Imaging of Osteosarcoma: Presenting Findings, Metastatic Patterns, and Features Related to Prognosis
Abstract
:1. Introduction
2. Initial Radiological Features Associated with the Diagnosis of Osteosarcoma and Its Histological Subtypes
2.1. Imaging Modalities Recommended for Local, Regional, and Distant Staging in Osteosarcomas
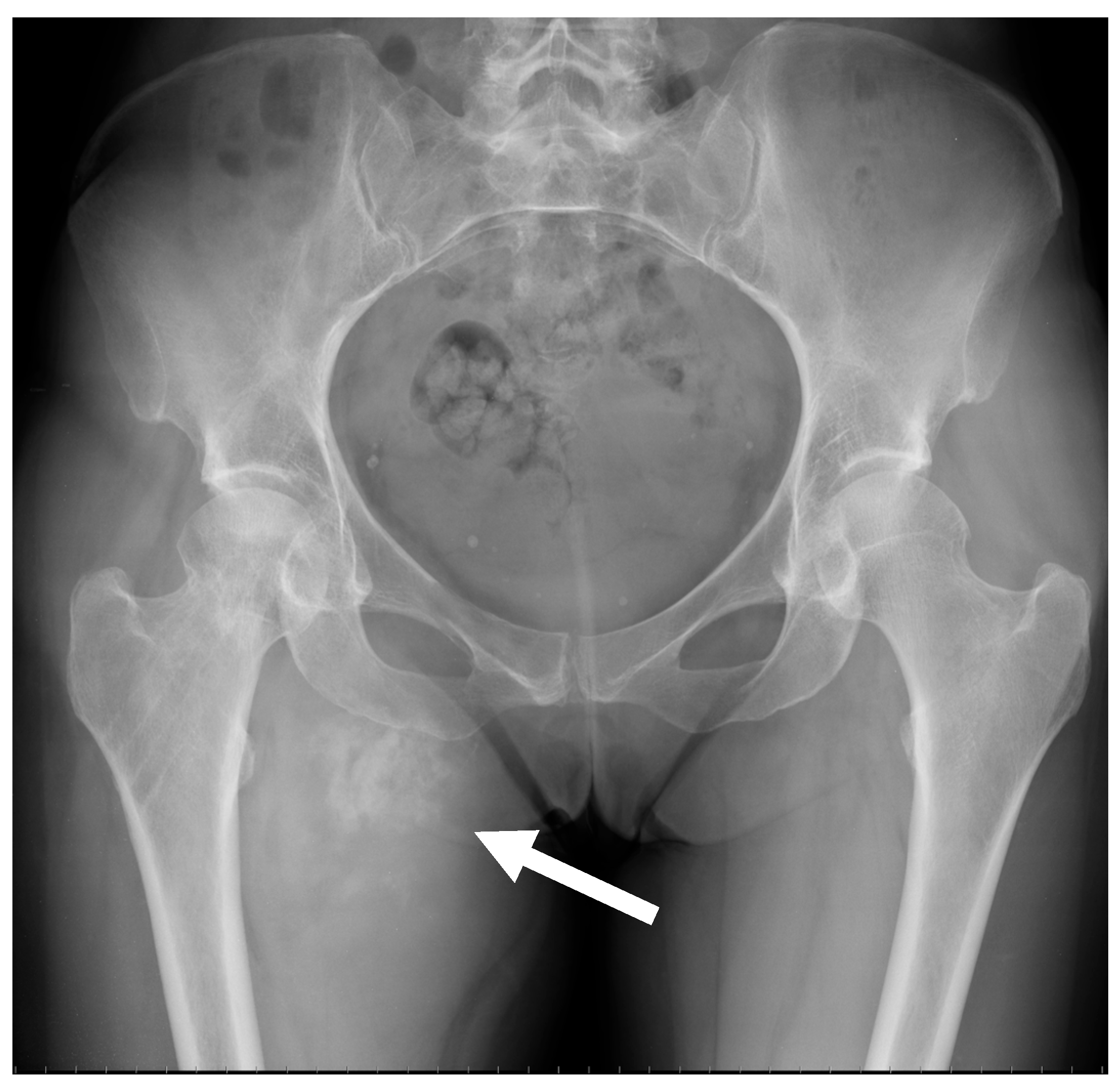
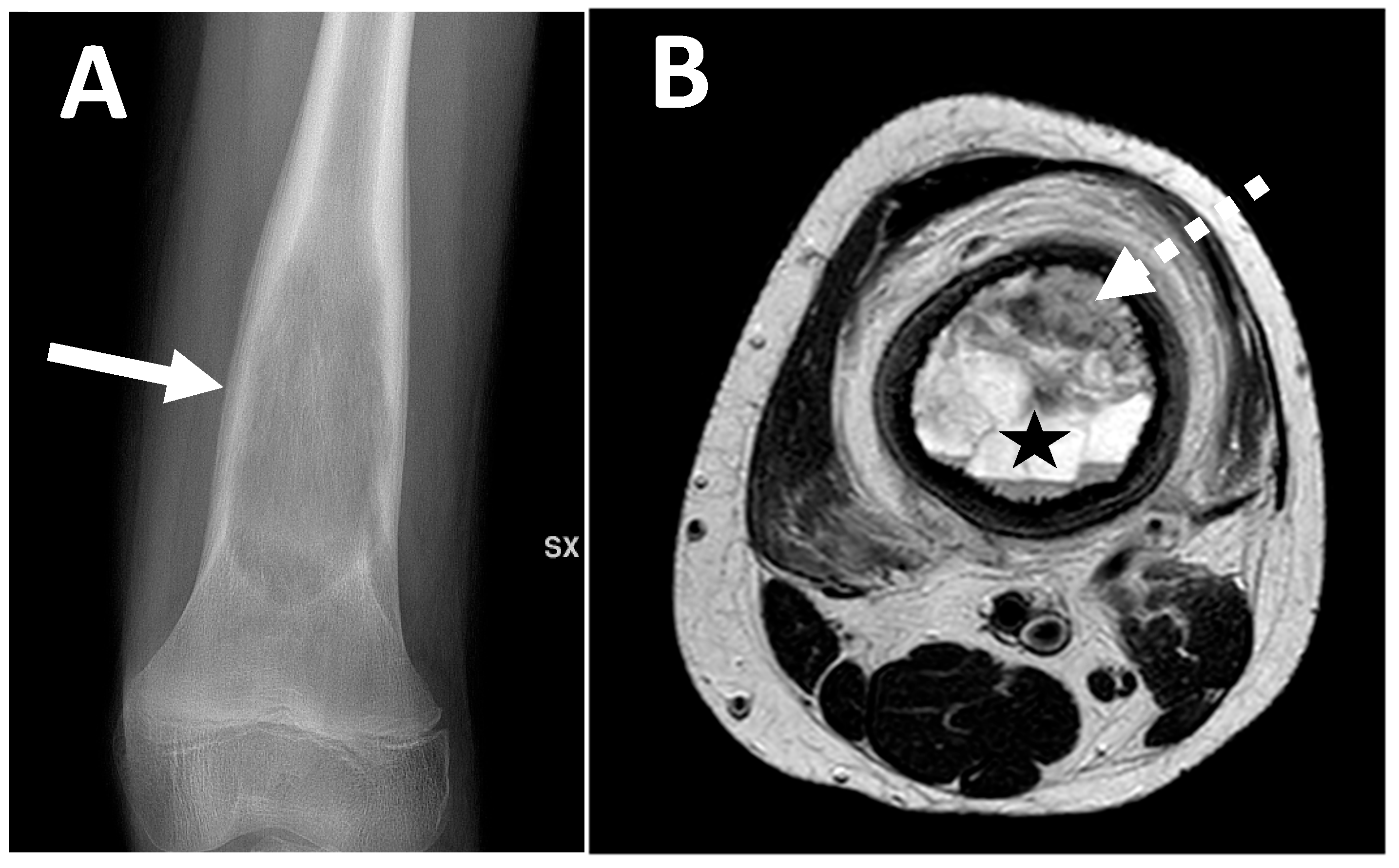
2.2. Radiological Findings on Conventional Radiographs
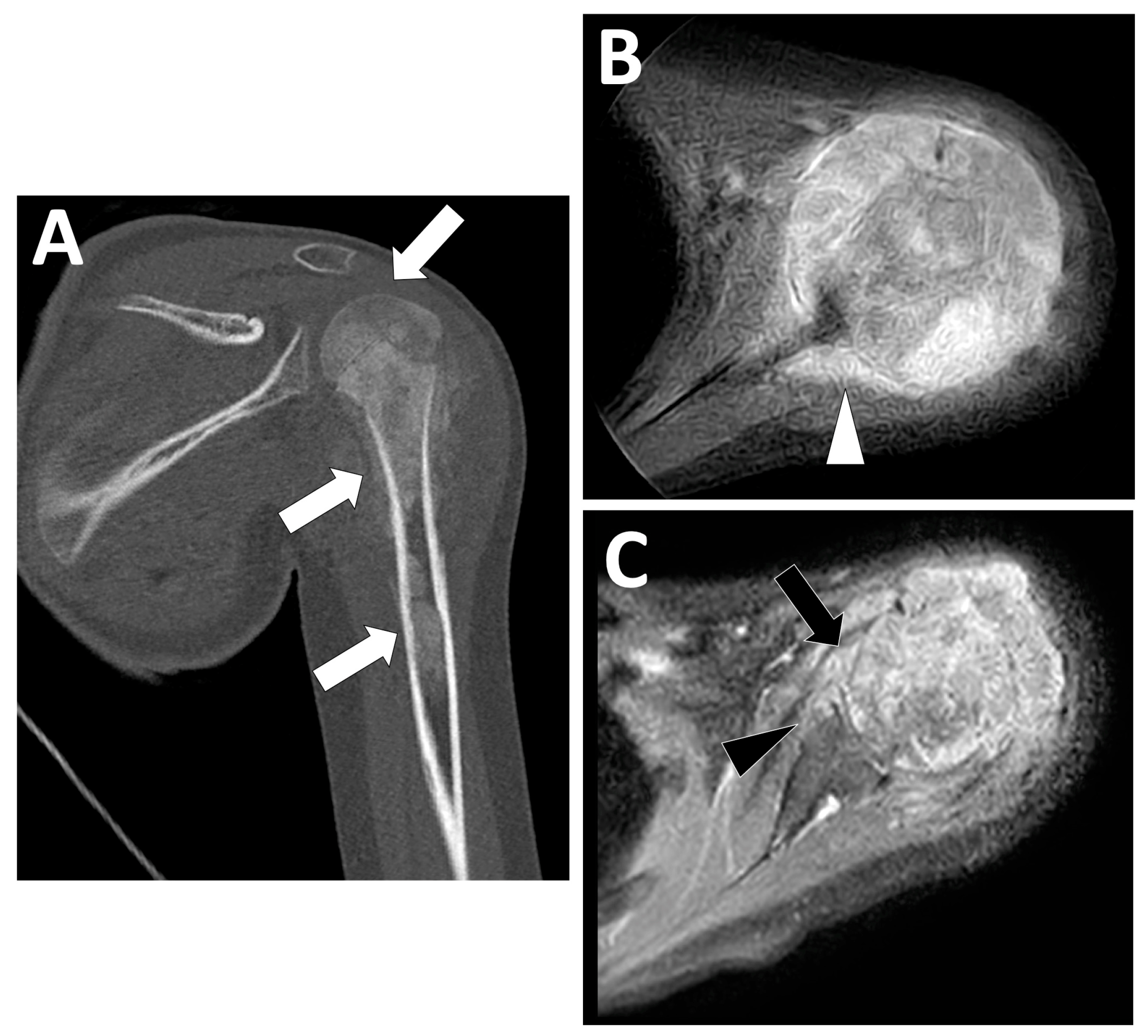
2.3. Radiological Findings on CT
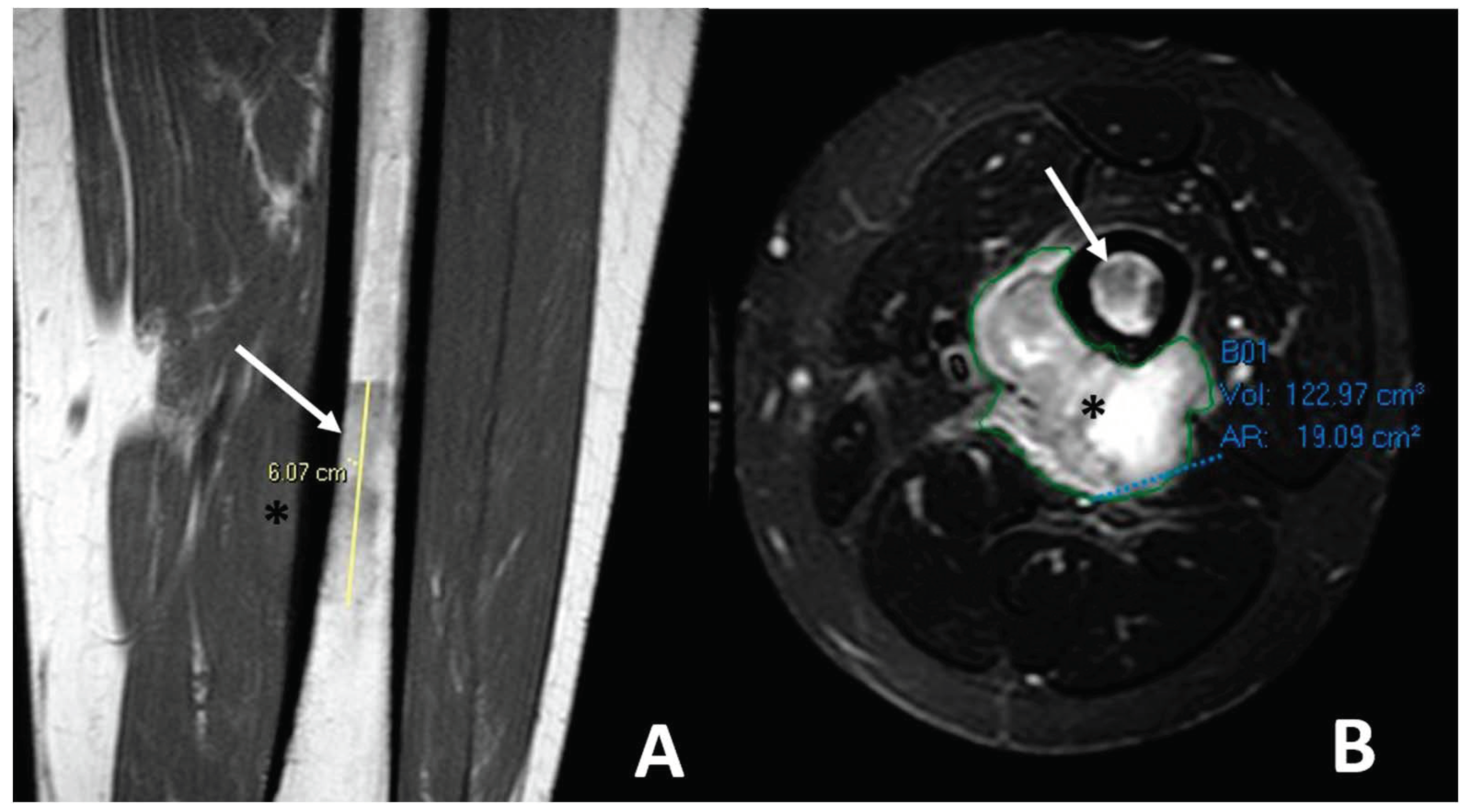
2.4. Radiological Findings on MRI
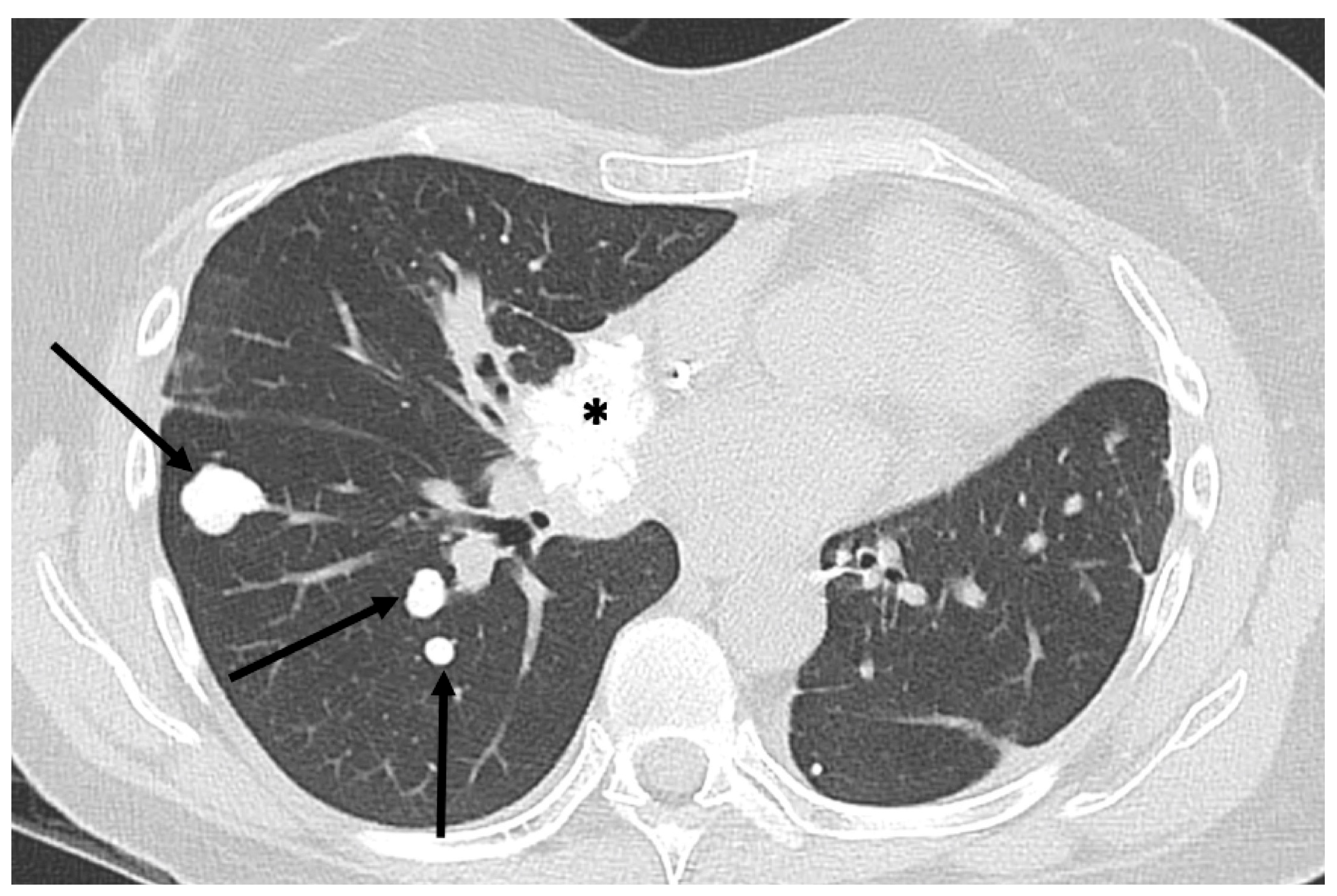
3. Metastatic Patterns of Osteosarcoma
4. Associations between Imaging Features and Patient Outcomes
4.1. Associations with the Response to Neoadjuvant Chemotherapy
4.1.1. Semantic Radiological Findings
4.1.2. Quantitative and Functional Imaging
4.1.3. Predictive Radiomics Models
4.2. Associations with EFS and OS
4.2.1. Semantic Radiological Findings
4.2.2. Quantitative and Functional Imaging
4.2.3. Predictive Radiomics Models
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kundu, Z.S. Classification, imaging, biopsy and staging of osteosarcoma. Indian J. Orthop. 2014, 48, 238–246. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yarmish, G.; Klein, M.J.; Landa, J.; Lefkowitz, R.A.; Hwang, S. Imaging characteristics of primary osteosarcoma: Nonconventional subtypes. Radiographics 2010, 30, 1653–1672. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, C.D.M.; Bridge, J.A.; Hogendoorn, P.C.W.; Martens, F. WHO Classification of Tumours of Soft Tissue and Bone, 5th ed.; IARC Press: Lyon, France, 2020. [Google Scholar]
