The Constellation of Risk Factors and Paraneoplastic Syndromes in Cholangiocarcinoma: Integrating the Endocrine Panel Amid Tumour-Related Biology (A Narrative Review)
Abstract
:Simple Summary
Abstract
1. Introduction
2. CCA-Associated Risk Factors and Potential Contributors
2.1. Chronic Biliary Diseases
2.2. Chronic Liver Conditions
2.3. Digestive Ailments
2.4. Parasitic Infections
2.5. Lifestyle Influence
2.6. Environmental Exposure
2.7. Genetic and Epigenetic (Potential) Interplay
3. Metabolic and Endocrine Interferences in CCA Development
3.1. Non-Alcoholic Fatty Liver Disease (NAFLD)
3.2. Obesity
3.3. Type 2 Diabetes Mellitus
3.4. Vitamin D Status
3.5. Glucagon-like Peptide 1 Receptor (GLP-1R)
3.6. Galanin System
3.7. Sex Hormone Therapy
4. Paraneoplastic Syndrome in CCAs
4.1. Dermatological Features Have Been Found as Followings
4.1.1. Acanthosis
4.1.2. Alopecia
4.1.3. Dermatomyositis
4.1.4. Porokeratosis
4.1.5. Necrotic Migratory Erythema
4.1.6. Persistent Erythema Multiform
4.1.7. Sweet Syndrome
4.1.8. Bazex Syndrome
4.1.9. Erythema
4.1.10. Pityriasis
4.1.11. Lupus
4.1.12. Leser–Trelat Sign
4.1.13. Porphyria
4.2. Neurological Paraneoplastic Elements
4.3. Renal Findings
4.4. Haematological Manifestations
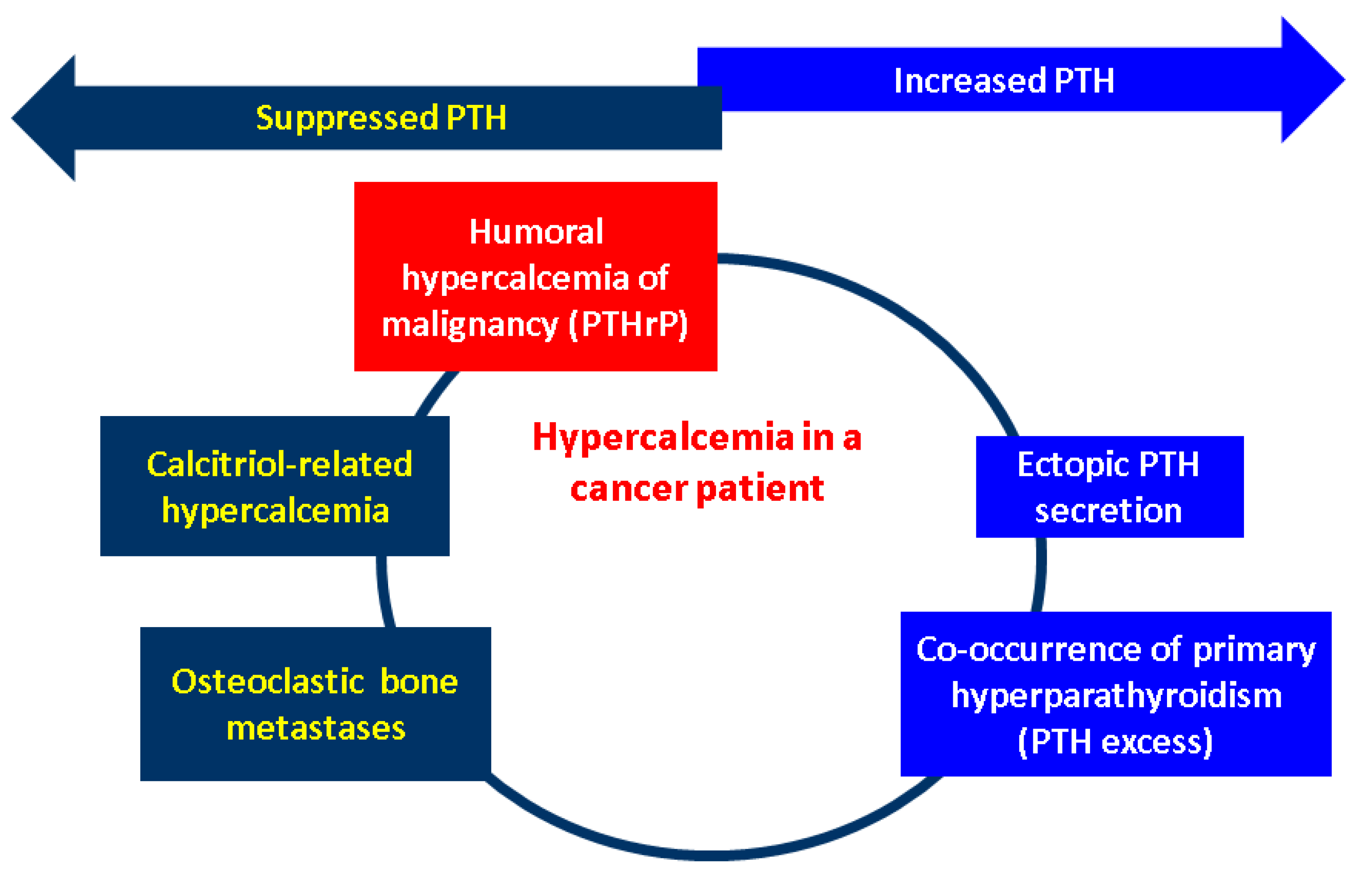
4.5. Humoral Manifestations
5. Discussion
5.1. Imagery Tools to Help the Clinical Assessment
5.2. Is There a Place for Endocrine Considerations in CCAs?
5.3. Current Limits and Further Expansion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANCA | anti-neutrophilic cytoplasmic antibodies |
| ATF2 | activating transcription factor-2 |
| CCA | cholangiocarcinoma |
| CA 19-9 | carbohydrate antigen 19-9 |
| CI | confidence interval |
| CEUS | contrast-enhanced ultrasound |
| dCCA | distal cholangiocarcinoma |
| DNA | deoxyribonucleic acid |
| DDP4 | dipeptidyl peptidase 4 inhibitors |
| ENDSs | electronic nicotine delivery systems |
| ERK | extracellular signal-related kinase |
| CCAs | extrahepatic cholangiocarcinoma |
| GLP-1R | glucagon-like peptide 1 receptor |
| GAL-R | galanin receptors |
| G-CSF | granulocyte-colony stimulation factor |
| HBV | hepatitis B virus chronic infection |
| HVC | hepatitis C virus chronic infection |
| iCCA | intrahepatic cholangiocarcinoma |
| JNK | c-Jun N-terminal kinase |
| NAFLD | non-alcoholic fatty liver disease |
| NASH | non-alcoholic steatohepatitis |
| NOX1 | KNOTTED-like homebox |
| NOX | NADPH oxidase |
| pCCA | perihilar cholangiocarcinoma |
| PSC | primary sclerosing cholangitis |
| PTHrP | parathyroid hormone-related protein |
| PTHLH | parathyroid hormone-like hormone |
| PAN | polyarteritis nodosa |
| RNA | ribonucleic acid |
| ROS | reactive oxygen species |
| RANKL | receptor activator of nuclear factor kappa B ligand |
| S1PR2 | sphingosine-1 phosphate receptor 2 |
| TGF-α | tumour growth factor-alpha |
| TNF-α | tumour necrosis factor-alpha |
| TAUS | transabdominal ultrasound |
References
- Khan, S.A.; Tavolari, S.; Brandi, G. Cholangiocarcinoma: Epidemiology and risk factors. Liver Int. 2019, 39 (Suppl. S1), 19–31. [Google Scholar] [CrossRef] [PubMed]
- Dar, F.S.; Abbas, Z.; Ahmed, I.; Atique, M.; Aujla, U.I.; Azeemuddin, M.; Aziz, Z.; Bhatti, A.B.H.; Bangash, T.A.; Butt, A.S.; et al. National guidelines for the diagnosis and treatment of hilar cholangiocarcinoma. World J. Gastroenterol. 2024, 30, 1018–1042. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Moon, S.H.; Kim, J.H. Diagnosis of Cholangiocarcinoma. Diagnostics 2023, 13, 233. [Google Scholar] [CrossRef]
- Brindley, P.J.; Bachini, M.; Ilyas, S.I.; Khan, S.A.; Loukas, A.; Sirica, A.E.; Teh, B.T.; Wongkham, S.; Gores, G.J. Cholangiocarcinoma. Nat. Rev. Dis. Primers 2021, 7, 65. [Google Scholar] [CrossRef]
- Izquierdo-Sanchez, L.; Lamarca, A.; La Casta, A.; Buettner, S.; Utpatel, K.; Klümpen, H.J.; Adeva, J.; Vogel, A.; Lleo, A.; Fabris, L.; et al. Cholangiocarcinoma landscape in Europe: Diagnostic, prognostic and therapeutic insights from the ENSCCA Registry. J. Hepatol. 2022, 76, 1109–1121. [Google Scholar] [CrossRef]
- Banales, J.M.; Marin, J.J.G.; Lamarca, A.; Rodrigues, P.M.; Khan, S.A.; Roberts, L.R.; Cardinale, V.; Carpino, G.; Andersen, J.B.; Braconi, C.; et al. Cholangiocarcinoma 2020: The next horizon in mechanisms and management. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 557–588. [Google Scholar] [CrossRef] [PubMed]
- Vithayathil, M.; Khan, S.A. Current epidemiology of cholangiocarcinoma in Western countries. J. Hepatol. 2022, 77, 1690–1698. [Google Scholar] [CrossRef]
- WHO World Health Organization (WHO). Mortality Database Health Statistics and Information Systems. 2019. Available online: https://www.who.int/data/data-collection-tools/who-mortality-database (accessed on 10 June 2024).
