Longitudinal Effects on Metabolic Biomarkers in Veterans 12 Months Following Discharge from Pharmacist-Provided Diabetes Care: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
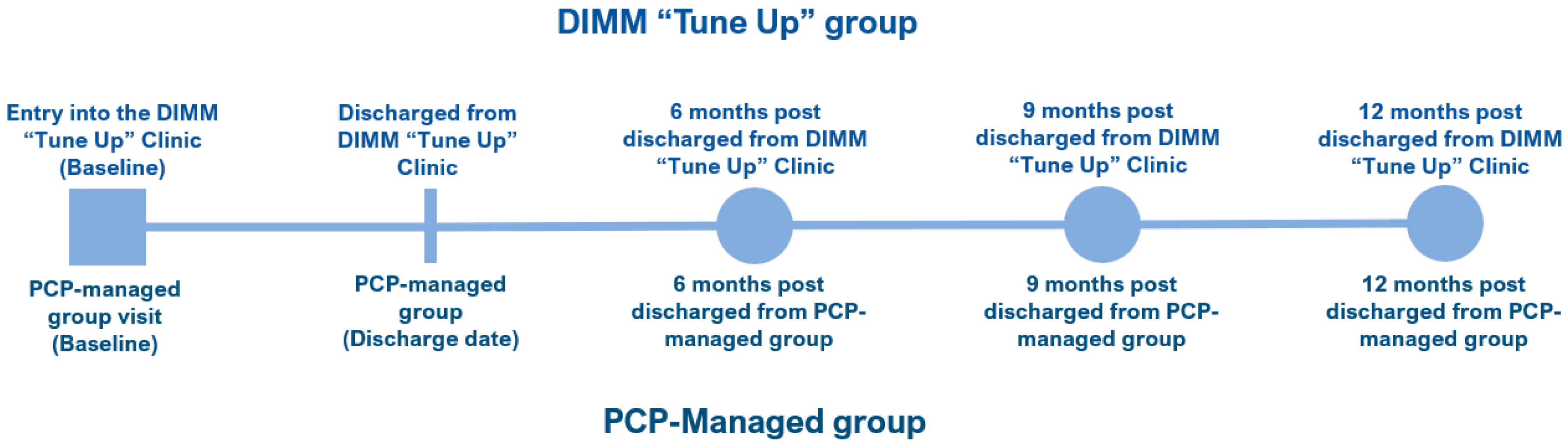
2.1. Study Design
2.2. DIMM “Tune Up” Clinic Intervention
2.3. DIMM-Managed Sample
2.4. Control Group and Matching Strategy
2.5. Variables
2.6. Statistical Analysis
3. Results
3.1. Demographics
3.2. Metabolic Biomarker Comparisons across Time
3.3. Metabolic Goal Attainment across Time
3.4. GEE Model Results
3.5. Sensitivity Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. GEE Model Results (Primary Aim Analysis)
| Outcome | Time | Marginal Effect (95% CI) | p-Value |
|---|---|---|---|
| HbA1c | Entry | −0.04 (−0.47, 0.39) | 0.861 |
| HbA1c | Discharge | −0.96 (−1.30, −0.63) | <0.001 |
| HbA1c | 6-month post | −0.72 (−1.12, −0.31) | <0.001 |
| HbA1c | 9-month post | −0.55 (−0.99, −0.10) | 0.016 |
| HbA1c | 12-month post | −0.32 (−0.79, 0.14) | 0.171 |
| FPG | Entry | −3.93 (−22.91, 15.06) | 0.685 |
| FPG | Discharge | −28.38 (−46.00, −10.76) | 0.002 |
| FPG | 6-month post | −24.02 (−48.03, −0.01) | 0.050 |
| FPG | 9-month post | −18.33 (−40.52, 3.85) | 0.105 |
| FPG | 12-month post | −16.20 (−39.87, 7.47) | 0.180 |
| LDL | Entry | −10.71 (−20.83, −0.59) | 0.038 |
| LDL | Discharge | −17.59 (−27.70, −7.49) | 0.001 |
| LDL | 6-month post | −15.42 (−25.12, −5.71) | 0.002 |
| LDL | 9-month post | −15.10 (−24.87, −5.33) | 0.002 |
| LDL | 12-month post | −9.82 (−19.97, 0.33) | 0.058 |
| HDL | Entry | 0.12 (3.16, 3.40) | 0.942 |
| HDL | Discharge | 0.98 (−2.61, 4.58) | 0.592 |
| HDL | 6-month post | 1.55 (−1.62, 4.71) | 0.339 |
| HDL | 9-month post | 1.23 (−2.56, 5.03) | 0.524 |
| HDL | 12-month post | 2.12 (−1.69, 5.93) | 0.276 |
Appendix B. GEE Models Using the Imputed Dataset
| Outcome | Time | Marginal Effect (95% CI) | p-Value |
|---|---|---|---|
| HbA1c | Entry | −0.05 (−0.47, 0.37) | 0.813 |
| HbA1c | Discharge | −1.02 (−1.35, 0.69) | <0.001 |
| HbA1c | 6-month post | −0.79 (−1.18, −0.39) | <0.001 |
| HbA1c | 9-month post | −0.57 (−1.01, −0.14) | 0.009 |
| HbA1c | 12-month post | −0.37 (−0.81, 0.08) | 0.109 |
| FPG | Entry | −3.80 (−21.86, 14.27) | 0.68 |
| FPG | Discharge | −30.80 (−47.83, −13.78) | <0.001 |
| FPG | 6-month post | −29.57 (−52.90, −6.24) | 0.013 |
| FPG | 9-month post | −21.67 (−43.01, −0.32) | 0.047 |
| FPG | 12-month post | −19.87 (−42.48, 2.74) | 0.085 |
| LDL | Entry | −9.99 (−19.91, −0.07) | 0.048 |
| LDL | Discharge | −16.47 (−26.34, −6.60) | 0.001 |
| LDL | 6-month post | −13.73 (−23.22, −4.24) | 0.005 |
| LDL | 9-month post | −14.16 (−23.70, −4.62) | 0.004 |
| LDL | 12-month post | −8.81 (−18.63, 1.00) | 0.078 |
