Dopamine, Serotonin, and Structure/Function Brain Defects as Biological Bases for Treatment Response in Delusional Disorder: A Systematic Review of Cases and Cohort Studies
Abstract
:1. Introduction
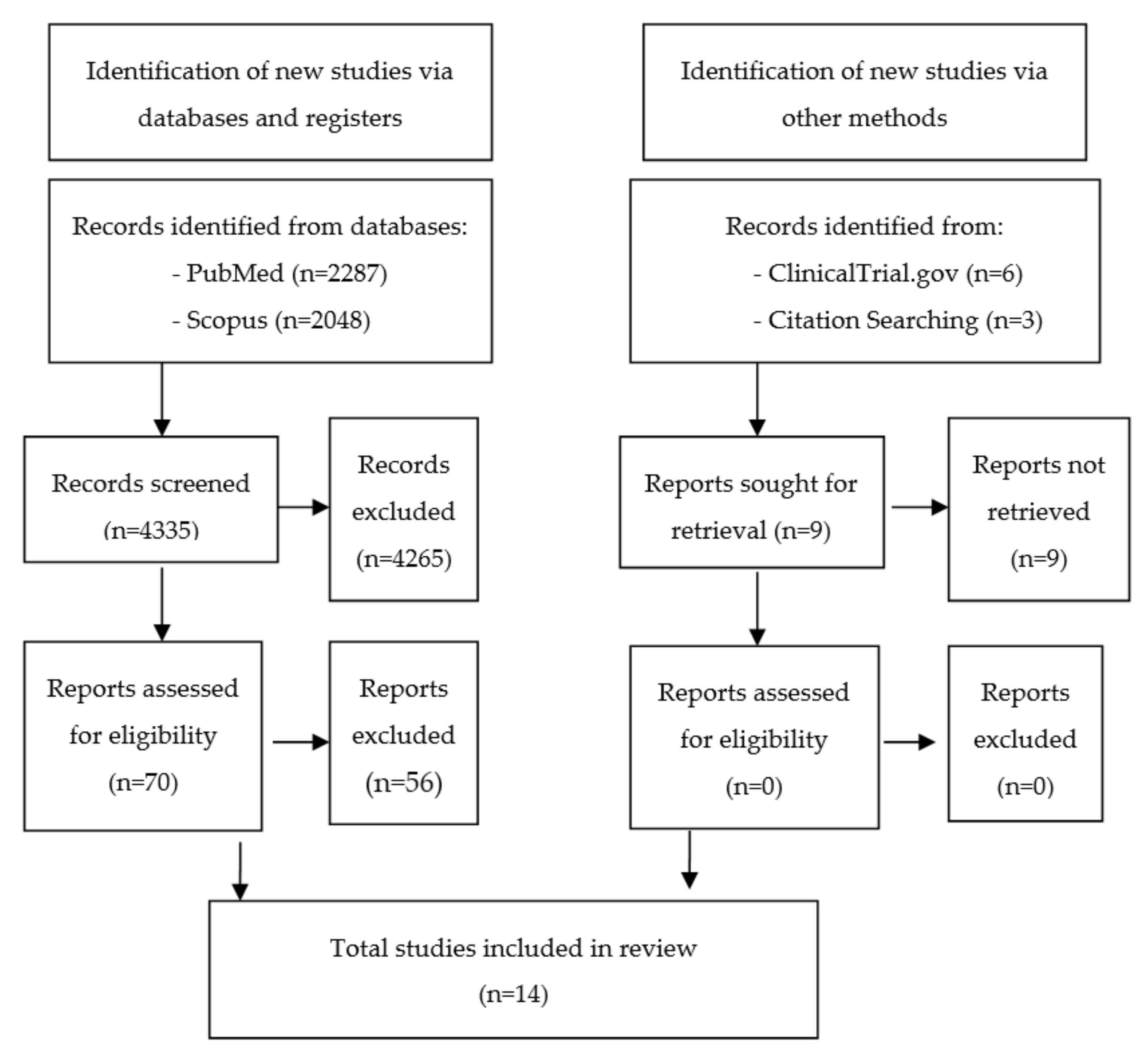
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Data Collection and Extraction
2.4. Assessment of Risk of Bias in Included Reports and Quality of Body of Evidence
2.5. Data Synthesis
3. Results
3.1. Reports
3.1.1. Case Reports
| (1) Dopaminergic dysfunction (‘dopamine psychosis’) (n = 5) | |
|---|---|
| 1- Ziprasidone induced-supersensitivity psychosis by chronic blockade of DRD2 in mesolimbic brain [49]. | |
| 2- Pretreatment levels of pHVA and implication of DRD2 Ser311Cys, DRD3 Ser9Gly and TH VNTR in DD [52] | |
| 3- DAT dysfunction in DDST [45] | |
| 4- Effectiveness of DRD2 partial agonists (aripiprazole) [48,51]. | |
| (2) Serotonergic dysfunction (n = 11) | |
| 1- Efficacy of partial agonism 5-HT1A and antagonism 5-HT2A in DDST [43,48,50,51]. | |
| 2- Efficacy of 5-HT2 antagonists in DDST [39,40,42,43,44] and DD [49]. | |
| 3- Efficacy of partial agonist at 5-HT1A and 5-HT7 antagonists in DD [50]. | |
| (3) Brain dysfunction (n = 8) | |
| 1- Serotonergic and dopaminergic reversal of reduced rCBF in left temporal and parietal lobes in DD [40,41,42,46,47]. | |
| 2- Serotoninergic and DRD2 partial agonistic reversal of reduced rCBF in right temporal and parietal lobes in DD [51]. | |
| 3- DRD2 partial antagonistic reversal of dysfunctional fronto-striato-thalamo-parietal network [41]. | |
| 4- Correction of basal ganglia and subcortical grey matter lesions correlates with good response in DD [48]. | |
| Authors and Year of Publication | Study Design | Method | Checklist CARE Guidelines | |
|---|---|---|---|---|
| Completed Items | Missing Subitems *,# | |||
| Umezaki et al., 2017 [51] | Case reports | Neuroimaging: 99m Tc ECD SPECT | 7/13 | 2, 5c, 8a, 8d, 10c, 10d, 12, 13 |
| Davis and Agarwal 2015 [50] | Case report | Clinical observation | 6/13 | 2, 3b, 3c, 6, 8a, 8b, 8d, 10a, 10b, 10d, 12, 13 |
| Rajkumar et al., 2014 [49] | Case report | Clinical observation | 6/13 | 2, 3d, 6, 8a, 8b, 8d, 10a, 10c, 12, 13 |
| Freudenmann et al., 2010 [48] | Case report | Neuroimaging: (a) Untreated state: FDOPA-PET, 123I-FP-CIT-SPECT, IBZM-SPECT and FDG-PET (b) After AP antipsychotic treatment: IBZM-SPECT, FDG-PET | 6/13 | 1, 2, 5a, 5c, 8b, 8d, 10a, 10c, 10d, 12, 13 |
| Hayashi et al., 2010 [47] | Case report | Neuroimaging: 99m- Tc ECD SPECT | 5/13 | 1, 2, 5a, 5c, 8b, 8d, 9b, 9c, 10a, 10c, 10d, 12, 13 |
| Akahane et al., 2009 [46] | Case report | Neuroimaging: SPECT-Xe-133 | 5/13 | 2, 5a, 5c, 6, 8b, 8d, 9c, 10a, 12, 13 |
| Bosmans and Verbanck, 2008 [44] | Case report | Clinical observation | 4/13 | 1, 2, 3a, 3b, 3c, 3d, 5a, 5c, 8b, 8d, 9b, 9c, 10a, 10c, 12, 13 |
| Huber et al., 2008 [45] | Case series (consecutive sampling) | Neuroimaging: MRI (T1, T2, FLAIR) | 6/13 | 1, 2, 5c, 8b, 10a, 12, 13 |
| Dimopoulos et al., 2008 [43] | Case report | Clinical observation | 4/13 | 1, 2, 3b, 5c, 6, 8b, 10a, 10c, 10d, 12, 13 |