- Picci, P. Osteosarcomas (OS). In Diagnosis of Musculoskeletal Tumors and Tumor-like Conditions; Picci, P., Manfrini, M., Donati, D.M., Gambarotti, M., Righi, A., Vanel, D., Dei Tos, A.P., Eds.; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Fuchs, B.; Pritchard, D.J. Etiology of osteosarcoma. Clin. Orthop. Relat. Res. 2002, 397, 40–52. [Google Scholar] [CrossRef] [PubMed]
- Bielack, S.S.; Kempf-Bielack, B.; Delling, G.; Exner, G.U.; Flege, S.; Helmke, K.; Kotz, R.; Salzer-Kuntschik, M.; Werner, M.; Winkelmann, W.; et al. Prognostic Factors in High-Grade Osteosarcoma of theExtremities or Trunk: An Analysis of 1,702 Patients Treatedon Neoadjuvant Cooperative Osteosarcoma Study GroupProtocols. J. Clin. Oncol. 2023, 41, 4323–4337. [Google Scholar] [CrossRef] [PubMed]
- Smeland, S.; Bielack, S.S.; Whelan, J.; Bernstein, M.; Hogendoorn, P.; Krailo, M.D.; Gorlick, R.; Janeway, K.A.; Ingleby, F.C.; Anninga, J.; et al. Survival and prognosis with osteosarcoma: Outcomes in more than 2000 patients in the EURAMOS-1 (European and American Osteosarcoma Study) cohort. Eur. J. Cancer 2019, 109, 36–50. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Strauss, S.J.; Frezza, A.M.; Abecassis, N.; Bajpai, J.; Bauer, S.; Biagini, R.; Bielack, S.; Blay, J.Y.; Bolle, S.; Bonvalot, S.; et al. Bone sarcomas: ESMO-EURACAN-GENTURIS-ERN PaedCan Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2021, 32, 1520–1536. [Google Scholar] [CrossRef] [PubMed]
- Crombé, A.; Spinnato, P.; Righi, A.; Leopardi, M.P.; Carpenzano, M.; Izzo, F.; Parmeggiani, A.; Linck, P.A.; Perret, R.; Cesari, M.; et al. Imaging presentation of extraskeletal osteosarcomas on CT and MRI and correlation with patients outcome: A two-center retrospective study of 54 patients. Diagn. Interv. Imaging 2023, 104, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Picci, P.; Bacci, G.; Campanacci, M.; Gasparini, M.; Pilotti, S.; Cerasoli, S.; Bertoni, F.; Guerra, A.; Capanna, R.; Albisinni, U.; et al. Histologic evaluation of necrosis in osteosarcoma induced by chemotherapy regional mapping of viable and nonviable tumor. Cancer 1985, 56, 1515–1521. [Google Scholar] [CrossRef] [PubMed]