| HDL | Entry | −2.19 (−5.99, 1.61) | 0.259 |
| HDL | Discharge | −0.37 (−3.86, 3.13) | 0.837 |
| HDL | 6-month post | 1.20 (−1.91, 4.32) | 0.448 |
| HDL | 9-month post | 0.44 (−3.20, 4.07) | 0.813 |
| HDL | 12-month post | 1.50 (−2.11, 5.11) | 0.415 |
References
- Centers for Disease Control and Prevention; National Center for Health Statistics. Underlysing Cause of Death 1999–2020 on CDC WONDER Online Database. Published 27 December 2020. Available online: https://wonder.cdc.gov/controller/datarequest/D76;jsessionid=58928F559EABA6E76A1E44A40BC3 (accessed on 27 February 2022).
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020; Centers for Disease Control and Prevention, U.S. Department of Health and Human Services: Washington, DC, USA, 2020. Available online: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf (accessed on 19 April 2022).
- Papatheodorou, K.; Banach, M.; Bekiari, E.; Rizzo, M.; Edmonds, M. Complications of Diabetes 2017. J. Diabetes Res. 2018, 2018, 3086167. [Google Scholar] [CrossRef] [PubMed]
- Fowler, M.J. Microvascular and Macrovascular Complications of Diabetes. Clin. Diabete. 2008, 26, 77–82. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Wan, X.H.; Zhao, G.H. Meta-analysis of the Risk of Cataract in Type 2 Diabetes. BMC Ophthalmol. 2014, 14, 94. [Google Scholar] [CrossRef]
- Goto, A.; Arah, O.A.; Goto, M.; Terauchi, Y.; Noda, M. Severe Hypoglycaemia and Cardiovascular Disease: Systematic Review and Meta-analysis with Bias Analysis. BMJ 2013, 347, f4533. [Google Scholar] [CrossRef] [Green Version]
- Brownrigg, J.R.W.; Schaper, N.C.; Hinchliffe, R.J. Diagnosis and Assessment of Peripheral Arterial Disease in the Diabetic Foot. Diabet Med. J. Br. Diabet Assoc. 2015, 32, 738–747. [Google Scholar] [CrossRef]
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44 (Suppl. S1), S15–S33. [Google Scholar] [CrossRef]
- Liu, Y.; Sayam, S.; Shao, X.; Wang, K.; Zheng, S.; Li, Y.; Wang, L. Prevalence of and Trends in Diabetes Among Veterans, United States, 2005–2014. Prev. Chronic. Dis. 2017, 14, E135. [Google Scholar] [CrossRef] [Green Version]
- Morello, C.M.; Rotunno, T.; Khoan, J.; Hirsch, J.D. Improved Glycemic Control With Minimal Change in Medication Regimen Complexity in a Pharmacist-Endocrinologist Diabetes Intense Medical Management (DIMM) “Tune Up” Clinic. Ann. Pharmacother. 2018, 52, 1091. [Google Scholar] [CrossRef]
- Morello, C.M.; Christopher, M.L.D.; Ortega, L.; Khoan, J.; Rotunno, T.; Edelman, S.V.; Henry, R.R.; Hirsch, J. Clinical Outcomes Associated with a Collaborative Pharmacist-Endocrinologist Diabetes Intense Medical Management “Tune Up” Clinic in Complex Patients. Ann Pharmacother. 2016, 50, 8–16. [Google Scholar] [CrossRef]
