Social Media and COVID-19—Perceptions and Public Deceptions of Ivermectin, Colchicine and Hydroxychloroquine: Lessons for Future Pandemics
Abstract
:1. Introduction
2. Results
2.1. Summary of Posts Analysed
2.2. Social Mentions of Repurposed Medicines
2.3. Ivermectin
2.4. Chloroquine (Hydroxychloroquine)
2.5. Colchicine
2.6. Social Media Trendlines and Reporter Segmentation Analysis
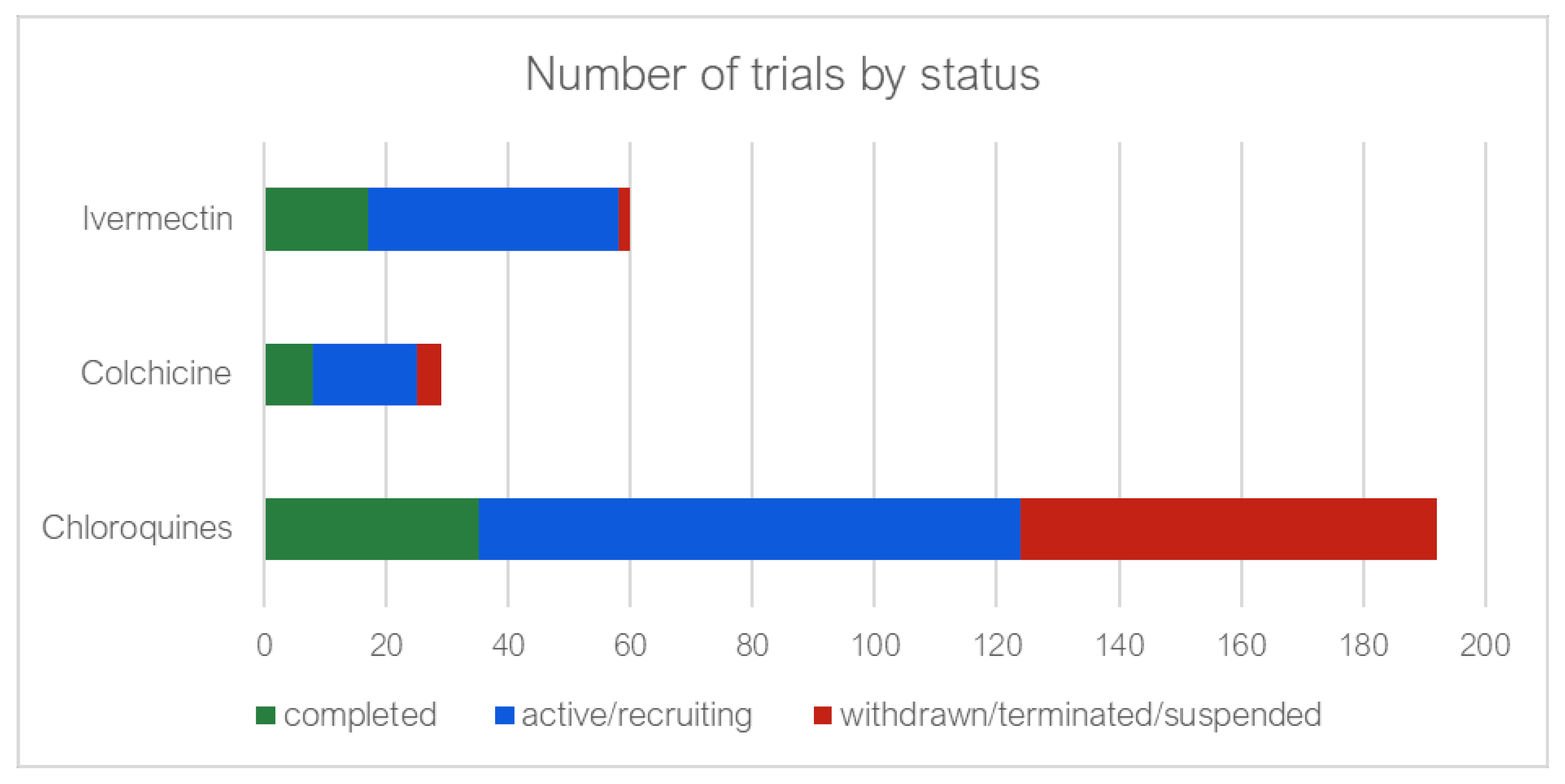
2.7. Clinical Trial Analysis
3. Discussion
4. Materials and Methods
4.1. Study Design and Setting
4.2. Data Collection
4.2.1. Social Media and Utilisation Data
4.2.2. Clinical Trials
4.3. Processing of Data and Statistics
4.3.1. Social Media
4.3.2. Clinical Trials
4.3.3. Triangulation and Trustworthiness of the Data
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rajendran, D.K.; Rajagopal, V.; Alagumanian, S.; Kumar, T.S.; Prabhakaran, S.S.; Kasilingam, D. Systematic literature review on novel corona virus SARS-CoV-2: A threat to human era. Virusdisease 2020, 31, 161–173. [Google Scholar] [CrossRef] [PubMed]
- Ogunleye, O.O.; Basu, D.; Mueller, D.; Sneddon, J.; Seaton, R.A.; Yinka-Ogunleye, A.F.; Wamboga, J.; Miljković, N.; Mwita, J.C.; Rwegerera, G.M.; et al. Response to the Novel Corona Virus (COVID-19) Pandemic Across Africa: Successes, Challenges, and Implications for the Future. Front. Pharmacol. 2020, 11, 1205. [Google Scholar] [CrossRef]
- Godman, B.; Haque, M.; Islam, S.; Iqbal, S.; Urmi, U.L.; Kamal, Z.M.; Shuvo, S.A.; Rahman, A.; Kamal, M.; Haque, M.; et al. Rapid Assessment of Price Instability and Paucity of Medicines and Protection for COVID-19 Across Asia: Findings and Public Health Implications for the Future. Front. Public Health 2020, 8, 585832. [Google Scholar] [CrossRef] [PubMed]
