Narrative Review of the Theoretical–Methodological Foundations of the TREINI Program
Abstract
:1. Introduction
2. Definition and Clinical Epidemiology of CP
3. Biopsychosocial Impacts of CP
3.1. Impairments in Body Structures and Functions
3.2. Activity Limitations
3.3. Restrictions on Participation
3.4. Contextual Barriers and Facilitators
4. Interventions for CP
5. Theoretical Foundations of the TREINI Program
| Component | Description | References |
|---|---|---|
| Family-Centered Practice | TREINI is based on Family-Centered Practice, which recognizes the relevance of family involvement in the process of recovery and child development. This approach promotes active collaboration between healthcare professionals, the child, and their family, ensuring that the family’s needs, values, and preferences are integrated into the planning and implementation of treatment. The importance of this practice lies in creating an environment of support and trust, improving adherence to treatment and enhancing therapeutic results. | Myrhaug, Jahnsen and Østensjø, 2016 [96] King and Chiarello, 2014 [97] King et al., 2004 [98] |
| Family–professional collaboration | Family–professional collaboration is supported by the TRIENI program by facilitating an in-depth understanding of the needs and priorities of the child and family, allowing for the personalization of treatment plans. This effective collaboration improves communication, strengthens mutual trust, and increases satisfaction with the services provided. The family’s active participation in the therapeutic process is essential for the continuity of care at home, which is crucial for the child’s continued evolution. Furthermore, the collaborative approach empowers parents, increasing their skills and confidence in relation to supporting their children’s development, resulting in better functional and emotional outcomes for the child and the family as a whole. | An and Palisano, 2014 [5] King and Chiarello, 2014 [97] Myrhaug, Jahnsen, and Østensjø, 2016 [96] |
| Evidence-based interdisciplinary practice | In the TREINI program, the interdisciplinary team is crucial to providing holistic and effective treatment. Professionals such as physical therapists, occupational therapists, speech therapists, and psychologists collaborate to create a comprehensive and personalized treatment plan. Each specialist addresses different patient needs, from mobility and motor coordination to communication and cognitive skills. Coordination between team members ensures integrated and complementary interventions, maximizing therapeutic results. | Andrade et al., 2012 [99] Das and Ganesh, 2019 [100] Hanson et al., 2024 [101] Rahlin and Rheault, 2024 [95] |
| Biopsychosocial approach | TREINI employs interventions that cover all domains of the International Classification of Functioning, Disability and Health (ICF), ensuring a holistic and comprehensive approach to patient care and rehabilitation. | Chen et al., 2014 [102] Andrade et al., 2012 [99] |
| Naturalistic learning environment | The TREINI program is based on the assumption that interventions carried out in the child’s living environments or in similar contexts promote greater gains and have a greater capacity to generalize these results. | Morgan, Novak, and Badawi, 2013 [103] Rostami and Malamiri, 2012 [104] Dunst et al., 2001 [105] |
| Intensive and prolonged training | The TRIENI program assumes that significant outcomes in terms of body structure and function, and involving tissue remodeling and activity-dependent neuroplasticity, require intense and prolonged interventions. The implementation of intensive programs has been increasingly recommended. For each functional goal, an intervention time of 15 to 25 h is required, depending on the complexity of the goal. TREINI recommends conducting an intensive interdisciplinary intervention, with a workload ranging from 40 to 80 h per month, according to the specific needs of the child. | Bleyenheuft et al., 2015 [106] Figueiredo et al., 2020 [107] Jackman et al., 2021 [108] |
| Best practices in pediatric rehabilitation | The TREINI program is aligned with the most recent scientific evidence, incorporating essential elements to promote functionality in individuals with CP. These elements include goal-directed practice of real-life tasks, active movements self-initiated by the child, application of motor learning principles, creation of an enriched environment, and family participation and involvement in therapeutic planning. | Bak and Lee, 2021 [109] Zai et al., 2022 [110] Novak et al., 2020 [6] Novak et al., 2014 [16] Khamis et al., 2020 [92] Korkalainen et al., 2023 [88] Whittingham et al., 2013 [94] |
| Supervision and continued education | The TREINI program provides online supervision for professionals, in addition to offering continuing education through regularly held courses and conferences. | Snowdon et al., 2016 [111] Coughtrey et al., 2024 [112] |
| Care management through app | TREINI uses a mobile application, TREINI+, designed to efficiently manage interdisciplinary healthcare. The TREINI+ application facilitates the implementation of home programs by providing a tool for therapists to guide families in integrating clinical activities into the home environment, and can be expanded to other living contexts, such as schools, parks, and squares. Furthermore, it allows the family to insert videos or photos of the child or young person carrying out activities in their natural environments, enabling the interdisciplinary team to observe the environment and behavior of the child or young person in activities that are meaningful to them and their family. | Fenning et al., 2022 [113] Zamin et al., 2019 [114] |
6. City of Tomorrow
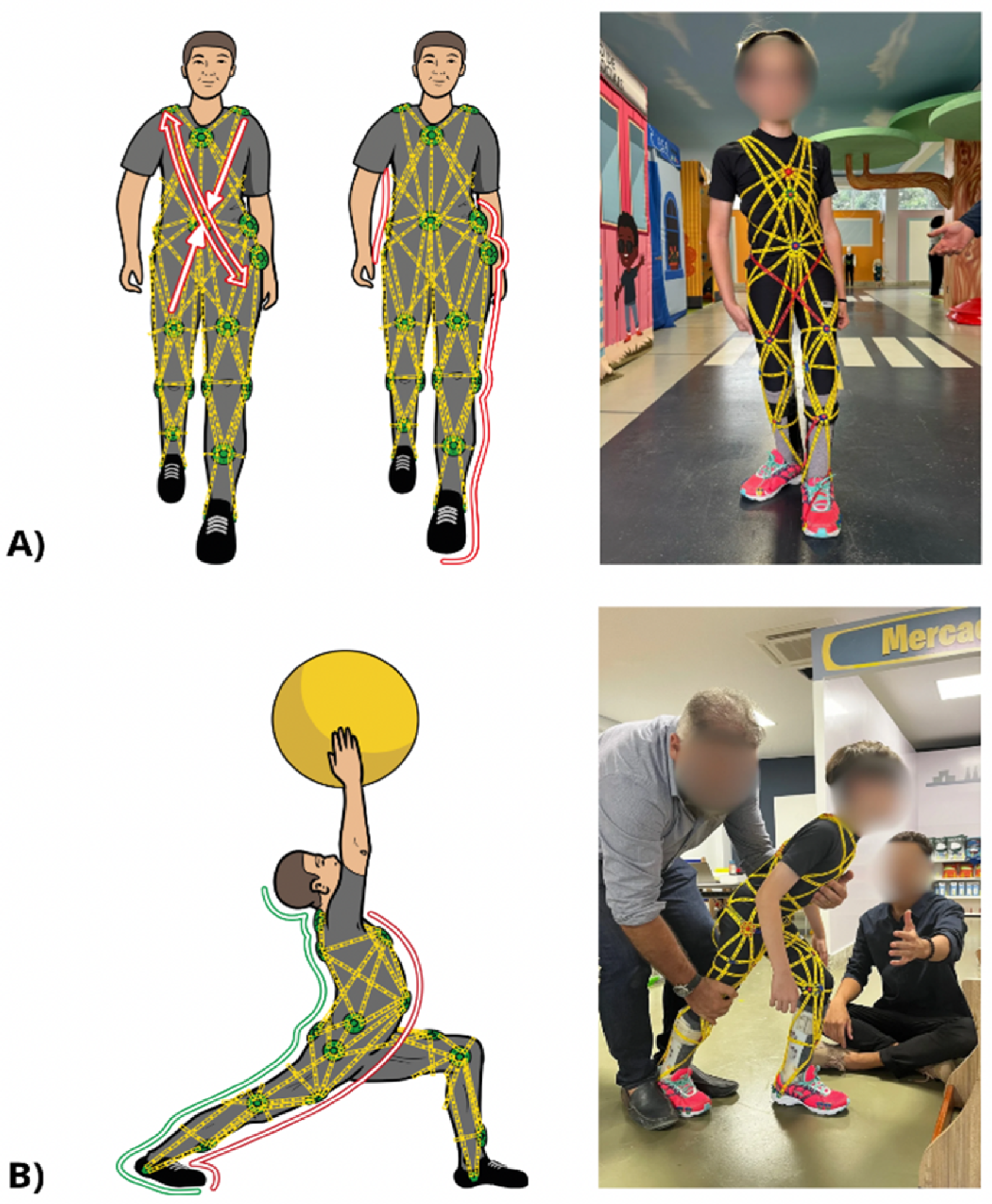
7. Therapeutic Suit (TREINI Exoflex) Based on Myofascial Meridians and Tensegrity
| Study | Objective | Included Studies | Participant Characteristics | Interventions (Suits) | Intervention Intensity | Comparisons | Methodological Quality | Conclusion |
|---|---|---|---|---|---|---|---|---|
| Martins et al., 2015 [142] | Evaluate the effectiveness of the suit on the functionality of children with CP | 4 RCTs published between 2006 and 2011 |
| TheraSuit (1) AdeliSuit (2) Modified suit with emphasis on lower limbs (1) |
| TheraSuit without elastic (1) Bobath (2) CT (1) | Low risk of bias on the PEDro Scale (score of 6.25) | Small improvement in gross motor function, with an effect size of 0.10 |
| Almeida et al., 2017 [132] | Evaluate evidence on the effects of the suit on the impairments and functional limitations of children with CP. | 13 studies published between 2000 and 2015:
|
|
|
|
| Quality varied from low to high as assessed by the Checklist for Measuring Study Quality | The DEFO and TheraTogs suits appear to improve postural alignment and gait performance in children with diplegic CP (evidence ranges from low to very low) |
| Wells, Marquez, and Wakely, 2017 [143] | Verify if suit therapy improves motor function in children with CP. | 16 studies published between 1995 and 2016:
|
|
|
|
| Average 19.5 (out of 27) on the Downs and Black Scale; Variable quality | The use of the suits did not improve motor function. |
| Karadağ-Saygı, and Giray, 2019 [144] | Evaluate the effectiveness of the suit therapy for CP. | 29 studies published between 1995 and 2018:
|
|
|
|
| High: 30%; Moderate: 50%; Low: 20% (Batsford scale) | The results of the RCTs showed that the use of the Suits + CT improved proximal stability, gross motor function, and gait. The other studies corroborated these findings. |
