Cytocidal Effects of Interstitial Photodynamic Therapy Using Talaporfin Sodium and a Semiconductor Laser in a Rat Intracerebral Glioma Model
Abstract
:1. Introduction
2. Material and Methods
2.1. Materials
2.1.1. Cell Culture
2.1.2. Rat Basal Ganglia C6 Transplantation Model
2.1.3. Talaporfin Sodium (TPS)
2.1.4. Laser Irradiation Fiber Probe
2.2. Methods
2.2.1. Implementation of i-PDT
2.2.2. Post-Irradiation Tissue Sampling
2.2.3. Histopathological Analyses
2.2.4. Statistical Processing
3. Results
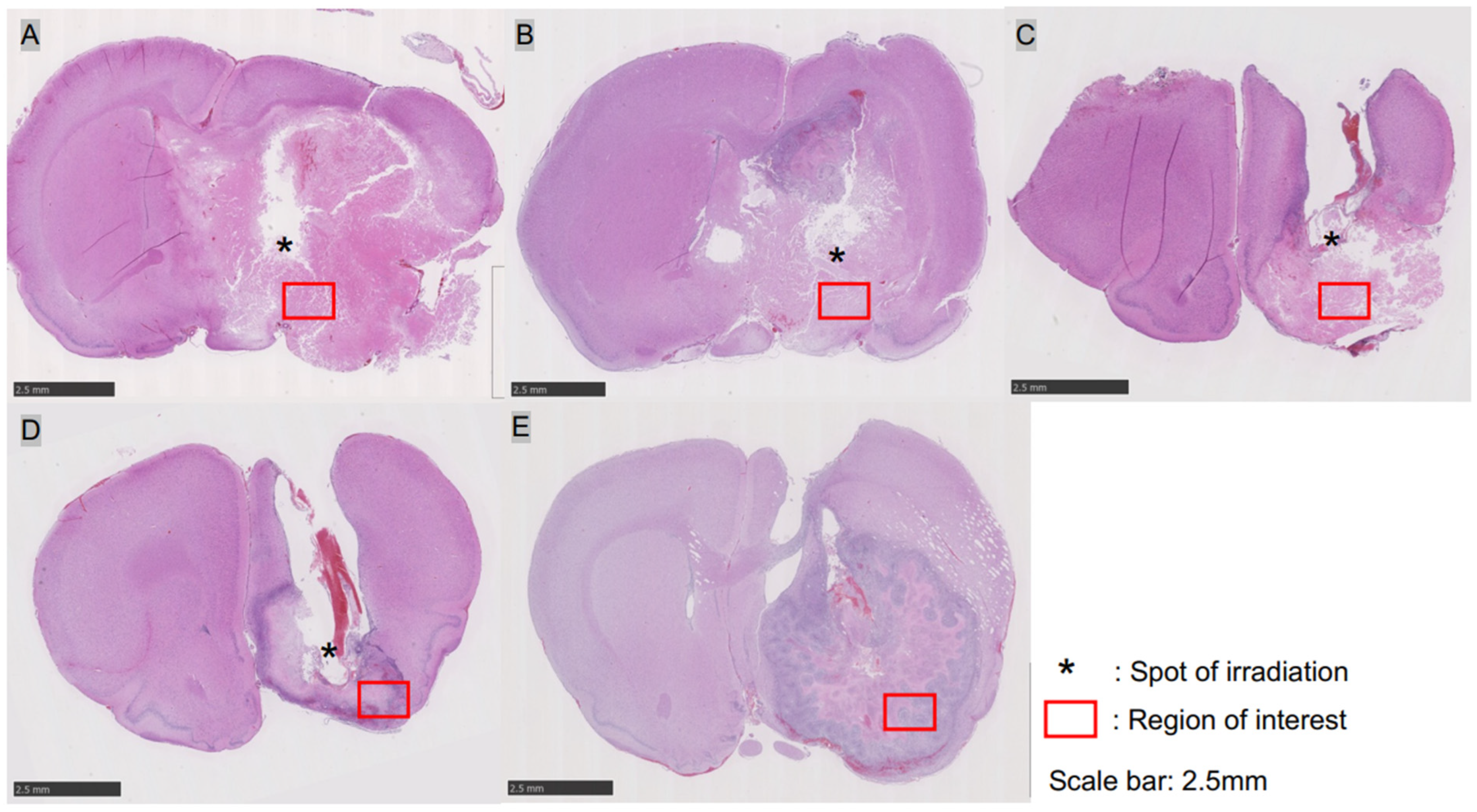
3.1. C6 Transplantation Rat Basal Ganglia Glioma Model
3.2. Tumor Pathology 24 h after i-PDT
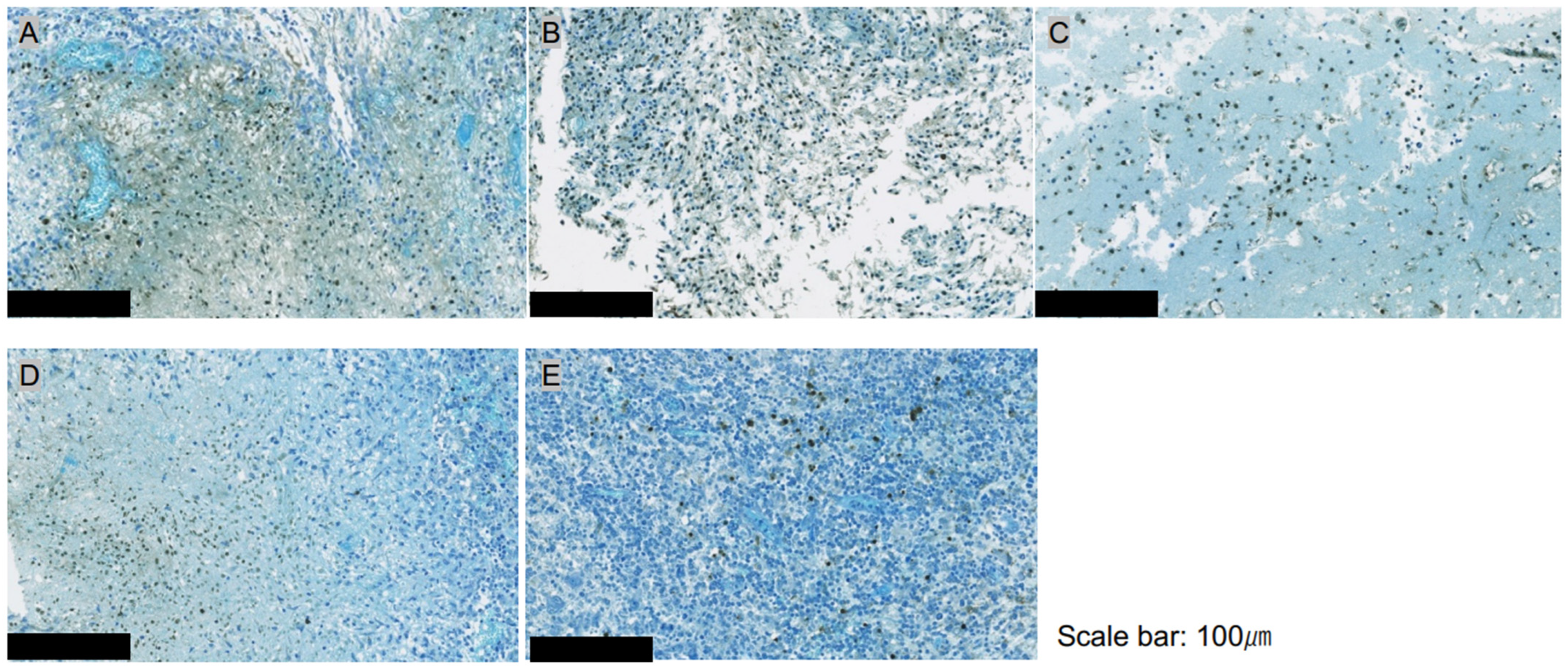
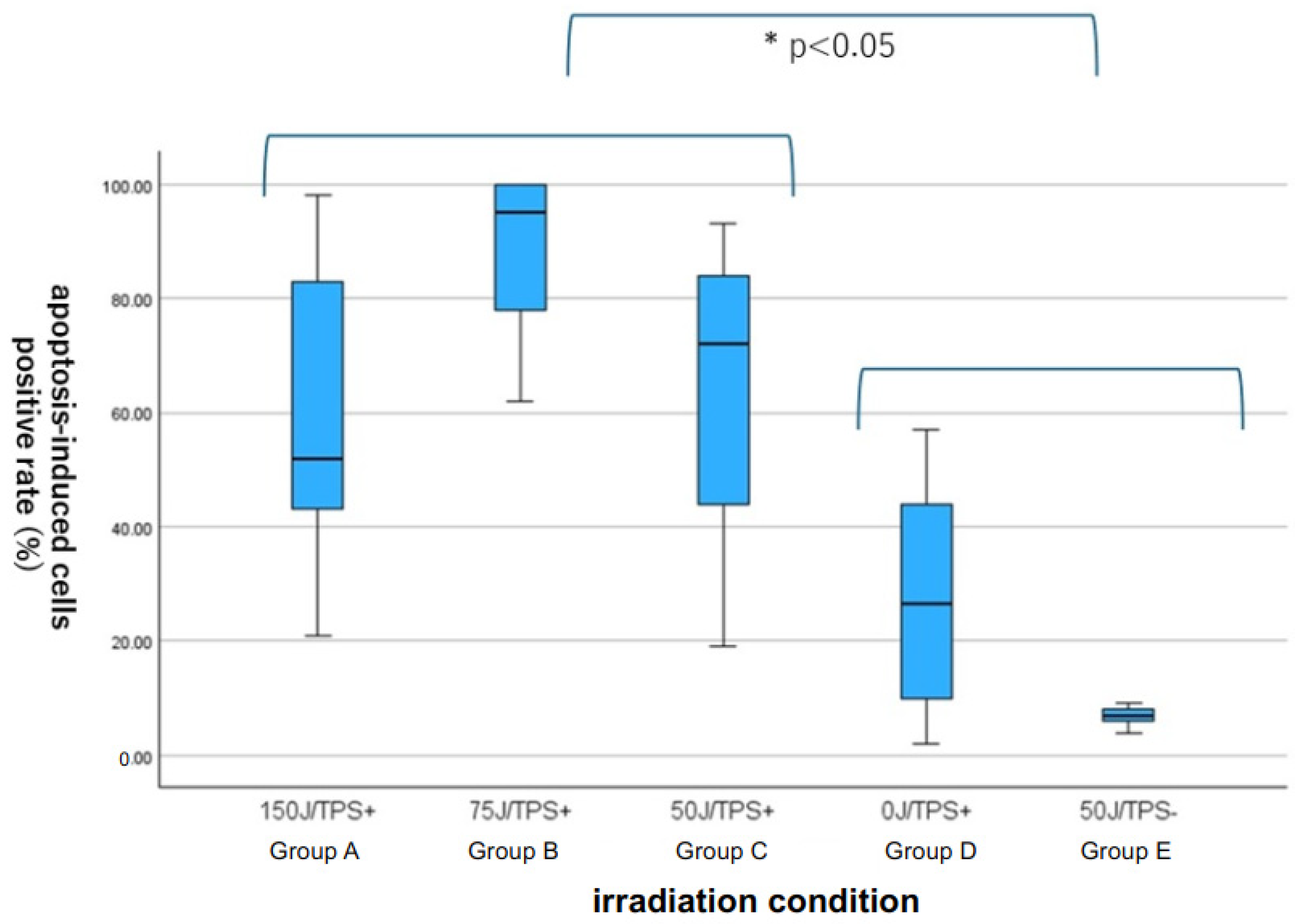
3.3. Quantitative Assessment of Apoptosis with ApopMark™
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ostrom, Q.T.; Bauchet, L.; Davis, F.G.; Deltour, I.; Fisher, J.L.; Langer, C.E.; Pekmezci, M.; Schwartzbaum, J.A.; Turner, M.C.; Walsh, K.M.; et al. The epidemiology of glioma in sdults: A “state of the science” review. Neuro-Oncol. 2014, 16, 896–913. [Google Scholar] [CrossRef] [PubMed]
- Ostrom, Q.T.; Gittleman, H.; Truitt, G.; Boscia, A.; Krunko, C.; Barnholtz-Sloan, J.S. CBTRUS statistical report: Primary brain and central nervous system tumors diagnosed in united states in 2011–2015. Neuro-Oncol. 2018, 20, iv1–iv86. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Mason, W.P.; van den Bent, M.J.; Weller, M.; Fisher, B.; Taphoorn, M.J.B.; Belanger, K.; Brandes, A.A.; Marosi, C.; Bogdahn, U.; et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 2005, 10, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Lacroix, M.; Abi-Said, D.; Fourney, D.R.; Gokaslan, W.; DeMonte, F.; Lang, F.F.; McCutcheon, E.; Hassenbusch, S.J.; Hokkand, E.; Hess, K.; et al. A multivariate analysis of 416 patients with glioblastoma multiforme: Prognosis, extent of resection, and survival. J. Neurosurg. 2001, 95, 190–198. [Google Scholar] [CrossRef] [PubMed]