| Hayashi et al., 2004 [42] | Case report | Neuroimaging: MRI; Xe-133 SPECT | 5/13 | 1, 2, 5a, 5c, 8b, 8d, 9c, 10a, 10c, 10d, 12, 13 |
| Ota et al., 2003 [41] | Case report | Neuroimaging: MRI, MRA, 99m- Tc ECD SPECT | 6/13 | 2, 5c, 5d, 8b, 8d, 9b, 9d, 10a, 10c, 10d, 12, 13 |
| Morimoto et al., 2002 [52] | Prospective observational cohort study | (a) Biochemistry: p HVA (HPLC) (b) Genetics: polymorphisms of DRD2 Ser311Cys, DRD3 Ser9Gly, TH VNTR (c) Clinical: AP response | - | - |
| Wada et al., 1999 (b) [40] | Case report | Neuroimaging: 133-Xe SPECT + MRI | 4/13 | 1, 2, 5a, 5c, 6, 8b, 8d, 9c, 10a, 10c, 10d, 12, 13 |
| Wada et al., 1999 (a) [39] | Case report | Clinical observation | 0/13 | 1, 2, 3a, 3b, 3c, 3d, 4, 5a, 5c, 5d, 6, 7, 8a, 8b, 8d, 9b, 9c, 9d, 10a, 10b, 10c, 10d, 11a, 11b, 11d, 12, 13 |
| Tools for Evaluating Methodological Quality of Case Reports | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Domains | Leading explanatory questions | [39] | [40] | [41] | [42] | [43] | [44] | [45] | [46] | [47] | [48] | [49] | [50] | [51] |
| Selection | 1. Do the patient(s) represent the whole experience of the investigator or is the selection method unclear to the extent that other patients (…)? | No | No | Yes | Yes | Yes | No | Yes | No | Yes | Yes | No | Yes | Yes |
| Ascertain-ment | 2. Was the exposure adequately ascertained? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 3. Was the outcome adequately ascertained? | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Causality | 4 *. Were other alternative causes that may explain the observation ruled out? | No | No | No | No | No | No | No | No | No | No | Yes | No | No |
| 5 *. Was there a challenge/rechallenge phenomenon | No | No | No | No | Yes | No | No | No | Yes | No | Yes | No | Yes | |
| 6 *. Was there a dose-response effect? | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | |
| 7. Was follow-up long enough for outcomes to occur? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Reporting | 8. Is the case(s) described with sufficient details to allow other investigators to replicate the research or to allow practitioners make inferences related to their own practice? | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| Total scores | Max. 8 | 5 | 6 | 6 | 7 | 7 | 6 | 7 | 6 | 7 | 7 | 6 | 7 | 7 |
3.1.2. Trial Addressing the Dopamine Hypothesis of Drug Response in DD
4. Discussion
Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Cys | Cysteine |
| DAT | Dopamine Transporter |
| DD | Delusional Disorder |
| DDST | Delusional Disorder Somatic Type |
| DRD2 | Dopamine Receptor D2 |
| DRD3 | Dopamine Receptor D3 |
| Gly | Glycine |
| pHVA | plasma homovallinic acid |
| rCBF | regional Cerebral Blood Flow |
| Ser | Serine |
| TH | Tyrosine Hydroxylase |
| VNTR | Variable Number of Tandem Repeat |
| 5-HT | 5-hydroxytryptamine |
Appendix A
| Patient, Population or Problem | Intervention or Exposure | Comparison | Outcome |
|---|---|---|---|
| What are the characteristics of the patients or population? What is the problem, condition or disease you are interested in? | What interventions are we considering? | What is the comparison or alternative to the intervention? | What are the possible or relevant outcomes? |