| Study | Methodological Quality * | Aims | Sample Size | Suit Groups | Comparison Groups | Measuring Instrument | Results | ||
|---|---|---|---|---|---|---|---|---|---|
| Sample | Intervention | Sample | Intervention | ||||||
| Emara et al., 2024 [145] | 6/10 | To investigate the effect of TheraTogs on foot pressure distribution, postural control, and endurance in children with CP | 34 | n: 17, Age: 8.57 ± 0.73 years GMFCS: I and II | Use of TheraTogs during ADLs; Parents trained and monitored weekly. Intensity: 8 to 10 h/day, for 12 weeks | n: 17 Age: 8.33 ± 0.61 years GMFCS: I and II | CT based on Bobath principles Intensity: 60 min per session, 3 times/week, for 12 weeks | Foot pressure distribution, Trunk control measurement scale, trunk position sense, 6MWT | Both groups showed significant improvements in all outcomes (p < 0.05). |
| El-Shamy and Kafy, 2021a [146] | 5/10 | To compare the effects of FES and TheraTogs on gait and balance in children with CP | 30 | n: 15, Age: 10.13 ± 1.25 years GMFCS: I and II | TheraTogs (unspecified protocol) + CT Intensity: 2 h/day, 3 times/week, for 3 months | n: 15 Age: 10.53±1.24 years GMFCS: I and II | FES in the fibular muscles + CT Intensity: 2 h/day 3x/week, for 3 months | Pro-Reflex Movement Analysis, Biodex Balance System | Both groups showed significant improvements in all outcomes. There was greater improvement in the FES group (p < 0.05) |
| El-Shamy and Kafy, 2021b [147] | 5/10 | Investigate the effectiveness of TheraTogs on gait pattern in children with CP | 30 | n: 15, Age: 10.13 ± 1.25 years GMFCS: I and II | TheraTogs (unspecified protocol) Intensity: 12 h/day. | n: 15 Age: 10.53 ± 1.24 years GMFCS: I and II | CT (stretching, strengthening and reflex inhibition). Intensity: 1h/day 3x/week, for 3 months | Pro-Reflex Movement Analysis | Both groups showed significant improvements in gait parameters. There was greater improvement in the TheraTogs group (p < 0.05) |
| El-Bagalaty and Ismaeel, 2021 [148] | 4/10 | Compare the use of Suit Therapy and whole-body vibration on the bone mineral density of children with CP | 46 | n: 23, Age: 5.13 ± 0.74 years GMFCS: NI | Use of the suit during progressive standing exercises + CT Intensity: 3 times/week, for 12 weeks | n: 23 Age: 5.0 ± 0.84 years GMFCS: NR | Whole-Body Vibration Training with Horizontal Displacements + CT Intensity: 20 min per session, 3x/week, for 12 weeks | Bone mineral density in the lumbar spine and femoral neck. | Bone mineral density improved in the whole-body vibration therapy group but not in the Suit therapy group (p < 0.05) |
8. TREINI Program Evaluation Strategy
| Outcome | Instrument | Description | References |
|---|---|---|---|
| Body structure and function | |||
| General cognitive ability | Raven’s Coloured Progressive Matrices | An assessment consisting of 36 items, used to estimate non-verbal reasoning in children. | Angelini et al., 1999 [152] |
| Muscle strength | Functional Strength Assessment (FSA) | Assesses the strength of the major muscle groups in children from 18 months onwards. | Jeffries et al., 2019 [153] |
| Range of motion | Spinal Alignment and Range of Motion Measure (SAROMM) | Provides an estimate of the overall spinal alignment and the range of motion and muscle extensibility in children with CP. | Jeffries et al., 2019 [153] |
| Balance | Pediatric balance scale (PBS) | A measure consisting of 14 items that assesses functional balance in the context of daily activities. | Franjoine et al., 2003 [154] |
| Orofacial motricity | Orofacial Myofunctional Evaluation Protocol with Scores (AMIOFE) | A structured set of procedures and criteria used to examine and document orofacial functions such as chewing, swallowing, breathing, articulation, and the posture of facial and oral muscles. | Felício et al., 2012 [155] |
| Hearing | Simplified Auditory Processing Assessment (ASPA) | Used to verify the efficiency with which an individual processes auditory information. It also identifies possible auditory processing disorders which may impair the ability to understand and interpret sounds. | Carvalho et al., 2019 [156] |
| Activity and Participation | |||
| Goal achievement | Goal attainment scale (GAS) | Quantifies the achievement of goals set during an intervention program. | Kiresuk et al., 2014 [157] |
| Occupational performance | Canadian Occupational Performance Measure (COPM) | Assesses performance in daily activities in the areas of self-care, productivity, and leisure. It detects changes in performance over time and after intervention. | Law et al., 1990 [158] |
| Functionality | Pediatric Evaluation of Disability Inventory–Computer Adaptive Test (PEDI-CAT) | A computerized assessment tool, based on caregiver reports, that measures daily activities, mobility, social/cognitive aspects, and responsibility. It aims to identify functional delays and assess a child’s individual progress after therapeutic interventions. | Haley et al., 2012 [159] |
| Gross motor function | Gross Motor Function Measure (GMFM) | Measures the ability to perform activities such as lying down, rolling, sitting, crawling, standing, and walking. | Russell et al., 1989 [160] |
| Behavior | Child Behavior Checklist (CBCL) | Assesses behavioral and emotional problems in children and adolescents. | Bordin et al., 2013 [161] |
| Gait speed | 10 m walk test (10MWT) | A simple assessment used to measure locomotor capacity in clinical and research settings. | Chrysagis, Skordilis, and Koutsouki, 2014 [162] |
| Mobility | Timed Up and Go (TUG) | Assesses gait and dynamic balance in children and adolescents. | Martín-Díaz et al., 2023 [163] |
| Manual dexterity | Nine-hole peg test (9HPT) | A standardized test that quantitatively assesses finger dexterity. | Poole et al., 2005 [164] |
| Behavior | Behavioral observation protocol (PROC) | A structured set of guidelines and procedures used to record and analyze the behavior of individuals in a specific environment. | Hage et al., 2012 [165] |
| Learning | School performance test (TDE) | A standardized tool used to assess the academic performance of students in various areas of knowledge. | Knijnik, Giacomoni, and Stein, 2013 [166] |
| Contextual factors | |||
| Environmental | Craig Hospital Inventory of Environmental Factors (CHIEF) | Used to document the impact of environmental factors on the social participation of people with disabilities. | Furtado et al., 2014 [167] |
| Life history | Autobiography | A tool for self-exploration and understanding of an individual’s identity, based on their life history, with the potential to reveal patterns of behavior, beliefs, and values, as well as promote self-awareness. | Sommer, 2003 [168] |
| Classification systems | |||
| Gross motor function | Gross Motor Function Classification System (GMFCS) | A five-point classification system used to describe the capacity of gross motor function in children with CP. | Palisano et al., 1997 [11] |
| Manual ability | Manual Ability Classification System (MACS) | A five-point classification system used to classify the manual abilities of children and adolescents with CP. | Eliasson et al., 2006 [12] |
| Communication | Communication Function Classification System (CFCS) | A five-point classification system used to classify the communicative function of children and adolescents with CP. | Hidecker et al., 2011 [169] |
| Mobility | Functional Strength Assessment (FMS) | A scale used to classify functional mobility in children and adolescents with CP. It takes into account the variety of assistive equipment that can be used. | Graham et al., 2004 [170] |
9. Challenges and Strategies for Implementing the TREINI Program Effectively