- Elvevi, A.; Laffusa, A.; Scaravaglio, M.; Rossi, R.E.; Longarini, R.; Stagno, A.M.; Cristoferi, L.; Ciaccio, A.; Cortinovis, D.L.; Invernizzi, P.; et al. Clinical treatment of cholangiocarcinoma: An updated comprehensive review. Ann. Hepatol. 2022, 27, 100737. [Google Scholar] [CrossRef] [PubMed]
- Barner-Rasmussen, N.; Pukkala, E.; Jussila, A.; Färkkilä, M. Epidemiology, risk of malignancy and patient survival in primary sclerosing cholangitis: A population-based study in Finland. Scand. J. Gastroenterol. 2020, 55, 74–81. [Google Scholar] [CrossRef]
- Boonstra, K.; Weersma, R.K.; van Erpecum, K.J.; Rauws, E.A.; Spanier, B.W.; Poen, A.C.; van Nieuwkerk, K.M.; Drenth, J.P.; Witteman, B.J.; Tuynman, H.A.; et al. Population-based epidemiology, malignancy risk, and outcome of primary sclerosing cholangitis. Hepatology 2013, 58, 2045–2055. [Google Scholar] [CrossRef]
- Bergquist, A.; Weismüller, T.J.; Levy, C.; Rupp, C.; Joshi, D.; Nayagam, J.S.; Montano-Loza, A.J.; Lytvyak, E.; Wunsch, E.; Milkiewicz, P.; et al. Impact on follow-up strategies in patients with primary sclerosing cholangitis. Liver Int. 2023, 43, 127–138. [Google Scholar] [CrossRef]
- Petrick, J.L.; Yang, B.; Altekruse, S.F.; Van Dyke, A.L.; Koshiol, J.; Graubard, B.I.; McGlynn, K.A. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: A population-based study in SEER-Medicare. PLoS ONE 2017, 12, e0186643. [Google Scholar] [CrossRef] [PubMed]
- Söreide, K.; Körner, H.; Havnen, J.; Söreide, J.A. Bile duct cysts in adults. Br. J. Surg. 2004, 91, 1538–1548. [Google Scholar] [CrossRef] [PubMed]
- Clements, O.; Eliahoo, J.; Kim, J.U.; Taylor-Robinson, S.D.; Khan, S.A. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma: A systematic review and meta-analysis. J. Hepatol. 2020, 72, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Jang, M.H.; Lee, Y.J.; Kim, H. Intrahepatic cholangiocarcinoma arising in Caroli’s disease. Clin. Mol. Hepatol. 2014, 20, 402–405. [Google Scholar] [CrossRef]
- Mansour, J.C.; Aloia, T.A.; Crane, C.H.; Heimbach, J.K.; Nagino, M.; Vauthey, J.N. Hilar cholangiocarcinoma: Expert consensus statement. HPB 2015, 17, 691–699. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, J.S.; Joo, M.K.; Lee, B.J.; Kim, J.H.; Yeon, J.E.; Park, J.J.; Byun, K.S.; Bak, Y.T. Hepatolithiasis and intrahepatic cholangiocarcinoma: A review. World J. Gastroenterol. 2015, 21, 13418–13431. [Google Scholar] [CrossRef]
- Cai, H.; Kong, W.T.; Chen, C.B.; Shi, G.M.; Huang, C.; Shen, Y.H.; Sun, H.C. Cholelithiasis and the risk of intrahepatic cholangiocarcinoma: A meta-analysis of observational studies. BMC Cancer 2015, 15, 831. [Google Scholar] [CrossRef]
- Palmer, W.C.; Patel, T. Are common factors involved in the pathogenesis of primary liver cancers? A meta-analysis of risk factors for intrahepatic cholangiocarcinoma. J. Hepatol. 2012, 57, 69–76. [Google Scholar] [CrossRef]
- Chang, J.S.; Tsai, C.R.; Chen, L.T. Medical risk factors associated with cholangiocarcinoma in Taiwan: A population-based case-control study. PLoS ONE 2013, 8, e69981. [Google Scholar] [CrossRef]
- Welzel, T.M.; Graubard, B.I.; El–Serag, H.B.; Shaib, Y.H.; Hsing, A.W.; Davila, J.A.; McGlynn, K.A. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: A population-based case-control study. Clin. Gastroenterol. Hepatol. 2007, 5, 1221–1228. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhao, Y.; Li, B.; Huang, J.; Wu, L.; Xu, D.; Yang, J.; He, J. Hepatitis viruses infection and risk of intrahepatic cholangiocarcinoma: Evidence from a meta-analysis. BMC Cancer 2012, 12, 289. [Google Scholar] [CrossRef]
- Li, M.; Li, J.; Li, P.; Li, H.; Su, T.; Zhu, R.; Gong, J. Hepatitis B virus infection increases the risk of cholangiocarcinoma: A meta-analysis and systematic review. J. Gastroenterol. Hepatol. 2012, 27, 1561–1568. [Google Scholar] [CrossRef]
- Zhang, H.; Zhu, B.; Zhang, H.; Liang, J.; Zeng, W. HBV Infection Status and the Risk of Cholangiocarcinoma in Asia: A Meta-Analysis. BioMed Res. Int. 2016, 2016, 3417976. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Hu, B.; Zhou, Z.Q.; Guan, J.; Zhang, Z.Y.; Zhou, G.W. Hepatitis C virus infection and the risk of intrahepatic cholangiocarcinoma and extrahepatic cholangiocarcinoma: Evidence from a systematic review and meta-analysis of 16 case-control studies. World J. Surg. Oncol. 2015, 13, 161. [Google Scholar] [CrossRef]
- Ralphs, S.; Khan, S.A. The role of the hepatitis viruses in cholangiocarcinoma. J. Viral Hepat. 2013, 20, 297–305. [Google Scholar] [CrossRef]
- Yaziji, N.; Martin, L.; Hillon, P.; Favre, J.P.; Henninger, J.F.; Piard, F. Cholangiocarcinoma arising from biliary micro-hamartomas in a man suffering from hemochromatosis. Ann. Pathol. 1997, 17, 346–349. [Google Scholar] [PubMed]
- Fernandez Pelaez, J.M.; Sanchez Martin, E.; Tirado Miranda, R.; Navarro Martinez, A.; Alamillo, S.A. Hemochromatosis and hilar cholangiocarcinoma: Report of a case. Rev. Esp. Enferm. Dig. 2000, 92, 474–475. [Google Scholar]
- Di Stefano, F.; Verna, N.; Balatsinou, L.; Schiavone, C.; Di Gioacchino, M. Genetic hemochromatosis with normal transferrin saturation in a man with cholangiocarcinoma and yellow nail syndrome. J. Gastroenterol. Hepatol. 2003, 18, 1221–1222. [Google Scholar] [CrossRef]
- Sulpice, L.; Rayar, M.; Boucher, E.; Pele, F.; Pracht, M.; Meunier, B.; Boudjema, K. Intrahepatic cholangiocarcinoma: Impact of genetic hemochromatosis on outcome and overall survival after surgical resection. J. Surg. Res. 2013, 180, 56–61. [Google Scholar] [CrossRef]
- Morcos, M.; Dubois, S.; Bralet, M.P.; Belghiti, J.; Degott, C.; Terris, B. Primary liver carcinoma in genetic hemochromatosis reveals a broad histologic spectrum. Am. J. Clin. Pathol. 2001, 116, 738–743. [Google Scholar] [CrossRef]
- Nkontchou, G.; Tran Van Nhieu, J.; Ziol, M.; Tengher, I.; Mahmoudi, A.; Roulot, D.; Bourcier, V.; Ganne Carrie, N.; Grando-Lemaire, V.; Trinchet, J.C.; et al. Peripheral intrahepatic cholangiocarcinoma occurring in patients without cirrhosis or chronic bile duct diseases: Epidemiology and histopathology of distant nontumoral liver in 57 White patients. Eur. J. Gastroenterol. Hepatol. 2013, 25, 94–98. [Google Scholar] [CrossRef]
- Pfeiffenberger, J.; Mogler, C.; Gotthardt, D.N.; Schulze-Bergkamen, H.; Litwin, T.; Reuner, U.; Hefter, H.; Huster, D.; Schemmer, P.; Członkowska, A.; et al. Hepatobiliary malignancies in Wilson disease. Liver Int. 2015, 35, 1615–1622. [Google Scholar] [CrossRef]