- Hirsch, J.D.; Kong, N.; Nguyen, K.T.; Cadiz, C.L.; Zhou, C.; Bajorek, S.A.; Bounthavong, M.; Morello, C.M. Improved Patient-Reported Medication Adherence, Patient Satisfaction, and Glycemic Control in a Collaborative Care Pharmacist-Led Diabetes “Tune-Up” Clinic. Int. J. Environ. Res. Public Health 2021, 18, 9242. [Google Scholar] [CrossRef]
- McInnis, T.; Strand, L.M.; Webb, C.E.; the PCPCC Medication Management Task Force. The Patient-Centered Medical Home: Integrating Comprehensive Medication Management to Optimize Patient Outcomes, 2nd ed.; Patient-Centered Primary Care Collaborative: Washington, DC, USA, 2012; Available online: https://www.pcpcc.org/sites/default/files/media/medmanagement.pdf (accessed on 19 April 2022).
- Hirsch, J.D.; Bounthavong, M.; Arjmand, A.; Ha, D.R.; Cadiz, C.L.; Zimmerman, A.; Ourth, H.; Morreale, A.P.; Edelman, S.V.; Morello, C.M. Estimated Cost-Effectiveness, Cost Benefit, and Risk Reduction Associated with an Endocrinologist-Pharmacist Diabetes Intense Medical Management “Tune-Up” Clinic. J. Manag. Care Spec. Pharm. 2017, 23, 318–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmidt, K.; Caudill, J.A.; Hamilton, T. Impact of Clinical Pharmacy Specialists on Glycemic Control in Veterans with Type 2 Diabetes. Am. J. Health-Syst. Pharm. 2019, 76 (Suppl. S1), S9–S14. [Google Scholar] [CrossRef] [PubMed]
- Biltaji, E.; Yoo, M.; Jennings, B.T.; Leiser, J.P.; McAdam-Marx, C. Outcomes Associated with Pharmacist-Led Diabetes Collaborative Drug Therapy Management in a Medicaid Population. J. Pharm. Health Serv. Res. 2017, 8, 59–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iqbal, M.Z.; Khan, A.H.; Iqbal, M.S.; Syed Sulaiman, S.A. A Review of Pharmacist-led Interventions on Diabetes Outcomes: An Observational Analysis to Explore Diabetes Care Opportunities for Pharmacists. J. Pharm. Bioallied Sci. 2019, 11, 299–309. [Google Scholar] [CrossRef]
- Gallo, V.; Egger, M.; McCormack, V.; Farmer, P.B.; Ioannidis, J.P.A.; Kirsch-Volders, M.; Matullo, G. STrengthening the Reporting of OBservational studies in Epidemiology—Molecular Epidemiology STROBE-ME: An extension of the STROBE statement. J. Clin. Epidemiol. 2011, 64, 1350–1363. [Google Scholar] [CrossRef] [Green Version]
- Everett, C.M.; Morgan, P.; Smith, V.A.; Woolson, S.; Edelman, D.; Hendrix, C.C.; Berkowitz, T.; White, B.; Jackson, G.L. Primary care provider type: Are there differences in patients’ intermediate diabetes outcomes? JAAPA 2019, 32, 36–42. [Google Scholar] [CrossRef]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef] [Green Version]
- Demirtas, H.; Freels, S.A.; Yucel, R.M. Plausibility of Multivariate Normality Assumption when Multiply Imputing Non-Gaussian Continuous Outcomes: A Simulation Assessment. J. Stat. Comput. Simul. 2008, 78, 69–84. [Google Scholar] [CrossRef]