- Tsao, S.-F.; Chen, H.; Tisseverasinghe, T.; Yang, Y.; Li, L.; Butt, Z.A. What social media told us in the time of COVID-19: A scoping review. Lancet Digit. Health 2021, 3, e175–e194. [Google Scholar] [CrossRef] [PubMed]
- Ng, Y.; Li, Z.; Chua, Y.X.; Chaw, W.L.; Zhao, Z.; Er, B.; Pung, R.; Chiew, C.J.; Lye, D.; Heng, D.; et al. Evaluation of the Effectiveness of Surveillance and Containment Measures for the First 100 Patients with COVID-19 in Singapore—January 2–February 29, 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 307–311. [Google Scholar] [CrossRef] [PubMed]
- WHO. COVID-19 Strategic Preparedness and Response Plan—Operational Planning Guidelines to Support Country Preparedness and Response. 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/covid-19-sprp-unct-guidelines.pdf?sfvrsn=81ff43d8_4 (accessed on 9 February 2022).
- Etando, A.; Amu, A.A.; Haque, M.; Schellack, N.; Kurdi, A.; Alrasheedy, A.A.; Timoney, A.; Mwita, J.C.; Rwegerera, G.M.; Patrick, O.; et al. Challenges and Innovations Brought about by the COVID-19 Pandemic Regarding Medical and Pharmacy Education Especially in Africa and Implications for the Future. Health 2021, 9, 1722. [Google Scholar] [CrossRef] [PubMed]
- WHO. Operational Considerations for Case Management of COVID-19 in Health Facility and Community: Interim Guidance. March 2020. Available online: https://www.who.int/publications/i/item/10665-331492 (accessed on 9 February 2022).