- Angele-Martinez, C.; Goodman, C.; Brumaghim, J. Metal-mediated DNA damage and cell death: Mechanisms, detection methods, and cellular consequences. Metallomics 2014, 6, 1358–1381. [Google Scholar] [CrossRef] [PubMed]
- Kamamoto, Y.; Makiura, S.; Sugihara, S.; Hiasa, Y.; Arai, M. The inhibitory effect of copper on DL-ethionine carcinogenesis in rats. Cancer Res. 1973, 33, 1129–1135. [Google Scholar]
- Wilkinson, M.L.; Portmann, B.; Williams, R. Wilson’s disease and hepatocellular carcinoma: Possible protective role of copper. Gut 1983, 24, 767–771. [Google Scholar] [CrossRef]
- Huai, J.P.; Ding, J.; Ye, X.H.; Chen, Y.P. Inflammatory bowel disease and risk of cholangiocarcinoma: Evidence from a meta-analysis of population-based studies. Asian Pac. J. Cancer Prev. 2014, 15, 3477–3482. [Google Scholar] [CrossRef] [PubMed]
- Axelrad, J.E.; Lichtiger, S.; Yajnik, V. Inflammatory bowel disease and cancer: The role of inflammation, immunosuppression, and cancer treatment. World J. Gastroenterol. 2016, 22, 4794–4801. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.; Li, J.V.; Athanasiou, T.; Ashrafian, H.; Nicholson, J.K. Understanding the role of gut microbiome-host metabolic signal disruption in health and disease. Trends Microbiol. 2011, 19, 349–359. [Google Scholar] [CrossRef]
- Saich, R.; Chapman, R. Primary sclerosing cholangitis, autoimmune hepatitis and overlap syndromes in inflammatory bowel disease. World J. Gastroenterol. 2008, 14, 331–337. [Google Scholar] [CrossRef]
- Sripa, B.; Kaewkes, S.; Sithithaworn, P.; Mairiang, E.; Laha, T.; Smout, M.; Pairojkul, C.; Bhudhisawasdi, V.; Tesana, S.; Thinkamrop, B.; et al. Liver fluke induces cholangiocarcinoma. PLoS Med. 2007, 4, e201. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.A. Helminths in the induction of cancer: Opisthorchis viverrini, Clonorchis sinensis and cholangiocarcinoma. Trop. Geogr. Med. 1980, 32, 95–100. [Google Scholar] [PubMed]
- Shin, H.R.; Oh, J.K.; Masuyer, E.; Curado, M.P.; Bouvard, V.; Fang, Y.Y.; Wiangnon, S.; Sripa, B.; Hong, S.T. Epidemiology of cholangiocarcinoma: An update focusing on risk factors. Cancer Sci. 2010, 101, 579–585. [Google Scholar] [CrossRef] [PubMed]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Biological agents. IARC Monogr. Eval. Carcinog. Risks Hum. 2012, 100B, 341–370. [Google Scholar]
- Shin, H.R.; Oh, J.K.; Lim, M.K.; Shin, A.; Kong, H.J.; Jung, K.W.; Won, Y.J.; Park, S.; Park, S.J.; Hong, S.T. Descriptive epidemiology of cholangiocarcinoma and clonorchiasis in Korea. J. Korean Med. Sci. 2010, 25, 1011–1016. [Google Scholar] [CrossRef]
- Sithithaworn, P.; Yongvanit, P.; Duenngai, K.; Kiatsopit, N.; Pairojkul, C. Roles of liver fluke infection as risk factor for cholangiocarcinoma. J. Hepatobiliary Pancreat. Sci. 2014, 21, 301–308. [Google Scholar] [CrossRef]
- Marahatta, S.B.; Punyarit, P.; Bhudisawasdi, V.; Paupairoj, A.; Wongkham, S.; Petmitr, S. Polymorphism of glutathione S-transferase omega gene and risk of cancer. Cancer Lett. 2006, 236, 276–281. [Google Scholar] [CrossRef]
- Songserm, N.; Promthet, S.; Sithithaworn, P.; Pientong, C.; Ekalaksananan, T.; Chopjitt, P.; Parkin, D.M. MTHFR polymorphisms and Opisthorchis viverrini infection: A relationship with increased susceptibility to cholangiocarcinoma in Thailand. Asian Pac. J. Cancer Prev. 2011, 12, 1341–1345. [Google Scholar]
- Petrick, J.L.; Campbell, P.T.; Koshiol, J.; Thistle, J.E.; Andreotti, G.; Beane-Freeman, L.E.; Buring, J.E.; Chan, A.T.; Chong, D.Q.; Doody, M.M.; et al. Tobacco, alcohol use and risk of hepatocellular carcinoma and intrahepatic cholangiocarcinoma: The liver cancer pooling project. Br. J. Cancer 2018, 118, 1005–1012. [Google Scholar] [CrossRef]
- Makiuchi, T.; Sobue, T.; Kitamura, T.; Sawada, N.; Iwasaki, M.; Yamaji, T.; Shimazu, T.; Inoue, M.; Tsugane, S. Smoking, Alcohol Consumption, and Risks for Biliary Tract Cancer and Intrahepatic Bile Duct Cancer. J. Epidemiol. 2019, 29, 180–186. [Google Scholar] [CrossRef]
- Zakhari, S. Overview: How is alcohol metabolized by the body? Alcohol. Res. Health 2006, 29, 245–254. [Google Scholar]
- Ye, X.H.; Huai, J.P.; Ding, J.; Chen, Y.P.; Sun, X.C. Smoking, alcohol consumption, and the risk of extrahepatic cholangiocarcinoma: A meta-analysis. World J. Gastroenterol. 2013, 19, 8780–8788. [Google Scholar] [CrossRef] [PubMed]
- Jinga, M.; Jurcuţ, C.; Vasilescu, F.; Becheanu, G.; Stancu, S.H.; Ciobaca, L.; Mircescu, G.; Jinga, V. A rare case of digestive hemorrhage in an elderly patient: Diagnosis and treatment difficulties. Rom. J. Morphol. Embryol. 2012, 53 (Suppl. S3), 831–834. [Google Scholar] [PubMed]
- Huang, Y.; You, L.; Xie, W.; Ning, L.; Lang, J. Smoking and risk of cholangiocarcinoma: A systematic review and meta-analysis. Oncotarget 2017, 8, 100570–100581. [Google Scholar] [CrossRef]
- Staretz, M.E.; Murphy, S.E.; Patten, C.J.; Nunes, M.G.; Koehl, W.; Amin, S.; Koenig, L.A.; Guengerich, F.P.; Hecht, S.S. Comparative metabolism of the tobacco-related carcinogens benzo[a]pyrene, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol, and N′-nitrosonornicotine in human hepatic microsomes. Drug Metab. Dispos. 1997, 25, 154–162. [Google Scholar]
- Park, J.H.; Hong, J.Y.; Han, K. Association between Smoking Cessation and the Risk of Cholangiocarcinoma and Ampulla of Vater Cancer: A Nationwide Cohort Study. Liver Cancer 2023, 12, 457–466. [Google Scholar] [CrossRef]
- Granata, S.; Vivarelli, F.; Morosini, C.; Canistro, D.; Paolini, M.; Fairclough, L.C. Toxicological Aspects Associated with Consumption from Electronic Nicotine Delivery System (ENDS): Focus on Heavy Metals Exposure and Cancer Risk. Int. J. Mol. Sci. 2024, 25, 2737. [Google Scholar] [CrossRef]
- Gallagher, K.P.; Vargas, P.A.; Santos-Silva, A.R. The use of E-cigarettes as a risk factor for oral potentially malignant disorders and oral cancer: A rapid review of clinical evidence. Med. Oral. Patol. Oral. Cir. Bucal 2024, 29, e18–e26. [Google Scholar] [CrossRef] [PubMed]
- Muthumalage, T.; Noel, A.; Thanavala, Y.; Alcheva, A.; Rahman, I. Challenges in current inhalable tobacco toxicity assessment models: A narrative review. Tob. Induc. Dis. 2024, 22, 102. [Google Scholar] [CrossRef]
- de Martel, C.; Plummer, M.; Franceschi, S. Cholangiocarcinoma: Descriptive epidemiology and risk factors. Gastroenterol. Clin. Biol. 2010, 34, 173–180. [Google Scholar] [CrossRef]