- Clara-Altamirano, M.A.; García-Ortega, D.Y.; Álvarez-Cano, A.; Velázquez-Rodríguez, S.; Lizcano-Suárez, A.R.; Rosas, L.C.; Uribe-Saloma, C.E.; Martínez-Said, H.; Villavicencio-Valencia, V.; Cuellar-Hubbe, M. Retraso en el diagnóstico de osteosarcoma en adultos: Un factor pronóstico que debemos considerar [Delayed diagnosis of osteosarcoma in adults: A prognostic factor to be considered]. Acta Ortop. Mex. 2024, 38, 164–171. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- Delfaut, E.M.; Beltran, J.; Johnson, G.; Rousseau, J.; Marchandise, X.; Cotten, A. Fat suppression in MR imaging: Techniques and pitfalls. Radiographics 1999, 19, 373–382, Erratum in Radiographics 1999, 19, 1092. [Google Scholar] [CrossRef] [PubMed]
- Kalisvaart, G.M.; Van Den Berghe, T.; Grootjans, W.; Lejoly, M.; Huysse, W.C.J.; Bovée, J.V.M.G.; Creytens, D.; Gelderblom, H.; Speetjens, F.M.; Lapeire, L.; et al. Evaluation of response to neoadjuvant chemotherapy in osteosarcoma using dynamic contrast-enhanced MRI: Development and external validation of a model. Skelet. Radiol. 2024, 53, 319–328. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guirguis, A.; Polster, J.; Karim, W.; Obuchowski, N.; Rosneck, J.; Goodwin, R.; Subhas, N. Interchangeability of CT and 3D “pseudo-CT” MRI for preoperative planning in patients with femoroacetabular impingement. Skelet. Radiol. 2020, 49, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Lodwick, G.S.; Wilson, A.J.; Farrell, C.; Virtama, P.; Dittrich, F. Determining growth rates of focal lesions of bone from radiographs. Radiology 1980, 134, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Zambo, I.; Veselý, K. WHO classification of tumours of soft tissue and bone 2013: The main changes compared to the 3rd edition. Cesk Patol. 2014, 50, 64–70. (In Czech) [Google Scholar] [PubMed]
