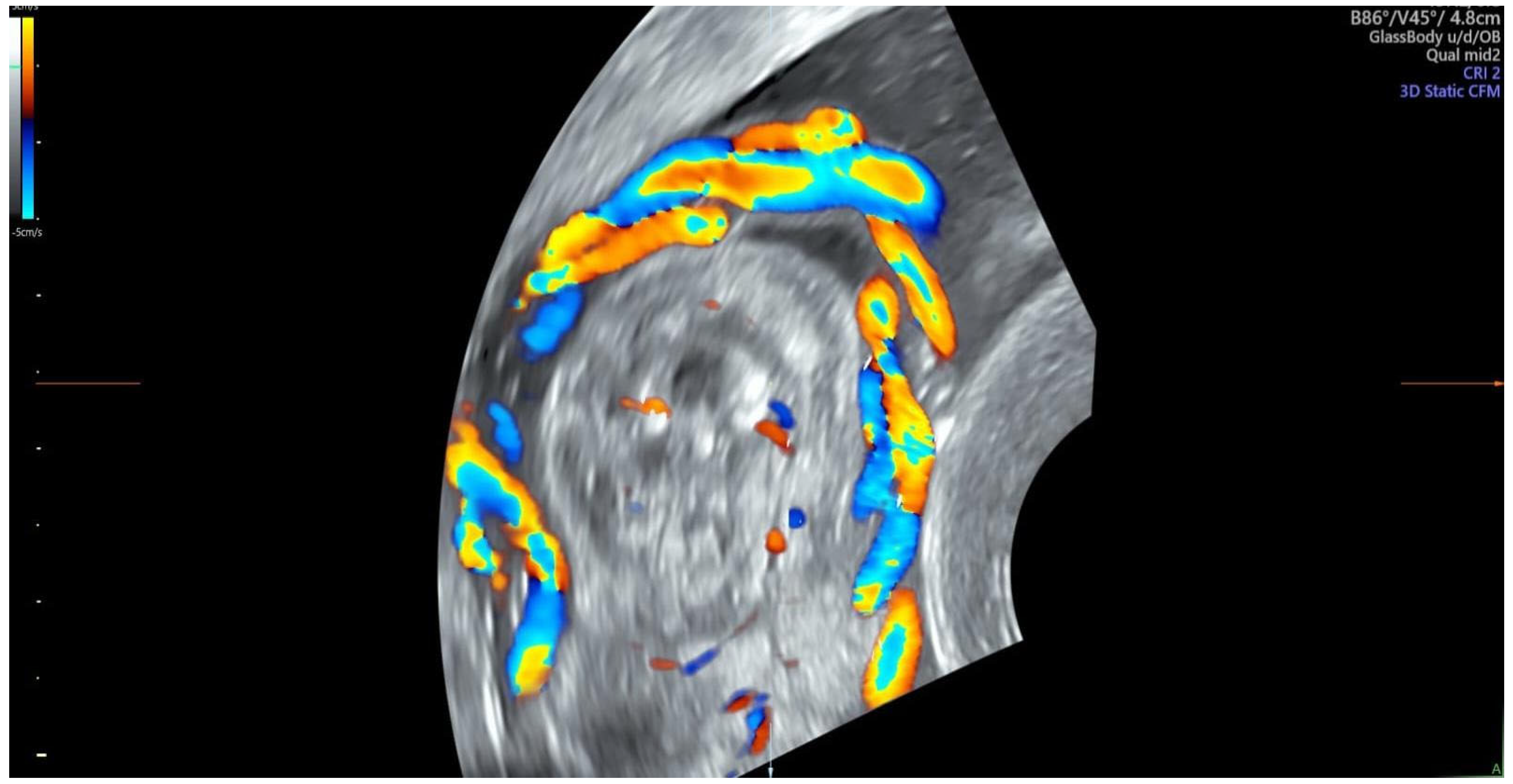
| Color Doppler |
|
| M-Mode |
|
| Speckle tracking |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murlewska, J.; Witkowski, S.; Biały, Ł.; Respondek-Liberska, M.; Słodki, M.; Strzelecka, I. Cardiac Adaptation and Preferential Streaming in Fetuses with Multiple Nuchal Cords. Diagnostics 2024, 14, 77. https://doi.org/10.3390/diagnostics14010077
Murlewska J, Witkowski S, Biały Ł, Respondek-Liberska M, Słodki M, Strzelecka I. Cardiac Adaptation and Preferential Streaming in Fetuses with Multiple Nuchal Cords. Diagnostics. 2024; 14(1):77. https://doi.org/10.3390/diagnostics14010077
Chicago/Turabian StyleMurlewska, Julia, Sławomir Witkowski, Łucja Biały, Maria Respondek-Liberska, Maciej Słodki, and Iwona Strzelecka. 2024. "Cardiac Adaptation and Preferential Streaming in Fetuses with Multiple Nuchal Cords" Diagnostics 14, no. 1: 77. https://doi.org/10.3390/diagnostics14010077