- Sanai, N.; Polly, M.Y.; McDermott, M.W.; Parsa, A.T.; Berger, M. An extent of resection threshold for newly diagnosed glioblastomas. J. Neurosurg. 2011, 115, 3–8. [Google Scholar] [CrossRef]
- Sales, A.H.; Beck, J.; Schnell, O.; Fung, C.; Meyer, B.; Gempt, J. Surgical treatment of glioblastoma: State-of-the-art and future trend. J. Clin. Med. 2022, 11, 5354. [Google Scholar] [CrossRef] [PubMed]
- Jusue-Torres, I.; Lee, J.; Germanwala, A.V.; Burns, T.; Parney, I.F. Effect of extent of resection on survival of patients with glioblastoma, IDH Wild-type, WHO Grade 4 (WHO 2021): Systematic review and meta-analysis. World Neurosurg. 2023, 171, e524–e532. [Google Scholar] [CrossRef] [PubMed]
- Karshnia, P.; Dono, A.; Young, J.S.; Juenger, S.T.; Teske, N.; Hani, L.; Sciortino, T.; Mau, C.Y.; Bruno, F.; Nunez, L.; et al. Prognostic validation of a new classification system for extent of resection in glioblastoma: A report of RANO resect group. Neuro-Oncol. 2024, 26, 584–586. [Google Scholar] [CrossRef]
- Keles, G.E.; Lamborn, K.R.; Chang, S.M.; Prados, M.D.; Berger, M.S. Volume of residual disease as a predictor of outcome in adult patients with recurrent supratentorial glioblastomas multiforme who are undergoing chemotherapy. J. Neurosurg. 2004, 100, 41–46. [Google Scholar] [CrossRef]
- Castano, A.P.; Demidova, T.N.; Hambrin, M.R. Mechanism of photodynamic therapy: Part three- photosensitizer pharmacokinetics, biodistribution, tumor localization and modes of tumor destruction. Photodiagn. Photodyn. Ther. 2005, 2, 91–106. [Google Scholar] [CrossRef]
- Quirk, B.J.; Brandal, G.; Donlon SVera, J.C.; Mang, T.S.; Foy ABLew, S.M.; Girotti, A.W.; Jogal, S.; LaViolette, P.S.; Connely, J.M.; Whelan, H.T. Photodynamic therapy (PDT) for malignant brain tumors-where do we stand? Photodiagn. Photodyn. Ther. 2015, 12, 530–544. [Google Scholar] [CrossRef] [PubMed]
- Stylli, S.S.; Kaye, A.H.; MacGregor, L.; Howes, M.; Rajendra, P. Photodynamic therapy of high grade glioma-long term survival. J. Clin. Neurosci. 2005, 12, 389–398. [Google Scholar] [CrossRef]