| Patients with delusional disorder (DD). Review studies reporting an hypothesis for the explanation of the biological underpinnings of treatment response in DD or reporting structural or functional neuroimaging findings. | Pharmacological treatment for DD. | Any comparator (placebo, different drugs, any other therapy) | Complete remission or marked improvement of psychotic symptoms in DD. New knowledge about the biology of treatment response in DD. |
| Tools for Evaluating Methodological Quality of Case Controls | |
|---|---|
| Leading Explanatory Questions | Morimoto et al., 2002 [52] |
| 1. Can we be confident in the assessment of exposure? | Definitely yes |
| 2. Can we be confident that cases had developed the outcome of interest and controls had not? | Probably yes |
| 3. Were the cases (those who were exposed and developed the outcome of interest) properly selected? | Probably yes |
| 4. Were the controls (those who were exposed and did not develop the outcome of interest) properly selected? | Probably yes |
| 5. Were cases and controls matched according to important prognostic variables or was statistical adjustment carried out for those variables? | Probably yes |
References
- Mews, M.R.; Quante, A. Comparative efficacy and acceptability of existing pharmacotherapies for delusional disorder: A retrospective case series and review of the literature. J. Clin. Psychopharmacol. 2013, 33, 512–519. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5™, 5th ed.; American Psychiatric Association: Arlington, TA, USA, 2013. [Google Scholar]
- Kendler, K.S. Demography of paranoid psychosis (delusional disorder): A review and comparison with schizophrenia and affective illness. Arch. Gen. Psychiatry 1982, 39, 890–902. [Google Scholar] [CrossRef]
- Manschreck, T.C.; Khan, N.L. Recent advances in the treatment of delusional disorder. Can. J. Psychiatry 2006, 51, 114–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roman-Avezuela, N.; Esteve-Díaz, N.; Domarco Manrique, L.; Domíngyez Longás, A.; Miguélez Fernández, C.; de Portugal, E. Gender differences in delusional disorder. Rev. Asoc. Esp. Neuropsiq. 2015, 35, 37–51. [Google Scholar]
- Kulkarni, K.R.; Arasappa, R.; Prasad, M.K.; Zutshi, A.; Chand, P.K.; Murthy, P.; Muralidharan, K. Gender Differences in Persistent Delusional Disorder. Indian J. Psychol. Med. 2017, 39, 216–217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wustmann, T.; Pillmann, F.; Marneros, A. Gender-related features of persistent delusional disorders. Eur. Arch. Psychiatry Clin. Neurosci. 2011, 261, 29–36. [Google Scholar] [CrossRef] [PubMed]
- De Portugal, E.; Martínez, C.; González, N.; del Amo, V.; Haro, J.M.; Cervilla, J.A. Clinical and cognitive correlates of psychiatric comorbidity in delusional disorder outpatients. Aust. N. Z. J. Psychiatry 2011, 45, 416–425. [Google Scholar] [CrossRef]
- González-Rodríguez, A.; Molina-Andreu, O.; Navarro Odriozola, V.; Gastó Ferrer, C.; Penadés, R.; Catalán, R. Delusional disorder: An overview of depressive symptoms and antidepressant use. Eur. J. Psychiatry 2013, 27, 265–276. [Google Scholar] [CrossRef] [Green Version]