- Nguyen, J.C.; Baghdadi, S.; Pogoriler, J.; Guariento, A.; Rajapakse, C.S.; Arkader, A. Pediatric Osteosarcoma: Correlation of Imaging Findings with Histopathologic Features, Treatment, and Outcome. Radiographics 2022, 42, 1196–1213. [Google Scholar] [CrossRef] [PubMed]
- Costelloe, C.M.; Madewell, J.E. Radiography in the initial diagnosis of primary bone tumors. AJR Am. J. Roentgenol. 2013, 200, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Madewell, J.E.; Ragsdale, B.D.; Sweet, D.E. Radiologic and pathologic analysis of solitary bone lesions. Part I: Internal margins. Radiol. Clin. N. Am. 1981, 19, 715–748. [Google Scholar] [CrossRef] [PubMed]
- Mehta, K.; McBee, M.P.; Mihal, D.C.; England, E.B. Radiographic Analysis of Bone Tumors: A Systematic Approach. Semin. Roentgenol. 2017, 52, 194–208. [Google Scholar] [CrossRef] [PubMed]
- Goyal, N.; Kalra, M.; Soni, A.; Baweja, P.; Ghonghe, N.P. Multi-modality imaging approach to bone tumors—State-of-the art. J. Clin. Orthop. Trauma 2019, 10, 687–701. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Onikul, E.; Fletcher, B.D.; Parham, D.M.; Chen, G. Accuracy of MR imaging for estimating intraosseous extent of osteosarcoma. AJR Am. J. Roentgenol. 1996, 167, 1211–1215. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, B.D.; Wall, J.E.; Hanna, S.L. Effect of hematopoietic growth factors on MR images of bone marrow in children undergoing chemotherapy. Radiology 1993, 189, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Limaiem, F.; Kuhn, J.; Tiwari, V.; Khaddour, K. Telangiectatic Osteosarcoma. Updated on 3 August 2023; In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK537309/ (accessed on 3 August 2023).
