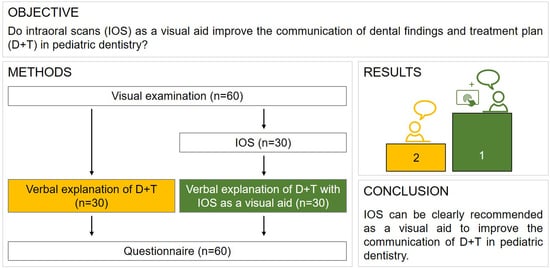
Improving the Communication of Dental Findings in Pediatric Dentistry by Using Intraoral Scans as a Visual Aid: A Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Visual Examination
2.3. Intraoral Scanning
2.4. Explanation of Dental Findings
2.5. Questionnaire
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hibbard, J.H. Engaging health care consumers to improve the quality of care. Med. Care 2003, 41, I61–I70. [Google Scholar] [CrossRef] [PubMed]
- Jafri, Z.; Ahmad, N.; Sawai, M.; Sultan, N.; Bhardwaj, A. Digital Smile Design-An innovative tool in aesthetic dentistry. J. Oral. Biol. Craniofac. Res. 2020, 10, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Bernhard, J.C.; Isotani, S.; Matsugasumi, T.; Duddalwar, V.; Hung, A.J.; Suer, E.; Baco, E.; Satkunasivam, R.; Djaladat, H.; Metcalfe, C.; et al. Personalized 3D printed model of kidney and tumor anatomy: A useful tool for patient education. World J. Urol. 2016, 34, 337–345. [Google Scholar] [CrossRef]
- Glaser, J.; Nouri, S.; Fernandez, A.; Sudore, R.L.; Schillinger, D.; Klein-Fedyshin, M.; Schenker, Y. Interventions to Improve Patient Comprehension in Informed Consent for Medical and Surgical Procedures: An Updated Systematic Review. Med. Decis. Making 2020, 40, 119–143. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, A.M.; Kleinman, D.V. Oral health literacy: The new imperative to better oral health. Dent. Clin. N. Am. 2008, 52, 333–344. [Google Scholar] [CrossRef]
- Rozier, R.G.; Slade, G.D.; Zeldin, L.P.; Wang, H. Parents’ satisfaction with preventive dental care for young children provided by nondental primary care providers. Pediatr. Dent. 2005, 27, 313–322. [Google Scholar] [PubMed]
- Leisenberg, D.; Groß, D. Visualisierungen und Visualisierungsstrategien in der Zahnheilkunde. Ethik Medizin 2017, 29, 23–39. [Google Scholar] [CrossRef]
- Shorey, R.; Moore, K.E. Clinical digital photography today: Integral to efficient dental communications. J. Calif. Dent. Assoc. 2009, 37, 175–177. [Google Scholar]
- Clark, J.M.; Paivio, A. Dual coding theory and education. Educ. Psychol. Rev. 1991, 3, 149–210. [Google Scholar] [CrossRef]
- Coachman, C.; Calamita, M.; Ricci, A. Digital Smile Design: A Digital Tool for Esthetic Evaluation, Team Communication, and Patient Management. In Ronald E. Goldstein’s Esthetics in Dentistry; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2018; pp. 84–111. [Google Scholar] [CrossRef]
- Sousa Dias, N.; Tsingene, F. SAEF—Smile’s Aesthetic Evaluation form: A useful tool to improve communications between clinicians and patients during multidisciplinary treatment. Eur. J. Esthet. Dent. 2011, 6, 160–176. [Google Scholar]
- Schlenz, M.A.; Schupp, B.; Schmidt, A.; Wöstmann, B.; Baresel, I.; Krämer, N.; Schulz-Weidner, N. New Caries Diagnostic Tools in Intraoral Scanners: A Comparative In Vitro Study to Established Methods in Permanent and Primary Teeth. Sensors 2022, 22, 2156. [Google Scholar] [CrossRef] [PubMed]
- Michou, S.; Lambach, M.S.; Ntovas, P.; Benetti, A.R.; Bakhshandeh, A.; Rahiotis, C.; Ekstrand, K.R.; Vannahme, C. Author Correction: Automated caries detection in vivo using a 3D intraoral scanner. Sci. Rep. 2022, 12, 13240. [Google Scholar] [CrossRef]
- Suese, K. Progress in digital dentistry: The practical use of intraoral scanners. Dent. Mater. J. 2020, 39, 52–56. [Google Scholar] [CrossRef]
- Gimenez, T.; Piovesan, C.; Braga, M.M.; Raggio, D.P.; Deery, C.; Ricketts, D.N.; Ekstrand, K.R.; Mendes, F.M. Visual Inspection for Caries Detection: A Systematic Review and Meta-analysis. J. Dent. Res. 2015, 94, 895–904. [Google Scholar] [CrossRef] [PubMed]
- Innes, N.P.T.; Chu, C.H.; Fontana, M.; Lo, E.C.M.; Thomson, W.M.; Uribe, S.; Heiland, M.; Jepsen, S.; Schwendicke, F. A Century of Change towards Prevention and Minimal Intervention in Cariology. J. Dent. Res. 2019, 98, 611–617. [Google Scholar] [CrossRef] [PubMed]
- Pitts, N. Detection, Assessment, Diagnosis and Monitoring of Caries; Karger: Basel, Switzerland, 2009; p. 21. [Google Scholar]
- Kuhnisch, J.; Ekstrand, K.R.; Pretty, I.; Twetman, S.; van Loveren, C.; Gizani, S.; Spyridonos Loizidou, M. Best clinical practice guidance for management of early caries lesions in children and young adults: An EAPD policy document. Eur. Arch. Paediatr. Dent. 2016, 17, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Splieth, C.; Breschi, L.; Banerjee, A.; Fontana, M.; Paris, S.; Burrow, M.F.; Crombie, F.; Page, L.F.; Gatón-Hernández, P.; et al. When to intervene in the caries process? An expert Delphi consensus statement. Clin. Oral. Investig. 2019, 23, 3691–3703. [Google Scholar] [CrossRef]
- Steffen, R.; Krämer, N.; Bekes, K. The Würzburg MIH concept: The MIH treatment need index (MIH TNI): A new index to assess and plan treatment in patients with molar incisior hypomineralisation (MIH). Eur. Arch. Paediatr. Dent. 2017, 18, 355–361. [Google Scholar] [CrossRef]
- Dulla, J.A.; Meyer-Lueckel, H. Molar-incisor hypomineralisation: Narrative review on etiology, epidemiology, diagnostics and treatment decision. Swiss Dent. J. 2021, 131, 886–895. [Google Scholar]
- Bekes, K.; Steffen, R.; Krämer, N. Update of the molar incisor hypomineralization: Würzburg concept. Eur. Arch. Paediatr. Dent. 2023, 24, 807–813. [Google Scholar] [CrossRef]
- Wang, S.J.; Briskie, D.; Hu, J.C.; Majewski, R.; Inglehart, M.R. Illustrated information for parent education: Parent and patient responses. Pediatr. Dent. 2010, 32, 295–303. [Google Scholar] [PubMed]
- WHO. Oral Health Surveys: Basic Methods. Available online: https://www.who.int/publication/i/item/9789241548649 (accessed on 12 December 2023).