- Yamamoto, Y.; Chikawa, J.; Uegaki, Y.; Usuda, N.; Kuwahara, Y.; Fukumoto, M. Histological type of Thorotrast-induced liver tumors associated with the translocation of deposited radionuclides. Cancer Sci. 2010, 101, 336–340. [Google Scholar] [CrossRef]
- Khan, S.A.; Toledano, M.B.; Taylor-Robinson, S.D. Epidemiology, risk factors, and pathogenesis of cholangiocarcinoma. HPB 2008, 10, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.T.; Lin, Y.J.; Li, C.Y.; Tsai, P.J.; Yang, C.Y.; Liou, S.H.; Wu, T.N. Cancer attributable to asbestos exposure in shipbreaking workers: A matched-cohort study. PLoS ONE 2015, 10, e0133128. [Google Scholar] [CrossRef]
- Boulanger, M.; Morlais, F.; Bouvier, V.; Galateau-Salle, F.; Guittet, L.; Marquignon, M.F.; Paris, C.; Raffaelli, C.; Launoy, G.; Clin, B. Digestive cancers and occupational asbestos exposure: Incidence study in a cohort of asbestos plant workers. Occup. Environ. Med. 2015, 72, 792–797. [Google Scholar] [CrossRef]
- Brandi, G.; Di Girolamo, S.; Farioli, A.; de Rosa, F.; Curti, S.; Pinna, A.D.; Ercolani, G.; Violante, F.S.; Biasco, G.; Mattioli, S. Asbestos: A hidden player behind the cholangiocarcinoma increase? Findings from a case-control analysis. Cancer Causes Control 2013, 24, 911–918. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, H.; Park, J.S. Beyond the Bile: Exploring the Microbiome and Metabolites in Cholangiocarcinoma. Life 2024, 14, 698. [Google Scholar] [CrossRef] [PubMed]
- Kerdkumthong, K.; Nanarong, S.; Roytrakul, S.; Pitakpornpreecha, T.; Tantimetta, P.; Runsaeng, P.; Obchoei, S. Quantitative proteomics analysis reveals possible anticancer mechanisms of 5′-deoxy-5′-methylthioadenosine in cholangiocarcinoma cells. PLoS ONE 2024, 19, e0306060. [Google Scholar] [CrossRef]
- Deng, S.; Lu, X.; Wang, X.; Liang, B.; Xu, H.; Yang, D.; Cui, G.; Yonemura, A.; Paine, H.; Zhou, Y.; et al. Overexpression of TBX3 suppresses tumorigenesis in experimental and human cholangiocarcinoma. Cell Death Dis. 2024, 15, 441. [Google Scholar] [CrossRef]
- Prabhakar, N.; Chiang, H.; Nabrinsky, E.; Eklund, J. Report of Cholangiocarcinoma with Transheterozygous BRCA1 and BRCA2 Co-mutation. Cureus 2024, 16, e60767. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhou, J.; Zhai, D.; Jiang, Q.; Yang, M.; Zhou, M. Gut microbiota regulates the ALK5/NOX1 axis by altering glutamine metabolism to inhibit ferroptosis of intrahepatic cholangiocarcinoma cells. Biochim. Biophys. Acta Mol. Basis Dis. 2024, 1870, 167152. [Google Scholar] [CrossRef]
- Zenoaga-Barbăroșie, C.; Berca, L.; Vassu-Dimov, T.; Toma, M.; Nica, M.I.; Alexiu-Toma, O.A.; Ciornei, C.; Albu, A.; Nica, S.; Nistor, C.; et al. The Predisposition for Type 2 Diabetes Mellitus and Metabolic Syndrome. Balkan J. Med. Genet. 2023, 26, 21–26. [Google Scholar] [CrossRef]
- Anghel, D.; Ciobîcă, L.M.; Stanciu, S.M.; Jurcuț, C.V.; Stoicescu, G.D.; Răduță, I.A.; Coca, A. Ankylosing spondylitis and cardiovascular risk—Case report. Rom. J. Mil. Med. 2016, 119, 39–42. [Google Scholar]
- Ionescu, O.P.; Stanciu, S.M.; Ciobîcă, M.L. Atherosclerosis in rheumatoid arthritis—The importance of imaging testing. Rom. J. Mil. Med. 2020, 123, 26–31. [Google Scholar]
- Zeng, L.; You, G.; Tanaka, H.; Srivatanakul, P.; Ohta, E.; Viwatthanasittiphong, C.; Matharit, M.; Chenvidhya, D.; Jedpiyawongse, A.; Tanaka, M.; et al. Combined effects of polymorphisms of DNA-repair protein genes and metabolic enzyme genes on the risk of cholangiocarcinoma. Jpn. J. Clin. Oncol. 2013, 43, 1190–1194. [Google Scholar] [CrossRef] [PubMed]
- Ko, K.H.; Kim, N.K.; Yim, D.J.; Hong, S.P.; Park, P.W.; Rim, K.S.; Kim, S.; Hwang, S.G. Polymorphisms of 5,10-methylenetetrahydrofolate reductase (MTHFR C677T) and thymidylate synthase enhancer region (TSER) as a risk factor of cholangiocarcinoma in a Korean population. Anticancer Res. 2006, 26, 4229–4233. [Google Scholar]
- Kinoshita, M.; Kubo, S.; Tanaka, S.; Takemura, S.; Nishioka, T.; Hamano, G.; Ito, T.; Tanaka, S.; Ohsawa, M.; Shibata, T. The association between non-alcoholic steatohepatitis and intrahepatic cholangiocarcinoma: A hospital based case-control study. J. Surg. Oncol. 2016, 113, 779–783. [Google Scholar] [CrossRef]
- Wongjarupong, N.; Assavapongpaiboon, B.; Susantitaphong, P.; Cheungpasitporn, W.; Treeprasertsuk, S.; Rerknimitr, R.; Chaiteerakij, R. Non-alcoholic fatty liver disease as a risk factor for cholangiocarcinoma: A systematic review and meta-analysis. BMC Gastroenterol. 2017, 17, 149. [Google Scholar] [CrossRef]
- De Lorenzo, S.; Tovoli, F.; Mazzotta, A.; Vasuri, F.; Edeline, J.; Malvi, D.; Boudjema, K.; Renzulli, M.; Jeddou, H.; D'Errico, A.; et al. Non-Alcoholic Steatohepatitis as a Risk Factor for Intrahepatic Cholangiocarcinoma and Its Prognostic Role. Cancers 2020, 12, 3182. [Google Scholar] [CrossRef]
- Parsi, M.A. Obesity and cholangiocarcinoma. World J. Gastroenterol. 2013, 19, 457–462. [Google Scholar] [CrossRef]
- Ciobîcă, L.M.; Sârbu, I.; Stanciu, S.M.; Coca, A. Behçet disease—Case presentation. Rom. J. Mil. Med. 2016, 119, 43–46. [Google Scholar] [CrossRef]
- Li, J.S.; Han, T.J.; Jing, N.; Li, L.; Zhang, X.H.; Ma, F.Z.; Liu, J.Y. Obesity and the risk of cholangiocarcinoma: A meta-analysis. Tumour Biol. 2014, 35, 6831–6838. [Google Scholar] [CrossRef]
- Pati, S.; Irfan, W.; Jameel, A.; Ahmed, S.; Shahid, R.K. Obesity and Cancer: A Current Overview of Epidemiology, Pathogenesis, Outcomes, and Management. Cancers 2023, 15, 485. [Google Scholar] [CrossRef]
- Jing, W.; Jin, G.; Zhou, X.; Zhou, Y.; Zhang, Y.; Shao, C.; Liu, R.; Hu, X. Diabetes mellitus and increased risk of cholangiocarcinoma: A meta-analysis. Eur. J. Cancer Prev. 2012, 21, 24–31. [Google Scholar] [CrossRef]
- Chaiteerakij, R.; Yang, J.D.; Harmsen, W.S.; Slettedahl, S.W.; Mettler, T.A.; Fredericksen, Z.S.; Kim, W.R.; Gores, G.J.; Roberts, R.O.; Olson, J.E.; et al. Risk factors for intrahepatic cholangiocarcinoma: Association between metformin use and reduced cancer risk. Hepatology 2013, 57, 648–655. [Google Scholar] [CrossRef]
- Tsilidis, K.K.; Kasimis, J.C.; Lopez, D.S.; Ntzani, E.E.; Ioannidis, J.P.A. Type 2 diabetes and cancer: Umbrella review of meta-analyses of observational studies. BMJ 2015, 350, g7607. [Google Scholar] [CrossRef]
- Rahman, S.U.; Sana, M.K.; Tahir, Z.; Ali, A.; Shah, P.A. Paraneoplastic syndromes in cholangiocarcinoma. World J. Hepatol. 2020, 12, 897–907. [Google Scholar] [CrossRef]
