Associations between the Number of Children, Depressive Symptoms, and Cognition in Middle-Aged and Older Adults: Evidence from the China Health and Retirement Longitudinal Study
Abstract
:1. Introduction
2. Materials and Methods
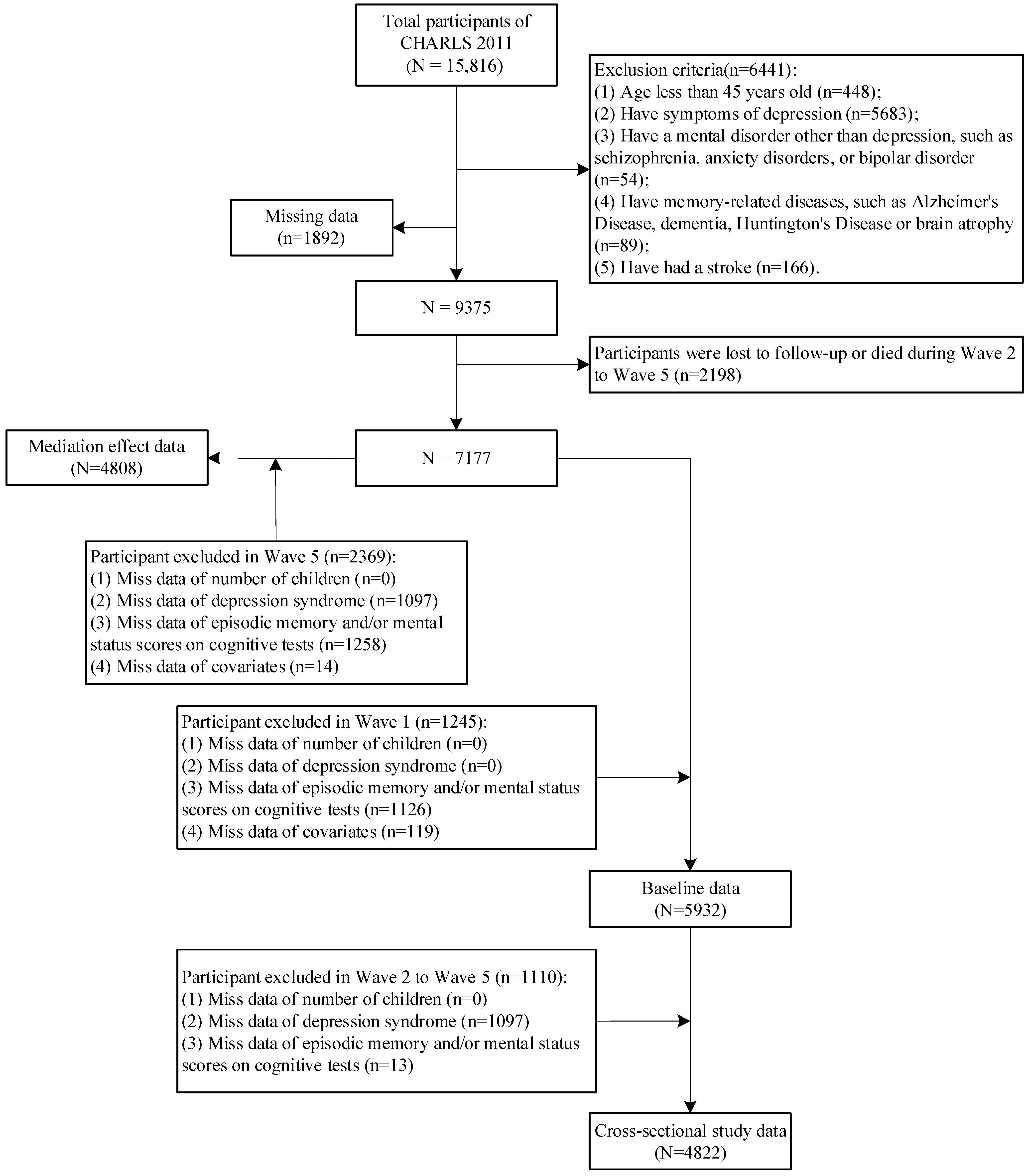
2.1. Study Population
2.2. Cognitive Function
2.3. Depressive Symptoms
2.4. Number of Children
2.5. Covariates
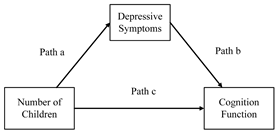
2.6. Statistical Analysis
- The equation for the mediator (depressive symptoms) is as follows:
- The equation for the outcome (cognitive function) is as follows:where represents the mediator (depressive symptoms); represents the outcome (cognitive function); represents the independent variable (number of children); , , , , and are the coefficients; and are the error terms.