- Kostron, H.; Fiegele, T.; Akatuna, E. Combination of FOSCAN mediated fluorescence guided resection and photodynamic therapy as a therapeutic concept of malignant brain tumors. Med. Laser Appl. 2006, 21, 285–290. [Google Scholar] [CrossRef]
- Stepp, H.; Beck, T.; Pongratz, T.; Meinel, T.; Kreth, F.W.; Tonn JCh Stummer, W. ALA and malignant glioma: Fluorescence-guided resection and photodynamic treatment. J. Environ. Pathol. Toxicol. Oncol. 2007, 26, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Muller, J.P.; Wilson, B.C. Photodynamic therapy of brain tumor—A work in progress. Laser Surg. Med. 2008, 38, 384–389. [Google Scholar] [CrossRef]
- Eljamel, S.; Goodman, C.; Moseley, H. ALA and porphyrin fluorescence guided resection and repetitive PDT in glioblastoma multiforme: A single centre phase III randomized controlled trial. Lasers Med. Sci. 2008, 23, 361–367. [Google Scholar] [CrossRef]
- Akimoto, J. Photodynamic therapy for malignant brain tumors. Neurol. Med. Chir. 2016, 56, 151–157. [Google Scholar] [CrossRef]
- Akimoto, J.; Haraoka, J.; Aizawa, K. Preliminary clinical report on safety and efficacy of photodynamic therapy using talaporfin sodium for malignant gliomas. Photodiagn. Photodyn. Ther. 2012, 9, 91–99. [Google Scholar] [CrossRef]
- Muragaki, Y.; Akimoto, J.; Maruyama, T.; Iseki, H.; Ikuta, S.; Nitta, M.; Maebayashi, K.; Saito, T.; Okada, Y.; Kaneko, S.; et al. Phase II clinical study on intraoperative photodynamic therapy with talaporfin sodium and semiconductor laser in patients with malignant brain tumors. J. Neurosurg. 2013, 119, 845–852. [Google Scholar] [CrossRef]
- Nitta, M.; Muragaki, Y.; Maruyama, T.; Iseki, H.; Komori, T.; Ikuta, S.; Saito, T.; Yasuda, T.; Hosono, J.; Okamoto, S.; et al. Role of photodynamic therapy using talaporfin sodium and a semiconductor laser in patients with newly diagnosed glioblastoma. J. Neurosurg. 2018, 131, 1361–1368. [Google Scholar] [CrossRef]
- Kim, Y.; Kudo, T.; Tamura, K.; Sumita, K.; Kobayashi, D.; Tanaka, Y.; Inaji, M.; Nariai, T.; Ishii, K.; Maehara, T. Clinical findings of thalamic and brain stem glioma including diffuse midline glioma, H3K27M mutant: A clinical study. No Shinkei Geka 2021, 49, 901–908, (In Japanese with English Abstract). [Google Scholar] [PubMed]