- De Portugal, E.; González, N.; Miriam, V.; Haro, J.M.; Usall, J.; Cervilla, J.A. Gender differences in delusional disorder: Evidence from an outpatient sample. Psychiatry Res. 2010, 177, 235–239. [Google Scholar] [CrossRef]
- González-Rodríguez, A.; Seeman, M.V. Addressing Delusions in Women and men with delusional disorder: Key Points for Clinical Management. Int. J. Environ. Res. Public Health 2020, 17, 4583. [Google Scholar] [CrossRef]
- Stone, J.M.; Raffin, M.; Morrison, P.; McGuire, P.K. The biological basis of antipsychotic response in schizophrenia. J. Psychopharmacol. 2010, 24, 953–964. [Google Scholar] [CrossRef]
- Yang, A.C.; Tsai, S.J. New targets for schizophrenia treatment beyond the dopamine hypothesis. Int. J. Mol. Sci. 2017, 18, 1689. [Google Scholar] [CrossRef]
- Kane, J.; Honigfeld, G.; Singer, J.; Meltzer, H. Clozapine for the treatment-resistant schizophrenic: A double-blind comparison with chlorpromazine. Arch. Gen. Psychiatry 1988, 45, 789–796. [Google Scholar] [CrossRef]
- Siskind, D.; McCartney, L.; Goldschlager, R.; Kisely, S. Clozapine v. First-and second-generation antipsychotics in treatment-refractory schizophrenia: Systematic review and meta-analysis. Br. J. Psychiatry 2016, 209, 385–392. [Google Scholar] [CrossRef] [Green Version]
- Samara, M.T.; Dold, M.; Gianatsi, M.; Nikolakopoulou, A.; Helfer, B.; Salanti, G.; Leucht, S. Efficacy, acceptability, and tolerability of antipsychotics in treatment-resistant schizophrenia: A network meta-analysis. JAMA Psychiatry 2016, 73, 199–210. [Google Scholar] [CrossRef] [Green Version]
- Matthysse, S. Dopamine and the pharmacology of schizophrenia: The state of the evidence. J. Psychiat. Res. 1974, 11, 107–113. [Google Scholar] [CrossRef]
- Van Rossum, J.M. The significance of dopamine receptor blockade for the action of neuroleptic drugs. Arch. Int. Pharm. Ther. 1966, 160, 492–494. [Google Scholar]
- Carlsson, A.; Lindqvist, M. Effect of chlorpromazine or haloperidol on formation of 3-methoxytyramine and normetanephrine in mouse brain. Acta Pharm. Toxicol. 1963, 20, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Madras, B.K. History of the discovery of the antipsychotic dopamine D2 receptor: A basis for the dopamine hypothesis of schizophrenia. J. Hist. Neurosci. 2013, 22, 62–78. [Google Scholar] [CrossRef]
- Seeman, P.; Chau-Wong, M.; Tedesco, J.; Wong, K. Brain receptors for antipsychotic drugs and dopamine: Direct binding assays. Proc. Natl. Acad. Sci. USA 1975, 72, 4376–4380. [Google Scholar] [CrossRef] [Green Version]
- Creese, I.; Burt, D.R.; Snyder, S.H. Dopamine receptor binding predicts clinical and pharmacological potencies of antischizophrenic drugs. Science 1976, 192, 481–483. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.C.; Diaz, J.; Pilon, C.; Sokoloff, P. Possible implications of the dopamine D(3) receptor in schizophrenia and in antipsychotic drug actions. Brain Res. Rev. 2000, 31, 277–287. [Google Scholar] [CrossRef]