3. Results
3.1. Participant Characteristics
3.2. Association between the Number of Children, Depression, and Cognitive Function
3.3. Mediating Effect of Depressive Symptoms
3.4. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bai, C.; Lei, X. New trends in population aging and challenges for China’s sustainable development. China Econ. J. 2020, 13, 3–23. [Google Scholar] [CrossRef]
- Williams, G.A.; Cylus, J.; Al Tayara, L.; Roubal, T.; Tsilaajav, T.; Barber, S.L. Can healthy ageing moderate the effects of population ageing on economic growth and health spending trends in Mongolia? A modelling study. Health Res. Policy Syst. 2022, 20, 122. [Google Scholar] [CrossRef] [PubMed]
- Boyle, P.A.; Wang, T.; Yu, L.; Wilson, R.S.; Dawe, R.; Arfanakis, K.; Schneider, J.A.; Bennett, D.A. To what degree is late life cognitive decline driven by age-related neuropathologies? Brain 2021, 144, 2166–2175. [Google Scholar] [CrossRef]
- Lim, Y.Y.; Kong, J.; Maruff, P.; Jaeger, J.; Huang, E.; Ratti, E. Longitudinal Cognitive Decline in Patients with Mild Cognitive Impairment or Dementia Due to Alzheimer’s Disease. JPAD-J. Prev. Alzheimers Dis. 2022, 9, 178–183. [Google Scholar] [CrossRef]
- Nguyen, J.C.; Killcross, A.S.; Jenkins, T.A. Obesity and cognitive decline: Role of inflammation and vascular changes. Front. Neurosci. 2014, 8, 375. [Google Scholar] [CrossRef]
- Huang, J.L.; Zhang, F.; Su, M.; Li, J.; Yi, W.; Hou, L.X.; Yang, S.M.; Liu, J.Y.; Zhang, H.A.; Ma, T.; et al. MeCP2 prevents age-associated cognitive decline via restoring synaptic plasticity in a senescence-accelerated mouse model. Aging Cell 2021, 20, e13451. [Google Scholar] [CrossRef]
- Yang, F.; Fu, M.; Hu, Q.; Guo, J. The associations between cognitive function and depressive symptoms among older Chinese population: A cohort study. Front. Psychiatry 2023, 14, 1081209. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, L.J.; Veronese, N.; Vernuccio, L.; Catanese, G.; Inzerillo, F.; Salemi, G.; Barbagallo, M. Nutrition, Physical Activity, and Other Lifestyle Factors in the Prevention of Cognitive Decline and Dementia. Nutrients 2021, 13, 4080. [Google Scholar] [CrossRef]
- Drew, D.A.; Weiner, D.E.; Sarnak, M.J. Cognitive Impairment in CKD: Pathophysiology, Management, and Prevention. Am. J. Kidney Dis. 2019, 74, 782–790. [Google Scholar] [CrossRef]
- Ren, Y.; Savadlou, A.; Park, S.; Siska, P.; Epp, J.R.; Sargin, D. The impact of loneliness and social isolation on the development of cognitive decline and Alzheimer’s Disease. Front. Neuroendocr. 2023, 69, 101061. [Google Scholar] [CrossRef]
- Lee, H.; Ryan, L.H.; Ofstedal, M.B.; Smith, J. Multigenerational Households During Childhood and Trajectories of Cognitive Functioning Among U.S. Older Adults. J. Gerontol. Ser. B 2020, 76, 1161–1172. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Jia, J. Association of intergenerational relationships with cognitive impairment among Chinese adults 80 years of age or older: Prospective cohort study. BMC Geriatr. 2022, 22, 838. [Google Scholar] [CrossRef] [PubMed]
- Mair, C.; Ornstein, K. Kinlessness and cognitive function among european older adults. Innov. Aging 2022, 6, 402. [Google Scholar] [CrossRef]
- Phillips, M.; Kobayashi, L.; Chakraborty, R.; Wagner, R.; Mahlalela, N.; Harezlak, J.; Brown, J.; Ludema, C.; Rosenberg, M. Number of children and mid- to later-life cognitive function and cognitive impairment in rural South Africa: Evidence from “Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa” (HAALSI). medRxiv 2023. [Google Scholar] [CrossRef]