- Sangle, N.A.; Layfield, L.J. Telangiectatic Osteosarcoma. Arch. Pathol. Lab. Med. 2012, 136, 572–576. [Google Scholar] [CrossRef] [PubMed]
- Chiesa, A.M.; Spinnato, P.; Miceli, M.; Facchini, G. Radiologic Assessment of Osteosarcoma Lung Metastases: State of the Art and Recent Advances. Cells 2021, 10, 553. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Oh, C.; Bishop, M.W.; Cho, S.Y.; Im, H.J.; Shulkin, B.L. 18F-FDG PET/CT in the Management of Osteosarcoma. J. Nucl. Med. 2023, 64, 842–851. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Zhang, Q.; Zhou, D.; Dong, J. Effectiveness of 18F-FDG PET/CT in the diagnosis and staging of osteosarcoma: A meta-analysis of 26 studies. BMC Cancer 2019, 19, 323. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Farina, A.; Gasperini, C.; Aparisi Gómez, M.P.; Bazzocchi, A.; Fanti, S.; Nanni, C. The Role of FDG-PET and Whole-Body MRI in High Grade Bone Sarcomas with Particular Focus on Osteosarcoma. Semin. Nucl. Med. 2022, 52, 635–646. [Google Scholar] [CrossRef] [PubMed]
- Karaarslan, E.; Alis, D.; Basar, Y.; Kumbasar, B.; Kalayci, C.B.; Alpan, B.; Ozger, H. The Role of Whole-Body Magnetic Resonance Imaging in Assessing Extrapulmonary Metastases in Osteosarcoma Staging and Restaging: A Pilot Study. J. Comput. Assist. Tomogr. 2023, 47, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Aryal, A.; Kumar, V.S.; Shamim, S.A.; Gamanagatti, S.; Khan, S.A. What Is the Comparative Ability of 18F-FDG PET/CT, 99mTc-MDP Skeletal Scintigraphy, and Whole-body MRI as a Staging Investigation to Detect Skeletal Metastases in Patients with Osteosarcoma and Ewing Sarcoma? Clin. Orthop. Relat. Res. 2021, 479, 1768–1779. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lecouvet, F.E.; Chabot, C.; Taihi, L.; Kirchgesner, T.; Triqueneaux, P.; Malghem, J. Present and future of whole-body MRI in metastatic disease and myeloma: How and why you will do it. Skelet. Radiol. 2024, 53, 1815–1831. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saifuddin, A.; Michelagnoli, M.; Pressney, I. Skip metastases in high-grade intramedullary appendicular osteosarcoma: An indicator of more aggressive disease? Skelet. Radiol. 2021, 50, 2415–2422. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.R. Secondary bone lesions in the affected limb in osteosarcoma (skip lesions), its classification and prognosis. Arch. Orthop. Trauma Surg. 2011, 131, 1351–1355. [Google Scholar] [CrossRef] [PubMed]
- Picci, P. Multicentric Osteosarcoma. In Atlas of Musculoskeletal Tumors and Tumorlike Lesions; Picci, P., Manfrini, M., Fabbri, N., Gambarotti, M., Vanel, D., Eds.; Springer: Cham, Switzerland, 2014. [Google Scholar] [CrossRef]
- Marcove, R.C.; Mike, V.; Hajek, J.V.; Levin, A.G.; Hutter, R.V. Osteogenic sarcoma under the age of 21: A review of 145 operative cases. J. Bone Jt. Surg. 1980, 52A, 411–420. [Google Scholar]
- Brader, P.; Abramson, S.J.; Price, A.P.; Ishill, N.M.; Emily, Z.C.; Moskowitz, C.S.; La Quaglia, M.P.; Ginsberg, M.S. Do characteristics of pulmonary nodules on computed tomography in children with known osteosarcoma help distinguish whether the nodules are malignant or benign? J. Pediatr. Surg. 2011, 46, 729–735. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ghosh, K.M.; Lee, L.H.; Beckingsale, T.B.; Gerrand, C.H.; Rankin, K.S. Indeterminate nodules in osteosarcoma: What’s the follow-up? Br. J. Cancer 2018, 118, 634–638. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ciccarese, F.; Bazzocchi, A.; Ciminari, R.; Righi, A.; Rocca, M.; Rimondi, E.; Picci, P.; Bacchi Reggiani, M.L.; Albisinni, U.; Zompatori, M.; et al. The many faces of pulmonary metastases of osteosarcoma: Retrospective study on 283 lesions submitted to surgery. Eur. J. Radiol. 2015, 84, 2679–2685. [Google Scholar] [CrossRef] [PubMed]
- Bacci, G.; Briccoli, A.; Rocca, M.; Ferrari, S.; Donati, D.; Longhi, A.; Bertoni, F.; Bacchini, P.; Giacomini, S.; Forni, C.; et al. Neoadjuvant chemotherapy for osteosarcoma of the extremities with metastases at presentation: Recent experience at the Rizzoli Institute in 57 patients treated with cisplatin, doxorubicin, and a high dose of methotrexate and ifosfamide. Ann. Oncol. 2003, 14, 1126–1134. [Google Scholar] [CrossRef] [PubMed]
- Holscher, H.C.; Bloem, J.L.; Vanel, D.; Hermans, J.; Nooy, M.A.; Taminiau, A.H.; Henry-Amar, M. Osteosarcoma: Chemotherapy-induced changes at MR imaging. Radiology 1992, 182, 839–844. [Google Scholar] [CrossRef] [PubMed]
- Kanthawang, T.; Wudhikulprapan, W.; Phinyo, P.; Settakorn, J.; Pruksakorn, D.; Link, T.M.; Pattamapaspong, N. Can conventional magnetic resonance imaging at presentation predict chemoresistance in osteosarcoma? Br. J. Radiol. 2024, 97, 451–461. [Google Scholar] [CrossRef] [PubMed]