- Lee, K.J.; Carlin, J.B. Multiple Imputation for Missing data: Fully Conditional Specification Versus Multivariate Normal Imputation. Am. J. Epidemiol. 2010, 171, 624–632. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, M.; Sherry, P.S.; Taylor, L.M.; Amato, M.; Tataronis, G.R.; Cushing, G. Pharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) study. J. Am. Pharm. Assoc. 2012, 52, 613–621. [Google Scholar] [CrossRef]
- Ip, E.J.; Shah, B.M.; Yu, J.; Chan, J.; Nguyen, L.T.; Bhatt, D.C. Enhancing Diabetes Care by Adding a Pharmacist to the Primary Care Team. Am. J. Health-Syst. Pharm. 2013, 70, 877–886. [Google Scholar] [CrossRef] [PubMed]
- Wubben, D.P.; Vivian, E.M. Effects of Pharmacist Outpatient Interventions on Adults with Diabetes Mellitus: A Systematic Review. Pharmacotherapy 2008, 28, 421–436. [Google Scholar] [CrossRef] [PubMed]
- Brummel, A.R.; Soliman, A.M.; Carlson, A.M.; de Oliveira, D.R. Optimal Diabetes Care Outcomes Following Face-to-Face Medication Therapy Management Services. Popul. Health Manag. 2013, 6, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Polonsky, W.H.; Henry, R.R. Poor Medication Adherence in Type 2 Diabetes: Recognizing the Scope of the Problem and Its Key Contributors. Patient Prefer. Adherence 2016, 10, 1299–1307. [Google Scholar] [CrossRef] [Green Version]
- Polonsky, W.H.; Fisher, L.; Hessler, D.; Edelman, S.V. What is So Tough about Self-monitoring of Blood Glucose? Perceived Obstacles among Patients with Type 2 Diabetes. Diabet Med. J. Br. Diabet Assoc. 2014, 31, 40–46. [Google Scholar] [CrossRef]
- De Vries, S.T.; Keers, J.C.; Visser, R.; de Zeeuw, D.; Haaijer-Ruskamp, F.M.; Voorham, J.; Denig, P. Medication Beliefs, Treatment Complexity, and Non-adherence to Different Drug Classes in Patients with Type 2 Diabetes. J. Psychosom. Res. 2014, 76, 134–138. [Google Scholar] [CrossRef] [Green Version]
- Egede, L.E.; Gebregziabher, M.; Echols, C.; Lynch, C.P. Longitudinal Effects of Medication Nonadherence on Glycemic Control. Ann. Pharmacother. 2014, 48, 562–570. [Google Scholar] [CrossRef]
- Hoogendoorn, C.J.; Shapira, A.; Roy, J.F.; Walker, E.A.; Cohen, H.W.; Gonzalez, J.S. Depressive Symptom Dimensions and Medication Non-adherence in Suboptimally Controlled Type 2 Diabetes. J. Diabetes Complicat. 2019, 33, 217–222. [Google Scholar] [CrossRef]
- U.S. Department of Veterans Affairs. VA/DoD Clinical Practice Guideline for the Management of Type 2 Diabetes Mellitus In Primary Care. Published online 2017. Available online: https://www.healthquality.va.gov/guidelines/CD/diabetes/VADoDDMCPGFinal508.pdf (accessed on 19 April 2022).
