Synthesis, Characterization and Biological Evaluation of Novel Benzamidine Derivatives: Newer Antibiotics for Periodontitis Treatment
Abstract
:1. Introduction
2. Results and Discussion
2.1. Chemistry
2.2. Biological Activity
2.2.1. In Vitro Antibacterial Activity of Synthesized Compounds
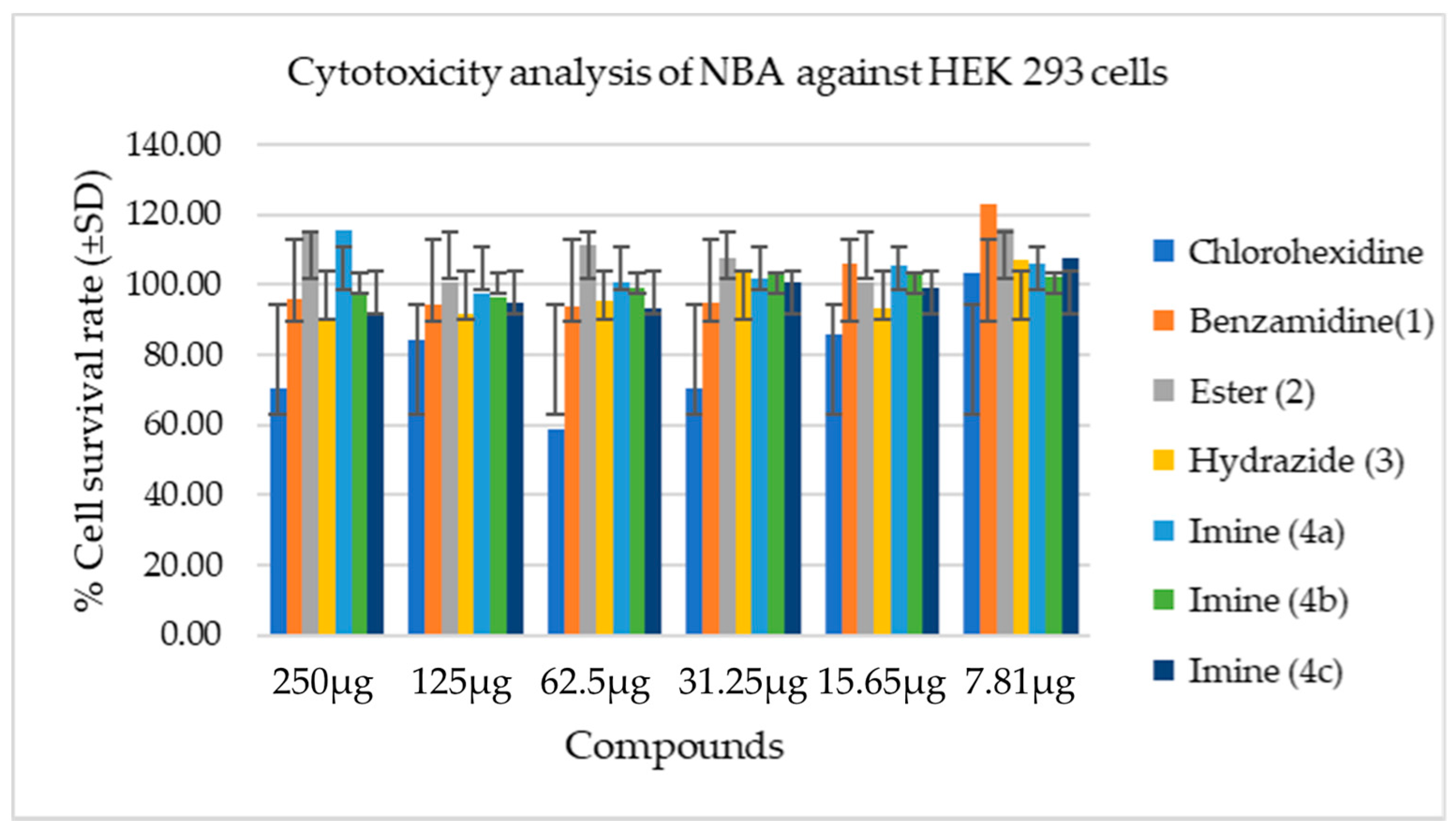
2.2.2. Cytotoxicity Analysis of Synthesized Compounds
3. Materials and Methods
3.1. General Information
3.2. Synthesis
3.2.1. Synthesis of Ethyl 2-(4-Carbamimidoylphenoxyacetate (2)
3.2.2. Synthesis of 2-(4-Carbamimidoylphenoxy) Acetohydrazide (3)
3.2.3. General Synthesis Procedure for the of N′-(Substituted Benzylidene)-2-(4-(N-(4-Hydroxybenzylidene)carbamimidoyl)phenoxy)acetohydrazide (4a–c)
3.3. Determination of Antimicrobial Activity
3.3.1. General Information
3.3.2. Cell Viability Assay
3.3.3. Cell Counting
3.3.4. Cell Treatment
3.3.5. 3-[4,5-Dimethylthiazol-2-yl]2,5-diphenyl Tetrazolium Bromide (MTT) Assay
3.3.6. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bendek, M.J.; Canedo-Marroquín, G.; Realini, O.; Retamal, I.N.; Hernández, M.; Hoare, A.; Busso, D.; Monteiro, L.J.; Illanes, S.E.; Chaparro, A. Periodontitis and gestational diabetes mellitus: A potential inflammatory vicious cycle. Int. J. Mol. Sci. 2021, 22, 11831. [Google Scholar] [CrossRef]
- Chen, M.X.; Zhong, Y.J.; Dong, Q.Q.; Wong, H.M.; Wen, Y.F. Global, regional, and national burden of severe periodontitis, 1990–2019: An analysis of the Global burden of disease study 2019. J. Clin. Periodontol. 2021, 48, 1165–1188. [Google Scholar] [CrossRef] [PubMed]
- How, K.Y.; Song, K.P.; Chan, K.G. Porphyromonas gingivalis: An overview of periodontopathic pathogen below the gum line. Front. Microbiol. 2016, 7, 53. [Google Scholar] [CrossRef] [PubMed]
- Dewhirst, F.E.; Chen, T.; Izard, J.; Paster, B.J.; Tanner, A.C.; Yu, W.H.; Lakshmanan, A.; Wade, W.G. The human oral microbiome. J. Bacteriol. 2010, 19, 5002–5017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olsen, I.; Potempa, J. Strategies for the inhibition of gingipains for the potential treatment of periodontitis and associated systemic diseases. J. Oral Microbiol. 2014, 6, 24800. [Google Scholar] [CrossRef] [Green Version]
- Barca, E.; Cifcibasi, E.; Cintan, S. Adjunctive use of antibiotics in periodontal therapy. J. Istanbul Univ. Fac. Dent. 2015, 49, 55–62. [Google Scholar] [CrossRef]
- Malki, F.; Touati, A.; Moulay, S.; Baltas, M. Antioxidant and antimicrobial activities of two amidine derivatives. Mediterr. J. Biosci. 2016, 1, 62–68. [Google Scholar]
