Lumbopelvic Stabilization with Two Methods of Triangular Osteosynthesis: A Biomechanical Study
Abstract
:1. Introduction
2. Materials and Methods
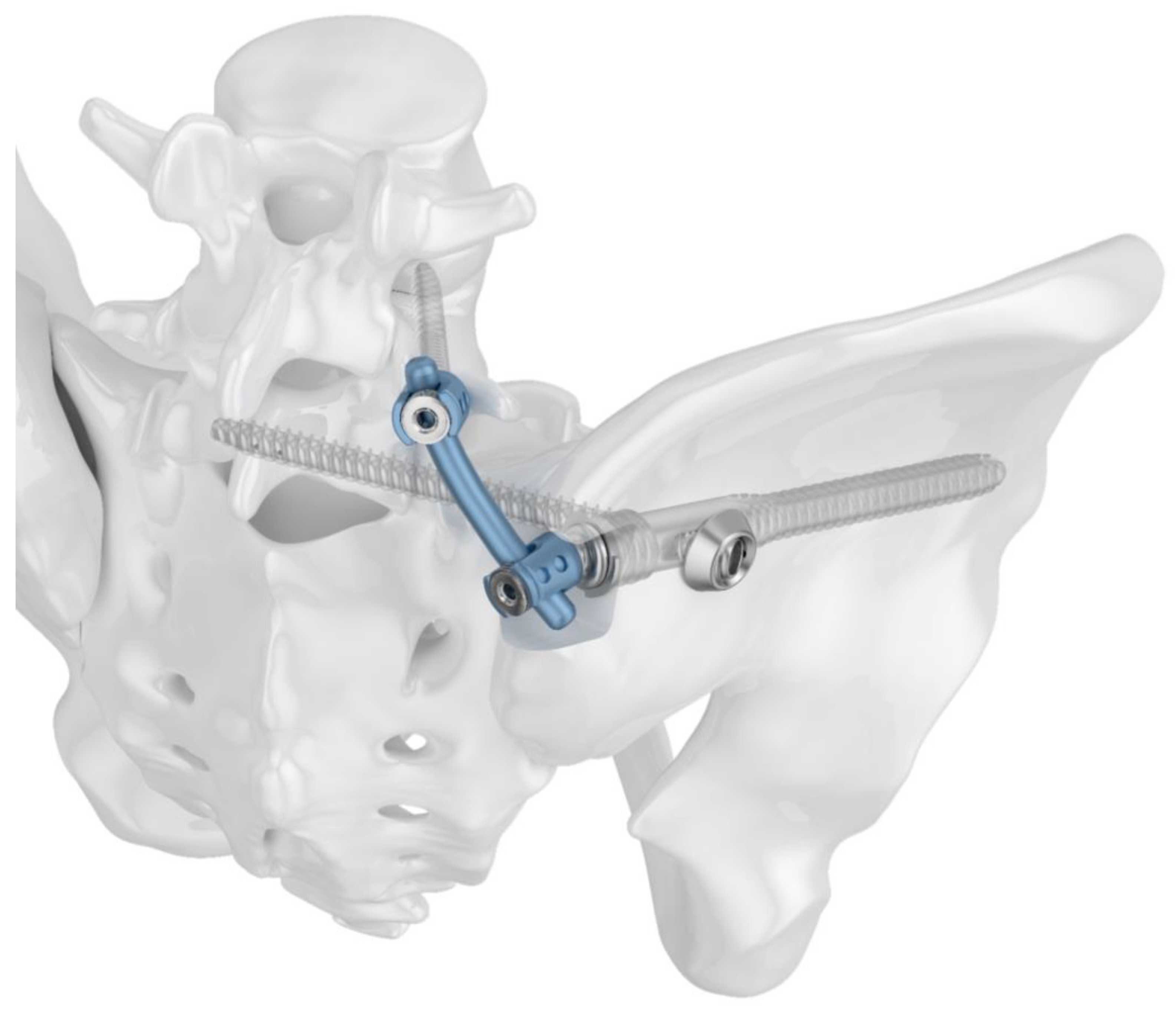
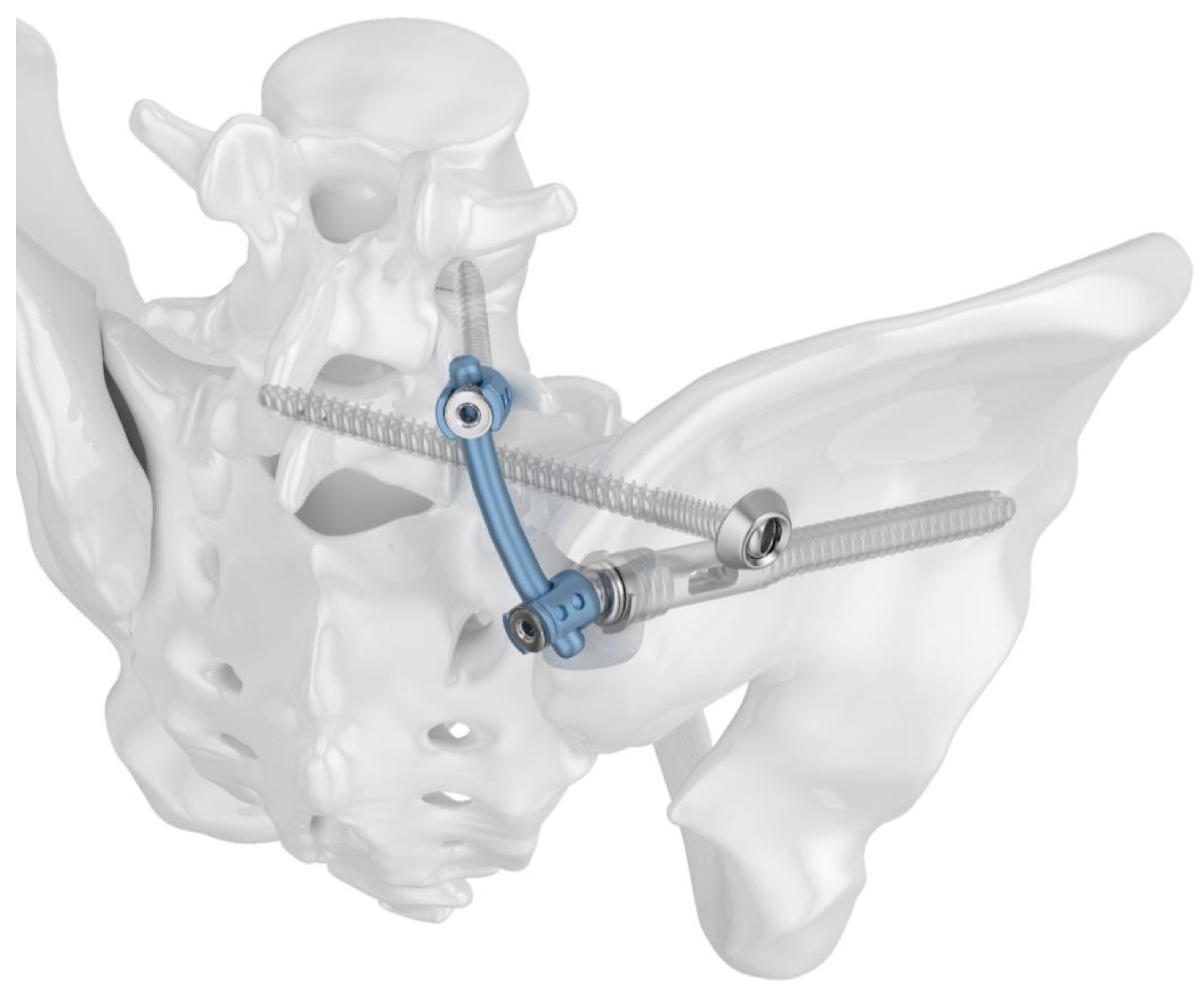
2.1. Implants
2.2. Bone Model
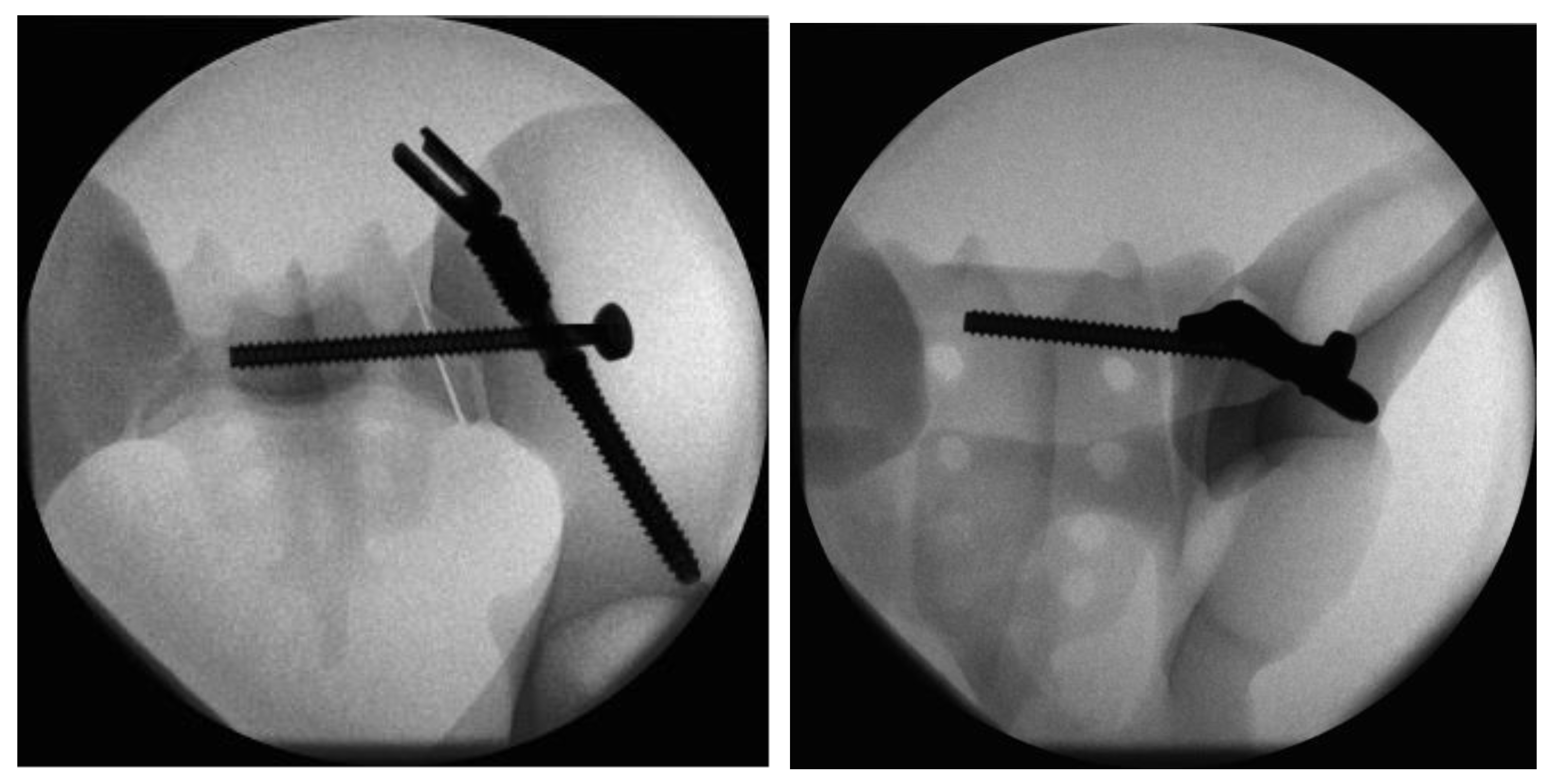
2.3. Fracture Model and Instrumentation
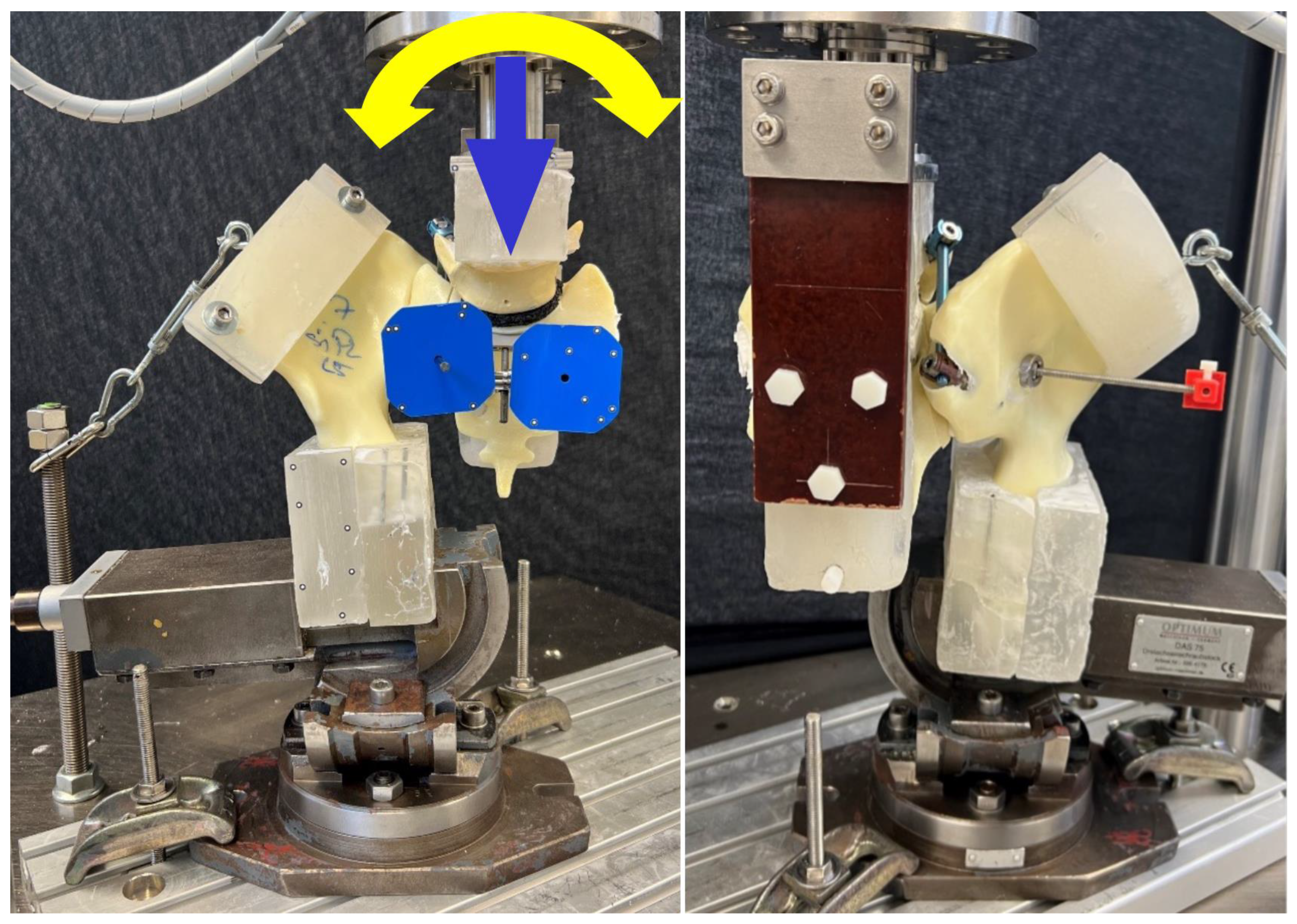
2.4. Biomechanical Testing
2.5. Data Evaluation
2.6. Statistics
3. Results
3.1. Initial Stiffness
3.2. Sacral Screw Cutout and Screw Loosening in Iliac Bone
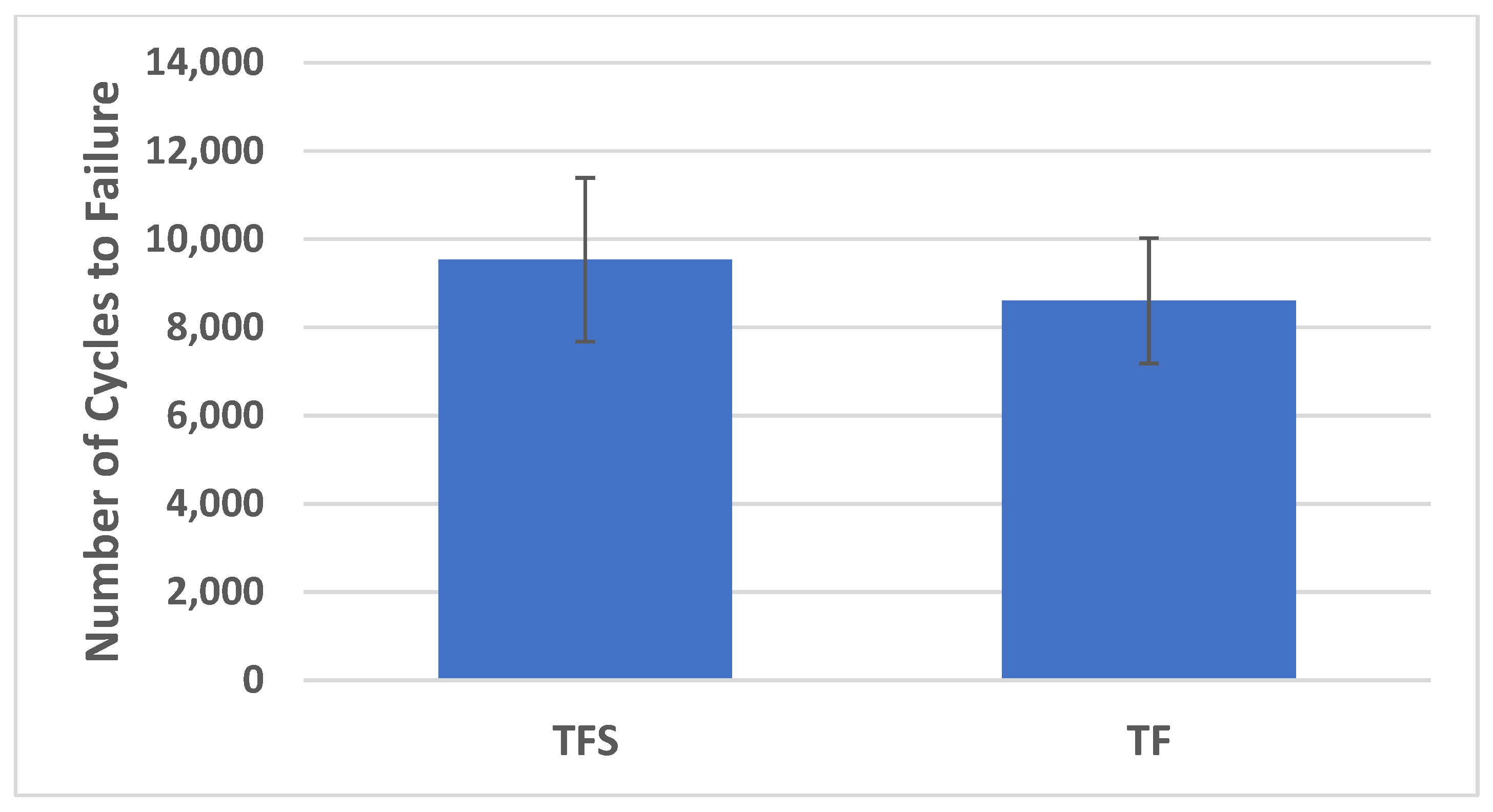
3.3. Cycles to Failure
3.4. Catastrophic Construct Failure Mode
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Audretsch, C.K.; Siegemund, A.; Ellmerer, A.; Herath, S.C. Sex Differences in Pelvic Fractures-a Retrospective Analysis of 16 359 Cases from the German Trauma Registry. Dtsch. Arztebl. Int. 2023, 120, 221–222. [Google Scholar] [CrossRef] [PubMed]
- Rollmann, M.F.; Herath, S.C.; Kirchhoff, F.; Braun, B.J.; Holstein, J.H.; Pohlemann, T.; Menger, M.D.; Histing, T. Pelvic ring fractures in the elderly now and then—A pelvic registry study. Arch. Gerontol. Geriatr. 2017, 71, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Rommens, P.M.; Hofmann, A. The FFP-classification: From eminence to evidence. Injury 2023, 54 (Suppl. S3), S10–S19. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, T.; Rottbeck, U.; Hofbauer, V.; Raschke, M.; Stange, R. Beckenringfrakturen im Alter. Der Unfallchirurg 2011, 114, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Riesner, H.J.; Palm, H.G.; Friemert, B.; Lang, P.; Ag Becken, D.G.U. [Triangular minimally invasive spinopelvic stabilization for type C pelvic fractures according to AO/OTA and type IV according to FFP]. Der Unfallchirurg 2021, 124, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Aude, M.; Jean-Jacques, B.; Laura, I.; Felicia, B.; Alexia, C.; Serge, R.; Mureille, S.; Pierre, B.; Florence, B. Fracture distribution in postmenopausal women: A FRISBEE sub-study. Arch. Osteoporos. 2022, 18, 3. [Google Scholar] [CrossRef] [PubMed]