- Saenz, J.L.; Díaz-Venegas, C.; Crimmins, E.M. Fertility History and Cognitive Function in Late Life: The Case of Mexico. J. Gerontol. Ser. B 2019, 76, e140–e152. [Google Scholar] [CrossRef]
- Du, Y.; Luo, Y.; Zheng, X.; Liu, J. Number of children and cognitive function among Chinese menopausal women: The mediating role of depressive symptoms and social participation. J. Affect. Disord. 2023, 340, 758–765. [Google Scholar] [CrossRef]
- Barrett, A.E.; Turner, R.J. Family structure and mental health: The mediating effects of socioeconomic status, family process, and social stress. J. Health Soc. Behav. 2005, 46, 156–169. [Google Scholar] [CrossRef]
- Dong, X.; Ng, N.; Santosa, A. Family structure and depressive symptoms among older adults in China: A marginal structural model analysis. J. Affect. Disord. 2023, 324, 364–369. [Google Scholar] [CrossRef]
- Aziz, R.; Steffens, D. Overlay of Late-Life Depression and Cognitive Impairment. Focus 2017, 15, 35–41. [Google Scholar] [CrossRef]
- Jellinger, K.A. Pathomechanisms of Vascular Depression in Older Adults. Int. J. Mol. Sci. 2022, 23, 308. [Google Scholar] [CrossRef]
- Köhler, S.; Thomas, A.J.; Barnett, N.A.; O’Brien, J.T. The pattern and course of cognitive impairment in late-life depression. Psychol. Med. 2010, 40, 591–602. [Google Scholar] [CrossRef] [PubMed]
- Manning, K.J.; Wu, R.; McQuoid, D.R.; Steffens, D.C.; Potter, G.G. Reliable Cognitive Decline in Late-Life Major Depression. Arch. Clin. Neuropsychol. 2023, 38, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Hu, Y.; Smith, J.P.; Strauss, J.; Yang, G. Cohort Profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 2012, 43, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Sonnega, A.; Faul, J.D.; Ofstedal, M.B.; Langa, K.M.; Phillips, J.W.R.; Weir, D.R. Cohort Profile: The Health and Retirement Study (HRS). Int. J. Epidemiol. 2014, 43, 576–585. [Google Scholar] [CrossRef]
- Mcardle, J.J.; Fisher, G.G.; Kadlec, K.M. Latent variable analyses of age trends of cognition in the Health and Retirement Study, 1992–2004. Psychol. Aging 2007, 22, 525–545. [Google Scholar] [CrossRef]
- Fu, H.; Si, L.; Guo, R. What Is the Optimal Cut-Off Point of the 10-Item Center for Epidemiologic Studies Depression Scale for Screening Depression Among Chinese Individuals Aged 45 and Over? An Exploration Using Latent Profile Analysis. Front. Psychiatry 2022, 13, 820777. [Google Scholar] [CrossRef]
- Brandt, J.; Spencer, M.; Folstein, M. The Telephone Interview for Cognitive Status. Neuropsychiatry Neuropsychol. Behav. Neurol. 1988, 1, 111–117. [Google Scholar]
- Andresen, E.M.; Malmgren Ja Fau-Carter, W.B.; Carter Wb Fau-Patrick, D.L.; Patrick, D.L. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Prev. Med. 1994, 10, 77–84. [Google Scholar]
- Chen, H.; Mui, A.C. Factorial validity of the Center for Epidemiologic Studies Depression Scale short form in older population in China. Int. Psychogeriatr. 2014, 26, 49–57. [Google Scholar] [CrossRef]
- Luo, H.; Li, J.; Zhang, Q.; Cao, P.; Ren, X.; Fang, A.; Liao, H.; Liu, L. Obesity and the onset of depressive symptoms among middle-aged and older adults in China: Evidence from the CHARLS. BMC Public Health 2018, 18, 909. [Google Scholar] [CrossRef]
- Heger-Laube, I.; Durollet, R. Ageing without Family Caregivers: A Heuristic for Understanding and Approaching a Complex Phenomenon. 2024. Available online: https://www.researchgate.net/publication/377329838_Ageing_Without_Family_Caregivers_A_Heuristic_for_Understanding_and_Approaching_ a_Complex_Phenomenon (accessed on 16 November 2023).