- Howes, O.D.; Kambeitz, J.; Kim, E.; Stahl, D.; Slifstein, M.; Abi-Dargham, A.; Kapur, S. The nature of dopamine dysfunction in schizophrenia and what this means for treatment. Arch. Gen. Psychiatry 2012, 69, 776–786. [Google Scholar] [CrossRef] [Green Version]
- Stahl, S.M. Beyond the dopamine hypothesis of schizophrenia to three neural networks of psychosis: Dopamine, serotonin, and glutamate. CNS Spectr. 2018, 23, 187–191. [Google Scholar] [CrossRef]
- Risbood, V.; Lee, J.R.; Roche-Desilets, J.; Fuller, M.A. Lurasidone: An atypical antipsychotic for schizophrenia. Ann. Pharmacother. 2012, 46, 1033–1046. [Google Scholar] [CrossRef]
- Smith, D.A.; Buckley, P.F. Pharmacotherapy of delusional disorders in the context of offending and the potential for compulsory treatment. Behav. Sci. Law 2006, 24, 351–367. [Google Scholar] [CrossRef]
- Volkow, N.D.; Ding, Y.; Fowler, J.S.; Wang, G.J.; Logan, J.; Gatley, J.S. Is methylphenidate like cocaine? Studies on their pharmacokinetics and distribution in human brain. Arch. Gen. Psychiatry 1995, 52, 456–463. [Google Scholar] [CrossRef]
- Learned-Coughlin, S.M.; Bergström, M.; Savitcheva, I.; Ascher, J.; Schmith, V.D.; Langstrom, B. In vivo activity of bupropion at the human dopamine transporter as measured by positron emission tomography. Biol. Psychiatry 2003, 54, 800–805. [Google Scholar] [CrossRef]
- King, B.H. Hypothesis: Involvement of the serotonergic system in the clinical expression of monosymptomatic hypochondriasis. Pharmacopsychiatry 1990, 23, 85–89. [Google Scholar] [CrossRef]
- Munro, A. Monosymptomatic hypochondriacal psychosis. Br. J. Psychiatry 1988, 153, 37–40. [Google Scholar] [CrossRef]
- Sondheimer, A. Case Study; clomipramine treatment of delusional disorder-somatic type. J. Am. Acad. Child Adolesc. Psychiatry 1988, 27, 188–192. [Google Scholar] [CrossRef]
- Munro, A. Monosymptomatic hypochondriacal psychosis manifesting as delusions of parasitosis. A description of four cases successfully treated with pimozide. Arch. Dermatol. 1978, 114, 940–943. [Google Scholar] [CrossRef]
- Emsley, R.; Asmal, L.; Du Plessis, S.; Chiliza, B.; Phahladira, L.; Kilian, S. Brain volume changes over the first year of treatment in schizophrenia: Relationships to antipsychotic treatment. Psychol. Med. 2017, 47, 2187. [Google Scholar] [CrossRef]
- Penadés, R.; González-Rodríguez, A.; Catalán, R.; Segura, B.; Bernardo, M.; Junqué, C. Neuroimaging studies of cognitive remediation in schizophrenia: A systematic and critical review. World J. Psychiatry 2017, 7, 34. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Moher, D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Riley, D.S.; Barber, M.S.; Kienle, G.S.; Aronson, J.K.; von Schoen-Angerer, T.; Tugwell, P.; Werthmann, P.G. CARE guidelines for case reports: Explanation and elaboration document. J. Clin. Epidemiol. 2017, 89, 218–235. [Google Scholar] [CrossRef]
- CLARITY Group at McMaster University. Tools to Assess Risk of Bias in Cohort Studies, Case Control Studies, Randomized Controlled Trials, and Longitudinal Symptom Research Studies Aimed at the General Population. 2013. Available online: https://www.evidencepartners.com/resources/methodological-resources (accessed on 10 August 2021).