- Maier, G.S.; Kolbow, K.; Lazovic, D.; Horas, K.; Roth, K.E.; Seeger, J.B.; Maus, U. Risk factors for pelvic insufficiency fractures and outcome after conservative therapy. Arch. Gerontol. Geriatr. 2016, 67, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Rommens, P.M.; Hofmann, A.; Kraemer, S.; Kisilak, M.; Boudissa, M.; Wagner, D. Operative treatment of fragility fractures of the pelvis: A critical analysis of 140 patients. Eur. J. Trauma Emerg. Surg. 2022, 48, 2881–2896. [Google Scholar] [CrossRef] [PubMed]
- Bukata, S.V.; Digiovanni, B.F.; Friedman, S.M.; Hoyen, H.; Kates, A.; Kates, S.L.; Mears, S.C.; Mendelson, D.A.; Serna, F.H., Jr.; Sieber, F.E.; et al. A guide to improving the care of patients with fragility fractures. Geriatr. Orthop. Surg. Rehabil. 2011, 2, 5–37. [Google Scholar] [CrossRef]
- Gribnau, A.J.; van Hensbroek, P.B.; Haverlag, R.; Ponsen, K.J.; Been, H.D.; Goslings, J.C. U-shaped sacral fractures: Surgical treatment and quality of life. Injury 2009, 40, 1040–1048. [Google Scholar] [CrossRef]
- Hunt, N.; Jennings, A.; Smith, M. Current management of U-shaped sacral fractures or spino-pelvic dissociation. Injury 2002, 33, 123–126. [Google Scholar] [CrossRef]
- Yi, C.; Hak, D.J. Traumatic spinopelvic dissociation or U-shaped sacral fracture: A review of the literature. Injury 2012, 43, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Prost, S.; Boudissa, M.; Fuentes, S.; Tropiano, P.; Tonetti, J.; Blondel, B. Minimally invasive triangular lumboiliac and iliosacral fixation of posterior pelvic ring injuries with vertical instability: Technical note. Orthop. Traumatol. Surg. Res. 2021, 107, 102993. [Google Scholar] [CrossRef]