10. Final Considerations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Rosenbaum, P.; Gorter, J.W. The ‘F-words’ in childhood disability: I swear this is how we should think! Child Care Health Dev. 2012, 38, 457–463. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability and Health (ICF); World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Longo, E.; de Campos, A.C.; Palisano, R.J. Let’s make pediatric physical therapy a true evidence-based field! Can we count on you? Braz. J. Phys. Ther. 2019, 23, 187–188. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Adolph, K.E.; Hoch, J.E. Motor Development: Embodied, Embedded, Enculturated, and Enabling. Annu. Rev. Psychol. 2019, 70, 141–164. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- An, M.; Palisano, R.J. Family-professional collaboration in pediatric rehabilitation: A practice model. Disabil. Rehabil. 2014, 36, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Novak, I.; Morgan, C.; Fahey, M.; Finch-Edmondson, M.; Galea, C.; Hines, A.; Langdon, K.; Namara, M.M.; Paton, M.C.; Popat, H.; et al. State of the Evidence Traffic Lights 2019: Systematic Review of Interventions for Preventing and Treating Children with Cerebral Palsy. Curr. Neurol. Neurosci. Rep. 2020, 20, 3. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vining, R.D.; Gosselin, D.M.; Thurmond, J.; Case, K.; Bruch, F.R. Interdisciplinary rehabilitation for a patient with incomplete cervical spinal cord injury and multimorbidity: A case report. Medicine 2017, 96, e7837. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. Suppl. 2007, 109, 8–14, Erratum in Dev. Med. Child Neurol. 2007, 49, 480. [Google Scholar] [PubMed]
- McIntyre, S.; Morgan, C.; Walker, K.; Novak, I. Cerebral palsy—Don’t delay. Dev. Disabil. Res. Rev. 2011, 17, 114–129. [Google Scholar] [CrossRef] [PubMed]
- Graham, H.K.; Harvey, A.; Rodda, J.; Nattrass, G.R.; Pirpiris, M. The Functional Mobility Scale (FMS). J. Pediatr. Orthop. 2004, 24, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Eliasson, A.C.; Krumlinde-Sundholm, L.; Rösblad, B.; Beckung, E.; Arner, M.; Ohrvall, A.M.; Rosenbaum, P. The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Dev. Med. Child Neurol. 2006, 48, 549–554. [Google Scholar] [CrossRef] [PubMed]
- Paulson, A.; Vargus-Adams, J. Overview of four functional classification systems commonly used in cerebral palsy. Children 2017, 4, 10. [Google Scholar] [CrossRef]
- Palisano, R.J.; Rosenbaum, P.; Bartlett, D.; Livingston, M.H. Content validity of the expanded and revised Gross Motor Function Classification System. Dev. Med. Child Neurol. 2008, 50, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.R.; Neelakantan, M.; Pandher, K.; Merrick, J. Cerebral palsy in children: A clinical overview. Transl. Pediatr. 2020, 9 (Suppl. 1), S125–S135. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Novak, I. Evidence-based diagnosis, health care, and rehabilitation for children with cerebral palsy. J. Child Neurol. 2014, 29, 1141–1156. [Google Scholar] [CrossRef] [PubMed]
- Odding, E.; Roebroeck, M.E.; Stam, H.J. The epidemiology of cerebral palsy: Incidence, impairments and risk factors. Disabil. Rehabil. 2006, 28, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Galea, C.; Mcintyre, S.; Smithers-Sheedy, H.; Reid, S.M.; Gibson, C.; Delacy, M.; Watson, L.; Goldsmith, S.; Badawi, N.; Blair, E.; et al. Cerebral palsy trends in Australia (1995–2009): A population-based observational study. Dev. Med. Child Neurol. 2019, 61, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Khandaker, G.; Smithers-Sheedy, H.; Islam, J.; Alam, M.; Jung, J.; Novak, I.; Booy, R.; Jones, C.; Badawi, N.; Muhit, M. Bangladesh Cerebral Palsy Register (BCPR): A pilot study to develop a national cerebral palsy (CP) register with surveillance of children for CP. BMC Neurol. 2015, 15, 173. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moreau, N.G.; Lieber, R.L. Effects of voluntary exercise on muscle structure and function in cerebral palsy. Dev. Med. Child Neurol. 2022, 64, 700–708. [Google Scholar] [CrossRef] [PubMed]
- Damiano, D.L.; Abel, M.F. Functional outcomes of strength training in spastic cerebral palsy. Arch. Phys. Med. Rehabil. 1998, 79, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Barber, L.; Carty, C.; Modenese, L.; Walsh, J.; Boyd, R.; Lichtwark, G. Medial gastrocnemius and soleus muscle-tendon unit, fascicle, and tendon interaction during walking in children with cerebral palsy. Dev. Med. Child Neurol. 2017, 59, 843–851. [Google Scholar] [CrossRef]
- Lieber, R.L.; Fridén, J. Morphologic and mechanical basis of muscle stiffness and weakness in cerebral palsy. Muscle Nerve 2002, 25, 528–535. [Google Scholar]
- Smith, L.R.; Lee, K.S.; Ward, S.R.; Chambers, H.G.; Lieber, R.L. Hamstring contractures in children with spastic cerebral palsy result from a stiffer extracellular matrix and increased in vivo sarcomere length. J. Physiol. 2011, 589 Pt 10, 2625–2639. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Thompson, N.; Stebbins, J.; Seniorou, M.; Newham, D. Muscle strength and walking ability in diplegic cerebral palsy: Implications for assessment and management. Gait Posture 2011, 33, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Lieber, R.L.; Theologis, T. Muscle-tendon unit in children with cerebral palsy. Dev. Med. Child Neurol. 2021, 63, 908–913. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.T.J.A.; Jiang, Y.Q.; Martin, J.H. Motor system plasticity after unilateral injury in the developing brain. Dev. Med. Child Neurol. 2017, 59, 1224–1229. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Howard, J.J.; Herzog, W. Skeletal Muscle in Cerebral Palsy: From Belly to Myofibril. Front. Neurol. 2021, 12, 620852. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Booth, C.M.; Cortina-Borja, M.J.; Theologis, T.N. Collagen accumulation in muscles of children with cerebral palsy and correlation with severity of spasticity. Dev. Med. Child Neurol. 2001, 43, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Robin, J.; Graham, H.K.; Selber, P.; Dobson, F.; Smith, K.; Baker, R. Proximal femoral geometry in cerebral palsy: A population-based cross-sectional study. J. Bone Jt. Surg. Br. 2008, 90, 1372–1379. [Google Scholar] [CrossRef] [PubMed]
- Wordie, S.J.; Robb, J.E.; Hägglund, G.; Bugler, K.E.; Gaston, M.S. Hip displacement and dislocation in a total population of children with cerebral palsy in Scotland. Bone Jt. J. 2020, 102, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.W.; Morgan, E.; Shelton, J.E.; Thorogood, C. Cerebral palsy: Introduction and diagnosis (part I). J. Pediatr. Health Care 2007, 21, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Dimitrijević, L.; Čolović, H.; Spalević, M.; Stanković, A.; Zlatanović, D.; Cvetković, B. Assessment and treatment of spasticity in children with cerebral palsy. Acta Fac. Medicae Naissensis 2014, 31, 163–169. [Google Scholar] [CrossRef]
- Saether, R.; Helbostad, J.L.; Riphagen, I.I.; Vik, T. Clinical tools to assess balance in children and adults with cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2013, 55, 988–999. [Google Scholar] [CrossRef] [PubMed]
- Dewar, R.; Love, S.; Johnston, L.M. Exercise interventions improve postural control in children with cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2015, 57, 504–520. [Google Scholar] [CrossRef] [PubMed]