- Chukkapalli, S.S.; Rivera, M.F.; Velsko, I.M.; Lee, J.Y.; Chen, H.; Zheng, D.; Bhattacharyya, I.; Gangula, P.R.; Lucas, A.R.; Kesavalu, L. Invasion of oral and aortic tissues by oral spirochete Treponema denticola in ApoE (-/-) mice causally links periodontal disease and atherosclerosis. Infect. Immun. 2014, 82, 1959–1967. [Google Scholar] [CrossRef] [Green Version]
- Onyeyilim, E.L.; Ezeokonkwo, M.A.; Ugwu, D.I.; Uzoewulu, C.P.; Eze, F.U.; Okonkwo, V.I.; Eze, C.C.; Ezugwu, J.A. Carbohydrazide analogues: A review of synthesis and biological activities. Mini Rev. Med. Chem. 2021, 21, 1. [Google Scholar] [CrossRef]
- Desale, V.J.; Mali, S.N.; Thorat, B.R.; Yamgar, R.S. Synthesis, admetSAR Predictions, DPPH Radical Scavenging Activity, Potent Anti-mycobacterial Studies of Hydrazones of Substituted 4-(anilino methyl) benzohydrazides (Part 2). Curr. Comput. Aided Drug Des. 2021, 17, 493–503. [Google Scholar] [CrossRef]
- Vaseghi, S.; Yousefi, M.; Shokrzadeh, M.; Hossaini, Z.; Hosseini-Khah, Z.; Emami, S. Synthesis, computational study cytotoxicity of 4-hydroxycoumarin-derived imines/enamines. Mol. Divers. 2021, 25, 1011–1024. [Google Scholar] [CrossRef]
- Cleiton, M.d.S.; Daniel, L.d.S.; Luzia, V.M.; Rosemeire, B.A.; Maria, A.d.R.; Cleide, V.B.M.; Ângelo, d.F. Schiff bases: A short review of their antimicrobial activities. J. Adv. Res. 2011, 2, 1–8. [Google Scholar]
- Rezki, N.; Al-Yahyawi, A.M.; Bardaweel, S.K.; Al-Blewi, F.F.; Aouad, M.R. Synthesis of novel 2,5- disubstituted-1,3,4-thiadiazoles clubbed 1,2,4-triazole, 1,3,4-thiadiazole, 1,3,4-oxadiazole and/or schiff base as potential antimicrobial and antiproliferative agents. Molecules 2015, 20, 16048–16067. [Google Scholar] [CrossRef] [Green Version]
- Yunnikova, L.P.; Akent’eva, T.A.; Aleksandrova, G.A. Synthesis and antimicrobial activity of amines and imines with a cycloheptatriene fragment. Pharm. Chem. J. 2013, 46, 723–725. [Google Scholar] [CrossRef]
- Silva, R.H.N.; Andrade, A.C.M.; Nóbrega, D.F.; de Castro, R.D.; Pessôa, H.L.F.; Rani, N.; de Sousa, D.P. Antimicrobial activity of 4-chlorocinnamic acid derivatives. Biomed. Res. Int. 2019, 2019, 3941242. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.J.; Kim, H.K. Antioxidant and antibacterial activity of caprylic acid vanillyl ester produced by lipase-mediated transesterification. J. Microbiol. Biotechnol. 2021, 31, 317–326. [Google Scholar] [CrossRef]