- Hirsch, J.D.; Steers, N.; Adler, D.S.; Kuo, G.M.; Morello, C.M.; Lang, M.; Singh, R.F.; Wood, Y.; Kaplan, R.M.; Mangione, C.M. Primary Care-Based, Pharmacist-Physician Collaborative Medication-Therapy Management of Hypertension: A Randomized, Pragmatic Trial. Clin. Ther. 2014, 36, 1244–1254. [Google Scholar] [CrossRef] [Green Version]
- Predmore, Z.S.; Roth, E.; Breslau, J.; Fischer, S.H.; Uscher-Pines, L. Assessment of Patient Preferences for Telehealth in Post–COVID-19 Pandemic Health Care. JAMA Netw. Open 2021, 4, e2136405. [Google Scholar] [CrossRef]
- Monaghesh, E.; Hajizadeh, A. The Role of Telehealth During COVID-19 Outbreak: A Systematic Review Based on Current Evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef] [PubMed]
- Reicher, S.; Sela, T.; Toren, O. Using Telemedicine during the COVID-19 Pandemic: Attitudes of Adult Health Care Consumers in Israel. Front Public Health 2021, 9, 653553. Available online: https://www.frontiersin.org/article/10.3389/fpubh.2021.653553 (accessed on 12 February 2022).
- Oliver, A. The Veterans Health Administration: An American Success Story? Milbank Q. 2007, 85, 5–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campbell, D.G.; Lombardero, A.; English, I.; Waltz, T.J.; Hoggatt, K.J.; Simon, B.F.; Lanto, A.B.; Simon, A.; Rubenstein, L.V.; Chaney, E.F. Depression Complexity Prevalence and Outcomes Among Veterans Affairs Patients in Integrated Primary Care. Fam. Syst. Health 2022, 40, 35–45. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | DIMM-Managed Group n = 123 | PCP-Managed Group n = 123 | p-Value a | Missing Data (DIMM, PCP) |
|---|---|---|---|---|
| Age (years) | 60.9 (8.3) | 60.4 (11.7) | 0.740 | 0, 0 |
| BMI (kg/m2) | 33.1 (6.2) | 32.7 (6.7) | 0.641 | 10, 7 |
| Male, n (%) | 119 (96.8%) | 117 (95.1%) | 0.518 | 0, 0 |
| HbA1c (%), mean (SD) | 10.2 (1.4) | 10.3 (1.9) | 0.779 | 0, 0 |
| LDL (mg/dL), mean (SD) | 86.8 (39.4) | 94.4 (37.8) | 0.136 | 9, 7 |
| HDL (mg/dL), mean (SD) | 40.0 (13.2) | 42.6 (16.6) | 0.184 | 2, 0 |
| TG (mg/dL), mean (SD) | 235.5 (204.1) | 244.1 (364.0) | 0.822 | 4, 0 |
| FPG (mg/dL), mean (SD) | 160.1 (72.3) | 163.3 (72.8) | 0.732 | 0, 0 |
| eGFR (mL/min), mean (SD) | 80.0 (28.7) | 81.3 (30.7) | 0.735 | 0, 0 |
| Congestive heart failure, n (%) | 19 (15.5%) | 14 (11.4%) | 0.350 | 0, 0 |
| Cardiac arrhythmias, n (%) | 23 (18.7%) | 19 (15.5%) | 0.498 | 0, 0 |
| Valvular disease, n (%) | 7 (5.7%) | 4 (3.3%) | 0.355 | 0, 0 |
| Pulmonary circulation disorder, n (%) | 8 (6.5%) | 3 (2.4%) | 0.123 | 0, 0 |
| Peripheral vascular disease, n (%) | 20 (16.3%) | 15 (12.2%) | 0.361 | 0, 0 |
| Hypertension (uncomplicated), n (%) | 113 (91.9%) | 108 (87.8%) | 0.291 | 0, 0 |
| Hypertension (complicated), n (%) | 14 (11.4%) | 13 (10.6%) | 0.838 | 0, 0 |
| Paralysis, n (%) | 3 (2.4%) | 3 (2.4%) | >0.999 | 0, 0 |