- Pierret, J.; Caudron, S.; Paysant, J.; Beyaert, C. Impaired postural control of axial segments in children with cerebral palsy. Gait Posture 2021, 86, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Wingert, J.R.; Burton, H.; Sinclair, R.J.; Brunstrom, J.E.; Damiano, D.L. Joint-position sense and kinesthesia in cerebral palsy. Arch. Phys. Med. Rehabil. 2009, 90, 447–453. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Helenius, I.J.; Viehweger, E.; Castelein, R.M. Cerebral palsy with dislocated hip and scoliosis: What to deal with first? J. Child Orthop. 2020, 14, 24–29. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stadskleiv, K. Cognitive functioning in children with cerebral palsy. Dev. Med. Child Neurol. 2020, 62, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Himmelmann, K.; Beckung, E.; Hagberg, G.; Uvebrant, P. Gross and fine motor function and accompanying impairments in cerebral palsy. Dev. Med. Child Neurol. 2006, 48, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Reid, S.M.; Meehan, E.M.; Arnup, S.J.; Reddihough, D.S. Intellectual disability in cerebral palsy: A population-based retrospective study. Dev. Med. Child Neurol. 2018, 60, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Sakash, A.; Broman, A.T.; Rathouz, P.J.; Hustad, K.C. Executive function in school-aged children with cerebral palsy: Relationship with speech and language. Res. Dev. Disabil. 2018, 78, 136–144. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Christ, S.E.; White, D.A.; Brunstrom, J.E.; Abrams, R.A. Inhibitory control following perinatal brain injury. Neuropsychology 2003, 17, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Weierink, L.; Vermeulen, R.J.; Boyd, R.N. Brain structure and executive functions in children with cerebral palsy: A systematic review. Res. Dev. Disabil. 2013, 34, 1678–1688. [Google Scholar] [CrossRef] [PubMed]
- Bottcher, L.; Flachs, E.M.; Uldall, P. Attentional and executive impairments in children with spastic cerebral palsy. Dev. Med. Child Neurol. 2010, 52, e42–e47. [Google Scholar] [CrossRef] [PubMed]
- Bax, M.; Tydeman, C.; Flodmark, O. Clinical and MRI correlates of cerebral palsy: The European Cerebral Palsy Study. JAMA 2006, 296, 1602–1608. [Google Scholar] [CrossRef] [PubMed]
- Menezes, E.D.C.; Santos, F.A.H.; Alves, F.L. Cerebral palsy dysphagia: A systematic review. Rev. CEFAC 2017, 19, 565–574. [Google Scholar] [CrossRef]
- Sherman, V.; Greco, E.; Moharir, M.; Beal, D.; Thorpe, K.; Martino, R. Feeding and swallowing impairment in children with stroke and unilateral cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2019, 61, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Benfer, K.A.; Weir, K.A.; Bell, K.L.; Ware, R.S.; Davies, P.S.; Boyd, R.N. Oropharyngeal dysphagia in preschool children with cerebral palsy: Oral phase impairments. Res. Dev. Disabil. 2014, 35, 3469–3481. [Google Scholar] [CrossRef] [PubMed]
- Penner, M.; Xie, W.Y.; Binepal, N.; Switzer, L.; Fehlings, D. Characteristics of pain in children and youth with cerebral palsy. Pediatrics 2013, 132, e407–e413. [Google Scholar] [CrossRef] [PubMed]
- García, C.C.; Alcocer-Gamboa, A.; Ruiz, M.P.; Caballero, I.M.; Faigenbaum, A.D.; Esteve-Lanao, J.; Saiz, B.M.; Lorenzo, T.M.; Lara, S.L. Metabolic, cardiorespiratory, and neuromuscular fitness performance in children with cerebral palsy: A comparison with healthy youth. J. Exerc. Rehabil. 2016, 12, 124–131. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Galli, J.; Loi, E.; Molinaro, A.; Calza, S.; Franzoni, A.; Micheletti, S.; Rossi, A.; Semeraro, F.; Fazzi, E.; CP Collaborative Group. Age-Related Effects on the Spectrum of Cerebral Visual Impairment in Children with Cerebral Palsy. Front. Hum. Neurosci. 2022, 16, 750464. [Google Scholar] [CrossRef] [PubMed]
- Weir, F.W.; Hatch, J.L.; McRackan, T.R.; Wallace, S.A.; Meyer, T.A. Hearing Loss in Pediatric Patients with Cerebral Palsy. Otol. Neurotol. 2018, 39, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, A.; Büğüşan, S.; Kara, Ö.K. Impairments, activity limitations, and participation restrictions of the international classification of functioning, disability, and health model in children with ambulatory cerebral palsy. Saudi Med. J. 2017, 38, 176–185. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Beckung, E.; Hagberg, G. Neuroimpairments, activity limitations, and participation restrictions in children with cerebral palsy. Dev. Med. Child Neurol. 2002, 44, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Öhrvall, A.M.; Eliasson, A.C.; Löwing, K.; Ödman, P.; Krumlinde-Sundholm, L. Self-care and mobility skills in children with cerebral palsy, related to their manual ability and gross motor function classifications. Dev. Med. Child Neurol. 2010, 52, 1048–1055. [Google Scholar] [CrossRef] [PubMed]
- Blank, R.; Hermsdörfer, J. Basic motor capacity in relation to object manipulation and general manual ability in young children with spastic cerebral palsy. Neurosci. Lett. 2009, 450, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Andersen, G.; Mjøen, T.R.; Vik, T. Prevalence of speech problems and the use of augmentative and alternative communication in children with cerebral palsy: A registry-based study in Norway. Perspect. Augment. Altern. Commun. 2010, 19, 1–28. [Google Scholar] [CrossRef]
- Critten, V.; Campbell, E.; Farran, E.; Messer, D. Visual perception, visual-spatial cognition and mathematics: Associations and predictions in children with cerebral palsy. Res. Dev. Disabil. 2018, 80, 180–191. [Google Scholar] [CrossRef] [PubMed]
- Wotherspoon, J.; Whittingham, K.; Sheffield, J.; Boyd, R.N. Cognition and learning difficulties in a representative sample of school-aged children with cerebral palsy. Res. Dev. Disabil. 2023, 138, 104504. [Google Scholar] [CrossRef] [PubMed]
- Brossard-Racine, M.; Hall, N.; Majnemer, A.; Shevell, M.I.; Law, M.; Poulin, C.; Rosenbaum, P. Behavioural problems in school age children with cerebral palsy. Eur. J. Paediatr. Neurol. 2012, 16, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Chiarello, L.A.; Palisano, R.J.; Avery, L.; Hanna, S.; On Track Study Team. Longitudinal Trajectories and Reference Percentiles for Participation in Family and Recreational Activities of Children with Cerebral Palsy. Phys. Occup. Ther. Pediatr. 2021, 41, 18–37. [Google Scholar] [CrossRef] [PubMed]
- Souto, D.O.; Cardoso de Sa, C.D.S.; de Lima Maciel, F.K.; Vila-Nova, F.; Gonçalves de Souza, M.; Guimarães Ferreira, R.; Longo, E.; Leite, H.R. I Would Like to Do It Very Much! Leisure Participation Patterns and Determinants of Brazilian Children and Adolescents with Physical Disabilities. Pediatr. Phys. Ther. 2023, 35, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Shields, N.; Synnot, A.J.; Barr, M. Perceived barriers and facilitators to physical activity for children with disability: A systematic review. Br. J. Sports Med. 2012, 46, 989–997. [Google Scholar] [CrossRef] [PubMed]
- Carlon, S.L.; Taylor, N.F.; Dodd, K.J.; Shields, N. Differences in habitual physical activity levels of young people with cerebral palsy and their typically developing peers: A systematic review. Disabil. Rehabil. 2013, 35, 647–655. [Google Scholar] [CrossRef] [PubMed]
- Alves, M.L.F.; Souto, D.O.; Romeros, A.C.S.F.; Magalhães, E.D.D.; Mendes, L.G.; Ayupe, K.M.A.; Chagas, P.S.C.; Campos, A.C.; Moreira, R.S.; Toledo, A.M.; et al. Characterization of environmental factors in children and adolescents with cerebral palsy in Minas Gerais: Participa Minas. Rev. Paul. Pediatr. 2024, 42, e2023043. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Massey, J.; Harniess, P.; Chinn, D.; Robert, G. Barriers and facilitators to parent-delivered interventions for children with or infants at risk of cerebral palsy. An integrative review informed by behaviour change theory. Disabil. Rehabil. 2024, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Earde, P.T.; Praipruk, A.; Rodpradit, P.; Seanjumla, P. Facilitators and Barriers to Performing Activities and Participation in Children with Cerebral Palsy: Caregivers’ Perspective. Pediatr. Phys. Ther. 2018, 30, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Pashmdarfard, M.; Richards, L.G.; Amini, M. Factors Affecting Participation of Children with Cerebral Palsy in Meaningful Activities: Systematic Review. Occup. Ther. Health Care 2021, 35, 442–479. [Google Scholar] [CrossRef] [PubMed]