- Soares, V.; Marini, M.B.; de Paula, L.A.; Gabry, P.S.; Amaral, A.; Malafaia, C.A.; Leal, I.C.R. Umbelliferone esters with antibacterial activity produced by lipase-mediated biocatalytic pathway. Biotechnol. Lett. 2021, 43, 469–477. [Google Scholar] [CrossRef]
- La Piana, L.; Viaggi, V.; Principe, L.; Di Bella, S.; Luzzaro, F.; Viale, M.; Bertola, N.; Vecchio, G. Polypyridine ligands as potential metallo-β-lactamase inhibitors. J. Inorg. Biochem. 2021, 215, 111315. [Google Scholar] [CrossRef] [PubMed]
- Popiołek, Ł. Updated information on antimicrobial activity of hydrazide-hydrazones. Int. J. Mol. Sci. 2021, 22, 9389. [Google Scholar] [CrossRef]
- Popiołek, Ł.; Biernasiuk, A. Synthesis and investigation of antimicrobial activities of nitrofurazone analogues containing hydrazide-hydrazone moiety. Saudi Pharm. J. 2017, 25, 1097–1102. [Google Scholar] [CrossRef]
- Kowalewska, M.; Kwiecień, H.; Śmist, M.; Wrześniewska, A. Synthesis of new benzofuran-2-carboxylic acid derivatives. J. Chem. 2013, 2013, 183717. [Google Scholar] [CrossRef] [Green Version]
- Mohamed, S. Antimicrobial activities of some synthesized pyridines, oxazines and thiazoles from 3-aryl-1-(2-naphthyl)prop-2-en-1-ones. Sci. Pharm. 2008, 76, 279–303. [Google Scholar] [CrossRef] [Green Version]
- Ravotti, R.O.; Fellmann, N.; Lardon, L.; Fischer, A.; Stamatiou, A.; Worlitschek, J. Synthesis and investigation of thermal properties of highly pure carboxylic fatty esters to be used as PCM. Appl. Sci. 2018, 8, 1069. [Google Scholar] [CrossRef] [Green Version]
- Al-Ajely, M.S.; Yaseen, A.N. Synthesis and characterization of some new hydrazides and their derivatives. Molecules 2015, 28, 10. [Google Scholar]
- Husain, A.; Varshney, M.M.; Parcha, V.; Ahmad, A.; Khan, S.A. Synthesis and biological evaluation of new hydrazide-Schiff bases. Bangladesh J. Pharmacol. 2015, 10, 555. [Google Scholar] [CrossRef] [Green Version]
- Hussain, Z.; Yousif, E.; Ahmed, A.; Altaie, A. Synthesis and characterization of Schiff’s bases of sulfamethoxazole. Org. Med. Chem. Lett. 2014, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Sakko, M.; Rautemaa-Richardson, R.; Sakko, S.; Richardson, M.; Sorsa, T. Antibacterial activity of 2-hydroxyisocaproic acid (HICA) against obligate anaerobic bacterial species associated with periodontal disease. Microbiol. Insights 2021, 14, 50086. [Google Scholar] [CrossRef]
- Fakheran, O.; Khademi, A.; Bagherniya, M.; Dehghannejad, M.; Sathyapalan, T.; Sahebkar, A. Antibacterial activity of curcumin against periodontal pathogens: A systematic review. Adv. Exp. Med. Biol. 2021, 1291, 239–249. [Google Scholar]