- Ayouni, I.; Maatoug, J.; Dhouib, W.; Zammit, N.; Ben Fredj, S.; Ghammam, R.; Ghannem, H. Effective public health measures to mitigate the spread of COVID-19: A systematic review. BMC Public Health 2021, 21, 1015. [Google Scholar] [CrossRef]
- Nussbaumer-Streit, B.; Mayr, V.; Dobrescu, A.I.; Chapman, A.; Persad, E.; Klerings, I.; Wagner, G.; Siebert, U.; Ledinger, D.; Zachariah, C. Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review. Cochrane Database Syst. Rev. 2020, 9, Cd013574. [Google Scholar] [CrossRef]
- Sefah, I.A.; Ogunleye, O.O.; Essah, D.O.; Opanga, S.A.; Butt, N.; Wamaitha, A.; Guantai, A.N.; Chikowe, I.; Khuluza, F.; Kibuule, D.; et al. Rapid Assessment of the Potential Paucity and Price Increases for Suggested Medicines and Protection Equipment for COVID-19 Across Developing Countries With a Particular Focus on Africa and the Implications. Front. Pharmacol. 2021, 11, 588106. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, M.; Dyer, S. Information and Disinformation: Social Media in the COVID-19 Crisis. Acad. Emerg. Med. 2020, 27, 640–641. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Padilla, D.A.; Tortolero-Blanco, L. Social media influence in the COVID-19 Pandemic. Int. Braz. J. Urol. 2020, 46 (Suppl. 1), 120–124. [Google Scholar] [CrossRef] [PubMed]
- Al-Dmour, H.; Masa’Deh, R.; Salman, A.; Abuhashesh, M.; Al-Dmour, R. Influence of Social Media Platforms on Public Health Protection Against the COVID-19 Pandemic via the Mediating Effects of Public Health Awareness and Behavioral Changes: Integrated Model. J. Med. Internet Res. 2020, 22, e19996. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Liu, Q. Social Media Use, eHealth Literacy, Disease Knowledge, and Preventive Behaviors in the COVID-19 Pandemic: Cross-Sectional Study on Chinese Netizens. J. Med. Internet Res. 2020, 22, e19684. [Google Scholar] [CrossRef] [PubMed]
- Kricorian, K.; Civen, R.; Equils, O. COVID-19 vaccine hesitancy: Misinformation and perceptions of vaccine safety. Hum. Vaccines Immunother. 2022, 18, 1950504. [Google Scholar] [CrossRef] [PubMed]
- Carrieri, V.; Madio, L.; Principe, F. Vaccine hesitancy and (fake) news: Quasi-experimental evidence from Italy. Health Econ. 2019, 28, 1377–1382. [Google Scholar] [CrossRef]
- Rocha, Y.M.; de Moura, G.A.; Desidério, G.A.; de Oliveira, C.H.; Lourenço, F.D.; Nicolete, L.D.D.F. The impact of fake news on social media and its influence on health during the COVID-19 pandemic: A systematic review. J. Public Health 2021, 1–10. [Google Scholar] [CrossRef]
- Yang, Y. Use of herbal drugs to treat COVID-19 should be with caution. Lancet 2020, 395, 1689–1690. [Google Scholar] [CrossRef]
- De, P.; Chakraborty, I.; Karna, B.; Mazumder, N. Brief review on repurposed drugs and vaccines for possible treatment of COVID-19. Eur. J. Pharmacol. 2021, 898, 173977. [Google Scholar] [CrossRef] [PubMed]
- Garcia, M.A.; Johnson, S.W.; Bosch, N.A.; Sisson, E.K.; Sheldrick, C.R.; Kumar, V.K.; Boman, K.; Bolesta, S.; Bansal, V.; Deo, N.; et al. Variation in Use of Repurposed Medications Among Patients With Coronavirus Disease 2019. From The Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study: Coronavirus Disease 2019 Registry Investigator Group. Crit. Care Explor. 2021, 3, e0566. [Google Scholar] [CrossRef] [PubMed]
- Machiels, J.D.; Bleeker-Rovers, C.P.; ter Heine, R.; Rahamat-Langendoen, J.; de Mast, Q.; Oever, J.T.; Bousema, T.; van Crevel, R.; Wertheim, H.F. Reply to Gautret et al: Hydroxychloroquine sulfate and azithromycin for COVID-19: What is the evidence and what are the risks? Int. J. Antimicrob. Agents 2020, 56, 106056. [Google Scholar] [CrossRef] [PubMed]