| Other neurologic disorder, n (%) | 4 (3.3%) | 5 (4.1%) | 0.734 | 0, 0 |
| Chronic pulmonary disease, n (%) | 29 (23.6%) | 20 (16.3%) | 0.151 | 0, 0 |
| Thyroid, n (%) | 12 (9.8%) | 10 (8.1%) | 0.655 | 0, 0 |
| Renal failure, n (%) | 19 (15.5%) | 14 (11.4%) | 0.350 | 0, 0 |
| Liver disease, n (%) | 23 (18.7%) | 24 (19.5%) | 0.871 | 0, 0 |
| Peptic ulcer disease, n (%) | 2 (1.6%) | 1 (0.8%) | 0.561 | 0, 0 |
| AIDS/HIV, n (%) | 1 (0.8%) | 1 (0.8%) | >0.999 | 0, 0 |
| Lymphoma, n (%) | 0 (0.0%) | 0 (0.0%) | N/A | 0, 0 |
| Metastatic cancer, n (%) | 2 (1.6%) | 1 (0.8%) | 0.561 | 0, 0 |
| Tumor without metastasis, n (%) | 10 (8.1%) | 15 (12.2%) | 0.291 | 0, 0 |
| Rheumatoid arthritis, n (%) | 3 (2.4%) | 0 (0.0%) | 0.081 | 0, 0 |
| Coagulopathy, n (%) | 4 (3.3%) | 3 (2.4%) | 0.701 | 0, 0 |
| Obesity, n (%) | 75 (61.0%) | 68 (55.3%) | 0.366 | 0, 0 |
| Depression, n (%) | 52 (42.3%) | 55 (44.7%) | 0.700 | 0, 0 |
| Bipolar, n (%) | 9 (7.3%) | 9 (7.3%) | >0.999 | 0, 0 |
| Generalized anxiety disorder, n (%) | 6 (4.9%) | 7 (5.7%) | 0.776 | 0, 0 |
| Schizophrenia, n (%) | 1 (0.8%) | 3 (2.4%) | 0.313 | 0, 0 |
| PTSD, n (%) | 3 (2.4%) | 7 (5.7%) | 0.197 | 0, 0 |
| End points | DIMM-Managed Group (n = 123) | PCP-Managed Group (n = 123) | p-Value a | Missing Data (DIMM, PCP) |
|---|---|---|---|---|
| HbA1c (%), mean (SD) | ||||
| Baseline | 10.24 (1.45) | 10.30 (1.92) | 0.780 | 0, 0 |
| Discharge | 7.25 (0.79) | 8.27 (1.67) | <0.001 | 0, 0 |
| 6 months | 7.62 (1.30) | 8.42 (1.82) | <0.001 | 0, 0 |
| 9 months | 7.80 (1.65) | 8.39 (1.84) | 0.009 | 0, 0 |
| 12 months | 7.97 (1.85) | 8.34 (1.78) | 0.105 | 0, 0 |
| FPG (mg/dL), mean (SD) | ||||
| Baseline | 160.09 (72.31) | 163.26 (72.79) | 0.732 | 0, 0 |
| Discharge | 141.25 (61.91) | 171.43 (73.17) | <0.001 | 0, 0 |
| 6 months | 163.63 (93.97) | 192.58 (94.78) | 0.017 | 0, 0 |
| 9 months | 162.26 (87.80) | 183.30 (83.21) | 0.055 | 0, 0 |
| 12 months | 167.10 (79.89) | 186.34 (100.42) | 0.098 | 0, 0 |
| LDL (mg/dL), mean (SD) | ||||
| Baseline | 86.80 (39.40) | 94.42 (37.80) | 0.136 | 9, 7 |
| Discharge | 77.13 (38.00) | 92.83 (39.73) | 0.002 | 4, 1 |
| 6 months | 78.27 (38.44) | 92.21 (41.09) | 0.007 | 2, 1 |
| 9 months | 77.30 (38.18) | 91.54 (40.61) | 0.005 | 2, 0 |
| 12 months | 81.56 (39.94) | 90.66 (41.41) | 0.082 | 2, 0 |
| HDL (mg/dL), mean (SD) | ||||
| Baseline | 39.99 (13.19) | 42.55 (16.59) | 0.184 | 2, 0 |
| Discharge | 41.54 (15.07) | 42.12 (12.77) | 0.750 | 2, 0 |
| 6 months | 41.28 (11.81) | 40.39 (13.26) | 0.579 | 1, 0 |
| 9 months | 41.07 (15.96) | 40.83 (12.86) | 0.895 | 1, 0 |
| 12 months | 41.60 (16.16) | 40.34 (12.34) | 0.494 | 1, 0 |