- Chen, C.; Tian, Y.; Ni, L.; Xu, Q.; Hu, Y.; Peng, B. The influence of social participation and depressive symptoms on cognition among middle-aged and older adults. Heliyon 2024, 10, e24110. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Weng, X.; Subramanian, S.V. Associations between older adults’ parental bereavement and their health and well-being: Evidence from the China health and retirement longitudinal study. J. Affect. Disord. 2020, 272, 207–214. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Liu, K.Y.; Costafreda, S.G.; Selbæk, G.; Alladi, S.; Ames, D.; Banerjee, S.; Burns, A.; Brayne, C.; et al. Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission. Lancet 2024, 404, 572–628. [Google Scholar] [CrossRef] [PubMed]
- Zellner, A.; Theil, H. Three-Stage Least Squares: Simultaneous Estimation of Simultaneous Equations. In Henri Theil’s Contributions to Economics and Econometrics: Econometric Theory and Methodology; Raj, B., Koerts, J., Eds.; Springer: Dordrecht, The Netherlands, 1992; pp. 147–178. [Google Scholar]
- Lin, Y.-C.; Washington-Nortey, P.-M.; Hill, O.W.; Serpell, Z.N. Family Functioning and Not Family Structure Predicts Adolescents’ Reasoning and Math Skills. J. Child Fam. Stud. 2019, 28, 2700–2707. [Google Scholar] [CrossRef]
- Hayes, A.F. Beyond Baron and Kenny: Statistical Mediation Analysis in the New Millennium. Commun. Monogr. 2009, 76, 408–420. [Google Scholar] [CrossRef]
- MacKinnon, D.P.; Lockwood, C.M.; Hoffman, J.M.; West, S.G.; Sheets, V. A comparison of methods to test mediation and other intervening variable effects. Psychol. Methods 2002, 7, 83–104. [Google Scholar] [CrossRef]
- Koopman, J.; Howe, M.; Hollenbeck, J.R. Pulling the Sobel Test up by its bootstraps. In More Statistical and Methodological Myths and Urban Legends; Routledge/Taylor & Francis Group: New York, NY, USA, 2015; pp. 224–243. [Google Scholar]
- Cardona, M.; Andres, P. Are social isolation and loneliness associated with cognitive decline in ageing? Front. Aging Neurosci. 2023, 15, 1075563. [Google Scholar] [CrossRef]
- Yin, S.; Yang, Q.; Xiong, J.; Li, T.; Zhu, X. Social Support and the Incidence of Cognitive Impairment Among Older Adults in China: Findings From the Chinese Longitudinal Healthy Longevity Survey Study. Front. Psychiatry 2020, 11, 254. [Google Scholar] [CrossRef]
- Peng, L. The Impact of Children on Their Parents’Labor Supply in China: An Instrumental Variable Approach. In Proceedings of the 2022 7th International Conference on Big Data Analytics (ICBDA), Guangzhou, China, 4–6 March 2022; pp. 317–329. [Google Scholar]
- Bonsang, E.; Skirbekk, V. Does Childbearing Affect Cognitive Health in Later Life? Evidence From an Instrumental Variable Approach. Demography 2022, 59, 975–994. [Google Scholar] [CrossRef]