- Bloom, D.E.; Cadarette, D. Infectious Disease Threats in the Twenty-First Century: Strengthening the Global Response. Front. Immunol. 2019, 10, 549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenhalgh, T.; Kostopoulou, O.; Harries, C. Making decisions about benefits and harms of medicines. BMJ 2004, 329, 47–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Begley, C.G.; Ashton, M.; Baell, J.; Bettess, M.; Brown, M.P.; Carter, B.; Charman, W.N.; Davis, C.; Fisher, S.; Frazer, I.; et al. Drug repurposing: Misconceptions, challenges, and opportunities for academic researchers. Sci. Transl. Med. 2021, 13, 5524. [Google Scholar] [CrossRef] [PubMed]
- Khadka, S.; Shrestha, D.B.; Budhathoki, P.; Rawal, E. Hydroxychloroquine in COVID-19: The Study Points to Premature Decisions on Efficacy While Bells Ringing for Safety. Clin. Pharmacol. Adv. Appl. 2020, 12, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Acharya, Y.; Sayed, A. Chloroquine and hydroxychloroquine as a repurposed agent against COVID-19: A narrative review. Ther. Adv. Infect. Dis. 2020, 7, 2049936120947517. [Google Scholar] [CrossRef]
- Gautret, P.; Lagier, J.C.; Parola, P.; Hoang, V.T.; Meddeb, L.; Mailhe, M.; Doudier, B.; Courjon, J.; Giordanengo, V.; Vieira, V.E.; et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int. J. Antimicrob. Agents 2020, 56, 105949. [Google Scholar] [CrossRef]
- Sulis, G.; Batomen, B.; Kotwani, A.; Pai, M.; Gandra, S. Sales of antibiotics and hydroxychloroquine in India during the COVID-19 epidemic: An interrupted time series analysis. PLoS Med. 2021, 18, e1003682. [Google Scholar] [CrossRef] [PubMed]
- Godman, B.; Haque, M.; Abubakar, A.R.; Ogunleye, O.O.; Sani, I.H.; Sefah, I.; Kurdi, A.; Islam, S. Changes in availability, utilization, and prices of medicines and protection equipment for COVID-19 in an Urban population of Northern Nigeria. J. Res. Pharm. Pract. 2021, 10, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Sefah, I.A.; Essah, D.O.; Haque, M.; Opanga, S.A.; Kumar, S.; Chikowe, I.; Kibuule, D.; Rampamba, E.M.; Kalungia, A.C.; Phuong, T.N.T.; et al. COVID-19, health care and self-medication issues in resource-limited settings: Findings and implications based on experiences in Ghana. Adv. Hum. Biol. 2021, 11, 224–233. [Google Scholar] [CrossRef]
- Anwar, A.; Malik, M.; Raees, V.; Anwar, A. Role of Mass Media and Public Health Communications in the COVID-19 Pandemic. Cureus 2020, 12, e10453. [Google Scholar] [CrossRef]
- Rosendaal, F.R. Review of: “Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial Gautret et al 2010”. Int. J. Antimicrob. Agents 2020, 56, 106063. [Google Scholar] [CrossRef] [PubMed]
- ISAC/Elsevier Statement. Joint ISAC and Elsevier statement on Gautret et al. Paper [PMID 32205204]. 2020. Available online: https://www.isac.world/news-and-publications/isac-elsevier-statement (accessed on 9 February 2022).
- RECOVERY Collaborative Group; Horby, P.; Mafham, M.; Linsell, L.; Bell, J.L.; Staplin, N.; Emberson, J.R.; Wiselka, M.; Ustianowski, A.; Elmahi, E.; et al. Effect of Hydroxychloroquine in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2020, 383, 2030–2040. [Google Scholar] [CrossRef] [PubMed]
- Manivannan, E.; Karthikeyan, C.; Moorthy, N.S.H.N.; Chaturvedi, S.C. The Rise and Fall of Chloroquine/Hydroxychloroquine as Compassionate Therapy of COVID-19. Front. Pharmacol. 2021, 12, 584940. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.; Bagozzi, D. WHO Discontinues Hydroxychloroquine and Lopinavir/Ritonavir Treatment Arms for COVID-19. World Health Organization News Release: 2020. Available online: https://www.who.int/news/item/04-07-2020-who-discontinues-hydroxychloroquine-and-lopinavir-ritonavir-treatment-arms-for-covid-19 (accessed on 9 February 2022).