- Ruatti, S.; Kerschbaumer, G.; Gay, E.; Milaire, M.; Merloz, P.; Tonetti, J. Technique for reduction and percutaneous fixation of U- and H-shaped sacral fractures. Orthop. Traumatol. Surg. Res. 2013, 99, 625–629. [Google Scholar] [CrossRef] [PubMed]
- Kulakowski, M.; Reichert, P.; Elster, K.; Sleczka, P.; Oleksy, L.; Krolikowska, A. Safety and efficacy of two ilioiliac tension band plates osteosynthesis of fragility fractures of the pelvis. Sci. Rep. 2022, 12, 20436. [Google Scholar] [CrossRef]
- Schmerwitz, I.U.; Jungebluth, P.; Lehmann, W.; Hockertz, T.J. Minimally invasive posterior locked compression plate osteosynthesis shows excellent results in elderly patients with fragility fractures of the pelvis. Eur. J. Trauma Emerg. Surg. 2021, 47, 37–45. [Google Scholar] [CrossRef]
- Boudissa, M.; Saad, M.; Kerschbaumer, G.; Ruatti, S.; Tonetti, J. Posterior transiliac plating in vertically unstable sacral fracture. Orthop. Traumatol. Surg. Res. 2020, 106, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Mehling, I.; Hessmann, M.H.; Rommens, P.M. Stabilization of fatigue fractures of the dorsal pelvis with a trans-sacral bar. Operative technique and outcome. Injury 2012, 43, 446–451. [Google Scholar] [CrossRef]
- Schildhauer, T.A.; Josten, C.; Muhr, G. Triangular osteosynthesis of vertically unstable sacrum fractures: A new concept allowing early weight-bearing. J. Orthop. Trauma 1998, 12, 307–314. [Google Scholar] [CrossRef]
- Yoshimura, S.; Inoue, M.; Nakajima, T.; Kubota, G.; Sato, Y.; Arai, T.; Orita, S.; Eguchi, Y.; Inage, K.; Shiga, Y.; et al. Minimally Invasive “Crab-Shaped Fixation” for Treating Patients with Fragility Fractures of the Pelvis. Spine Surg. Relat. Res. 2021, 5, 425–430. [Google Scholar] [CrossRef]