- Wada, T.; Kawakatsu, S.; Nadaoka, T.; Okuyama, N.; Otani, K. Clomipramine treatment of delusional disorder, somatic type. Int. Clin. Psychopharmacol. 1999, 14, 181–183. [Google Scholar] [CrossRef]
- Wada, T.; Kawakatsu, S.; Komatani, A.; Okuyama, N.; Otani, K. Possible association between delusional disorder, somatic type and reduced regional cerebral blood flow. Prog. Neuropsychopharmacol. Biol. Psychiatry 1999, 23, 353–357. [Google Scholar] [CrossRef]
- Ota, M.; Mizukami, K.; Katano, T.; Sato, S.; Takeda, T.; Asada, T. A case of delusional disorder, somatic type with remarkable improvement of clinical symptoms and single photon emission computed tomograpy findings following modified electroconvulsive therapy. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2003, 27, 881–884. [Google Scholar] [CrossRef]
- Hayashi, H.; Oshino, S.; Ishikawa, J.; Kawakatsu, S.; Otani, K. Paroxetine treatment of delusional disorder, somatic type. Hum. Psychopharmacol. 2004, 19, 351–352. [Google Scholar] [CrossRef] [PubMed]
- Dimopoulos, N.P.; Mitsonis, C.I.; Psarra, V.V. Delusional disorder, somatic type treated with aripiprazole-mirtazapine combination. J. Psychopharmacol. 2008, 22, 812–814. [Google Scholar] [CrossRef] [PubMed]
- Bosmans, A.; Verbanck, P. Successful treatment of delusional disorder of the somatic type or “delusional parasitosis” with olanzapine. Pharmacopsychiatry 2008, 41, 121–122. [Google Scholar] [CrossRef] [PubMed]
- Huber, M.; Karner, M.; Kirchler, E.; Lepping, P.; Freudenmann, R.W. Striatal lesions in delusional parasitosis revealed by magnetic resonance imaging. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2008, 32, 1967–1971. [Google Scholar] [CrossRef]
- Akahane, T.; Hayashi, H.; Suzuki, H.; Kawakatsu, S.; Otani, K. Extremely grotesque somatic delusions in a patient of delusional disorder and its response to risperidone treatment. Gen. Hosp. Psychiatry 2009, 31, 185–186. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, H.; Akahane, T.; Suzuki, H.; Sasaki, T.; Kawakatsu, S.; Otani, K. Successful treatment by paroxetine of delusional disorder, somatic type, accompanied by severe secondary depression. Clin. Neuropharmacol. 2010, 33, 48–49. [Google Scholar] [CrossRef]
- Freudenmann, R.W.; Kölle, M.; Huwe, A.; Luster, M.; Reske, S.N.; Huber, M.; Schönfeldt-Lecuona, C. Delusional infestation: Neural correlates and antipsychotic therapy investigated by multimodal neuroimaging. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2010, 34, 1215–1222. [Google Scholar] [CrossRef]
- Rajkumar, R.P. Supersensitivity psychosis and its response to asenapine in a patient with delusional disorder. Case Rep. Psychiatry 2014, 2014, 215732. [Google Scholar] [CrossRef]
- Davis, L.; Agarwal, G. Successful Treatment of Delusional Disorder, Persecutory Type with Lurasidone: A Case Report. J. Schizophr. Res. 2015, 2, 1014. [Google Scholar]
- Umezaki, Y.; Uezato, A.; Toriihara, A.; Nishikawa, T.; Toyofuku, A. Two cases of oral somatic delusions ameliorated with brain perfusion asymmetry: A case report. Clin. Neuropsychopharmacol. 2017, 40, 97. [Google Scholar] [CrossRef] [Green Version]