- Souto, D.O.; de Sousa, M.O.; Ferreira, R.G.; Brandão, A.C.; Carrera, P.B.; Leite, H.R. What are the barriers and facilitators to participation of people with Down syndrome? A scoping review. Dev. Med. Child Neurol. 2024, 66, 1013–1030. [Google Scholar] [CrossRef] [PubMed]
- Badia, M.; Orgaz, B.; Gómez-Vela, M.; Longo, E. Environmental needs and facilitators available for children and adolescents with cerebral palsy: Adaptation and validation of the European Child Environment Questionnaire (ECEQ) Spanish version. Disabil. Rehabil. 2014, 36, 1536–1548. [Google Scholar] [CrossRef] [PubMed]
- Gilmour, A.F.; Fuchs, D.; Wehby, J.H. Are Students with Disabilities Accessing the Curriculum? A Meta-Analysis of the Reading Achievement Gap Between Students with and without Disabilities. Except. Child. 2019, 85, 329–346. [Google Scholar] [CrossRef]
- Novak, I.; McIntyre, S.; Morgan, C.; Campbell, L.; Dark, L.; Morton, N.; Stumbles, E.; Wilson, S.A.; Goldsmith, S. A systematic review of interventions for children with cerebral palsy: State of the evidence. Dev. Med. Child Neurol. 2013, 55, 885–910. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, E.; Salam, R.A.; Middleton, P.; Makrides, M.; McIntyre, S.; Badawi, N.; Crowther, C.A. Antenatal and intrapartum interventions for preventing cerebral palsy: An overview of Cochrane systematic reviews. Cochrane Database Syst. Rev. 2017, 8, CD012077. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Zhang, C.; Gu, J.; Wu, W.; Shen, Z.; Zhou, X.; Lu, H. A randomized, placebo-controlled trial of human umbilical cord blood mesenchymal stem cell infusion for children with cerebral palsy. Cell Transpl. 2018, 27, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Kahraman, A.; Seyhan, K.; Değer, Ü.; Kutlutürk, S.; Mutlu, A. Should botulinum toxin A injections be repeated in children with cerebral palsy? A systematic review. Dev. Med. Child Neurol. 2016, 58, 910–917. [Google Scholar] [CrossRef]
- Armstrong, E.L.; Boyd, R.N.; Horan, S.A.; Kentish, M.J.; Ware, R.S.; Carty, C.P. Functional electrical stimulation cycling, goal-directed training, and adapted cycling for children with cerebral palsy: A randomized controlled trial. Dev. Med. Child Neurol. 2020, 62, 1406–1413. [Google Scholar] [CrossRef] [PubMed]
- Toovey, R.; Bernie, C.; Harvey, A.R.; McGinley, J.L.; Spittle, A.J. Task-specific gross motor skills training for ambulant school-aged children with cerebral palsy: A systematic review. BMJ Paediatr. Open. 2017, 1, e000078. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tinderholt Myrhaug, H.; Østensjø, S.; Larun, L.; Odgaard-Jensen, J.; Jahnsen, R. Intensive training of motor function and functional skills among young children with cerebral palsy: A systematic review and meta-analysis. BMC Pediatr. 2014, 14, 292. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ramey, S.L.; DeLuca, S.C.; Stevenson, R.D.; Conaway, M.; Darragh, A.R.; Lo, W.; CHAMP. Constraint-Induced Movement Therapy for Cerebral Palsy: A Randomized Trial. Pediatrics 2021, 148, e2020033878. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, R.G.; Yang, C.N.; Qu, Y.L.; Koduri, M.P.; Chien, C.W. Effectiveness of hand-arm bimanual intensive training on upper extremity function in children with cerebral palsy: A systematic review. Eur. J. Paediatr. Neurol. 2020, 25, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Mandak, K.; Light, J.; Boyle, S. The effects of literacy interventions on single-word reading for individuals who use aided AAC: A systematic review. Augment. Altern. Commun. 2018, 34, 206–218. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.; Novak, I.; Dale, R.C.; Guzzetta, A.; Badawi, N. Single blind randomised controlled trial of GAME (Goals—Activity—Motor Enrichment) in infants at high risk of cerebral palsy. Res. Dev. Disabil. 2016, 55, 256–267. [Google Scholar] [CrossRef] [PubMed]
- Polatajko, H.J.; Mandich, A.D.; Miller, L.T.; Macnab, J.J. Cognitive orientation to daily occupational performance (CO-OP): Part II—The evidence. Phys. Occup. Ther. Pediatr. 2001, 20, 83–106. [Google Scholar] [CrossRef] [PubMed]
- King, G.; Currie, M.; Bartlett, D.J.; Gilpin, M.; Willoughby, C.; Tucker, M.A.; Strachan, D.; Baxter, D. The development of expertise in pediatric rehabilitation therapists: Changes in approach, self-knowledge, and use of enabling and customizing strategies. Dev. Neurorehabil. 2007, 10, 223–240. [Google Scholar] [CrossRef] [PubMed]
- Levy, E.S.; Chang, Y.M.; Hwang, K.; McAuliffe, M.J. Perceptual and Acoustic Effects of Dual-Focus Speech Treatment in Children with Dysarthria. J. Speech Lang. Hear. Res. 2021, 64, 2301–2316. [Google Scholar] [CrossRef] [PubMed]
- Carl, M.; Levy, E.S.; Icht, M. Speech treatment for Hebrew-speaking adolescents and young adults with developmental dysarthria: A comparison of mSIT and Beatalk. Int. J. Lang. Commun. Disord. 2022, 57, 660–679. [Google Scholar] [CrossRef] [PubMed]
- Korkalainen, J.; McCabe, P.; Smidt, A.; Morgan, C. Motor Speech Interventions for Children with Cerebral Palsy: A Systematic Review. J. Speech Lang. Hear. Res. 2023, 66, 110–125. [Google Scholar] [CrossRef] [PubMed]
- Ward, R.; Leitão, S.; Strauss, G. An evaluation of the effectiveness of PROMPT therapy in improving speech production accuracy in six children with cerebral palsy. Int. J. Speech Lang. Pathol. 2014, 16, 355–371. [Google Scholar] [CrossRef] [PubMed]
- Avagyan, A.; Mkrtchyan, H.; Shafa, F.A.; Mathew, J.A.; Petrosyan, T. Eficácia e variáveis determinantes de intervenções de comunicação aumentativa e alternativa em pacientes com paralisia cerebral com déficit de comunicação: Uma revisão sistemática. Codas 2021, 33, e20200244. [Google Scholar] [CrossRef] [PubMed]
- Long, H.L.; Mahr, T.J.; Natzke, P.; Rathouz, P.J.; Hustad, K.C. Longitudinal change in speech classification between 4 and 10 years in children with cerebral palsy. Dev. Med. Child Neurol. 2022, 64, 1096–1105. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Khamis, A.; Novak, I.; Morgan, C.; Tzannes, G.; Pettigrew, J.; Cowell, J.; Badawi, N. Motor Learning Feeding Interventions for Infants at Risk of Cerebral Palsy: A Systematic Review. Dysphagia 2020, 35, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Parkes, J.; White-Koning, M.; Dickinson, H.O.; Thyen, U.; Arnaud, C.; Beckung, E.; Fauconnier, J.; Marcelli, M.; McManus, V.; Michelsen, S.I.; et al. Psychological problems in children with cerebral palsy: A cross-sectional European study. J. Child Psychol. Psychiatry 2008, 49, 405–413. [Google Scholar] [CrossRef]
- Whittingham, K.; Wee, D.; Sanders, M.R.; Boyd, R. Predictors of psychological adjustment, experienced parenting burden and chronic sorrow symptoms in parents of children with cerebral palsy. Child Care Health Dev. 2013, 39, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Rahlin, M.; Rheault, W. The Interdisciplinary Team and Effective Interprofessional Collaboration in Health Care. In Physical Therapy for Children with Cerebral Palsy; Routledge: London, UK, 2024; pp. 103–110. [Google Scholar]
- Myrhaug, H.T.; Jahnsen, R.; Østensjø, S. Family-centred practices in the provision of interventions and services in primary health care: A survey of parents of preschool children with cerebral palsy. J. Child Health Care 2016, 20, 109–119. [Google Scholar] [CrossRef] [PubMed]