- Berk, T.; Zderic, I.; Schwarzenberg, P.; Halvachizadeh, S.; Teuben, M.; Richards, G.; Gueorguiev, B.; Pape, H.C. Cerclage augmentation of S1-S2 transsacral screw fixation in osteoporotic posterior pelvis ring injuries: A biomechanical feasibility study. J. Orthop. Res. 2023, 41, 2740–2748. [Google Scholar] [CrossRef]
- Kassem, E.; Khaled, S.A.; Karim, M.A.; El-Hamalawy, A.G.; Fahmy, M. Does minimally invasive percutaneous transilial internal fixator became an effective option for sacral fractures? A prospective study with novel implantation technique. Eur. J. Trauma Emerg. Surg. 2023, 49, 1535–1544. [Google Scholar] [CrossRef]
- Bozorgmanesh, M.; Latifi, R.; Hassannejad, N. Innovative Technique for Posterior Fixation of Vertically Unstable Pelvic Ring Fracture: A Case Report. Arch. Bone Jt. Surg. 2023, 11, 658–661. [Google Scholar] [CrossRef]
- Fan, S.; Luo, H.; Chen, S.; Xiang, H.; Mai, Q.; Zhu, Z.; Chen, Y.; Hou, Z.; Chen, W.; Zhu, Q.; et al. Effect of different lumbar-iliac fixation and sacral slope for Tile C1.3 pelvic fractures: A biomechanical study. J. Orthop. Traumatol. 2024, 25, 32. [Google Scholar] [CrossRef] [PubMed]
- Rovere, G.; De Mauro, D.; Smakaj, A.; Sassara, G.; De Vitis, R.; Farsetti, P.; Camarda, L.; Maccauro, G.; Liuzza, F. Triangular osteosynthesis and lumbopelvic fixation as a valid surgical treatment in posterior pelvic ring lesions: A systematic review. Front. Surg. 2024, 11, 1266393. [Google Scholar] [CrossRef] [PubMed]
- Steelman, K.; Bray, R.; Vaidya, R. Technical Note on Placement of Low-Profile Triangular Osteosynthesis for Unstable Posterior Pelvic Ring Injuries. J. Orthop. Trauma 2022, 36, e337–e342. [Google Scholar] [CrossRef]
- Gruneweller, N.; Leunig, J.; Zderic, I.; Gueorguiev, B.; Wahnert, D.; Vordemvenne, T. Stabilization of Traumatic Iliosacral Instability Using Innovative Implants: A Biomechanical Comparison. J. Clin. Med. 2023, 13, 194. [Google Scholar] [CrossRef] [PubMed]