- Morimoto, K.; Miyatake, R.; Nakamura, M.; Watanabe, T.; Hirao, T.; Suwaki, H. Delusional disorder: Molecular genetic evidence for dopamine psychosis. Neuropsychopharmacology 2002, 26, 794–801. [Google Scholar] [CrossRef]
- Huber, M.; Kirchler, E.; Karner, M.; Pycha, R. Delusional parasitosis and the dopamine transporter. A new insight of etiology? Med. Hypotheses 2007, 68, 1351–1358. [Google Scholar] [CrossRef]
- Abi-Dargham, A. Do we still believe in the dopamine hypothesis? New data bring new evidence. Int. J. Neuropsychopharmacol. 2004, 7 (Suppl. S1), S1–S5. [Google Scholar] [CrossRef]
- Kapur, S.; Agid, O.; Mizrahi, R.; Li, M. How antipsychotics work—From receptors to reality. NeuroRx 2006, 3, 10–21. [Google Scholar] [CrossRef]
- Howes, O.D.; Egerton, A.; Allan, V.; McGuire, P.; Stokes, P.; Kapur, S. Mechanisms underlying psychosis and antipsychotic treatment response in schizophrenia: Insights from PET and SPECT imaging. Curr. Pharm. Des. 2009, 15, 2550–2559. [Google Scholar] [CrossRef] [Green Version]
- Muñoz-Negro, J.E.; Gómez-Sierra, F.J.; Peralta, V.; González-Rodríguez, A.; Cervilla, J.A. A systematic review of studies with clinician-rated scales on the pharmacological treatment of delusional disorder. Int. Clin. Psychopharmacol. 2020, 35, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Vollenweider, F.X.; Vontobel, P.; Hell, D.; Leenders, K.L. 5-HT modulation of dopamine release in basal ganglia in psilocybin-induced psychosis in man—A PET study with [11 C] raclopride. Neuropsychopharmacology 1999, 20, 424–433. [Google Scholar] [CrossRef] [Green Version]
- Freeman, D.; Dunn, G.; Fowler, D.; Bebbington, P.; Kuipers, E.; Emsley, R.; Garety, P. Current paranoid thinking in patients with delusions: The presence of cognitive-affective biases. Schizophr. Bull. 2013, 39, 1281–1287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serretti, A.; Lattuada, E.; Cusin, C.; Smeraldi, E. Factor analysis of delusional disorder symptomatology. Compr. Psychiatry 1999, 40, 143–147. [Google Scholar] [CrossRef]
- De Portugal, E.; González, N.; del Amo, V.; Haro, J.M.; Díaz-Caneja, C.M.; Luna del Castillo, J.d.D.; Cervilla, J.A. Empirical redefinition of delusional disorder and its phenomenology: The DELIREMP study. Compr. Psychiatry 2013, 54, 243–255. [Google Scholar] [CrossRef] [PubMed]
- González-Rodríguez, A.; Molina-Andreu, O.; Penadés, R.; Catalan, R.; Bernardo, M. Structural and Functional Neuroimaging findings in Delusional Disorder and Therapeutic Implications. Open Psychiatry J. 2015, 9, 17–25. [Google Scholar] [CrossRef]
- Muñoz-Negro, J.E.; Ibáñez-Casas, I.; de Portugal, E.; Lozano-Gutiérrez, V.; Martínez-Leal, R.; Cervilla, J.A. A Psychopathological Comparison between Delusional Disorder and Schizophrenia. Can. J. Psychiatry 2017, 63, 12–19. [Google Scholar] [CrossRef]
- Peralta, V.; Cuesta, M.J. Delusional disorder and schizophrenia: A comparative study across multiple domains. Psychol. Med. 2016, 46, 2829–2839. [Google Scholar] [CrossRef]
- Opjordsmoen, S. Delusional Disorder as a Partial Psychosis. Schizophr. Bull. 2014, 40, 244–247. [Google Scholar] [CrossRef] [Green Version]