- Dalmage, M.; LoPresti, M.A.; Sarkar, P.; Ranganathan, S.; Abdelmageed, S.; Pagadala, M.; Shlobin, N.A.; Lam, S.; DeCuypere, M. Survival and neurological outcomes after stereotactic biopsy of diffuse intrinsic pontine glioma: A systematic review. J. Neurosurg. Pediatr. 2023, 32, 665–672. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Botero, G.; Girty, M.; Mokhtari, K.; Labussiere, M.; Idbaith, A.; Delattre, J.Y.; Laigle-Donadey, F.; Sanson, M. Molecular analysis of diffuse intrinsic gliomas in adults. J. Neurooncol. 2014, 116, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Daoud, E.V.; Rajaram, V.; Cai, C.; Oberle, R.J.; Martin, G.R.; Raisanen, J.M.; White, C.L., 3rd; Foong, C.; Mickey, B.E.; Pan, E.; et al. Adult brain stem gliomas with H3K27M mutation: Radiology, pathology and prognosis. J. Neuropathol. Exp. Neurol. 2018, 77, 302–311. [Google Scholar] [CrossRef]
- Dellaretti, M.; Reyns, N.; Touzet, G.; Dubois, F.; Gusmao, S.; Pereira, J.L.; Blond, S. Diffuse brain stem glioma: Prognostic factors. J. Neurosurg. 2012, 117, 810–814. [Google Scholar] [CrossRef]
- Leibetseder, A.; Leitner, J.; Mair, M.J.; Meckel, S.; Hainfellner, J.A.; Aichholzer, M.; Widhalm, G.; Dickmann, K.; Weis, S.; Furtner, J.; et al. Prognostic factors in adult brainstem glioma: A tertiary care center analysis and review of the literature. J. Neurol. 2022, 269, 1574–1590. [Google Scholar] [CrossRef]
- Faulkner, H.; Arnaout, O.; Hoshide, R.; Young, I.M.; Yeung, J.T.; Sughrue, M.E.; Teo, C. The surgical resection of brainstem glioma: Outcome and prognostic factors. World Neurosurg. 2021, 146, e639–e690. [Google Scholar] [CrossRef]
- Barsouk, A.; Baldassari, M.P.; Khanna, O.; Andrews, C.E.; Ye, D.Y.; Velagapudi, L.; Al Saiegh, F.; Hafazalla, K.; Cunningham, E.; Patel, H.; et al. Glioblastoma with deep supratentorial extension is associated with a worse overall survival. J. Clin. Neurosci. 2021, 93, 82–87. [Google Scholar] [CrossRef]