- Zderic, I.; Wagner, D.; Schopper, C.; Lodde, M.; Richards, G.; Gueorguiev, B.; Rommens, P.; Acklin, Y.P. Screw-in-screw fixation of fragility sacrum fractures provides high stability without loosening-biomechanical evaluation of a new concept. J. Orthop. Res. 2021, 39, 761–770. [Google Scholar] [CrossRef]
- Josten, C.; Schildhauer, T.A.; Muhr, G. [Therapy of unstable sacrum fractures in pelvic ring. Results of of osteosynthesis with early mobilization]. Chirurg 1994, 65, 970–975. [Google Scholar]
- Schildhauer, T.A.; Ledoux, W.R.; Chapman, J.R.; Henley, M.B.; Tencer, A.F.; Routt, M.L., Jr. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: A cadaveric and biomechanical evaluation under cyclic loads. J. Orthop. Trauma 2003, 17, 22–31. [Google Scholar] [CrossRef]
- Keel, M.J.; Benneker, L.M.; Siebenrock, K.A.; Bastian, J.D. Less invasive lumbopelvic stabilization of posterior pelvic ring instability: Technique and preliminary results. J. Trauma 2011, 71, E62–E70. [Google Scholar] [CrossRef] [PubMed]
- Schmal, H.; Froberg, L.; Larsen, M.S.; Sudkamp, N.P.; Pohlemann, T.; Aghayev, E.; Goodwin Burri, K. Evaluation of strategies for the treatment of type B and C pelvic fractures: Results from the German Pelvic Injury Register. Bone Joint J. 2018, 100-B, 973–983. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, F.; Bățagă, T. Torque Control during Bone Insertion of Cortical Screws. Procedia Manuf. 2020, 46, 484–490. [Google Scholar] [CrossRef]
- Gruneweller, N.; Raschke, M.J.; Zderic, I.; Widmer, D.; Wahnert, D.; Gueorguiev, B.; Richards, R.G.; Fuchs, T.; Windolf, M. Biomechanical comparison of augmented versus non-augmented sacroiliac screws in a novel hemi-pelvis test model. J. Orthop. Res. 2017, 35, 1485–1493. [Google Scholar] [CrossRef] [PubMed]
- Oberkircher, L.; Masaeli, A.; Bliemel, C.; Debus, F.; Ruchholtz, S.; Krüger, A. Primary stability of three different iliosacral screw fixation techniques in osteoporotic cadaver specimens-a biomechanical investigation. Spine J. 2016, 16, 226–232. [Google Scholar] [CrossRef]