- Lygidakis, N.A.; Wong, F.; Jälevik, B.; Vierrou, A.M.; Alaluusua, S.; Espelid, I. Best Clinical Practice Guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH): An EAPD Policy Document. Eur. Arch. Paediatr. Dent. 2010, 11, 75–81. [Google Scholar] [CrossRef]
- Schaefer, G.; Pitchika, V.; Litzenburger, F.; Hickel, R.; Kühnisch, J. Evaluation of occlusal caries detection and assessment by visual inspection, digital bitewing radiography and near-infrared light transillumination. Clin. Oral. Investig. 2018, 22, 2431–2438. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [PubMed]
- James, X.; Hawkins, A.; Rowel, R. An Assessment of the Cultural Appropriateness of Emergency Preparedness Communication for Low Income Minorities. J. Homel. Secur. Emerg. Manag. 2007, 4, 3. [Google Scholar] [CrossRef]
- Montoya, M.F. Diagnostic Outcomes of Digital Images for Comprehensive Examination in Pediatric Dentistry: An Intraexaminer Agreement Assessment. Available online: https://digitalcommons.library.uab.edu/cgi/viewcontent.cgi?article=1066&context=etd-collection (accessed on 12 December 2023).
- Groman, R.; Ginsburg, J. Racial and ethnic disparities in health care: A position paper of the American College of Physicians. Ann. Intern. Med. 2004, 141, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Freire-Maia, J.; Clementino, L.C.; Martins-Júnior, P.A.; Freire-Maia, F.B. Interest in oral health education through digital technologies: A cross-sectional study. Gen. Dent. 2021, 69, 13–17. [Google Scholar]
- Edwards, J.; Waite-Jones, J.; Schwarz, T.; Swallow, V. Digital Technologies for Children and Parents Sharing Self-Management in Childhood Chronic or Long-Term Conditions: A Scoping Review. Children 2021, 8, 1203. [Google Scholar] [CrossRef]
- Yuzbasioglu, E.; Kurt, H.; Turunc, R.; Bilir, H. Comparison of digital and conventional impression techniques: Evaluation of patients’ perception, treatment comfort, effectiveness and clinical outcomes. BMC Oral Health 2014, 14, 10. [Google Scholar] [CrossRef]
- Pisano, M.; Bramanti, A.; Menditti, D.; Sangiovanni, G.; Santoro, R.; Amato, A. Modern Approaches to Providing Telematics Oral Health Services in Pediatric Dentistry: A Narrative Review. Appl. Sci. 2023, 13, 8331. [Google Scholar] [CrossRef]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schulz-Weidner, N.; Gruber, M.; Schraml, E.M.; Wöstmann, B.; Krämer, N.; Schlenz, M.A. Improving the Communication of Dental Findings in Pediatric Dentistry by Using Intraoral Scans as a Visual Aid: A Randomized Clinical Trial. Dent. J. 2024, 12, 15. https://doi.org/10.3390/dj12010015
Schulz-Weidner N, Gruber M, Schraml EM, Wöstmann B, Krämer N, Schlenz MA. Improving the Communication of Dental Findings in Pediatric Dentistry by Using Intraoral Scans as a Visual Aid: A Randomized Clinical Trial. Dentistry Journal. 2024; 12(1):15. https://doi.org/10.3390/dj12010015
Chicago/Turabian StyleSchulz-Weidner, Nelly, Marina Gruber, Eva May Schraml, Bernd Wöstmann, Norbert Krämer, and Maximiliane Amelie Schlenz. 2024. "Improving the Communication of Dental Findings in Pediatric Dentistry by Using Intraoral Scans as a Visual Aid: A Randomized Clinical Trial" Dentistry Journal 12, no. 1: 15. https://doi.org/10.3390/dj12010015
APA StyleSchulz-Weidner, N., Gruber, M., Schraml, E. M., Wöstmann, B., Krämer, N., & Schlenz, M. A. (2024). Improving the Communication of Dental Findings in Pediatric Dentistry by Using Intraoral Scans as a Visual Aid: A Randomized Clinical Trial. Dentistry Journal, 12(1), 15. https://doi.org/10.3390/dj12010015