- King, G.; Chiarello, L. Family-centered care for children with cerebral palsy: Conceptual and practical considerations to advance care and practice. J. Child Neurol. 2014, 29, 1046–1054. [Google Scholar] [CrossRef] [PubMed]
- King, S.; Teplicky, R.; King, G.; Rosenbaum, P. Family-centered service for children with cerebral palsy and their families: A review of the literature. Semin. Pediatr. Neurol. 2004, 11, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Andrade, P.M.; Ferreira, F.O.; Mendonça, A.P.; Haase, V.G. Content identification of the interdisciplinary assessment of cerebral palsy using the International Classification of Functioning, Disability and Health as reference. Disabil. Rehabil. 2012, 34, 1790–1801. [Google Scholar] [CrossRef] [PubMed]
- Das, S.P.; Ganesh, G.S. Evidence-based Approach to Physical Therapy in Cerebral Palsy. Indian J. Orthop. 2019, 53, 20–34. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hanson, J.; Sasitharan, A.; Ogourtsova, T.; Majnemer, A. Knowledge translation strategies used to promote evidence-based interventions for children with cerebral palsy: A scoping review. Disabil. Rehabil. 2024, 1–13, Erratum in Disabil. Rehabil. 2024, 1. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.L.; Tseng, M.H.; Shieh, J.Y.; Lu, L.; Huang, C.Y. Determinants of quality of life in children with cerebral palsy: A comprehensive biopsychosocial approach. Res. Dev. Disabil. 2014, 35, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.; Novak, I.; Badawi, N. Enriched environments and motor outcomes in cerebral palsy: Systematic review and meta-analysis. Pediatrics 2013, 132, e735–e746. [Google Scholar] [CrossRef] [PubMed]
- Rostami, H.R.; Malamiri, R.A. Effect of treatment environment on modified constraint-induced movement therapy results in children with spastic hemiplegic cerebral palsy: A randomized controlled trial. Disabil. Rehabil. 2012, 34, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Dunst, C.J.; Trivette, C.M.; Humphries, T.; Raab, M.; Roper, N. Contrasting approaches to natural learning environment interventions. Infants Young Child 2001, 14, 48–63. [Google Scholar] [CrossRef]
- Bleyenheuft, Y.; Ebner-Karestinos, D.; Surana, B.; Paradis, J.; Sidiropoulos, A.; Renders, A.; Friel, K.M.; Brandao, M.; Rameckers, E.; Gordon, A.M. Intensive upper- and lower-extremity training for children with bilateral cerebral palsy: A quasi-randomized trial. Dev. Med. Child Neurol. 2017, 59, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, P.R.P.; Mancini, M.C.; Feitosa, A.M.; Teixeira, C.M.M.F.; Guerzoni, V.P.D.; Elvrum, A.G.; Ferre, C.L.; Gordon, A.M.; BrandÃo, M.B. Hand-arm bimanual intensive therapy and daily functioning of children with bilateral cerebral palsy: A randomized controlled trial. Dev. Med. Child Neurol. 2020, 62, 1274–1282. [Google Scholar] [CrossRef] [PubMed]
- Jackman, M.; Sakzewski, L.; Morgan, C.; Boyd, R.N.; Brennan, S.E.; Langdon, K.; Toovey, R.A.M.; Greaves, S.; Thorley, M.; Novak, I. Interventions to improve physical function for children and young people with cerebral palsy: International clinical practice guideline. Dev. Med. Child Neurol. 2022, 64, 536–549. [Google Scholar] [CrossRef] [PubMed]
- Bak, A.R.; Lee, J.S. A systematic review of task-oriented training to improve the physical function and activities of daily of living of children with cerebral palsy. J. Korean Acad. Sens. Integr. 2011, 19, 54–68. [Google Scholar]
- Zai, W.; Xu, N.; Wu, W.; Wang, Y.; Wang, R. Effect of task-oriented training on gross motor function, balance and activities of daily living in children with cerebral palsy: A systematic review and meta-analysis. Medicine 2022, 101, e31565. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Snowdon, D.A.; Hau, R.; Leggat, S.G.; Taylor, N.F. Does clinical supervision of health professionals improve patient safety? A systematic review and meta-analysis. Int. J. Qual. Health Care 2016, 28, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Coughtrey, A.E.; Bennett, S.D.; Stanick, C.; Chorpita, B.; Dalrymple, E.; Fonagy, P.; Helen Cross, J.; Ford, T.; Heyman, I.; Moss-Morris, R.; et al. Training and supervision of physical health professionals to implement mental health care in paediatric epilepsy clinics. Epilepsy Behav. 2024, 157, 109905. [Google Scholar] [CrossRef] [PubMed]
- Fenning, R.M.; Butter, E.M.; Macklin, E.A.; Norris, M.; Hammersmith, K.J.; McKinnon-Bermingham, K.; Chan, J.; Stephenson, K.G.; Albright, C.; Scherr, J.; et al. Parent Training for Dental Care in Underserved Children with Autism: A Randomized Controlled Trial. Pediatrics 2022, 149, e2021050691. [Google Scholar] [CrossRef]
- Zamin, N.; Norwawi, N.M.; Arshad, N.I.; Rambli, D.R.A. Make me speak: A mobile app for children with cerebral palsy. Int. J. Adv. Trends Comput. Sci. Eng. 2019, 8, 368–373. [Google Scholar] [CrossRef]
- Loffi, R.G.; Cruz, T.K.F.; Paiva, G.M.; Souto, D.O.; Barreto, S.R.; Santana, P.A.N.; Nascimento, A.A.A.C.; Costa, F.R.M.; Cota, E.B.; Haase, V.G. Theoretical-Methodological Foundations for the Global Integration Method (Método de Integração Global-MIG) in the Treatment of Autism Spectrum Disorder. Children 2024, 11, 191. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Loffi, R.G. Exoesqueleto Flexível Baseado nas Linhas Miofasciais e Padrões Geométricos Gerais. Depositante: TREINI Biotecnologia. LTDA. Patente Brasileira BR102018009935-3 A2, 19 November 2019. [Google Scholar]
- Stecco, A.; Giordani, F.; Fede, C.; Pirri, C.; De Caro, R.; Stecco, C. From Muscle to the Myofascial Unit: Current Evidence and Future Perspectives. Int. J. Mol. Sci. 2023, 24, 4527. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.C.; et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA Pediatr. 2017, 171, 897–907, Erratum in JAMA Pediatr. 2017, 171, 919. [Google Scholar] [CrossRef] [PubMed]
- Hadders-Algra, M.; Boxum, A.G.; Hielkema, T.; Hamer, E.G. Effect of early intervention in infants at very high risk of cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2017, 59, 246–258. [Google Scholar] [CrossRef] [PubMed]
- Ko, E.J.; Sung, I.Y.; Moon, H.J.; Yuk, J.S.; Kim, H.S.; Lee, N.H. Effect of Group-Task-Oriented Training on Gross and Fine Motor Function, and Activities of Daily Living in Children with Spastic Cerebral Palsy. Phys. Occup. Ther. Pediatr. 2020, 40, 18–30. [Google Scholar] [CrossRef] [PubMed]
- Novak, I.; Honan, I. Effectiveness of paediatric occupational therapy for children with disabilities: A systematic review. Aust. Occup. Ther. J. 2019, 66, 258–273. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cameron, C.E.; Brock, L.L.; Murrah, W.M.; Bell, L.H.; Worzalla, S.L.; Grissmer, D.; Morrison, F.J. Fine motor skills and executive function both contribute to kindergarten achievement. Child Dev. 2012, 83, 1229–1244. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alexander, K.E.; Clutterbuck, G.L.; Johnston, L.M. Effectiveness of school-based physiotherapy intervention for children. Disabil. Rehabil. 2024, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Santacreu, J. El entrenamiento en autoinstrucciones. In Manual de Técnicas de Terapia y Modificación de Conducta; Caballo, V.E., Ed.; Siglo Veintinuno: Madrid, Spain, 2020; pp. 607–626. [Google Scholar]
- Sousa Junior, R.R.; Souto, D.O.; Camargos, A.C.R.; Clutterbuck, G.L.; Leite, H.R. Moving together is better: A systematic review with meta-analysis of sports-focused interventions aiming to improve physical activity participation in children and adolescents with cerebral palsy. Disabil. Rehabil. 2023, 45, 2398–2408, Erratum in Disabil. Rehabil. 2023, 45, 3033. [Google Scholar] [CrossRef] [PubMed]