- Cuenod, C.A.; Balvay, D. Perfusion and vascular permeability: Basic concepts and measurement in DCE-CT and DCE-MRI. Diagn. Interv. Imaging 2013, 94, 1187–1204. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Reddick, W.E.; Glass, J.O.; Ji, Q.; Billups, C.A.; Wu, J.; Hoffer, F.A.; Kaste, S.C.; Jenkins, J.J.; Ortega Flores, X.C.; et al. Dynamic contrast-enhanced magnetic resonance imaging as a prognostic factor in predicting event-free and overall survival in pediatric patients with osteosarcoma. Cancer 2012, 118, 3776–3785. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hao, Y.; An, R.; Xue, Y.; Li, F.; Wang, H.; Zheng, J.; Fan, L.; Liu, J.; Fan, H.; Yin, H. Prognostic value of tumoral and peritumoral magnetic resonance parameters in osteosarcoma patients for monitoring chemotherapy response. Eur. Radiol. 2021, 31, 3518–3529. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wahl, R.L.; Jacene, H.; Kasamon, Y.; Lodge, M.A. From RECIST to PERCIST: Evolving Considerations for PET response criteria in solid tumors. J. Nucl. Med. 2009, 50 (Suppl. S1), 122S–150S. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Davis, J.C.; Daw, N.C.; Navid, F.; Billups, C.A.; Wu, J.; Bahrami, A.; Jenkins, J.J.; Snyder, S.E.; Reddick, W.E.; Santana, V.M.; et al. 18F-FDG Uptake During Early Adjuvant Chemotherapy Predicts Histologic Response in Pediatric and Young Adult Patients with Osteosarcoma. J. Nucl. Med. 2018, 59, 25–30. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Palmerini, E.; Colangeli, M.; Nanni, C.; Fanti, S.; Marchesi, E.; Paioli, A.; Picci, P.; Cambioli, S.; Donati, D.; Cevolani, L.; et al. The role of FDG PET/CT in patients treated with neoadjuvant chemotherapy for localized bone sarcomas. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 215–223. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Li, Y.; Xie, L.; Sun, X.; Cai, Z.; Wang, S.; Wang, Q.; Sun, K.; Guo, W. An evaluation of the response to neoadjuvant chemotherapy for osteosarcoma of extremities: PERCIST versus RECIST 1.1 criteria after long-term follow-up. Ann. Nucl. Med. 2022, 36, 553–561, Erratum in Ann. Nucl. Med. 2022, 36, 785. [Google Scholar] [CrossRef] [PubMed]
- Gillies, R.J.; Anderson, A.R.; Gatenby, R.A.; Morse, D.L. The biology underlying molecular imaging in oncology: From genome to anatome and back again. Clin. Radiol. 2010, 65, 517–521. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lambin, P.; Leijenaar, R.T.H.; Deist, T.M.; Peerlings, J.; de Jong, E.E.C.; van Timmeren, J.; Sanduleanu, S.; Larue, R.T.H.M.; Even, A.J.G.; Jochems, A.; et al. Radiomics: The bridge between medical imaging and personalized medicine. Nat. Rev. Clin. Oncol. 2017, 14, 749–762. [Google Scholar] [CrossRef] [PubMed]
- Nakaura, T.; Higaki, T.; Awai, K.; Ikeda, O.; Yamashita, Y. A primer for understanding radiology articles about machine learning and deep learning. Diagn. Interv. Imaging 2020, 101, 765–770. [Google Scholar] [CrossRef] [PubMed]
- Tao, J.; Liang, C.; Yin, K.; Fang, J.; Chen, B.; Wang, Z.; Lan, X.; Zhang, J. 3D convolutional neural network model from contrast-enhanced CT to predict spread through air spaces in non-small cell lung cancer. Diagn. Interv. Imaging 2022, 103, 535–544. [Google Scholar] [CrossRef] [PubMed]
- Ronot, M.; Soyer, P. Can radiomics outperform pathology for tumor grading? Diagn. Interv. Imaging 2024, 105, 3–4. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Zhang, C.; Hu, Y.; Zhang, J.; Liu, Y.; Si, L.; Xing, Y.; Ding, D.; Geng, J.; Jiao, Q.; et al. Automated prediction of the neoadjuvant chemotherapy response in osteosarcoma with deep learning and an MRI-based radiomics nomogram. Eur. Radiol. 2022, 32, 6196–6206. [Google Scholar] [CrossRef] [PubMed]
- Zheng, F.; Yin, P.; Liang, K.; Wang, Y.; Hao, W.; Hao, Q.; Hong, N. Fusion Radiomics-Based Prediction of Response to Neoadjuvant Chemotherapy for Osteosarcoma. Acad. Radiol. 2024, 31, 2444–2455. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Hu, Y.; Si, L.; Jia, G.; Xing, Y.; Zhang, H.; Yao, W. A systematic review of radiomics in osteosarcoma: Utilizing radiomics quality score as a tool promoting clinical translation. Eur. Radiol. 2021, 31, 1526–1535. [Google Scholar] [CrossRef] [PubMed]
- Bouhamama, A.; Leporq, B.; Khaled, W.; Nemeth, A.; Brahmi, M.; Dufau, J.; Marec-Bérard, P.; Drapé, J.L.; Gouin, F.; Bertrand-Vasseur, A.; et al. Prediction of Histologic Neoadjuvant Chemotherapy Response in Osteosarcoma Using Pretherapeutic MRI Radiomics. Radiol. Imaging Cancer 2022, 4, e210107. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- White, L.M.; Atinga, A.; Naraghi, A.M.; Lajkosz, K.; Wunder, J.S.; Ferguson, P.; Tsoi, K.; Griffin, A.; Haider, M. T2-weighted MRI radiomics in high-grade intramedullary osteosarcoma: Predictive accuracy in assessing histologic response to chemotherapy, overall survival, and disease-free survival. Skelet. Radiol. 2023, 52, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.; Yang, P.F.; Chen, S.; Shao, Y.Y.; Xu, L.; Wu, Y.; Teng, W.; Zhou, X.Z.; Li, B.H.; Luo, C.; et al. A Delta-radiomics model for preoperative evaluation of Neoadjuvant chemotherapy response in high-grade osteosarcoma. Cancer Imaging 2020, 20, 7. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, Y.; Zhi, L.; Li, J.; Wang, M.; Chen, G.; Yin, S. Magnetic Resonance Imaging Radiomics Predicts Histological Response to Neoadjuvant Chemotherapy in Localized High-grade Osteosarcoma of the Extremities. Acad. Radiol. 2024; Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Loi, S.; Sirtaine, N.; Piette, F.; Salgado, R.; Viale, G.; Van Eenoo, F.; Rouas, G.; Francis, P.; Crown, J.P.; Hitre, E.; et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. J. Clin. Oncol. 2013, 31, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Bramer, J.A.; van Linge, J.H.; Grimer, R.J.; Scholten, R.J. Prognostic factors in localized extremity osteosarcoma: A systematic review. Eur. J. Surg. Oncol. 2009, 35, 1030–1036. [Google Scholar] [CrossRef] [PubMed]