- Wang, J.; Gu, D. Determination of antimicrobial resistance of salmonella in pork. Methods Mol. Biol. 2021, 2182, 179–186. [Google Scholar]
- Snoch, W.; Stępień, K.; Prajsnar, J.; Staroń, J.; Szaleniec, M.; Guzik, M. Influence of chemical modifications of polyhydroxyalkanoate-derived fatty acids on their antimicrobial properties. Catalysts 2019, 9, 510. [Google Scholar] [CrossRef] [Green Version]
- Fischer, C.L.; Walters, K.S.; Drake, D.R.; Dawson, D.V.; Blanchette, D.R.; Brogden, K.A.; Wertz, P.W. Oral mucosal lipids are antibacterial against Porphyromonas gingivalis, induce ultrastructural damage, and alter bacterial lipid and protein compositions. Int. J. Oral Sci. 2013, 5, 130–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdel-Rahman, A.A.H.; El-Sayed, W.A.; Abdel-Bary, H.M.; Abdel-Megied, A.E.S.; Morcy, E.M.I. Amino acid derivatives, VIII [1]: Synthesis and antimicrobial evaluation of α-amino acid esters bearing an indole side chain. Mon. Chem. 2008, 139, 1095–1101. [Google Scholar] [CrossRef]
- Ahluwalia, V.V.; Kumar, J.; Rana, V.S.; Singh, R.; Sati, O.P.; Walia, S. Synthesis and antimicrobial activity of esters of 3-ethoxy-4-hydroxybenzaldehyde oxime. Toxicol. Environ. Chem. 2017, 99, 1–9. [Google Scholar] [CrossRef]
- Lubenets, V.; Vasylyuk, S.; Monka, N.; Bolibrukh, K.; Komarovska-Porokhnyavets, O.; Baranovych, D.; Musyanovych, R.; Zaczynska, E.; Czarny, A.; Nawrot, U.; et al. Synthesis and antimicrobial properties of 4-acylaminobenzenethiosulfoacid S-esters. Saudi Pharm. J. 2017, 25, 266–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Popiołek, Ł.; Biernasiuk, A. Design, synthesis, and in vitro antimicrobial activity of hydrazide-hydrazones of 2-substituted acetic acid. Chem. Biol. Drug Des. 2016, 88, 873–883. [Google Scholar] [CrossRef] [PubMed]
- Rasras, A.J.M.; Al-Tel, T.H.; Al-Aboudi, A.F.; Al-Qawasmeh, R.A. Synthesis and antimicrobial activity of cholic acid hydrazone analogues. Eur. J. Med. Chem. 2010, 45, 2307–2313. [Google Scholar] [CrossRef]
- Rollas, S.; Güniz Küçükgüzel, Ş. Biological activities of hydrazone derivatives. Molecules 2007, 12, 1910–1939. [Google Scholar] [CrossRef] [Green Version]
- Shirinzadeh, H.; Altanlar, N.; Yucel, N.; Ozden, S.; Suzen, S. Antimicrobial evaluation of indole-containing hydrazone derivatives. Z. Nat. C 2011, 66, 340–344. [Google Scholar] [CrossRef]