- Oberkircher, L.; Masaeli, A.; Hack, J.; Figiel, J.; Bliemel, C.; Ruchholtz, S.; Kruger, A. Pull-out strength evaluation of cement augmented iliac screws in osteoporotic spino-pelvic fixation. Orthop. Traumatol. Surg. Res. 2021, 107, 102945. [Google Scholar] [CrossRef] [PubMed]
- Yinger, K.; Scalise, J.; Olson, S.A.; Bay, B.K.; Finkemeier, C.G. Biomechanical comparison of posterior pelvic ring fixation. J. Orthop. Trauma 2003, 17, 481–487. [Google Scholar] [CrossRef]
- Goncalves, R.M.; Freitas, A.; Aragao, V.A.D.; Azevedo, F.E.R.; Lopes, N.B.; Mangueira, L.J.A.; da Silva, L.H.P.; Pires, R.E.; Giordano, V. Comparison of sacroiliac screw techniques for unstable sacroiliac joint disruptions: A finite element model analysis. Injury 2023, 54 (Suppl. S6), 110783. [Google Scholar] [CrossRef]
- Wagner, D.; Kamer, L.; Rommens, P.M.; Sawaguchi, T.; Richards, R.G.; Noser, H. 3D statistical modeling techniques to investigate the anatomy of the sacrum, its bone mass distribution, and the trans-sacral corridors. J. Orthop. Res. 2014, 32, 1543–1548. [Google Scholar] [CrossRef]
- Wagner, D.; Kamer, L.; Sawaguchi, T.; Noser, H.; Uesugi, M.; Baranowski, A.; Gruszka, D.; Rommens, P.M. Space available for trans-sacral implants to treat fractures of the pelvis assessed by virtual implant positioning. Arch. Orthop. Trauma Surg. 2019, 139, 1385–1391. [Google Scholar] [CrossRef]
- Wu, Q.; Zhang, Y.; Wang, S.; Liu, R.; Liu, G. Different Lengths of Percutaneous Transverse Iliosacral Screw in Geometric Osseous Fixation Pathway: A Finite-Element Analysis. Indian J. Orthop. 2022, 56, 1354–1362. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Zhang, S.; Sun, T.; Wang, D.; Lian, W.; Tan, J.; Zou, D.; Zhao, Y. Mechanical comparison between lengthened and short sacroiliac screws in sacral fracture fixation: A finite element analysis. Orthop. Traumatol. Surg. Res. 2013, 99, 601–606. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, S.; Nishida, N.; Soehnlen, S.; Kelkar, A.; Kumaran, Y.; Seki, T.; Sakai, T.; Goel, V.K. Pelvic Ring Fractures: A Biomechanical Comparison of Sacral and Lumbopelvic Fixation Techniques. Bioengineering 2024, 11, 348. [Google Scholar] [CrossRef] [PubMed]
- Cintean, R.; Fritzsche, C.; Zderic, I.; Gueorguiev-Ruegg, B.; Gebhard, F.; Schutze, K. Sacroiliac versus transiliac-transsacral screw osteosynthesis in osteoporotic pelvic fractures: A biomechanical comparison. Eur. J. Trauma Emerg. Surg. 2023, 49, 2553–2560. [Google Scholar] [CrossRef] [PubMed]
- Fradet, L.; Bianco, R.J.; Tatsumi, R.; Coleman, J.; Aubin, C.E. Biomechanical comparison of sacral and transarticular sacroiliac screw fixation. Spine Deform. 2020, 8, 853–862. [Google Scholar] [CrossRef] [PubMed]
- Vanderschot, P.; Kuppers, M.; Sermon, A.; Lateur, L. Trans-iliac-sacral-iliac-bar procedure to treat insufficiency fractures of the sacrum. Indian J. Orthop. 2009, 43, 245–252. [Google Scholar] [CrossRef]
- Wagner, D.; Kisilak, M.; Porcheron, G.; Kramer, S.; Mehling, I.; Hofmann, A.; Rommens, P.M. Trans-sacral bar osteosynthesis provides low mortality and high mobility in patients with fragility fractures of the pelvis. Sci. Rep. 2021, 11, 14201. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Zhao, Y.; Hong, H.; Huang, T.; Li, Y. Biomechanical comparison of four triangular osteosynthesis fixations for unilateral vertical sacral fractures. Sci. Rep. 2023, 13, 4424. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Zhang, G.; Zhang, S.; Ji, X.; Li, J.; Du, C.; Zhao, W.; Zhang, L. Biomechanical study of transsacral-transiliac screw fixation versus lumbopelvic fixation and bilateral triangular fixation for “H”- and “U”-type sacrum fractures with traumatic spondylopelvic dissociation: A finite element analysis study. J. Orthop. Surg. Res. 2021, 16, 428. [Google Scholar] [CrossRef]