- Kaneko, S. Photodynamic therapy for human malignant glioma. JJSLSM 2011, 32, 131–138, (In Japanese with English Abstract). [Google Scholar] [CrossRef]
- Beck, T.J.; Kreth, F.W.; Beyer, W.; Mehrkens, J.H.; Obermeier, A.; Stepp, H.; Stummer, W.; Baumgartner, R. Interstitial photodynamic therapy of nonresectable malignant glioma recurrence using 5-aminolevulinic acid induced protoporphyrin IX. Laser Surg. Med. 2007, 39, 386–393. [Google Scholar] [CrossRef]
- Stepp, H.; Stummer, W. 5-ALA in the management of malignant glioma. Laser Surg. Med. 2018, 50, 399–419. [Google Scholar] [CrossRef] [PubMed]
- Foglar, M.; Aumiller, M.; Bochmann, K.; Buchner, A.; El Fahim, M.; Quach, S.; Sroka, R.; Stepp, H.; Thon, N.; Forbrig, R. Interstitial photodynamic therapy of glioblastomas; A long-term follow-up analysis of survival and volumetric MRI data. Cancers 2023, 15, 2603. [Google Scholar] [CrossRef] [PubMed]
- Nagai, K.; Akimoto, J.; Fukami, S.; Saito, Y.; Ogawa, E.; Takanashi, M.; Kuroda, M.; Kohno, M. Efficacy of interstitial photodynamic therapy using talaporfin sodium and a semiconductor laser for a mouse allograft glioma model. Sci. Rep. 2024, 14, 9137. [Google Scholar] [CrossRef]
- Cramer, S.W.; Chen, C.C. Photodynamic therapy for treatment of glioblastoma. Front. Surg. 2020, 6, 81. [Google Scholar] [CrossRef] [PubMed]
- Vermandel, M.; Dupont, C.; Lecomte, F.; Leroy, H.A.; Tuleasca, C.; Mordon, S.; Hadipanayis, C.G.; Reynes, N. Standardized intraoperative 5-ALA photodynamic therapy for newly diagnosed glioblastoma patients: A preliminary analysis of the INDYGO trial. J. Neurooncol. 2021, 152, 501–514. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudi, K.; Garvey, K.L.; Bouras, A.; Cramer, G.; Stepp, H.; Hesu Raj, J.G.; Bozec, D.; Busch, T.M.; Hadipanayis, C.G. 5-aminolevulinic acid photodynamic therapy for the treatment of high-grade gliomas. J. Neurooncol. 2019, 141, 595–607. [Google Scholar] [CrossRef]
- Brain Tumor Registry of Japan (2005–2008). Neurol. Med. Chir. 2017, 57, 9–102. [CrossRef]