- Thuss-Patience, P.C.; Kretzschmar, A.; Bichev, D.; Deist, T.; Hinke, A.; Breithaupt, K.; Dogan, Y.; Gebauer, B.; Schumacher, G.; Reichardt, P. Survival advantage for irinotecan versus best supportive care as second-line chemotherapy in gastric cancer—A randomised phase III study of the Arbeitsgemeinschaft Internistische Onkologie (AIO). Eur. J. Cancer 2011, 47, 2306–2314. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wu, L.; Li, B.; Cheng, Y.; Li, X.; Wang, X.; Han, L.; Wu, X.; Fan, Y.; Yu, Y.; et al. Toripalimab Plus Chemotherapy for Patients with Treatment-Naive Advanced Non-Small-Cell Lung Cancer: A Multicenter Randomized Phase III Trial (CHOICE-01). J. Clin. Oncol. 2023, 41, 651–663. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kelley, L.M.; Schlegel, M.; Hecker-Nolting, S.; Kevric, M.; Haller, B.; Rössig, C.; Reichardt, P.; Kager, L.; Kühne, T.; Gosheger, G.; et al. Pathological Fracture and Prognosis of High-Grade Osteosarcoma of the Extremities: An Analysis of 2847 Consecutive Cooperative Osteosarcoma Study Group (COSS) Patients. J. Clin. Oncol. 2020, 38, 823–833. [Google Scholar] [CrossRef] [PubMed]
- Tomer, G.; Cohen, I.J.; Kidron, D.; Katz, K.; Yosipovitch, Z.; Meller, I.; Zaizov, R. Prognostic factors in non-metastatic limb osteosarcoma: A 20-year experience of one center. Int. J. Oncol. 1999, 15, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Lan, T.; Cai, H.; Lu, A.; Yu, W. Meta-analysis of serum lactate dehydrogenase and prognosis for osteosarcoma. Medicine 2018, 97, e0741. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- van Trommel, M.F.; Kroon, H.M.; Bloem, J.L.; Hogendoorn, P.C.; Taminiau, A.H. MR imaging based strategies in limb salvage surgery for osteosarcoma of the distal femur. Skelet. Radiol. 1997, 26, 636–641. [Google Scholar] [CrossRef] [PubMed]
- Bodden, J.; Neumann, J.; Rasper, M.; Fingerle, A.A.; Knebel, C.; von Eisenhart-Rothe, R.; Specht, K.; Mogler, C.; Bollwein, C.; Schwaiger, B.J.; et al. Diagnosis of joint invasion in patients with malignant bone tumors: Value and reproducibility of direct and indirect signs on MR imaging. Eur. Radiol. 2022, 32, 4738–4748. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kalisvaart, G.M.; Evenhuis, R.E.; Grootjans, W.; Van Den Berghe, T.; Callens, M.; Bovée, J.V.M.G.; Creytens, D.; Gelderblom, H.; Speetjens, F.M.; Lapeire, L.; et al. Relative Wash-In Rate in Dynamic Contrast-Enhanced Magnetic Resonance Imaging as a New Prognostic Biomarker for Event-Free Survival in 82 Patients with Osteosarcoma: A Multicenter Study. Cancers 2024, 16, 1954. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hawkins, D.S.; Conrad EU 3rd Butrynski, J.E.; Schuetze, S.M.; Eary, J.F. [F-18]-fluorodeoxy-D-glucose-positron emission tomography response is associated with outcome for extremity osteosarcoma in children and young adults. Cancer 2009, 115, 3519–3525. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Costelloe, C.M.; Macapinlac, H.A.; Madewell, J.E.; Fitzgerald, N.E.; Mawlawi, O.R.; Rohren, E.M.; Raymond, A.K.; Lewis, V.O.; Anderson, P.M.; Bassett, R.L., Jr.; et al. 18F-FDG PET/CT as an indicator of progression-free and overall survival in osteosarcoma. J. Nucl. Med. 2009, 50, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Im, H.J.; Zhang, Y.; Wu, H.; Wu, J.; Daw, N.C.; Navid, F.; Shulkin, B.L.; Cho, S.Y. Prognostic Value of Metabolic and Volumetric Parameters of FDG PET in Pediatric Osteosarcoma: A Hypothesis-generating Study. Radiology 2018, 287, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Su, Y.; Duan, J.; Qiu, Q.; Ge, X.; Wang, A.; Yin, Y. Radiomics signature extracted from diffusion-weighted magnetic resonance imaging predicts outcomes in osteosarcoma. J. Bone Oncol. 2019, 19, 100263. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, H.; Liu, J.; Cheng, Z.; Lu, X.; Wang, X.; Lu, M.; Li, S.; Xiang, Z.; Zhou, Q.; Liu, Z.; et al. Development and external validation of an MRI-based radiomics nomogram for pretreatment prediction for early relapse in osteosarcoma: A retrospective multicenter study. Eur. J. Radiol. 2020, 129, 109066. [Google Scholar] [CrossRef] [PubMed]










| Osteosarcoma Subtype | Frequency | Age and Sex Prevalence | Skeletal Regions Most Frequently Involved |
|---|---|---|---|
| Conventional high-grade osteosarcoma 1 | 75–80% | 10–20 years old; M:F = 1.5:1 | Distal femoral bone, proximal tibia, or humerus (70%) |
| Telangiectatic 1 | 2–12% | 10–20 years old; M:F = 1.5:1 | Around knee or shoulder joint (70%) |
| Secondary 1 | 4% | 50–80 years old; M:F = 1.5:1 | Around knee or hip joint |
| High grade of bone surface 1 | 1–2% | 10–40 years old; M:F = 1.5:1 | Tibia and femur (both near knee and in diaphysis) |
| Small cell 1 | 1% | 5–25 years old; M:F = 1:1.5 | Around knee joint |
| Extraskeletal 1,* | 2–5% | 50–80 years old; M:F = 1:1.5 | Thigh (soft tissue) |
| Parosteal 2 | <4% | 10–45 years old; M:F = 1:1.5 | Around knee joint (in 60% of cases, posterior aspect of distal femur) |
| Central low-grade 2 | 2–3% | 10–50 years old; M:F = 1:1 | Around knee joint |
| Periosteal 2 | >1% | 10–20 years old; M:F = 1.5:1 | Tibia and femur (both near knee and in diaphysis) |
| Osteosarcoma Subtype | Radiologic Pattern | Periosteal Reaction | Other Imaging Features |
|---|---|---|---|
| Conventional osteosarcoma | Mixed (lytic and sclerotic) or completely eburneous | Sunburst, Codman triangle, other irregular/aggressive types | Soft-tissue components frequently displayed |
| Telangiectatic | Purely osteolytic | None or thin regular | Multicystic pattern with fluid–fluid levels and solid components on MRI |