- Saghir, S.A.; AlGabri, N.A.; Alagawany, M.M.; Attia, Y.A.; Alyileili, S.R.; Elnesr, S.S.; Shafi, M.E.; Al-Shargi, O.Y.; Al-Balagi, N.; Alwajeeh, A.S.; et al. Chloroquine and Hydroxychloroquine for the Prevention and Treatment of COVID-19: A Fiction, Hope or Hype? An Updated Review. Ther. Clin. Risk Manag. 2021, 17, 371–387. [Google Scholar] [CrossRef]
- Abena, P.M.; Decloedt, E.H.; Bottieau, E.; Suleman, F.; Adejumo, P.; Sam-Agudu, N.A.; Muyembe TamFum, J.-J.; Seydi, M.; Eholie, S.P.; Mills, E.J.; et al. Chloroquine and Hydroxychloroquine for the Prevention or Treatment of novel coronavirus disease (COVID-19) in Africa: Caution for Inappropriate Off-label Use in Healthcare Settings. Am. J. Trop. Med. Hyg. 2020, 102, 1184–1188. [Google Scholar] [CrossRef]
- Ferner, R.E.; Aronson, J.K. Chloroquine and hydroxychloroquine in COVID-19. BMJ 2020, 369, m1432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, H.; Peto, R.; Henao-Restrepo, A.M.; Preziosi, M.P.; Sathiyamoorthy, V.; Abdool Karim, Q.; Alejandria, M.M.; Hernández García, C.; Kieny, M.P.; Malekzadeh, R.; et al. Repurposed Antiviral Drugs for COVID-19—Interim WHO Solidarity Trial Results. N. Engl. J. Med. 2021, 384, 497–511. [Google Scholar] [CrossRef] [PubMed]
- Lamontagne, F.; Agoritsas, T.; Siemieniuk, R.; Rochwerg, B.; Bartoszko, J.; Askie, L.; Macdonald, H.; Amin, W.; Bausch, F.J.; Burhan, E.; et al. A living WHO guideline on drugs to prevent COVID-19. BMJ 2021, 372, n526. [Google Scholar] [CrossRef]
- Horby, P.W.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Emberson, J.; Palfreeman, A.; Raw, J.; Elmahi, E.; Prudon, B.; et al. Lopinavir–ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet 2020, 396, 1345–1352. [Google Scholar] [CrossRef]
- Abubakar, A.R.; Sani, I.H.; Godman, B.; Kumar, S.; Islam, S.; Jahan, I.; Haque, M. Systematic Review on the Therapeutic Options for COVID-19: Clinical Evidence of Drug Efficacy and Implications. Infect. Drug Resist. 2020, 13, 4673–4695. [Google Scholar] [CrossRef] [PubMed]
- Dyer, O. COVID-19: Remdesivir has little or no impact on survival, WHO trial shows. BMJ 2020, 371, m4057. [Google Scholar] [CrossRef] [PubMed]
- Schlesinger, N.; Firestein, B.L.; Brunetti, L. Colchicine in COVID-19: An Old Drug, New Use. Curr. Pharmacol. Rep. 2020, 6, 137–145. [Google Scholar] [CrossRef]
- Karatza, E.; Ismailos, G.; Karalis, V. Colchicine for the treatment of COVID-19 patients: Efficacy, safety, and model informed dosage regimens. Xenobiotica 2021, 51, 643–656. [Google Scholar] [CrossRef] [PubMed]
- Chiu, L.; Lo, C.-H.; Shen, M.; Chiu, N.; Aggarwal, R.; Lee, J.; Choi, Y.-G.; Lam, H.; Prsic, E.H.; Chow, R.; et al. Colchicine use in patients with COVID-19: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0261358. [Google Scholar] [CrossRef] [PubMed]
- Nawangsih, E.N.; Kusmala, Y.Y.; Rakhmat, I.I.; Handayani, D.R.; Juliastuti, H.; Wibowo, A.; Lim, M.A.; Pranata, R. Colchicine and mortality in patients with coronavirus disease 2019 (COVID-19) pneumonia: A systematic review, meta-analysis, and meta-regression. Int. Immunopharmacol. 2021, 96, 107723. [Google Scholar] [CrossRef] [PubMed]
- Schellack, N.; Padayachee, N. Ivermectin in the treatment of COVID-19- friend or foe? S. Afr. Gen. Pract. 2021, 2, 15–19. [Google Scholar] [CrossRef]
- Dixit, A.; Yadav, R.; Singh, A.V. Ivermectin: Potential Role as Repurposed Drug for COVID-19. Malays. J. Med. Sci. 2020, 27, 154–158. [Google Scholar] [CrossRef]