- González-Castro, N. Trastorno Delirante: ¿Es Realmente Diferente de la Esquizofrenia? Ph.D. Thesis, Universitat Autònoma de Barcelona, BCN, Cerdanyola del Vallès, Spain, 2014. [Google Scholar]
- Lo, Y.; Tsai, S.J.; Chang, C.H.; Hwang, J.P.; Sim, C.B. Organic delusional disorder in psychiatric in-patients: Comparison with delusional disorder. Acta Psychiatr. Scand. 1997, 95, 161–163. [Google Scholar] [CrossRef] [PubMed]
- Maher, B. Delusional thinking and cognitive disorder. Integr. Phychol. Behav. Sci. 2005, 40, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Bebbington, P.; Freeman, D. Transdiagnostic Extension of Delusions: Schizophrenia and Beyond. Schizophr. Bull. 2017, 43, 273–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- K⊘rner, A.; Lopez, A.G.; Lauritzen, L.; Andersen, P.K.; Kessing, L.V. Delusional disorder in old age and the risk of developing dementia—A nationwide register-based study. Aging Ment. Health 2008, 12, 625–629. [Google Scholar] [CrossRef] [PubMed]
- Lähteenvuo, M.; Taipale, H.; Tanskanen, A.; Mittendorfer-Rutz, E.; Tiihonen, J. Effectiveness of pharmacotherapies for delusional disorder in a Swedish national cohort of 9076 patients. Schizophr. Res. 2021, 228, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Elkis, H.; Buckley, P.F. Treatment-resistant schizophrenia. Psychiatr. Clin. 2016, 39, 239–265. [Google Scholar] [CrossRef]
- Gillespie, A.L.; Samanaite, R.; Mill, J.; Egerton, A.; MacCabe, J.H. Is treatment-resistant schizophrenia categorically distinctfrom treatment-responsive schizophrenia? A systematic review. BMC Psychiatry 2017, 17, 12. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guàrdia, A.; González-Rodríguez, A.; Seeman, M.V.; Álvarez, A.; Estrada, F.; Acebillo, S.; Labad, J.; Monreal, J.A. Dopamine, Serotonin, and Structure/Function Brain Defects as Biological Bases for Treatment Response in Delusional Disorder: A Systematic Review of Cases and Cohort Studies. Behav. Sci. 2021, 11, 141. https://doi.org/10.3390/bs11100141
Guàrdia A, González-Rodríguez A, Seeman MV, Álvarez A, Estrada F, Acebillo S, Labad J, Monreal JA. Dopamine, Serotonin, and Structure/Function Brain Defects as Biological Bases for Treatment Response in Delusional Disorder: A Systematic Review of Cases and Cohort Studies. Behavioral Sciences. 2021; 11(10):141. https://doi.org/10.3390/bs11100141
Chicago/Turabian StyleGuàrdia, Armand, Alexandre González-Rodríguez, Mary V. Seeman, Aida Álvarez, Francesc Estrada, Sidharta Acebillo, Javier Labad, and José A. Monreal. 2021. "Dopamine, Serotonin, and Structure/Function Brain Defects as Biological Bases for Treatment Response in Delusional Disorder: A Systematic Review of Cases and Cohort Studies" Behavioral Sciences 11, no. 10: 141. https://doi.org/10.3390/bs11100141
APA StyleGuàrdia, A., González-Rodríguez, A., Seeman, M. V., Álvarez, A., Estrada, F., Acebillo, S., Labad, J., & Monreal, J. A. (2021). Dopamine, Serotonin, and Structure/Function Brain Defects as Biological Bases for Treatment Response in Delusional Disorder: A Systematic Review of Cases and Cohort Studies. Behavioral Sciences, 11(10), 141. https://doi.org/10.3390/bs11100141