- Nayak, S.G.; Poojary, B. Synthesis of novel Schiff bases containing arylpyrimidines as promising antibacterial agents. Heliyon 2019, 5, 8. [Google Scholar] [CrossRef] [Green Version]
- Akbari Dilmaghani, K.; Nasuhi Pur, F.; Hatami Nezhad, M. Synthesis and antibacterial evaluation of new thione substituted 1,2,4-triazole schiff bases as novel antimicrobial agents. Iran. J. Pharm. Res. 2015, 14, 693–699. [Google Scholar]
- Fonkui, T.Y.; Ikhile, M.I.; Njobeh, P.B.; Ndinteh, D.T. Benzimidazole Schiff base derivatives: Synthesis, characterization and antimicrobial activity. BMC Chem. 2019, 13, 127. [Google Scholar] [CrossRef] [PubMed]
- Sabaa, M.W.; Elzanaty, A.M.; Abdel-Gawad, O.F.; Arafa, E.G. Synthesis, characterization and antimicrobial activity of Schiff bases modified chitosan-graft-poly(acrylonitrile). Int. J. Biol. Macromol. 2018, 109, 1280–1291. [Google Scholar] [CrossRef]
- Bali, E.B.; Açık, L.; Akca, G.; Sarper, M.; Elçi, M.P.; Avcu, F.; Vural, M. Antimicrobial activity against periodontopathogenic bacteria, antioxidant and cytotoxic effects of various extracts from endemic Thermopsis turcica. Asian Pac. J. Trop. Biomed. 2014, 4, 505–514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohieldin, E.A.M.; Muddathir, A.M.; Mitsunaga, T. Inhibitory activities of selected Sudanese medicinal plants on Porphyromonas gingivalis and matrix metalloproteinase-9 and isolation of bioactive compounds from Combretum hartmannianum (Schweinf) bark. BMC Complement. Altern. Med. 2017, 17, 224. [Google Scholar] [CrossRef] [PubMed]
- Tsou, S.H.; Hu, S.W.; Yang, J.J.; Yan, M.; Lin, Y.Y. Potential oral health care agent from coffee against virulence factor of periodontitis. Nutrients 2019, 11, 2235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ronayne, C.T.; Solano, L.N.; Nelson, G.L.; Lueth, E.A.; Hubbard, S.L.; Schumacher, T.J.; Gardner, Z.S.; Jonnalagadda, S.K.; Gurrapu, S.; Holy, J.; et al. Synthesis and biological evaluation of 2-alkoxycarbonylallyl esters as potential anticancer agents. Bioorg. Med. Chem. Lett. 2017, 27, 776–780. [Google Scholar] [CrossRef]
- Mossoba, M.E.; Mapa, M.S.T.; Araujo, M.; Zhao, Y.; Flannery, B.; Flynn, T.; Sprando, J.; Wiesenfeld, P.; Sprando, R.L. In vitro toxicological assessment of free 3-MCPD and select 3-MCPD esters on human proximal tubule HK-2 cells. Cell Biol. Toxicol. 2019, 36, 209–221. [Google Scholar] [CrossRef]