- Garegnani, L.I.; Madrid, E.; Meza, N. Misleading clinical evidence and systematic reviews on ivermectin for COVID-19. BMJ Evid.-Based Med. 2021. [Google Scholar] [CrossRef]
- Roman, Y.M.; Burela, P.A.; Pasupuleti, V.; Piscoya, A.; Vidal, J.E.; Hernandez, A.V. Ivermectin for the treatment of COVID-19: A systematic review and meta-analysis of randomized controlled trials. Clin. Infect. Dis. 2021, ciab591. [Google Scholar] [CrossRef]
- Wadvalla, B.-A. COVID-19: Ivermectin’s politicisation is a warning sign for doctors turning to orphan treatments. BMJ 2021, 373, n747. [Google Scholar] [CrossRef] [PubMed]
- SAHPRA. Chloroquine and Hydroxychloroquine for Treatment of COVID-19: Evidence Review of Clinical Benefits and Harms; South African National Department of Health: Pretoria, South Africa, 2021. [Google Scholar]
- SAHPRA. Ivermectin for Prophylaxis of COVID-19; South African National Department of Health: Pretoria, South Africa, 2021. [Google Scholar]
- SAHPRA. Colchicine for COVID-19: Evidence Review of the Clinical Benefit and Harm; South African National Department of Health: Pretoria, South Africa, 2021. [Google Scholar]
- Carrion-Alvarez, D.; Tijerina-Salina, P.X. Fake news in COVID-19: A perspective. Health Promot. Perspect. 2020, 10, 290–291. [Google Scholar] [CrossRef] [PubMed]
- Apuke, O.D.; Omar, B. Fake news and COVID-19: Modelling the predictors of fake news sharing among social media users. Telemat. Inform. 2021, 56, 101475. [Google Scholar] [CrossRef] [PubMed]
- Saag, M.S. Misguided use of hydroxychloroquine for COVID-19: The infusion of politics into science. JAMA 2020, 324, 2161–2162. [Google Scholar] [CrossRef] [PubMed]
- Molina, J.; Delaugerre, C.; Le Goff, J.; Mela-Lima, B.; Ponscarme, D.; Goldwirt, L.; de Castro, N. No evidence of rapid antiviral clearance or clinical benefit with the combination of hydroxychloroquine and azithromycin in patients with severe COVID-19 infection. Méd. Mal. Infect. 2020, 50, 384. [Google Scholar] [CrossRef]
- Somberg, J. Science, Politics and Hydroxychloroquine. Cardiol. Res. 2020, 11, 267–268. [Google Scholar] [CrossRef] [PubMed]
- Tardif, J.-C.; Bouabdallaoui, N.; L’Allier, P.L.; Gaudet, D.; Shah, B.; Pillinger, M.H.; Lopez-Sendon, J.; da Luz, P.; Verret, L.; Audet, S.; et al. Colchicine for community-treated patients with COVID-19 (COLCORONA): A phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial. Lancet Respir. Med. 2021, 9, 924–932. [Google Scholar] [CrossRef]
- Recovery Collaborative Group. Colchicine in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet Respir. Med. 2021, 9, 1419–1426. [Google Scholar] [CrossRef]
- Gupta, D.; Sahoo, A.K.; Singh, A. Ivermectin: Potential candidate for the treatment of COVID 19. Braz. J. Infect. Dis. 2020, 24, 369–371. [Google Scholar] [CrossRef] [PubMed]
- Caly, L.; Druce, J.D.; Catton, M.G.; Jans, D.A.; Wagstaff, K.M. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antivir. Res. 2020, 178, 104787. [Google Scholar] [CrossRef] [PubMed]
- Charan, J.; Kaur, R.J.; Bhardwaj, P.; Haque, M.; Sharma, P.; Misra, S.; Godman, B. Rapid review of suspected adverse drug events due to remdesivir in the WHO database; findings and implications. Expert Rev. Clin. Pharmacol. 2021, 14, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Calvo, R.A.; Deterding, S.; Ryan, R.M. Health surveillance during COVID-19 pandemic. BMJ 2020, 369, m1373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ezeibe, C.C.; Ilo, C.; Ezeibe, E.N.; Oguonu, C.N.; Nwankwo, N.A.; Ajaero, C.K.; Osadebe, N. Political distrust and the spread of COVID-19 in Nigeria. Glob. Public Health 2020, 15, 1–14. [Google Scholar] [CrossRef]