| Secondary | Lytic heterogeneous | Aggressive types | Different depending on pre-existing lesions |
| High-grade of bone surface | Mixed mineralized and non-mineralized soft-tissue components without cleavage with bone cortex | Uncommon | Cortex erosion (50%), intramedullary involvement (50%) |
| Small cell | Usually similar to classic osteosarcoma | Usually similar to classic osteosarcoma | Usually similar to classic osteosarcoma |
| ESOS | Soft-tissue mass with inhomogeneous contrast enhancement, various degrees of internal necrosis | None | Internal mineralization frequently displayed (60%) |
| Parosteal | Lobulated osseous mass fused with cortical bone, usually with large dimensions, broad implant base | None, non-aggressive ones, or only cortical thickening | Cauliflower-like mass, thin linear cleavage between portions of tumor and cortical bone, frequent intramedullary involvement |
| Central low grade | Lytic, eburneous, or mixed, usually with large dimensions | If present, regular/non-aggressive | Soft-tissue mass (50%) |
| Periosteal | Periosteal dense mass with well-defined borders | None or sometimes Codman triangle | Cortex may be intact or focally eroded, but bone canal is not involved |
| Metastases at Diagnosis | Lung Involvement | Bone Involvement |
|---|---|---|
| 15–20% | 80% | 10–30% |
| 60% calcified or ossified | 10–25% skip metastases, while locations in other bones are rarer | |
| 40% non-calcified |
| Imaging Feature | Clinical Significance |
|---|---|
| - Large tumor size and volume (longest diameter > 7–10 cm, volume > 150 mL, volume >1/3 of involved bone) - Increased tumor volume and diameter during NACT | - Lower response rate to NACT - Decreased OS and EFS |
| - Intra-articular tumor spreading | - Difficult to perform limb-sparing surgery - Increased risk of local recurrence - Decreased OS |
| - Proximity to major blood vessels | - Difficult to perform limb-sparing surgery - Increased risk of local recurrence - Decreased OS |
| - Location in difficult sites for surgery (axial skeleton, girdles, skull base, proximal humerus, or femur) | - Impossibility of surgery or difficulty in removing whole tumor - Decreased OS and EFS |
| - Occurrence of pathological fracture | - Tumor spread outside of bone and/or hematic spread - Decreased OS and increased risk of local recurrence (debated) |
| - Presence of distant metastases | - Decreased OS |
| - MRI signal of internal hemorrhagic areas * | - Decreased OS |
| - MRI signal intensity inhomogeneity (T2-WI) * | - Decreased OS |
| - Necrotic area > 50% of tumor volume | - Lower response rate |
| - Peritumoral soft tissue edema - No decrease in peritumoral edema during NACT | - Lower response rate to NACT |
| Modality, Sequence | Quantitative Imaging Data | Clinical Significance |
|---|---|---|
| DCE-MRI | Lower Ktrans and Vp, change in Kep between inner and outer tumor areas at intermediate evaluation | Good histologic response |
| Lower Ktrans measured inside tumor after NACT | Good histologic response | |
| Decrease in Ktrans from baseline to pre-surgical MRI | Good histologic response | |
| Relative wash-in rate ratio (rWIR) < 2.3 (poor radiological response) | Poor histologic response | |
| Difference between outer and inner values of Ve at baseline | Lower EFS | |
| Lower baseline peritumoral Ve (cut-off = 0.2485) and lower post-chemotherapy intra-tumoral Ktrans (cut-off = 0.2275) | Longer EFS and OS | |
| Lower intra-tumoral Ktrans at baseline and after chemotherapy | Longer OS | |
| DWI | - Mean ADC difference before and after NACT - ADC ratio significantly higher in good responders compared to poor responders | Higher decrease in good histologic responders |
| - Peritumoral ADC measured in peritumoral area after NACT - Changes in peritumoral ADC from baseline to end of NACT | Higher decrease in good histologic responders | |
| Higher post-chemotherapy peritumoral ADC | Longer OS | |
| 18F-FDG PET/CT | Low baseline SUVmax (cut-off = 6) | Good histologic response |
| High baseline SUVmax (cut-off = 15) | Lower EFS and PFS | |
| Low post-chemotherapy SUVmax (cut-off = 2–3) | Good histologic response | |
| High post-chemotherapy SUVmax (cut-off = 2.5–5) | Lower EFS and PFS | |
| TBR > 0.46–0.60 | Good histologic response | |
| Decrease in SUVmax between baseline and post-cNACT ≥ 52–60% | Good histologic response | |
| PERCIST criteria | Good histologic response | |
| High baseline MTV (cut-off = 238), | Lower EFS, PFS, and OS | |
| Higher baseline TLG (cut-off = 1022), | Lower OS | |
| Low TLG change (cut-off = 10%) | Lower EFS and PFS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crombé, A.; Simonetti, M.; Longhi, A.; Hauger, O.; Fadli, D.; Spinnato, P. Imaging of Osteosarcoma: Presenting Findings, Metastatic Patterns, and Features Related to Prognosis. J. Clin. Med. 2024, 13, 5710. https://doi.org/10.3390/jcm13195710
Crombé A, Simonetti M, Longhi A, Hauger O, Fadli D, Spinnato P. Imaging of Osteosarcoma: Presenting Findings, Metastatic Patterns, and Features Related to Prognosis. Journal of Clinical Medicine. 2024; 13(19):5710. https://doi.org/10.3390/jcm13195710
Chicago/Turabian StyleCrombé, Amandine, Mario Simonetti, Alessandra Longhi, Olivier Hauger, David Fadli, and Paolo Spinnato. 2024. "Imaging of Osteosarcoma: Presenting Findings, Metastatic Patterns, and Features Related to Prognosis" Journal of Clinical Medicine 13, no. 19: 5710. https://doi.org/10.3390/jcm13195710