- Asif, M.; Husain, A. Analgesic, anti-inflammatory, and antiplatelet profile of hydrazones containing synthetic molecules. J. Appl. Chem. 2013, 2013, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Grande, F.; Yamada, R.; Cao, X.; Aiello, F.; Garofalo, A.; Neamati, N. Synthesis and biological evaluation of novel hydrazide based cytotoxic agents. Expert Opin. Investig. Drugs 2009, 18, 555–568. [Google Scholar] [CrossRef]
- Jabeen, M.; Ahmad, S.; Shahid, K.; Sadiq, A.; Rashid, U. Ursolic acid hydrazide based organometallic complexes: Synthesis, characterization, antibacterial, antioxidant, and docking studies. Front. Chem. 2018, 6, 55. [Google Scholar] [CrossRef]
- Popiołek, Ł.; Piątkowska-Chmiel, I.; Gawrońska-Grzywacz, M.; Biernasiuk, A.; Izdebska, M.; Herbet, M.; Sysa, M.; Malm, A.; Dudka, J.; Wujec, M. New hydrazide-hydrazones and 1,3-thiazolidin-4-ones with 3-hydroxy-2-naphthoic moiety: Synthesis, in vitro and in vivo studies. Biomed. Pharmacother. 2018, 103, 1337–1347. [Google Scholar] [CrossRef]
- Yusof, E.N.M.; Latif, M.A.M.; Tahir, M.I.M.; Sakoff, J.A.; Simone, M.I.; Page, A.J.; Veerakumarasivam, A.; Tiekink, E.R.T.; Ravoof, T.B.S.A. O-vanillin derived schiff bases and their organotin (IV) compounds: Synthesis, structural characterisation, in-silico studies and cytotoxicity. Int. J. Mol. Sci. 2019, 20, 854. [Google Scholar] [CrossRef] [Green Version]
- Hamed, A.A.; Abdelhamid, I.A.; Saad, G.R.; Elkady, N.A.; Elsabee, M.Z. Synthesis, characterization and antimicrobial activity of a novel chitosan Schiff bases based on heterocyclic moieties. Int. J. Biol. Macromol. 2020, 15, 492–501. [Google Scholar] [CrossRef] [PubMed]
- Burak, A.k.; Özeroglu, E.; Taspinar, M. The use of methylene blue as mouthwash in periodontology. East J. Med. 2015, 7, 215–221. [Google Scholar]
- Samanth, D.S.A.; Varghese, D.S.S. The most effective concentration of chlorhexidine as a mouthwash—Systematic review. J. Pharm. Sci. 2017, 9, 4. [Google Scholar]
- Fuloria, S.; Fuloria, N.K.; Sundram, K.; Kathiresan, S.; Saurabh, S.; Khushboo, G.; Ajay, J.; Ugrappa, S.; Malipeddi, H.; Shiva, S. Synthesis and discerning of antibiotic potential of PCMX based novel azetidinones. Acta Pol. Pharm. 2017, 76, 1711–1715. [Google Scholar]
- Herrera, H.A.; Franco, O.L.; Fang, L.; Día, C.A. Susceptibility of Porphyromonas gingivalis and Streptococcus mutans to antibacterial effect from Mammea americana. Adv. Pharmacol. Sci. 2014, 2014, 384815. [Google Scholar]
- Susceptibility Testing. CLSI Supplement M100S, 26th ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2016; ISBN 1-56238-923-8.