- Chan, R.K. Tackling COVID-19 risk in Hong Kong: Examining distrust, compliance and risk management. Curr. Sociol. 2021, 0011392121990026. [Google Scholar] [CrossRef]
- Aghion, P.; Algan, Y.; Cahuc, P.; Shleifer, A. Regulation and Distrust. Q. J. Econ. 2010, 125, 1015–1049. [Google Scholar] [CrossRef]
- Cadogan, C.A.; Hughes, C.M. On the frontline against COVID-19: Community pharmacists’ contribution during a public health crisis. Res. Soc. Adm. Pharm. 2021, 17, 2032–2035. [Google Scholar] [CrossRef]
- Hedima, E.W.; Adeyemi, M.S.; Ikunaiye, N.Y. Community Pharmacists: On the frontline of health service against COVID-19 in LMICs. Res. Social. Adm. Pharm. 2021, 17, 1964–1966. [Google Scholar] [CrossRef]
- Kibuule, D.; Nambahu, L.; Sefah, I.A.; Kurdi, A.; Phuong, T.N.T.; Kwon, H.Y.; Godman, B. Activities in Namibia to limit the prevalence and mortality from COVID-19 including community pharmacy activities and the implications. Sch. Acad. J. Pharm. 2021, 5, 82–92. [Google Scholar] [CrossRef]
- Marković-Peković, V.; Grubiša, N.; Burger, J.; Bojanić, L.; Godman, B. Initiatives to reduce nonprescription sales and dispensing of antibiotics: Findings and implications. J. Res. Pharm. Pract. 2017, 6, 120. [Google Scholar] [CrossRef]
- Gross, M.; Latham, D. What’s skill got to do with it?: Information literacy skills and self-views of ability among first-year college students. J. Am. Soc. Inf. Sci. Technol. 2012, 63, 574–583. [Google Scholar] [CrossRef] [Green Version]
- Dunn, A.G.; Leask, J.; Zhou, X.; Mandl, K.D.; Coiera, E. Associations between Exposure to and Expression of Negative Opinions about Human Papillomavirus Vaccines on Social Media: An Observational Study. J. Med. Internet Res. 2015, 17, e144. [Google Scholar] [CrossRef] [PubMed]
- Milan, S. When Algorithms Shape Collective Action: Social Media and the Dynamics of Cloud Protesting. Soc. Media Soc. 2015, 1, 2056305115622481. [Google Scholar] [CrossRef] [Green Version]
- Wyche, S.; Olson, J. Gender, Mobile, and Mobile Internet| Kenyan Women’s Rural Realities, Mobile Internet Access, and “Africa Rising”. Inf. Technol. Int. Dev. 2018, 14, 15. [Google Scholar]
- Chisango, G.; Marongwe, N. The digital divide at three disadvantaged secondary schools in Gauteng, South Africa. J. Educ. 2021, 2021, 149–165. [Google Scholar] [CrossRef]
- Chowdhury, K.; Haque, M.; Nusrat, N.; Adnan, N.; Islam, S.; Lutfor, A.B.; Begum, D.; Rabbany, A.; Karim, E.; Malek, A.; et al. Management of Children Admitted to Hospitals across Bangladesh with Suspected or Confirmed COVID-19 and the Implications for the Future: A Nationwide Cross-Sectional Study. Antibiotics 2022, 11, 105. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Haque, M.; Shetty, A.; Acharya, J.; Kumar, M.; Sinha, V.K.; Manohar, B.; Gowere, M.; Godman, B. Current management of children with COVID-19 in hospitals in India; Pilot study and findings. Adv. Hum. Biol. 2022, 12, 16. [Google Scholar] [CrossRef]
- Opanga, S.A.; Rizvi, N.; Wamaitha, A.; Sefah, I.A.; Godman, B. Availability of Medicines in Community Pharmacy to Manage Patients with COVID-19 in Kenya; Pilot Study and Implications. Sch. Acad. J. Pharm. 2021, 3, 36–42. [Google Scholar] [CrossRef]