- Sawada, R.; Ishikawa, T.; Ota, M.; Katsuragi, J.; Sasaki, Y.; Suzuki, M.; Umimura, T.; Nagashima, Y.; Hashiba, D.; Yoshimoto, T.; et al. Novel within ring fixation using iliac screws and an iliosacral screw locking system technique for fragility fracture of the pelvis. Surg. Neurol. Int. 2022, 13, 421. [Google Scholar] [CrossRef]
- Gruneweller, N.; Wahnert, D.; Vordemvenne, T. Instability of the posterior pelvic ring: Introduction of innovative implants. J. Orthop. Surg. Res. 2021, 16, 625. [Google Scholar] [CrossRef] [PubMed]
- Lodde, M.F.; Katthagen, J.C.; Schopper, C.O.; Zderic, I.; Richards, G.; Gueorguiev, B.; Raschke, M.J.; Hartensuer, R. Biomechanical Comparison of Five Fixation Techniques for Unstable Fragility Fractures of the Pelvic Ring. J. Clin. Med. 2021, 10, 2326. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grüneweller, N.; Leunig, J.; Zderic, I.; Gueorguiev, B.; Colcuc, C.; Wähnert, D.; Vordemvenne, T. Lumbopelvic Stabilization with Two Methods of Triangular Osteosynthesis: A Biomechanical Study. J. Clin. Med. 2024, 13, 4744. https://doi.org/10.3390/jcm13164744
Grüneweller N, Leunig J, Zderic I, Gueorguiev B, Colcuc C, Wähnert D, Vordemvenne T. Lumbopelvic Stabilization with Two Methods of Triangular Osteosynthesis: A Biomechanical Study. Journal of Clinical Medicine. 2024; 13(16):4744. https://doi.org/10.3390/jcm13164744
Chicago/Turabian StyleGrüneweller, Niklas, Julia Leunig, Ivan Zderic, Boyko Gueorguiev, Christian Colcuc, Dirk Wähnert, and Thomas Vordemvenne. 2024. "Lumbopelvic Stabilization with Two Methods of Triangular Osteosynthesis: A Biomechanical Study" Journal of Clinical Medicine 13, no. 16: 4744. https://doi.org/10.3390/jcm13164744