- Lee, A.-R.; Torres, J.; Flores Romero, K.R. Adult Child Financial Disadvantage and the Cognitive Trajectories Among Older Parents in the United States. J. Gerontol. Ser. B 2024, 79, gbae123. [Google Scholar] [CrossRef]
- Lin, I.F.; Wu, H.S. Sibling Influences, Sibling Similarities, and Parent Care in Late Life. Ou Mei Yan Jiu 2019, 49, 45–73. [Google Scholar] [PubMed]
- Lin, I.-F.; Wolf, D.A. Division of Parent Care Among Adult Children. J. Gerontol. Ser. B 2019, 75, 2230–2239. [Google Scholar] [CrossRef] [PubMed]
- Ruseski, J.E.; Humphreys, B.R.; Hallmann, K.; Breuer, C. Family structure, time constraints, and sport participation. Eur. Rev. Aging Phys. Act. 2011, 8, 57–66. [Google Scholar] [CrossRef]
- Carson, V.; Adamo, K.; Rhodes, R.E. Associations of Parenthood with Physical Activity, Sedentary Behavior, and Sleep. Am. J. Health Behav. 2018, 42, 80–89. [Google Scholar] [CrossRef]
- Taylor, C.A.; Bouldin, E.D.; Greenlund, K.J.; McGuire, L.C. Comorbid Chronic Conditions Among Older Adults with Subjective Cognitive Decline, United States, 2015–2017. Innov. Aging 2020, 4, igz045. [Google Scholar] [CrossRef] [PubMed]
- Bordier, L.; Doucet, J.; Boudet, J.; Bauduceau, B. Update on cognitive decline and dementia in elderly patients with diabetes. Diabetes Metab. 2014, 40, 331–337. [Google Scholar] [CrossRef]
- Forte, G.; Casagrande, M. Effects of Blood Pressure on Cognitive Performance in Aging: A Systematic Review. Brain Sci. 2020, 10, 919. [Google Scholar] [CrossRef]
- Penning, M.J.; Wu, Z. Marital Status, Childlessness, and Social Support among Older Canadians. Can. J. Aging/La Rev. Can. Du Vieil. 2014, 33, 426–447. [Google Scholar] [CrossRef]
- Yang, X.; Pan, A.; Gong, J.; Wen, Y.; Ye, Y.; Wu, J.H.Y.; Pan, X.-F.; Yang, C.-X. Prospective associations between depressive symptoms and cognitive functions in middle-aged and elderly Chinese adults. J. Affect. Disord. 2020, 263, 692–697. [Google Scholar] [CrossRef]
- Zhou, L.; Ma, X.; Wang, W. Relationship between Cognitive Performance and Depressive Symptoms in Chinese Older Adults: The China Health and Retirement Longitudinal Study (CHARLS). J. Affect. Disord. 2021, 281, 454–458. [Google Scholar] [CrossRef]
- Wang, G.; Zhou, Y.; Duan, J.; Kan, Q.; Cheng, Z.; Tang, S. Effects of adverse childhood health experiences on cognitive function in Chinese middle-aged and older adults: Mediating role of depression. BMC Public Health 2023, 23, 1293. [Google Scholar] [CrossRef] [PubMed]
- Gili, M.; López-Navarro, E.; Castro, A.; Homar, C.; Navarro, C.; García-Toro, M.; García-Campayo, J.; Roca, M. Gender differences in mental health during the economic crisis. Psicothema 2016, 28, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.Y.; Hu, H.Y.; Ou, Y.N.; Wang, Z.T.; Ma, Y.H.; Tan, L.; Yu, J.-T. Socioeconomic Status and Risks of Cognitive Impairment and Dementia: A Systematic Review and Meta-Analysis of 39 Prospective Studies. J. Prev. Alzheimer’s Dis. 2023, 10, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Peen, J.; Schoevers, R.A.; Beekman, A.T.; Dekker, J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr. Scand. 2010, 121, 84–93. [Google Scholar] [CrossRef]