- Zhou, H.; Hylemon, P.B. Bile acids are nutrient signaling hormones. Steroids 2014, 86, 62–68. [Google Scholar] [CrossRef]
- Casadei-Gardini, A.; Filippi, R.; Rimini, M.; Rapposelli, I.G.; Fornaro, L.; Silvestris, N.; Aldrighetti, L.; Aimar, G.; Rovesti, G.; Bartolini, G.; et al. Effects of Metformin and Vitamin D on Clinical Outcome in Cholangiocarcinoma Patients. Oncology 2021, 99, 292–299. [Google Scholar] [CrossRef]
- Powała, A.; Żołek, T.; Brown, G.; Kutner, A. Structure and the Anticancer Activity of Vitamin D Receptor Agonists. Int. J. Mol. Sci. 2024, 25, 6624. [Google Scholar] [CrossRef]
- Zhao, S.; Qian, F.; Wan, Z.; Chen, X.; Pan, A.; Liu, G. Vitamin D and major chronic diseases. Trends Endocrinol. Metab. 2024; online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Bird, R.P. Vitamin D and cancer. Adv. Food Nutr. Res. 2024, 109, 92–159. [Google Scholar] [CrossRef]
- Chiang, K.C.; Yeh, C.N.; Lin, K.J.; Su, L.J.; Yen, T.C.; Pang, J.H.; Kittaka, A.; Sun, C.C.; Chen, M.F.; Jan, Y.Y.; et al. Chemopreventive and chemotherapeutic effect of dietary supplementation of vitamin D on cholangiocarcinoma in a Chemical-Induced animal model. Oncotarget 2014, 5, 3849–3861. [Google Scholar] [CrossRef]
- Kennedy, L.; Baker, K.; Hodges, K.; Graf, A.; Venter, J.; Hargrove, L.; Harris, R.; Harnish, E.; Meng, F.; Francis, H. Dysregulation of vitamin D3 synthesis leads to enhanced cholangiocarcinoma growth. Dig. Liver Dis. 2013, 45, 316–322. [Google Scholar] [CrossRef]
- Sookprasert, A.; Pugkhem, A.; Khuntikeo, N.; Chur-in, S.; Chamadol, N.; Prawan, A.; Janeklang, S.; Vaeteewoottacharn, K.; Kukongviriyapan, V.; Pairojkul, C.; et al. Evaluation of efficacy, safety and tolerability of high dose-intermittent calcitriol supplementation to advanced intrahepatic cholangiocarcinoma patients-a pilot study. Asian Pac. J. Cancer Prev. 2012, 13, 161–167. [Google Scholar]
- Chiang, K.C.; Yeh, T.S.; Huang, C.C.; Chang, Y.C.; Juang, H.H.; Cheng, C.T.; Pang, J.S.; Hsu, J.T.; Takano, M.; Chen, T.C.; et al. MART-10 represses cholangiocarcinoma cell growth and high vitamin D receptor expression indicates better prognosis for cholangiocarcinoma. Sci. Rep. 2017, 7, 43773. [Google Scholar] [CrossRef] [PubMed]
- Chiang, K.C.; Yeh, C.N.; Huang, C.C.; Yeh, T.S.; SPang, J.H.; Hsu, J.T.; Chen, L.W.; Kuo, S.F.; Kittaka, A.; Chen, T.C.; et al. 25(OH)D Is Effective to Repress Human Cholangiocarcinoma Cell Growth through the Conversion of 25(OH)D to 1alpha,25(OH)2D3. Int. J. Mol. Sci. 2016, 17, 1326. [Google Scholar] [CrossRef]
- Trakoonsenathong, R.; Kunprom, W.; Aphivatanasiri, C.; Yueangchantuek, P.; Pimkeeree, P.; Sorin, S.; Khawkhiaw, K.; Chiu, C.F.; Okada, S.; Wongkham, S.; et al. Liraglutide exhibits potential anti-tumor effects on the progression of intrahepatic cholangiocarcinoma, in vitro and in vivo. Sci. Rep. 2024, 14, 13726. [Google Scholar] [CrossRef]
- Ueda, P.; Wintzell, V.; Melbye, M.; Eliasson, B.; Svensson, A.M.; Franzén, S.; Gudbjörnsdottir, S.; Hveem, K.; Jonasson, C.; Svanström, H.; et al. Use of incretin-based drugs and risk of cholangiocarcinoma: Scandinavian cohort study. Diabetologia 2021, 64, 2204–2214. [Google Scholar] [CrossRef]
- Huber, S.; Fitzner, T.; Feichtinger, R.G.; Hochmann, S.; Kraus, T.; Sotlar, K.; Kofler, B.; Varga, M. Galanin System in the Human Bile Duct and Perihilar Cholangiocarcinoma. Cells 2023, 12, 1678. [Google Scholar] [CrossRef]
- Petrescu, A.D.; Grant, S.; Williams, E.; Frampton, G.; Parks, N.; Blaney, H.; Davies, M.; John, R.; Reinhart, E.H.; McMillin, M.; et al. Coordinated Targeting of Galanin Receptors on Cholangiocytes and Hepatic Stellate Cells Ameliorates Liver Fibrosis in Multidrug Resistance Protein 2 Knockout Mice. Am. J. Pathol. 2020, 190, 586–601. [Google Scholar] [CrossRef] [PubMed]
- Falkenstetter, S.; Leitner, J.; Brunner, S.M.; Rieder, T.N.; Kofler, B.; Weis, S. Galanin System in Human Glioma and Pituitary Adenoma. Front. Endocrinol. 2020, 11, 155. [Google Scholar] [CrossRef] [PubMed]
- Sandru, F.; Carsote, M.; Dumitrascu, M.C.; Albu, S.E.; Valea, A. Glucocorticoids and Trabecular Bone Score. J. Med. Life 2020, 13, 449–453. [Google Scholar] [CrossRef]
- Nistor, C.E.; Ciuche, A.; Cucu, A.P.; Serban, B.; Cursaru, A.; Cretu, B.; Cirstoiu, C. Clavicular Malignancies: A Borderline Surgical Management. Medicina 2022, 58, 910. [Google Scholar] [CrossRef]
- Carsote, M.; Valea, A.; Dumitru, N.; Terzea, D.; Petrova, E.; Albu, S.; Buruiana, A.; Ghemigian, A. Metastases in daily endocrine practice. Arch. Balk. Med. Union. 2016, 51, 476–480. [Google Scholar]
- Rubino, J.G.; Flemming, J.A. Menopausal hormone therapy and risk of biliary tract cancers: Addressing the ant, not the elephant in the room. Hepatology 2022, 75, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Kamani, M.; Akgor, U.; Gültekin, M. Review of the literature on combined oral contraceptives and cancer. Ecancermedicalscience 2022, 16, 1416. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Jiang, L.; Li, F.; Li, Q.; Yuan, S.; Huang, S.; Fu, Y.; Yan, X.; Chen, J.; Li, H.; et al. The epidemiological trends of biliary tract cancers in the United States of America. BMC Gastroenterol. 2022, 22, 546. [Google Scholar] [CrossRef]
- Zhang, G.Q.; Chen, J.L.; Luo, Y.; Mathur, M.B.; Anagnostis, P.; Nurmatov, U.; Talibov, M.; Zhang, J.; Hawrylowicz, C.M.; Lumsden, M.A.; et al. Menopausal hormone therapy and women’s health: An umbrella review. PLoS Med. 2021, 18, e1003731. [Google Scholar] [CrossRef]
- Li, F.; Chen, Q.; Yang, Y.; Li, M.; Zhang, L.; Yan, Z.; Zhang, J.; Wang, K. ESR1 as a recurrence-related gene in intrahepatic cholangiocarcinoma: A weighted gene coexpression network analysis. Cancer Cell Int. 2021, 21, 225. [Google Scholar] [CrossRef]
- Kaewlert, W.; Sakonsinsiri, C.; Namwat, N.; Sawanyawisuth, K.; Ungarreevittaya, P.; Khuntikeo, N.; Armartmuntree, N.; Thanan, R. The Importance of CYP19A1 in Estrogen Receptor-Positive Cholangiocarcinoma. Horm. Cancer 2018, 9, 408–419. [Google Scholar] [CrossRef]
- Lu, C.; Miao, J.; Li, M.; Zheng, Q.; Xu, F.; Pan, Y.; Wang, Y.; Yang, Z.; Xia, X.; Zhu, H.; et al. Characterization of the Estrogen Response Helps to Predict Prognosis and Identify Potential Therapeutic Targets in Cholangiocarcinoma. Front. Oncol. 2022, 12, 870840. [Google Scholar] [CrossRef]
- Jackson, S.S.; Pfeiffer, R.M.; Gabbi, C.; Anderson, L.; Gadalla, S.M.; Koshiol, J. Menopausal hormone therapy and risk of biliary tract cancers. Hepatology 2022, 75, 309–321. [Google Scholar] [CrossRef]
