1
Department of Biostatistics, Harvard TH Chan School of Public Health, Boston, MA 02120, USA
2
Emergency Preparedness Research Evaluation and Practice (EPREP) Program, Division of Policy Translation and Leadership Development, Harvard TH Chan School of Public Health, Boston, MA 02120, USA
3
Carlo F. Dondena Research Center and COVID Crisis Lab, Bocconi University, 20136 Milan, Italy
4
Centre for Evaluation Methods, Wolfson Institute of Population Health, Barts and The London School of Medicine and Dentistry, Queen Mary University of London, London E1 2AB, UK
Vaccines 2022, 10(10), 1652; https://doi.org/10.3390/vaccines10101652 - 1 Oct 2022
Cited by 5 | Viewed by 2316
Abstract
Vaccine hesitancy is a key contributor to reduced COVID-19 vaccine uptake and remains a threat to COVID-19 mitigation strategies as many countries are rolling out the campaign for booster shots. The goal of our study is to identify and compare the top vaccine
[...] Read more.
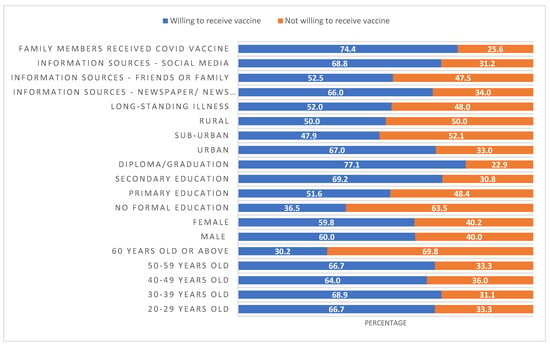
Vaccine hesitancy is a key contributor to reduced COVID-19 vaccine uptake and remains a threat to COVID-19 mitigation strategies as many countries are rolling out the campaign for booster shots. The goal of our study is to identify and compare the top vaccine concerns in four countries: Canada, Italy, Sweden, and the USA and how these concerns relate to vaccine hesitancy. While most individuals in these countries are now vaccinated, we expect our results to be helpful in guiding vaccination efforts for additional doses, and more in general for other vaccines in the future. We sought to empirically test whether vaccine related concerns followed similar thematic issues in the four countries included in this study, and then to see how these themes related to vaccine hesitancy using data from a cross-sectional survey conducted in May 2021. We applied CFA and created vaccine concern scales for analysis. We then utilized these results in regression-based modeling to determine how concerns related to vaccine hesitancy and whether there were similar or different concerns by country. The results quantitatively highlight that the same vaccine related concerns permeated multiple countries at the same point in time. This implies that COVID-19 vaccination communications could benefit from global collaboration.
Full article
(This article belongs to the Special Issue Vaccination and Public Health)
▼
Show Figures