- Tsutsumi, M.; Miki, Y.; Akimoto, J.; Haraoka, J.; Aizawa, K.; Hirano, K.; Beppu, M. Photodymamic therapy with talaporfin sodium induced dose-dependent apoptotic cell death in human glioma cell lines. Photodiagn. Photodyn. Ther. 2013, 10, 103–110. [Google Scholar] [CrossRef]
- Miki, Y.; Akimoto, J.; Hiranuma, M.; Fujiwara, Y. Effect of talaporfin-mediated photodynamic therapy on cell death modalities in human glioblastoma T98G cells. J. Toxicol. Sci. 2014, 39, 821–827. [Google Scholar] [CrossRef]
- Miki, Y.; Akimoto, J.; Yokoyama, S.; Homma, T.; Tsutsumi, M.; Haraoka, J.; Hirano, K.; Beppu, M. Photodynamic therapy in combination with talaporfin sodium induces mitochondrial apoptotic cell death accompanied with necrosis in glioma cells. Biol. Pharm. Bull. 2013, 36, 215–221. [Google Scholar] [CrossRef]
- Miki, Y.; Akimoto, J.; Omata, H.; Moritake, K.; Hiranuma, M.; Hironaka, C.; Fujiwara, Y.; Beppu, M. Concomitant treatment with temozolomide enhances apoptotic cell death in glioma cells induced by photodynamic therapy with talaporfin sodium. Photodiagn. Photodyn. Ther. 2014, 11, 556–564. [Google Scholar] [CrossRef] [PubMed]
- Miki, Y.; Akimoto, J.; Moritake, K.; Hironaka, C.; Fujiwara, Y. Photodynamic therapy using talaporfin sodium induces concentration-dependent programmed necroptosis in human glioblastoma T98G cells. Lasers Med. Sci. 2015, 30, 1739–1745. [Google Scholar] [CrossRef] [PubMed]
- Namatame, H.; Akimoto, J.; Matsumura, H.; Haraoka, J.; Aizawa, K. Photodynamic therapy of C6-implanted glioma cells in the rat brain employing second-generation photosensitizer talaporfin sodium. Photodiagn. Photodyn. Ther. 2008, 5, 198–209. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, E.; Arai, T.; Usuda, J.; Otani, K.; Maehara, S.; Imai, K.; Kudo, Y.; Ono, S.; Ikeda, N. Photodynamic treatment using a small diameter diffused light irradiation probe made of plastic optical fiber. JJSLM 2020, 41, 25–29, (In Japanese with English Abstract). [Google Scholar] [CrossRef]
- Moy, W.J.; Patel, S.J.; Lertsakdadet, B.S.; Arora, R.P.; Nielsen, K.M.; Kelly, K.M.; Choi, B. Preclinical in vivo evaluation of Npe6-mediated photodynamic therapy on normal vasculature. Lasers Med. Sci. 2012, 44, 158–162. [Google Scholar] [CrossRef]