- Petrick, J.L.; McMenamin, Ú.C.; Zhang, X.; Zeleniuch-Jacquotte, A.; Wactawski-Wende, J.; Simon, T.G.; Sinha, R.; Sesso, H.D.; Schairer, C.; Rosenberg, L.; et al. Exogenous hormone use, reproductive factors and risk of intrahepatic cholangiocarcinoma among women: Results from cohort studies in the Liver Cancer Pooling Project and the UK Biobank. Br. J. Cancer 2020, 123, 316–324. [Google Scholar] [CrossRef]
- Khalid, S.; Laput, G.; Khorfan, K.; Roytman, M. Development of Liver Cancers as an Unexpected Consequence of Anabolic Androgenic Steroid Use. Cureus 2023, 15, e34357. [Google Scholar] [CrossRef] [PubMed]
- Pothuri, V.S.; Anzelmo, M.; Gallaher, E.; Ogunlana, Y.; Aliabadi-Wahle, S.; Tan, B.; Crippin, J.S.; Hammill, C.W. Transgender Males on Gender-Affirming Hormone Therapy and Hepatobiliary Neoplasms: A Systematic Review. Endocr. Pract. 2023, 29, 822–829. [Google Scholar] [CrossRef] [PubMed]
- Fadahunsi, O.O.; Ibitoye, B.O.; Adisa, A.O.; Alatise, O.I.; Adetiloye, V.A.; Idowu, B.M. Diagnostic accuracy of ultrasonography in adults with obstructive jaundice. J. Ultrason. 2020, 20, e100–e105. [Google Scholar] [CrossRef]
- Costa, M.; Valente, A.; Freire Coelho, A.; Meireles, S.; Barbosa, M. Acanthosis Nigricans Manifesting as a Paraneoplastic Syndrome Associated With Cholangiocarcinoma. Cureus 2023, 15, e35853. [Google Scholar] [CrossRef]
- Suchonwanit, P.; McMichael, A.J. Alopecia in Association with Malignancy: A Review. Am. J. Clin. Dermatol. 2018, 19, 853–865. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, E.; Paraskeva, P.; Smyrnis, A.; Konstantopoulos, K. Alopecia: A common paraneoplastic manifestation of cholangiocarcinoma in humans and animals. BMJ Case Rep. 2012, 2012, bcr2012006217. [Google Scholar] [CrossRef]
- Ciobîcă, M.L.; Ionescu, O.P.; Săndulescu, B.A. Osteoporosis and the fracture risk in systemic lupus erythematosus. Rom. J. Mil. Med. 2020, 123, 341–347. [Google Scholar]
- Suh, K.J.; Park, J.K.; Cho, S.; Park, H.; Baek, H.W.; Lee, K.; Lee, D.S.; Lee, K.H. Dermatomyositis in a Patient with Cholangiocarcinoma Detected by an [(18)F]-Fluorodeoxyglucose Positron Emission Tomography-Computed Tomography Scan. Cancer Res. Treat. 2016, 48, 848–852. [Google Scholar] [CrossRef] [PubMed]
- Nistor, C.E.; Staden, R.S.; Dumitru, A.V.; Stanciu Găvan, C. A Screening Test for Early Diagnosis of Microcellular Bronchopulmonary Cancer-Pilot Study. J. Clin. Med. 2019, 9, 76. [Google Scholar] [CrossRef]
- Sotoodian, B.; Mahmood, M.N.; Salopek, T.G. Clinical and Dermoscopic Features of Pigmented Disseminated Superficial Actinic Porokeratosis: Case Report and Literature Review. J. Cutan. Med. Surg. 2018, 22, 229–231. [Google Scholar] [CrossRef] [PubMed]
- Chiyomaru, K.; Takai, T.; Ohashi, A.; Nishigori, C. Necrolytic migratory erythema with cholangiocarcinoma: Pseudoglucagonoma syndrome. Eur. J. Dermatol. 2010, 20, 238–239. [Google Scholar] [CrossRef]
- Tzovaras, V.; Liberopoulos, E.N.; Zioga, A.; Pavlidis, N.; Elisaf, M. Persistent erythema multiforme in a patient with extrahepatic cholangiocarcinoma. Oncology 2007, 73, 127–129. [Google Scholar] [CrossRef] [PubMed]
- Nistor, C.E.; Ciuche, A.; Cucu, A.P.; Nitipir, C.; Slavu, C.; Serban, B.; Cursaru, A.; Cretu, B.; Cirstoiu, C. Management of Lung Cancer Presenting with Solitary Bone Metastasis. Medicina 2022, 58, 1463. [Google Scholar] [CrossRef]
- Chacko, A.M.; Carrero, G.; Akhouri, S. A Case Report of Erythema Multiforme Secondary to Atorvastatin Use. Cureus 2024, 16, e52175. [Google Scholar] [CrossRef]
- Cohen, P.R.; Holder, W.R.; Tucker, S.B.; Kono, S.; Kurzrock, R. Sweet syndrome in patients with solid tumors. Cancer 1993, 72, 2723–2731. [Google Scholar] [CrossRef]
- Shinojima, Y.; Toma, Y.; Terui, T. Sweet syndrome associated with intrahepatic cholangiocarcinoma producing granulocyte colony-stimulating factor. Br. J. Dermatol. 2006, 155, 1103–1104. [Google Scholar] [CrossRef]
- Lemaire, C.C.; Portilho, A.L.C.; Pinheiro, L.V.; Vivas, R.A.; Britto, M.; Montenegro, M.; Rodrigues, L.F.F.; Arruda, S.; Lyra, A.C.; Cavalcante, L.N. Sweet syndrome as a paraneoplastic manifestation of cholangiocarcinoma: A case report. World J. Clin. Cases 2020, 8, 4122–4127. [Google Scholar] [CrossRef]
- Holzgruber, J.; Oberneder-Popper, J.; Guenova, E.; Hötzenecker, W. Acrokeratosis Paraneoplastica (Bazex Syndrome): A Case Report. Case Rep. Dermatol. 2022, 14, 307–312. [Google Scholar] [CrossRef]
- Ciuche, A.; Nistor, C.; Motaş, C.; Horvat, T. Minimally invasive surgery in the treatment of malignant pleuro-pericardial effusions. Chirurgia 2012, 107, 206–212. [Google Scholar] [PubMed]
- Stone, S.P.; Buescher, L.S. Life-threatening paraneoplastic cutaneous syndromes. Clin. Dermatol. 2005, 23, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Boyd, A.S.; Neldner, K.H.; Menter, A. Erythema gyratum repens: A paraneoplastic eruption. J. Am. Acad. Dermatol. 1992, 26 Pt 1, 757–762. [Google Scholar] [CrossRef] [PubMed]
- Nistor, C.E.; Găvan, C.S.; Ciritel, A.A.; Nemes, A.F.; Ciuche, A. The Association of Minimally Invasive Surgical Approaches and Mortality in Patients with Malignant Pleuropericarditis-A 10 Year Retrospective Observational Study. Medicina 2022, 58, 718. [Google Scholar] [CrossRef]
- Liau, M.M.; Long, V.; Yang, S.S. Erythema gyratum repens: A paraneoplastic eruption. BMJ Case Rep. 2016, 2016, bcr2016214665. [Google Scholar] [CrossRef]
- Bar-Ilan, E.; Gat, A.; Sprecher, E.; Zeeli, T. Paraneoplastic pityriasis rubra pilaris: Case report and literature review. Clin. Exp. Dermatol. 2017, 42, 54–57. [Google Scholar] [CrossRef]
- Opneja, A.; Mahajan, S.; Kapoor, S.; Marur, S.; Yang, S.H.; Manno, R. Unusual Paraneoplastic Presentation of Cholangiocarcinoma. Case Rep. Med. 2015, 2015, 806835. [Google Scholar] [CrossRef]
- Morgenthau, A.; Almudaires, A. Klatskin's cholangiocarcinoma presenting with the sign of Leser-Trelat. BMJ Case Rep. 2019, 12, e232507. [Google Scholar] [CrossRef]
- Scully, C.; Barrett, W.A.; Gilkes, J.; Rees, M.; Sarner, M.; Southcott, R.J. Oral acanthosis nigricans, the sign of Leser-Trélat and cholangiocarcinoma. Br. J. Dermatol. 2001, 145, 506–507. [Google Scholar] [CrossRef]
- Sökmen, M.; Demirsoy, H.; Ersoy, O.; Gökdemir, G.; Akbayir, N.; Karaca, C.; Ozdil, K.; Kesici, B.; Calişkan, C.; Yilmaz, B. Paraneoplastic porphyria cutanea tarda associated with cholangiocarcinoma: Case report. Turk. J. Gastroenterol. 2007, 18, 200–205. [Google Scholar] [PubMed]