- Verschuren, O.; Ketelaar, M.; Gorter, J.W.; Helders, P.J.; Uiterwaal, C.S.; Takken, T. Exercise training program in children and adolescents with cerebral palsy: A randomized controlled trial. Arch. Pediatr. Adolesc. Med. 2007, 161, 1075–1081. [Google Scholar] [CrossRef] [PubMed]
- Hadad, B.S.; Schwartz, S.; Binur, N. Reduced perceptual specialization in autism: Evidence from the other-race face effect. J. Exp. Psychol. Gen. 2019, 148, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Williams, Z.J.; He, J.L.; Cascio, C.J.; Woynaroski, T.G. A review of decreased sound tolerance in autism: Definitions, phenomenology, and potential mechanisms. Neurosci. Biobehav. Rev. 2021, 121, 1–17. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vincent, L.B.; Openden, D.; Gentry, J.A.; Long, L.A.; Matthews, N.L. Promoting Social Learning at Recess for Children with ASD and Related Social Challenges. Behav. Anal. Pract. 2017, 11, 19–33. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Oliveira, V.C. Estabilidade articular da coluna vertebral: Teorias contemporâneas e novos paradigmas. Fisioter. Bras. 2009, 10, 284–289. [Google Scholar] [CrossRef]
- Bar-Haim, S.; Harries, N.; Belokopytov, M.; Frank, A.; Copeliovitch, L.; Kaplanski, J.; Lahat, E. Comparison of efficacy of Adeli suit and neurodevelopmental treatments in children with cerebral palsy. Dev. Med. Child Neurol. 2006, 48, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Almeida, K.M.; Fonseca, S.T.; Figueiredo, P.R.; Aquino, A.A.; Mancini, M.C. Effects of interventions with therapeutic suits (clothing) on impairments and functional limitations of children with cerebral palsy: A systematic review. Braz. J. Phys. Ther. 2017, 21, 307–320. [Google Scholar] [CrossRef]
- Levin, S.M. Theories about spinal loading. Spine 1987, 12, 422–423. [Google Scholar] [CrossRef]
- Levin, S.M. The tensegrity-truss as a model for spine mechanics: Biotensegrity. J. Mech. Med. Biol. 2002, 2, 375–388. [Google Scholar] [CrossRef]
- Ingber, D.E. Tensegrity and mechanotransduction. J. Bodyw. Mov. Ther. 2008, 12, 198–200. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Turvey, M.T.; Fonseca, S.T. The Medium of Haptic Perception: A Tensegrity Hypothesis. J. Mot. Behav. 2014, 46, 143–187. [Google Scholar] [CrossRef]
- Myers, T.W. Anatomy Trains; Churchill Livingstone: Oxford, UK, 2001; 332p. [Google Scholar]
- Stecco, C.; Porzionato, A.; Macchi, V.; Tiengo, C.; Parenti, A.; Aldegheri, R.; Delmas, V.; De Caro, R. Histological characteristics of the deep fascia of the upper limb. Italy J. Anat. Embryol. 2006, 111, 105–110. [Google Scholar]
- Stecco, A.; Macchi, V.; Stecco, C.; Porzionato, A.; Day, J.A.; Delmas, V.; De Caro, R. Anatomical study of myofascial continuity in the anterior region of the upper limb. J. Bodyw. Mov. Ther. 2009, 13, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Schleip, R.; Müller, D.G. Training principles for fascial connective tissues: Scientific foundation and suggested practical applications. J. Bodyw. Mov. Ther. 2013, 17, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Schleip, R.; Bayer, J. Fascial Fitness: How to Be Vital, Elastic and Dynamic in Everyday Life and Sport; Lotus Pub: Lotus, CA, USA, 2017; 224p. [Google Scholar]
- Martins, E.; Cordovil, R.; Oliveira, R.; Letras, S.; Lourenço, S.; Pereira, I.; Ferro, A.; Lopes, I.; Silva, C.R.; Marques, M. Efficacy of suit therapy on functioning in children and adolescents with cerebral palsy: A systematic review and meta-analysis. Dev. Med. Child Neurol. 2016, 58, 348–360. [Google Scholar] [CrossRef] [PubMed]
- Wells, H.; Marquez, J.; Wakely, L. Suit Therapy does not Improve Function in Children with Cerebral Palsy: A Systematic Review. Phys. Occup. Ther. Pediatr. 2018, 38, 395–416. [Google Scholar] [CrossRef] [PubMed]
- Karadağ-Saygı, E.; Giray, E. The clinical aspects and effectiveness of suit therapies for cerebral palsy: A systematic review. Turk. J. Phys. Med. Rehabil. 2019, 65, 93–110. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Emara, H.A.; Al-Johany, A.H.; Khaled, O.A.; Al-Shenqiti, A.M.; Ali, A.R.H.; Aljohani, M.M.; Sobh, E. Effect of the Dynamic Orthotic Suit on Postural Control, and Endurance in Children with Spastic Diplegic Cerebral Palsy: A Randomized Controlled Trial. J. Multidiscip. Healthc. 2024, 17, 419–428. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- El-Shamy, S.M.; El Kafy, E.M.A. Effect of functional electrical stimulation versus TheraTogs on gait and balance in children with hemiplegic cerebral palsy: A randomized controlled trial. Bull. Fac. Phys. Ther. 2021, 26, 38. [Google Scholar] [CrossRef]
- El-Shamy, S.M.; Abd El Kafy, E.M. Efficacy of axial TheraTogs on gait pattern in children with dyskinetic cerebral palsy: A randomized controlled trial. Bull. Fac. Phys. Ther. 2021, 26, 12. [Google Scholar] [CrossRef]
- El-Bagalaty, A.E.; Ismaeel, M.M.I. Suit therapy versus whole-body vibration on bone mineral density in children with spastic diplegia. J. Musculoskelet. Neuronal Interact. 2021, 21, 79–84. [Google Scholar] [PubMed] [PubMed Central]
- Fede, C.; Petrelli, L.; Guidolin, D.; Porzionato, A.; Pirri, C.; Fan, C.; De Caro, R.; Stecco, C. Evidence of a new hidden neural network into deep fasciae. Sci. Rep. 2021, 11, 12623. [Google Scholar] [CrossRef]
- Mackrill, T.; Ebsen, F.; Birkholm Antczak, H.; Leth Svendsen, I. Care planning using SMART criteria in statutory youth social work in Denmark: Reflections, challenges and solutions. Nord. Soc. Work Res. 2018, 8, 64–74. [Google Scholar] [CrossRef]
- Rosenbaum, P.; Stewart, D. The World Health Organization International Classification of Functioning, Disability, and Health: A model to guide clinical thinking, practice and research in the field of cerebral palsy. Semin. Pediatr. Neurol. 2004, 11, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Angelini, A.L.; Alves, I.C.B.; Custdio, E.M.; Duarte, W.F.; Duarte, J.L.M. Manual: Matrizes Progressivas Coloridas de Raven; Centro Editor de Testes e Pesquisas em Psicologia: São Paulo, Brazil, 1999. [Google Scholar]
- Jeffries, L.M.; LaForme Fiss, A.; Westcott McCoy, S.; Bartlett, D.; Avery, L.; Hanna, S.; On Track Study Team. Developmental Trajectories and Reference Percentiles for Range of Motion, Endurance, and Muscle Strength of Children with Cerebral Palsy. Phys. Ther. 2019, 99, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Franjoine, M.R.; Gunther, J.S.; Taylor, M.J. Pediatric balance scale: A modified version of the berg balance scale for the school-age child with mild to moderate motor impairment. Pediatr. Phys. Ther. 2003, 15, 114–128. [Google Scholar] [CrossRef] [PubMed]
- De Felício, C.M.; Medeiros, A.P.; de Oliveira Melchior, M. Validity of the ‘protocol of oro-facial myofunctional evaluation with scores’ for young and adult subjects. J. Oral. Rehabil. 2012, 39, 744–753. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, N.G.; Ubiali, T.; Amaral, M.I.R.D.; Colella-Santos, M.F. Procedures for central auditory processing screening in schoolchildren. Braz. J. Otorhinolaryngol. 2019, 85, 319–328. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kiresuk, T.J.; Smith, A.; Cardillo, J.E. Goal Attainment Scaling: Applications, Theory, and Measurement; Psychology Press: London, UK, 2014. [Google Scholar]
- Law, M.; Baptiste, S.; McColl, M.; Opzoomer, A.; Polatajko, H.; Pollock, N. The Canadian occupational performance measure: An outcome measure for occupational therapy. Can. J. Occup. Ther. 1990, 57, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Haley, S.M.; Coster, W.J.; Dumas, H.M.; Fragala-Pinkham, M.A.; Moed, R. PEDI-CAT: Development, Standardization and Administration Manual; Boston University: Boston, MA, USA, 2012. [Google Scholar]