- Parrish, A.G.; Blockman, M.; Cohen, K.; Dawood, H.; De Waal, R.; Gray, A.L.; Kredo, T.; Leong, T.D.; Nel, J.; Rees, H.; et al. Meta-analytic magic, ivermectin, and socially responsible reporting. S. Afr. Med. J. 2021, 111, 934–937. [Google Scholar] [CrossRef] [PubMed]
- Schellack, N.; Benjamin, D.; Brink, A.; Duse, A.; Faure, K.; Goff, D.; Mendelson, M.; Meyer, J.; Miot, J.; Perovic, O.; et al. A situational analysis of current antimicrobial governance, regulation, and utilization in South Africa. Int. J. Infect. Dis. 2017, 64, 100–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lincoln, Y.S.; Guba, E.G. Naturalistic Inquiry Newbury Park; Sage: Thousand Oaks, CA, USA, 1985. [Google Scholar]
- Bonanno, P.V.; Ermisch, M.; Godman, B.; Martin, A.; Bergh, J.V.D.; Bezmelnitsyna, L.; Bucsics, A.; Arickx, F.; Bybau, A.; Bochenek, T.; et al. Adaptive Pathways: Possible Next Steps for Payers in Preparation for Their Potential Implementation. Front. Pharmacol. 2017, 8, 497. [Google Scholar] [CrossRef] [Green Version]
- Godman, B.; Haque, M.; McKimm, J.; Abu Bakar, M.; Sneddon, J.; Wale, J.; Campbell, S.; Martin, A.P.; Hoxha, I.; Abilova, V.; et al. Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries: Findings and implications for the future. Curr. Med. Res. Opin. 2019, 36, 301–327. [Google Scholar] [CrossRef] [PubMed]








| Stratification | Total | News | Forum | Blogs | Tumblr | |
|---|---|---|---|---|---|---|
| Total number of posts collected | 77,257 | 65,850 | 7726 | 2588 | 1046 | 47 |
| Number of posts filtered and contextualized to authors/reporters | 25,021 | 15,460 | 6540 | 2150 | 824 | 47 |
| Total number of posts analysed | 11,688 | 5800 | 5076 | 560 | 205 | 47 |
| Number of posts identified to be relevant | 6884 | 1558 | 5076 | 44 | 205 | 1 |
| Number of unique authors/reporters identified from relevant posts | 1070 | 907 | 70 | 28 | 64 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schellack, N.; Strydom, M.; Pepper, M.S.; Herd, C.L.; Hendricks, C.L.; Bronkhorst, E.; Meyer, J.C.; Padayachee, N.; Bangalee, V.; Truter, I.; et al. Social Media and COVID-19—Perceptions and Public Deceptions of Ivermectin, Colchicine and Hydroxychloroquine: Lessons for Future Pandemics. Antibiotics 2022, 11, 445. https://doi.org/10.3390/antibiotics11040445
Schellack N, Strydom M, Pepper MS, Herd CL, Hendricks CL, Bronkhorst E, Meyer JC, Padayachee N, Bangalee V, Truter I, et al. Social Media and COVID-19—Perceptions and Public Deceptions of Ivermectin, Colchicine and Hydroxychloroquine: Lessons for Future Pandemics. Antibiotics. 2022; 11(4):445. https://doi.org/10.3390/antibiotics11040445
Chicago/Turabian StyleSchellack, Natalie, Morné Strydom, Michael S. Pepper, Candice L. Herd, Candice Laverne Hendricks, Elmien Bronkhorst, Johanna C. Meyer, Neelaveni Padayachee, Varsha Bangalee, Ilse Truter, and et al. 2022. "Social Media and COVID-19—Perceptions and Public Deceptions of Ivermectin, Colchicine and Hydroxychloroquine: Lessons for Future Pandemics" Antibiotics 11, no. 4: 445. https://doi.org/10.3390/antibiotics11040445
APA StyleSchellack, N., Strydom, M., Pepper, M. S., Herd, C. L., Hendricks, C. L., Bronkhorst, E., Meyer, J. C., Padayachee, N., Bangalee, V., Truter, I., Ellero, A. A., Myaka, T., Naidoo, E., & Godman, B. (2022). Social Media and COVID-19—Perceptions and Public Deceptions of Ivermectin, Colchicine and Hydroxychloroquine: Lessons for Future Pandemics. Antibiotics, 11(4), 445. https://doi.org/10.3390/antibiotics11040445