- Schmidt, S.L.; Schmidt, J.J.; Tolentino, J.C.; Ferreira, C.G.; de Almeida, S.A.; Alvarenga, R.P.; Simoes, E.N.; Schmidt, G.J.; Canedo, N.H.; Chimelli, L. Cholangiocarcinoma associated with limbic encephalitis and early cerebral abnormalities detected by 2-deoxy-2-[fluorine-18]fluoro-D-glucose integrated with computed tomography-positron emission tomography: A case report. J. Med. Case Rep. 2016, 10, 200. [Google Scholar] [CrossRef]
- Bruhnding, A.; Notch, D.; Beard, A. Anti-Yo positive paraneoplastic cerebellar degeneration in the setting of cholangiocarcinoma. J. Clin. Neurosci. 2017, 36, 71–72. [Google Scholar] [CrossRef]
- Normand, G.; Jolivot, A.; Rabeyrin, M.; Hervieu, V.; Valette, P.J.; Scoazec, J.Y.; Gougon, J.M.; Juillard, L.; Dumortier, J. Paraneoplastic fibrillary glomerulonephritis associated with intrahepatic cholangiocarcinoma: When diagnosis of a rare kidney disease leads to successful hepatic cancer treatment. Clin. Res. Hepatol. Gastroenterol. 2017, 41, e8–e11. [Google Scholar] [CrossRef] [PubMed]
- Solans-Laqué, R.; Bosch-Gil, J.A.; Pérez-Bocanegra, C.; Selva-O'Callaghan, A.; Simeón-Aznar, C.P.; Vilardell-Tarres, M. Paraneoplastic vasculitis in patients with solid tumors: Report of 15 cases. J. Rheumatol. 2008, 35, 294–304. [Google Scholar]
- Hatzis, G.S.; Papachristodoulou, A.; Delladetsima, I.K.; Moutsopoulos, H.M. Polyarteritis nodosa associated with cholangiocarcinoma. Lupus 1998, 7, 301–306. [Google Scholar] [CrossRef]
- Horsted, F.; West, J.; Grainge, M.J. Risk of venous thromboembolism in patients with cancer: A systematic review and meta-analysis. PLoS Med. 2012, 9, e1001275. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.K.; Kim, D.U.; Baek, D.H.; Ha, D.W.; Lee, B.E.; Ryu, D.Y.; Cheong, J.H.; Kim, G.H.; Song, G.A.; Jang, A.L. Venous thromboembolism in patients with cholangiocarcinoma: Focus on risk factors and impact on survival. Eur. J. Gastroenterol. Hepatol. 2012, 24, 444–449. [Google Scholar] [CrossRef]
- Blum, M.F.; Ma, V.Y.; Betbadal, A.M.; Bonomo, R.A.; Raju, R.R.; Packer, C.D. Trousseau's Syndrome in Cholangiocarcinoma: The Risk of Making the Diagnosis. Clin. Med. Res. 2016, 14, 53–59. [Google Scholar] [CrossRef]
- Zahidin, M.A.; Iberahim, S.; Hassan, M.N.; Zulkafli, Z.; Mohd Noor, N.H. Clinical and Laboratory Diagnosis of Antiphospholipid Syndrome: A Review. Cureus 2024, 16, e61713. [Google Scholar] [CrossRef]
- Samadian, S.; Estcourt, L. Recurrent thrombo-embolic episodes: The association of cholangiocarcinoma with antiphospholipid syndrome. Postgrad. Med. J. 1999, 75, 45–46. [Google Scholar] [CrossRef]
- Ham, H.; Kim, H.Y.; Seo, K.J.; Lee, S.L.; Kim, C.W. Cholangiocarcinoma with a paraneoplastic leukemoid reaction mimicking a pyogenic liver abscess. Korean J. Intern. Med. 2015, 30, 110–113. [Google Scholar] [CrossRef]
- Sohda, T.; Shiga, H.; Nakane, H.; Watanabe, H.; Takeshita, M.; Sakisaka, S. Cholangiocellular carcinoma that produced both granulocyte-colony-stimulating factor and parathyroid hormone-related protein. Int. J. Clin. Oncol. 2006, 11, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Xi, L.F.; Jin, Y.; Li, J.T. Intrahepatic sarcomatoid cholangiocarcinoma: A case report of the youngest patient on record and a review of the condition's characteristics. Front. Surg. 2022, 9, 963952. [Google Scholar] [CrossRef] [PubMed]
- Raza, A.; Houk, L.; Yousaf, W.; Smiley, D.; Coberly, L. Unusual para-neoplastic manifestation of cholangiocarcinoma. J. Gastrointest. Cancer 2013, 44, 228–230. [Google Scholar] [CrossRef] [PubMed]
- González Amores, Y.; Hernando Rebollar, S.; Casado Bernabeu, A. Lupus as a paraneoplastic manifestation of cholangiocarcinoma. Rev. Esp. Enferm. Dig. 2016, 108, 292. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.; McPherson, T. Paraneoplastic subacute cutaneous lupus erythematosus associated with cholangiocarcinoma. Australas. J. Dermatol. 2016, 57, e5–e7. [Google Scholar] [CrossRef]
- Erdinc, B.; Ramachandran, P.; Yadav, R.; Sahni, S.; Joseph, G. Cholangiocarcinoma Presenting as Humoral Hypercalcemia of Malignancy: A Case Report and Literature Review. Cureus 2019, 11, e6481. [Google Scholar] [CrossRef]
- Harsch, I.A.; Konturek, P.C. Humoral Hypercalcemia in a Patient with Cholangiocellular Carcinoma—Effective Therapy with Denosumab. Am. J. Case Rep. 2019, 20, 1325–1330. [Google Scholar] [CrossRef]
- Ozawa, N.; Doi, S.; Tsujikawa, T.; Mabuchi, M.; Kajiyama, Y.; Sato, K.; Kikuchi, K.; Takahashi, M.; Kawamoto, M.; Yasuda, I. Intrahepatic cholangiocarcinoma producing granulocyte colony-stimulating factor and parathyroid hormone-related protein. Nihon Shokakibyo Gakkai Zasshi 2017, 114, 1285–1292. [Google Scholar]
- Chauhan, A.; Likasitwatanakul, P.; Ahmed, A.; Sibley, S.D. A Case of Fibroblast Growth Factor Receptor Fusion-Positive Intrahepatic Cholangiocarcinoma With Humoral Hypercalcemia of Malignancy. Cureus 2024, 16, e58741. [Google Scholar] [CrossRef]
- Meegada, S.; Eisen, R.; Coons, G.; Verma, R. Intrahepatic Cholangiocarcinoma Associated with High Procalcitonin, Hypercalcemia, Polycythemia and Leukocytosis. Cureus 2020, 12, e6587. [Google Scholar] [CrossRef] [PubMed]
- Baiocchi, L.; Sato, K.; Ekser, B.; Kennedy, L.; Francis, H.; Ceci, L.; Lenci, I.; Alvaro, D.; Franchitto, A.; Onori, P.; et al. Cholangiocarcinoma: Bridging the translational gap from preclinical to clinical development and implications for future therapy. Expert. Opin. Investig. Drugs 2021, 30, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Joo, I.; Lee, J.M.; Yoon, J.H. Imaging Diagnosis of Intrahepatic and Perihilar Cholangiocarcinoma: Recent Advances and Challenges. Radiology 2018, 288, 7–13. [Google Scholar] [CrossRef]
- Razumilava, N.; Gores, G.J.; Lindor, K.D. Cancer surveillance in patients with primary sclerosing cholangitis. Hepatology 2011, 54, 1842–1852. [Google Scholar] [CrossRef]
- Liu, G.J.; Wang, W.; Lu, M.D.; Xie, X.Y.; Xu, H.X.; Xu, Z.F.; Chen, L.D.; Wang, Z.; Liang, J.Y.; Huang, Y.; et al. Contrast-Enhanced Ultrasound for the Characterization of Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma. Liver Cancer 2015, 4, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Olthof, S.C.; Othman, A.; Clasen, S.; Schraml, C.; Nikolaou, K.; Bongers, M. Imaging of Cholangiocarcinoma. Visc. Med. 2016, 32, 402–410. [Google Scholar] [CrossRef]