| End Points | Baseline | Discharge | 6-Months Post-Discharge | 9-Months Post-Discharge | 12-Months Post-Discharge | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Metabolic Goals | DIMM | PCP | p-Value a | DIMM | PCP | p-Value a | DIMM | PCP | p-Value a | DIMM | PCP | p-Value a | DIMM | PCP | p-Value a |
| HbA1c < 7, n (%) | 0 (0.0%) | 0 (0.0%) | n/a | 45 (36.6%) | 25 (20.3%) | 0.005 | 38 (30.9%) | 29 (23.6%) | 0.197 | 38 (30.9%) | 29 (23.6%) | 0.197 | 32 (26.0%) | 29 (23.6%) | 0.658 |
| HbA1c < 8, n (%) | 0 (0.0%) | 0 (0.0%) | n/a | 101 (82.1%) | 61 (49.6%) | <0.001 | 83 (67.5%) | 58 (47.2%) | 0.001 | 77 (62.6%) | 61 (49.6%) | 0.040 | 70 (56.9%) | 58 (47.2%) | 0.126 |
| HbA1c < 9, n (%) | 18 (14.6%) | 35 (28.5%) | 0.008 | 123 (100.0%) | 85 (69.1%) | <0.001 | 108 (87.8%) | 82 (66.7%) | <0.001 | 101 (82.1%) | 84 (68.3%) | 0.012 | 97 (78.9%) | 85 (69.1%) | 0.081 |
| FPG = 70–130, n (%) | 41 (33.3%) | 39 (31.7%) | 0.785 | 58 (47.2%) | 36 (29.3%) | 0.004 | 47 (38.2%) | 33 (26.8%) | 0.057 | 50 (40.7%) | 33 (26.8%) | 0.022 | 50 (40.7%) | 33 (26.8%) | 0.022 |
| LDL < 70, n (%) | 42 (36.2%) | 29 (23.4%) | 0.077 | 61 (50.0%) | 36 (30.3%) | 0.002 | 49 (40.2%) | 41 (33.9%) | 0.311 | 55 (44.7%) | 39 (32.3%) | 0.045 | 50 (40.7%) | 40 (33.1%) | 0.219 |
| LDL < 100, n (%) | 80 (69.0%) | 68 (59.7%) | 0.140 | 104 (85.3%) | 75 (63.0%) | <0.001 | 100 (82.0%) | 75 (62.0%) | 0.001 | 103 (83.7%) | 77 (63.6%) | <0.001 | 95 (77.2%) | 78 (64.5%) | 0.028 |
| HDL > 40, n (%) | 52 (42.3%) | 61 (50.4%) | 0.203 | 61 (49.6%) | 65 (53.7%) | 0.519 | 60 (48.8%) | 55 (45.1%) | 0.562 | 56 (45.5) | 58 (47.5%) | 0.752 | 62 (50.4%) | 57 (46.7%) | 0.564 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morello, C.M.; Lai, L.; Chen, C.; Leung, C.M.; Hirsch, J.D.; Bounthavong, M. Longitudinal Effects on Metabolic Biomarkers in Veterans 12 Months Following Discharge from Pharmacist-Provided Diabetes Care: A Retrospective Cohort Study. Pharmacy 2022, 10, 63. https://doi.org/10.3390/pharmacy10030063
Morello CM, Lai L, Chen C, Leung CM, Hirsch JD, Bounthavong M. Longitudinal Effects on Metabolic Biomarkers in Veterans 12 Months Following Discharge from Pharmacist-Provided Diabetes Care: A Retrospective Cohort Study. Pharmacy. 2022; 10(3):63. https://doi.org/10.3390/pharmacy10030063
Chicago/Turabian StyleMorello, Candis M., Lytia Lai, Claire Chen, Chui Man Leung, Jan D. Hirsch, and Mark Bounthavong. 2022. "Longitudinal Effects on Metabolic Biomarkers in Veterans 12 Months Following Discharge from Pharmacist-Provided Diabetes Care: A Retrospective Cohort Study" Pharmacy 10, no. 3: 63. https://doi.org/10.3390/pharmacy10030063
APA StyleMorello, C. M., Lai, L., Chen, C., Leung, C. M., Hirsch, J. D., & Bounthavong, M. (2022). Longitudinal Effects on Metabolic Biomarkers in Veterans 12 Months Following Discharge from Pharmacist-Provided Diabetes Care: A Retrospective Cohort Study. Pharmacy, 10(3), 63. https://doi.org/10.3390/pharmacy10030063