| Compound (µg/mL) | Organisms/Strain | |||||
|---|---|---|---|---|---|---|
| P. gingivalis | E. coli | S. aureus | S. epidermidis | P. aeruginosa | S. pyogenes | |
| Compound 2 | 62.50 | 55.55 | 125 | 83.33 | 62.50 | 125 |
| Compound 3 | 62.50 | 31.25 | 62.50 | 62.50 | 41.66 | 104 |
| Compound 4a | 62.50 | 31.25 | 62.50 | 31.25 | 31.25 | 104 |
| Compound 4b | 62.50 | 31.25 | 62.50 | 62.50 | 31.25 | 83.33 |
| Compound 4c | 31.25 | 31.25 | 83.33 | 62.50 | 52 | 62.50 |
| Benzamidine (1) | 62.50 | 31.25 | 125 | 52 | 62.50 | 104.16 |
| Ampicillin | 0.15 | 15.62 | 7.81 | 31.25 | - | 7.81 |
| Kanamycin | - | - | - | - | 46.87 | - |
| Compound (µg/mL) | Organisms/Strain | |||||
|---|---|---|---|---|---|---|
| P. gingivalis | E. coli | S. aureus | S. epidermidis | P. aeruginosa | S. pyogenes | |
| Compound 2 | 125 | - | - | - | - | - |
| Compound 3 | 125 | - | - | 125 | - | - |
| Compound 4a | 125 | - | 125 | 62.50 | 125 | - |
| Compound 4b | 125 | - | 125 | 125 | - | - |
| Compound 4c | 62.50 | 125 | - | - | 125 | - |
| Benzamidine (1) | 125 | - | - | - | - | |
| Ampicillin | 0.62 | 62.50 | 62.50 | 125 | - | 62.50 |
| Kanamycin | - | - | - | - | 187.50 | - |
| Concentration | Chlorhexidine | Compound 1 | Compound 2 | Compound 3 | Compound 4a | Compound 4b | Compound 4c |
|---|---|---|---|---|---|---|---|
| 250 µg | 70.23 ± 13.62 | 96.03 ±17.65 * | 114.80 ± 10.81 *** | 114.80 ± 10.81 | 115.74 ± 20.62 *** | 97.27 ± 17.44 * | 91.29 ± 15.47 |
| 125 µg | 84.15 ±17.16 | 94.41 ± 9.93 | 100.71 ± 6.74 | 100.71 ± 6.74 | 97.66 ± 6.08 | 96.69 ± 17.14 | 94.59 ± 6.03 |
| 62.50 µg | 58.81 ± 6.68 | 93.56 ± 10.72 * | 111.10 ± 16.38 *** | 111.10 ± 16.38 *** | 100.74 ± 13.44 *** | 99.20 ± 19.54 *** | 93.04 ± 15.18 *** |
| 31.25 µg | 70.45 ± 17.57 | 94.83 ± 17.46 * | 107.65 ± 29.99 ** | 107.65 ± 29.99 | 101.89 ± 11.23 | 102.85 ± 12.81 | 100.59 ± 13.36 |
| 15.65 µg | 86.00 ± 18.64 | 105.89 ± 19.53 | 100.67 ± 29.35 | 100.67 ± 29.35 ** | 105.31 ± 17.71 * | 103.30 ± 17.78 ** | 99.28 ± 18.53 * |
| 7.81 µg | 103.49 ± 18.04 | 122.87 ± 17.59 | 116.06 ± 19.78 | 116.06 ± 19.78 | 106.1 ± 26.76 | 102.09 ± 22.91 | 107.60 ± 23.88 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sa’ad, M.A.; Kavitha, R.; Fuloria, S.; Fuloria, N.K.; Ravichandran, M.; Lalitha, P. Synthesis, Characterization and Biological Evaluation of Novel Benzamidine Derivatives: Newer Antibiotics for Periodontitis Treatment. Antibiotics 2022, 11, 207. https://doi.org/10.3390/antibiotics11020207
Sa’ad MA, Kavitha R, Fuloria S, Fuloria NK, Ravichandran M, Lalitha P. Synthesis, Characterization and Biological Evaluation of Novel Benzamidine Derivatives: Newer Antibiotics for Periodontitis Treatment. Antibiotics. 2022; 11(2):207. https://doi.org/10.3390/antibiotics11020207
Chicago/Turabian StyleSa’ad, Mohammad Auwal, Ramasamy Kavitha, Shivkanya Fuloria, Neeraj Kumar Fuloria, Manickam Ravichandran, and Pattabhiraman Lalitha. 2022. "Synthesis, Characterization and Biological Evaluation of Novel Benzamidine Derivatives: Newer Antibiotics for Periodontitis Treatment" Antibiotics 11, no. 2: 207. https://doi.org/10.3390/antibiotics11020207
APA StyleSa’ad, M. A., Kavitha, R., Fuloria, S., Fuloria, N. K., Ravichandran, M., & Lalitha, P. (2022). Synthesis, Characterization and Biological Evaluation of Novel Benzamidine Derivatives: Newer Antibiotics for Periodontitis Treatment. Antibiotics, 11(2), 207. https://doi.org/10.3390/antibiotics11020207