- Xu, J.; Liu, N.; Polemiti, E.; Garcia-Mondragon, L.; Tang, J.; Liu, X.; Lett, T.; Yu, L.; Nöthen, M.M.; Feng, J.; et al. Effects of urban living environments on mental health in adults. Nat. Med. 2023, 29, 1456–1467. [Google Scholar] [CrossRef]
- Wong, A.; Chau, A.K.C.; Fang, Y.; Woo, J. Illuminating the Psychological Experience of Elderly Loneliness from a Societal Perspective: A Qualitative Study of Alienation between Older People and Society. Int. J. Environ. Res. Public Health 2017, 14, 824. [Google Scholar] [CrossRef]
- Fan, X.; Guo, X.; Ren, Z.; Li, X.; He, M.; Shi, H.; Zha, S.; Qiao, S.; Zhao, H.; Li, Y.; et al. The prevalence of depressive symptoms and associated factors in middle-aged and elderly Chinese people. J. Affect. Disord. 2021, 293, 222–228. [Google Scholar] [CrossRef]
| Variables, n (%) | Number of Children (N = 5932) | χ2/t-Statistic | p-Value | ||||
|---|---|---|---|---|---|---|---|
| 0 (n = 55) | 1 (n = 1102) | 2 (n = 2268) | 3 (n = 1386) | ≥4 (n = 1121) | |||
| Age (mean ± SD, years) | 56.91 ± 7.85 | 53.13 ± 6.35 | 54.73 ± 6.92 | 58.40 ± 7.91 | 64.07 ± 8.19 | 1500.000 | <0.001 *** |
| Gender | |||||||
| Female | 16 (0.58) | 527 (19.21) | 1035 (37.73) | 625 (22.79) | 540 (19.69) | 10.365 | 0.035 * |
| Male | 39 (1.22) | 575 (18.03) | 1233 (38.66) | 761 (23.86) | 581 (18.22) | ||
| Residence | |||||||
| Rural | 29 (0.85) | 366 (10.75) | 1323 (38.84) | 910 (26.72) | 778 (22.84) | 369.681 | <0.001 *** |
| Urban | 26 (1.03) | 736 (29.14) | 945 (37.41) | 476 (18.84) | 343 (13.58) | ||
| Education level | |||||||
| Below Primary School | 24 (1.21) | 201 (10.11) | 663 (33.33) | 520 (26.14) | 581 (29.21) | 507.464 | <0.001 *** |
| Primary School | 11 (0.81) | 199 (14.62) | 506 (37.18) | 365 (26.82) | 280 (20.57) | ||
| Middle School | 12 (0.76) | 375 (23.64) | 699 (44.07) | 338 (21.31) | 162 (10.21) | ||
| High School and Above | 8 (0.80) | 327 (32.83) | 400 (40.16) | 163 (16.37) | 98 (9.84) | ||
| Marital status | |||||||
| Divorced/Separated/Widowed/Never Married | 21 (4.95) | 66 (15.57) | 99 (23.35) | 82 (19.34) | 156 (36.79) | 189.050 | <0.001 *** |
| Married/Cohabitated | 34 (0.62) | 1036 (18.81) | 2169 (39.38) | 1304 (23.67) | 965 (17.52) | ||
| Total Cognition (mean ± SD, score) | 12.16 ± 3.34 | 13.80 ± 2.99 | 13.01 ± 3.14 | 12.37 ± 3.24 | 11.48 ± 3.51 | 502.032 | <0.001 *** |
| Episodic Memory | 3.58 ± 1.54 | 4.42 ± 1.63 | 4.11 ± 1.62 | 3.79 ± 1.60 | 3.45 ± 1.64 | 318.144 | <0.001 *** |