- Pfrepper, C. Paraneoplastic Thromboembolism and Thrombophilia: Significance in Visceral Medicine. Visc. Med. 2020, 36, 280–287. [Google Scholar] [CrossRef]
- Tai, N.; Inoue, D. Bone and calcium metabolism associated with malignancy. Malignancy-associated hypercalcemia. Clin. Calcium 2018, 28, 1503–1508. [Google Scholar]
- Nistor, C.E.; Stanciu-Găvan, C.; Vasilescu, F.; Dumitru, A.V.; Ciuche, A. Attitude of the surgical approach in hyperparathyroidism: A retrospective study. Exp. Ther. Med. 2021, 22, 959. [Google Scholar] [CrossRef]
- Ashihara, N.; Nakajima, K.; Nakamura, Y.; Kobayashi, M.; Shirahata, K.; Maeda, C.; Uehara, T.; Gomi, D.; Ito, N. Denosumab is Effective for Controlling Serum Calcium Levels in Patients with Humoral Hypercalcemia of Malignancy Syndrome: A Case Report on Parathyroid Hormone-related Protein-producing Cholangiocarcinoma. Intern. Med. 2016, 55, 3453–3457. [Google Scholar] [CrossRef]
- Tang, J.; Liao, Y.; He, S.; Shi, J.; Peng, L.; Xu, X.; Xie, F.; Diao, N.; Huang, J.; Xie, Q.; et al. Autocrine parathyroid hormone-like hormone promotes intrahepatic cholangiocarcinoma cell proliferation via increased ERK/JNK-ATF2-cyclinD1 signaling. J. Transl. Med. 2017, 15, 238. [Google Scholar] [CrossRef] [PubMed]
- Kane, J.F.; Johnson, R.W. e-Evaluating the Role of PTHrP in Breast Cancer. Cancers 2023, 15, 2670. [Google Scholar] [CrossRef] [PubMed]
- Mc Donald, D.; Drake, M.T.; Crowley, R.K. Treatment of hypercalcaemia of malignancy in adults. Clin. Med. 2023, 23, 503–507. [Google Scholar] [CrossRef]
- El-Hajj Fuleihan, G.; Clines, G.A.; Hu, M.I.; Marcocci, C.; Murad, M.H.; Piggott, T.; Van Poznak, C.; Wu, J.Y.; Drake, M.T. Treatment of Hypercalcemia of Malignancy in Adults: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2023, 108, 507–528. [Google Scholar] [CrossRef] [PubMed]
- Nistor, C.; Ciuche, A.; Constantinescu, I. Emergency surgical tracheal decompression in a huge retrosternal goiter. Acta Endocrinol. 2017, 13, 370–374. [Google Scholar] [CrossRef]
- Piantanida, E.; Ippolito, S.; Gallo, D.; Masiello, E.; Premoli, P.; Cusini, C.; Rosetti, S.; Sabatino, J.; Segato, S.; Trimarchi, F.; et al. The interplay between thyroid and liver: Implications for clinical practice. J. Endocrinol. Investig. 2020, 43, 885–899. [Google Scholar] [CrossRef]
- Benner, B.J.M.; Alsma, J.; Feelders, R.A. Hyponatraemia and hyperpigmentation in primary adrenal insufficiency. BMJ Case Rep. 2019, 12, e227200. [Google Scholar] [CrossRef]
- Nistor, C.E.; Pantile, D.; Gavan, C.S.; Ciuche, A. Pneumothorax on COVID-19 patients-retrospective clinical observations. Rom. J. Leg. Med. 2022, 30, 112–116. [Google Scholar] [CrossRef]
- Zhou, X.; Huang, T.; Pan, H.; Du, A.; Wu, T.; Lan, J.; Song, Y.; Lv, Y.; He, F.; Yuan, K. Bioinformatics and system biology approaches to determine the connection of SARS-CoV-2 infection and intrahepatic cholangiocarcinoma. PLoS ONE 2024, 19, e0300441. [Google Scholar] [CrossRef]
- Wiwanitkit, V. Thioredoxin reductase-1 and incidence of COVID-19 among cholangiocarcinoma patients in tropical endemic area. J. Cancer Res. Ther. 2023, 19, 845. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Li, J.; Xiao, W.; Zhang, Y.; Lv, Y.; Yu, X.; Zheng, J. The Therapeutic Potential of Galectin-3 in the Treatment of Intrahepatic Cholangiocarcinoma Patients and Those Compromised with COVID-19. Front. Mol. Biosci. 2021, 8, 666054. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Pavuluri, S.; Srinivasan, K.; Ghouse, M. Thrombotic Microangiopathy in a Patient with COVID-19 Infection and Metastatic Cholangiocarcinoma. J. Hematol. 2021, 10, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, S.; Gokhale, P.; Katte, T.; Acharya, S.; Rasalkar, A.A.; Vidapanakal, S.; Manas, R.; Chinnam, S.; Narayanan, P.; Shettihalli, A.K.; et al. Assessing the Vulnerability of Cancer Patients for COVID-19. ACS Omega 2022, 7, 35735–35742. [Google Scholar] [CrossRef]

| Conditions | Key Elements | Reference Numbers |
|---|---|---|
| Chronic biliary diseases | Primary sclerosing cholangitis | [7,8,9] |
| Bile ducts cysts or choledochal cysts (including Caroli’s disease) | [13,14,16,17] | |
| Hepatholithiasis | [17] | |
| Chronic liver conditions | Cirrhosis | [1,9,15,20,21,22] |
| Hepatitis B and C virus chronic infections | [15,23,24,25,26,27] | |
| Hemochromatosis | [1,28,29,30,31,32,33] | |
| Wilson’s disease | [34,35,36,37] | |
| Digestive ailments | Inflammatory bowel disease (ulcerative colitis, Crohn’s disease) Chronic pancreatitis Duodenal or gastric ulcer | [1,13,15,38,39] |
| Parasitic infections (liver fluke) | Opisthorchis viverrini or Clonorchis sinensis | [1,6,9,15,42,43,44] |
| Lifestyle influence | Chronic alcohol consumption | [44,45] |
| Cigarette smoking | [55,56,57] | |
| Environmental exposure | Thorotrast | [61,62] |
| Asbestos | [64,65,66] | |
| Genetic and epigenetic considerations | BRCA to TBX3, p53 | [69,70,71] |
| Metabolic and endocrine interferences | Non-alcoholic fatty liver disease | [78,79] |
| Obesity | [80,81,82,83] | |
| Type 2 diabetes mellitus | [1,5,9,15,84,85,86] | |
| Vitamin D deficiency | [90,91] | |
| Modulation of glucagon-like peptide 1 receptor | [98] | |
| Modulation of galanin system | [100,101] | |
| Sex hormone therapy (oestrogens in adult females) | [107,108,109] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciobica, M.-L.; Sandulescu, B.-A.; Chicea, L.-M.; Iordache, M.; Groseanu, M.-L.; Carsote, M.; Nistor, C.; Radu, A.-M. The Constellation of Risk Factors and Paraneoplastic Syndromes in Cholangiocarcinoma: Integrating the Endocrine Panel Amid Tumour-Related Biology (A Narrative Review). Biology 2024, 13, 662. https://doi.org/10.3390/biology13090662
Ciobica M-L, Sandulescu B-A, Chicea L-M, Iordache M, Groseanu M-L, Carsote M, Nistor C, Radu A-M. The Constellation of Risk Factors and Paraneoplastic Syndromes in Cholangiocarcinoma: Integrating the Endocrine Panel Amid Tumour-Related Biology (A Narrative Review). Biology. 2024; 13(9):662. https://doi.org/10.3390/biology13090662
Chicago/Turabian StyleCiobica, Mihai-Lucian, Bianca-Andreea Sandulescu, Liana-Maria Chicea, Mihaela Iordache, Maria-Laura Groseanu, Mara Carsote, Claudiu Nistor, and Ana-Maria Radu. 2024. "The Constellation of Risk Factors and Paraneoplastic Syndromes in Cholangiocarcinoma: Integrating the Endocrine Panel Amid Tumour-Related Biology (A Narrative Review)" Biology 13, no. 9: 662. https://doi.org/10.3390/biology13090662