- Russell, D.J.; Rosenbaum, P.L.; Cadman, D.T.; Gowland, C.; Hardy, S.; Jarvis, S. The gross motor function measure: A means to evaluate the effects of physical therapy. Dev. Med. Child Neurol. 1989, 31, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Bordin, I.A.; Rocha, M.M.; Paula, C.S.; Teixeira, M.C.; Achenbach, T.M.; Rescorla, L.A.; Silvares, E.F. Child Behavior Checklist (CBCL), Youth Self-Report (YSR) and Teacher’s Report Form(TRF): An overview of the development of the original and Brazilian versions. Cad. Saude Publica 2013, 29, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Chrysagis, N.; Skordilis, E.K.; Koutsouki, D. Validity and clinical utility of functional assessments in children with cerebral palsy. Arch. Phys. Med. Rehabil. 2014, 95, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Martín-Díaz, P.; Carratalá-Tejada, M.; Molina-Rueda, F.; Cuesta-Gómez, A. Reliability and agreement of the timed up and go test in children and teenagers with autism spectrum disorder. Eur. J. Pediatr. 2023, 182, 3577–3585. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Poole, J.L.; Burtner, P.A.; Torres, T.A.; McMullen, C.K.; Markham, A.; Marcum, M.L.; Anderson, J.B.; Qualls, C. Measuring dexterity in children using the Nine-hole Peg Test. J. Hand Ther. 2005, 18, 348–351. [Google Scholar] [CrossRef] [PubMed]
- Hage, S.R.D.V.; Pereira, T.C.; Zorzi, J.L. Protocolo de Observação Comportamental-PROC: Valores de referência para uma análise quantitativa. Rev. CEFAC 2022, 14, 677–690. [Google Scholar] [CrossRef]
- Knijnik, L.F.; Giacomoni, C.; Stein, L.M. Teste de Desempenho Escolar: Um estudo de levantamento. Psico-USF 2013, 18, 407–416. [Google Scholar] [CrossRef]
- Furtado, S.R.; Sampaio, R.F.; Vaz, D.V.; Pinho, B.A.; Nascimento, I.O.; Mancini, M.C. Brazilian version of the instrument of environmental assessment Craig Hospital Inventory of Environmental Factors (CHIEF): Translation, cross-cultural adaptation and reliability. Braz. J. Phys. Ther. 2014, 18, 259–267. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sommer, R. The use of autobiography in psychotherapy. J. Clin. Psychol. 2003, 59, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Hidecker, M.J.; Paneth, N.; Rosenbaum, P.L.; Kent, R.D.; Lillie, J.; Eulenberg, J.B.; Chester, K., Jr.; Johnson, B.; Michalsen, L.; Evatt, M.; et al. Developing and validating the Communication Function Classification System for individuals with cerebral palsy. Dev. Med. Child Neurol. 2011, 53, 704–710. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cruz, T.K.F.; Nascimento, A.A.A.C.; Lima, A.F.B.; Oliveira, G.S.; Souto, D.O. Efeitos do Programa TREINI® no desempenho e satisfação de metas funcionais de crianças e adolescentes com paralisia cerebral: Uma análise preliminar. Fisioter. Bras. 2024, 25, 1481–1496. [Google Scholar] [CrossRef]


| Unit | Description | Theoretical–Methodological Foundation | References |
|---|---|---|---|
| Therapeutic suit (TREINI Exoflex) mounting | Spaces to store and assemble the flexible therapeutic suit (TREINI Exoflex). | Promote stability and postural correction, and improve balance, muscle strength, and quality of movements performed. | Loffi, 2019 [116] Stecco et al., 2023 [117] |
| Baby room | Early intervention, including Parental Guidance and Training for the stimulation of socio-emotional, communication, motor, and cognitive skills. | Maximizes child development through integrated and evidence-based strategies, fully exploring the brain plasticity and developmental potential characteristic of the early years of life. | Novak et al., 2017 [118] Hadders-Algra et al., 2017 [119] |
| Home | Training in activities of daily living, transfer and mobility, family literacy and numeracy, as well as socio-emotional, communication, and autobiographical skills. | Stimulates daily living skills through goal-directed and task-specific training. It uses family literacy and numeracy and autobiography as precursors for the development of cognitive and socio-emotional skills, as well as for learning mathematics and reading and writing. | Ko et al., 2020 [120] Novak and Honan, 2019 [121] |
| School | Activities developed through narrative grammar involving literacy and numeracy, socio-emotional skills, postural control, manual function, and functional mobility. | Oral and written activities involving words and numbers are based on cognitive–neuropsychological models of lexical processing. Motor interventions focus on improving motor ability in order to participate in school activities. | Cameron et al., 2012 [122] Alexander et al., 2024 [123] |
| Supermarket | Cognitive and motor planning, motor function training, shopping, socio-emotional and functional communication skills, and learning. | Understanding the cognitive script of grocery shopping allows the child to develop linguistic and conceptual skills in categorization and vocabulary, as well as numerical-arithmetic, social, and planning skills. Skills such as reaching, grasping, trunk rotation, and squatting, among other motor abilities, are also encouraged. | Santacreu, 2020 [124] Ko et al., 2020 [120] |
| Fitness space | Basic physical-sport skills, understanding of rules, and emotional regulation. Communication skills and social interaction related to sports practice. | The child develops basic motor skills, cardiorespiratory conditioning, and participation in group sports. Fundamental skills such as jumping, kicking, running, and throwing are trained, along with socio-emotional skills. | Sousa Junior et al., 2023 [125] Verschuren et al., 2007 [126] |
| Stimulus-control, controlled instability, and fixation rooms | Three stimulus-controlled rooms designed to develop skills in children with concentration difficulties. In each room, the level of support is adjusted, with a gradual increase in stimuli as the support decreases. | Systematic desensitization of stimuli and gradual fading of support for hypersensitivity to environmental stimuli and concentration training. | Hadad and Schwartz, 2019 [127] Williams et al., 2021 [128] |
| Social Rules Gym | Development of social and pragmatic skills. | Aims to develop communication skills, relationship building, understanding and respect for social norms, self-control and emotional regulation, as well as social problem-solving, to improve participants’ social interaction. | Vincent et al., 2017 [129] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loffi, R.G.; Souto, D.O.; Cruz, T.K.F.; Lima, A.F.B.d.; Rocha, F.R.M.C.; Barreto, S.R.; Santana, P.A.N.; Nascimento, A.A.A.C.; Haase, V.G. Narrative Review of the Theoretical–Methodological Foundations of the TREINI Program. Children 2024, 11, 1181. https://doi.org/10.3390/children11101181
Loffi RG, Souto DO, Cruz TKF, Lima AFBd, Rocha FRMC, Barreto SR, Santana PAN, Nascimento AAAC, Haase VG. Narrative Review of the Theoretical–Methodological Foundations of the TREINI Program. Children. 2024; 11(10):1181. https://doi.org/10.3390/children11101181
Chicago/Turabian StyleLoffi, Renato Guimarães, Deisiane Oliveira Souto, Thalita Karla Flores Cruz, Arthur Felipe Barroso de Lima, Fabiana Rachel Martins Costa Rocha, Simone Rosa Barreto, Patrícia Aparecida Neves Santana, Amanda Aparecida Alves Cunha Nascimento, and Vitor Geraldi Haase. 2024. "Narrative Review of the Theoretical–Methodological Foundations of the TREINI Program" Children 11, no. 10: 1181. https://doi.org/10.3390/children11101181