| Mental Status | 8.58 ± 2.42 | 9.39 ± 1.96 | 8.90 ± 2.22 | 8.58 ± 2.42 | 8.02 ± 2.64 | 246.147 | <0.001 *** |
| CES-D10 a (mean ± SD, score) | 4.70 ± 2.30 | 3.79 ± 2.64 | 4.15 ± 2.75 | 4.46 ± 2.80 | 4.51 ± 2.76 | 101.993 | <0.001 *** |
| Sleep Duration(h) | |||||||
| (0, 6] | 17 (0.69) | 404 (16.32) | 899 (36.32) | 628 (25.37) | 527 (21.29) | 52.395 | <0.001 *** |
| (6, 8] | 34 (1.15) | 617 (20.87) | 1178 (39.85) | 644 (21.79) | 483 (16.34) | ||
| >8 | 4 (0.80) | 81 (16.17) | 191 (38.12) | 114 (22.75) | 111 (22.16) | ||
| Life Satisfaction | |||||||
| Very Good | 1 (4.76) | 3 (14.29) | 5 (23.81) | 3 (14.29) | 9 (42.86) | 50.770 | <0.001 *** |
| Good | 7 (1.54) | 88 (19.38) | 153 (33.70) | 105 (23.13) | 101 (22.25) | ||
| Fair | 35 (0.89) | 752 (19.18) | 1562 (39.85) | 903 (23.04) | 668 (17.04) | ||
| Poor | 10 (0.71) | 231 (16.33) | 508 (35.90) | 345 (24.38) | 321 (22.69) | ||
| Very poor | 2 (1.64) | 28 (22.95) | 40 (32.79) | 30 (24.59) | 22 (18.03) | ||
| Smoking | 29 (1.16) | 434 (17.43) | 961 (38.59) | 591 (23.73) | 475 (19.08) | 6.123 | 0.190 |
| Drinking | 23 (1.03) | 478 (21.31) | 897 (39.99) | 501 (22.34) | 344 (15.34) | 43.632 | <0.001 *** |
| Hypertension | 12 (0.90) | 237 (17.77) | 453 (33.96) | 337 (25.26) | 295 (22.11) | 20.925 | <0.001 *** |
| Diabetes | 1 (0.33) | 69 (23.00) | 105 (35.00) | 76 (25.33) | 49 (16.33) | 7.016 | 0.135 |
| Lung Disease | 8 (2.12) | 47 (12.47) | 134 (35.54) | 88 (23.34) | 100 (26.53) | 27.447 | <0.001 *** |
| Strokeb | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | - | - |
| Mental Disorderc | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | - | - |
| Heart Disease | 7 (1.38) | 79 (15.61) | 175 (34.58) | 138 (27.27) | 107 (21.15) | 10.881 | 0.028 * |
| Liver Disease | 4 (2.44) | 41 (25.00) | 51 (31.10) | 36 (21.95) | 32 (19.51) | 10.327 | 0.035 * |
| Kidney Disease | 7 (3.07) | 39 (17.11) | 90 (39.47) | 56 (24.56) | 36 (15.79) | 13.474 | 0.009 ** |
| Models | Episodic Memory | Mental Status | Total Cognition | |||
|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | |
| Crude model | ||||||
| Number of Children | ||||||
| 1 | Ref. | - | Ref. | - | Ref. | - |
| 0 | −0.147 * | (−0.280, −0.013) | −0.100 * | (−0.192, −0.009) | −0.117 ** | (−0.203, −0.031) |
| 2 | −0.066 *** | (−0.093, −0.040) | −0.062 *** | (−0.081, −0.043) | −0.064 *** | (−0.081, −0.046) |
| 3 | −0.125 *** | (−0.155, −0.094) | −0.091 *** | (−0.113, −0.069) | −0.103 *** | (−0.123, −0.083) |
| ≥4 | −0.222 *** | (−0.259, −0.185) | −0.125 *** | (−0.150, −0.100) | −0.159 *** | (−0.183, −0.136) |
| Depression | ||||||
| 0 | Ref. | - | Ref. | - | Ref. | - |
| 1 | −0.141 *** | (−0.166,−0.115) | −0.102 *** | (−0.119,−0.085) | −0.116 *** | (−0.132, −0.100) |
| Model 1 | ||||||
| Number of Children | ||||||
| 1 | Ref. | - | Ref. | - | Ref. | - |
| 0 | −0.055 | (−0.178, 0.068) | −0.053 | (−0.137, 0.031) | −0.054 | (−0.131, 0.004) |