- McMahoon, K.S.; Wieman, J.; Moore, P.H.; Fingar, V.H. Effect of photodynamic therapy using mono-L-asparthyl chlorine e6 on vessel constriction, vessel leakage, and tumor response. Cancer Res. 1994, 54, 5374–5379. [Google Scholar]
- Dudzik, T.; Domanski, I.; Makuch, S. The impact of photodynamic therapy on immune system in cancer-an update. Front. Immunol. 2024, 15, 1335920. [Google Scholar] [CrossRef]
- Sasaki, M.; Tanaka, M.; Kojima, Y.; Nishie, H.; Shimura, T.; Kubota, E.; Kataoka, H. Anti-tumor immunity enhancement by photodynamic therapy with talaporfin sodium and anti-programmed death 1 antibody. Mol. Ther. Oncolytics 2023, 28, 118–131. [Google Scholar] [CrossRef]


| Group | N | Energy Density (J/cm2) | Power Density (mW/cm2) | Input Power (mW) | Time (Second) | TPS |
|---|---|---|---|---|---|---|
| A | 5 | 150 | 150 | 8.3 | 1025 | (+) |
| B | 5 | 75 | 73 | 4 | 1025 | (+) |
| C | 5 | 50 | 150 | 8.3 | 334 | (+) |
| D | 5 | 0 | 0 | 0 | 0 | (+) |
| E | 5 | 50 | 150 | 8.3 | 334 | (−) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saito, Y.; Fukami, S.; Nagai, K.; Ogawa, E.; Kuroda, M.; Kohno, M.; Akimoto, J. Cytocidal Effects of Interstitial Photodynamic Therapy Using Talaporfin Sodium and a Semiconductor Laser in a Rat Intracerebral Glioma Model. Biomedicines 2024, 12, 2141. https://doi.org/10.3390/biomedicines12092141
Saito Y, Fukami S, Nagai K, Ogawa E, Kuroda M, Kohno M, Akimoto J. Cytocidal Effects of Interstitial Photodynamic Therapy Using Talaporfin Sodium and a Semiconductor Laser in a Rat Intracerebral Glioma Model. Biomedicines. 2024; 12(9):2141. https://doi.org/10.3390/biomedicines12092141
Chicago/Turabian StyleSaito, Yuki, Shinjiro Fukami, Kenta Nagai, Emiyu Ogawa, Masahiko Kuroda, Michihiro Kohno, and Jiro Akimoto. 2024. "Cytocidal Effects of Interstitial Photodynamic Therapy Using Talaporfin Sodium and a Semiconductor Laser in a Rat Intracerebral Glioma Model" Biomedicines 12, no. 9: 2141. https://doi.org/10.3390/biomedicines12092141