| 2 | −0.007 | (−0.033, 0.018) | −0.020 * | (−0.038, −0.002) | −0.015 | (−0.031, 0.002) |
| 3 | −0.018 | (−0.049, 0.013) | −0.031 ** | (−0.053, −0.010) | −0.026 ** | (−0.045, −0.006) |
| ≥4 | −0.053 ** | (−0.091, −0.015) | −0.046 *** | (−0.071, −0.020) | −0.048 *** | (−0.071, −0.024) |
| Depression | ||||||
| 0 | Ref. | - | Ref. | - | Ref. | - |
| 1 | −0.106 *** | (−0.130, −0.083) | −0.062 *** | (−0.078, −0.046) | −0.078 *** | (−0.093, −0.063) |
| Model 2 | ||||||
| Number of Children | ||||||
| 1 | Ref. | - | Ref. | - | Ref. | - |
| 0 | −0.061 | (−0.183, 0.061) | −0.060 | (−0.143, 0.024) | −0.060 | (−0.137, 0.016) |
| 2 | −0.006 | (−0.032, 0.019) | −0.018 * | (−0.036, −0.001) | −0.013 | (−0.029, 0.003) |
| 3 | −0.015 | (−0.046, 0.015) | −0.028 * | (−0.049, −0.007) | −0.023 * | (−0.042, −0.003) |
| ≥4 | −0.049 * | (−0.087, −0.011) | −0.041 *** | (−0.067, −0.016) | −0.043 *** | (−0.067, −0.020) |
| Depression | ||||||
| 0 | Ref. | - | Ref. | - | Ref. | - |
| 1 | −0.102 *** | (−0.127, −0.077) | −0.063 *** | (−0.080, −0.046) | −0.078 *** | (−0.093, −0.062) |
| Models | Crude Model | Model 1 | Model 2 | |
|---|---|---|---|---|
 Path a: Exposure predicting mediator Path b: Mediator predicting outcome Path c: Exposure predicting outcome | Coefficients (95% CI) | |||
| Path a | 0.035 *** (0.022, 0.047) | 0.020 ** (0.006, 0.034) | 0.019 ** (0.006, 0.033) | |
| Path b | −1.336 *** (−1.531, −1.142) | −0.955 *** (−1.135, −0.773) | −0.972 *** (−1.159, −0.786) | |
| Path c | −0.613 *** (−0.701, −0.524) | −0.171 *** (−0.261, −0.081) | −0.159 *** (−0.248, −0.069) | |
| Effect | ||||
| Total effect a | −0.566 *** (−0.653, −0.479) | −0.152 *** (−0.241, −0.063) | −0.140 ** (−0.228, −0.051) | |
| Indirect effect b | −0.046 *** (−0.065, −0.029) | −0.019 ** (−0.034, −0.005) | −0.019 ** (−0.034, −0.006) | |
| pMe c | 8.13% | 12.50% | 13.57% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, Y.; Mai, H.; Bian, Y. Associations between the Number of Children, Depressive Symptoms, and Cognition in Middle-Aged and Older Adults: Evidence from the China Health and Retirement Longitudinal Study. Healthcare 2024, 12, 1928. https://doi.org/10.3390/healthcare12191928
Zhao Y, Mai H, Bian Y. Associations between the Number of Children, Depressive Symptoms, and Cognition in Middle-Aged and Older Adults: Evidence from the China Health and Retirement Longitudinal Study. Healthcare. 2024; 12(19):1928. https://doi.org/10.3390/healthcare12191928
Chicago/Turabian StyleZhao, Yongze, Huaxin Mai, and Ying Bian. 2024. "Associations between the Number of Children, Depressive Symptoms, and Cognition in Middle-Aged and Older Adults: Evidence from the China Health and Retirement Longitudinal Study" Healthcare 12, no. 19: 1928. https://doi.org/10.3390/healthcare12191928






