Dose Reduction and Image Quality Optimization of Pediatric Chest Radiography Using a Tungsten Filter
Abstract
:1. Introduction
2. Materials and Methods
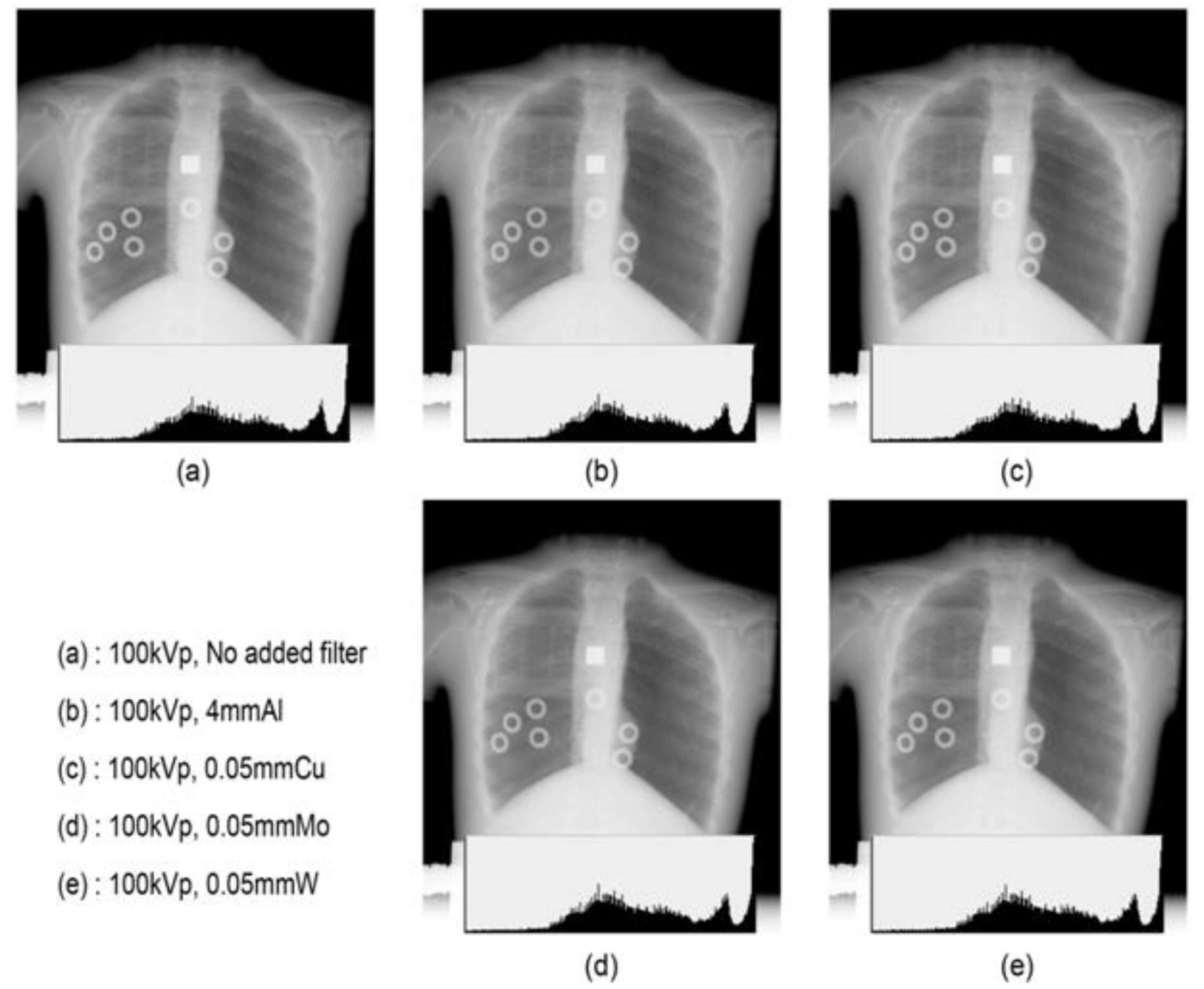
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Communicating Radiation Risks in Paediatric Imaging: Information to Support Healthcare Discussions about Benefit and Risk; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Tapiovaara, M.J.; Sandborg, M.; Dance, D.R. A search for improved technique factors in paediatric fluoroscopy. Phys. Med. Biol. 1999, 44, 537–559. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Boyd, B. Diagnostic Imaging of Pregnant Women and Fetuses: Literature Review. Bioengineering 2022, 9, 236. [Google Scholar] [CrossRef]
- Carlsson, G.A.; Chan, H.P. Commentary: Progress in optimization of patient dose and image quality in X-ray diagnostics. Phys. Med. Biol. 1999, 44, 001. [Google Scholar] [CrossRef]
- Villagran, J.E.; Hobbs, B.B.; Taylor, K.W. Reduction of patient exposure by use of heavy elements as radiation filters in diagnostic radiology. Radiology 1978, 127, 249–254. [Google Scholar] [CrossRef]
- United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). Annex A. Epidemiological Studies of Radiation and Cancer. In 2008a UNSCEAR 2006 Report; UNSCEAR: New York, NY, USA, 2008. [Google Scholar]
- Little, M.P. Cancer and non-cancer effects in Japanese atomic bomb survivors. J. Radiol. Prot. 2009, 29, A43. [Google Scholar] [CrossRef] [PubMed]
- Little, M.P. Comparison of the risks of cancer incidence and mortality following radiation therapy for benign and malignant disease with the cancer risks observed in the Japanese A-bomb survivors. Int. J. Radiat. Biol. 2001, 77, 431–464. [Google Scholar] [CrossRef] [PubMed]
- The National Academics. Health Effects of Exposure to Low Levels of Ionizing Radiation: BEIR V Board on Radiation Effects Research; National Research Council of the National Academies: Washington, DC, USA, 1990. [Google Scholar]
- The National Academics. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. Board on Radiation Effects Research; National Research Council of the National Academies: Washington, DC, USA, 2006. [Google Scholar]
- Hamer, O.W.; Sirlin, C.B.; Strotzer, M.; Borisch, I.; Zorger, N.; Feuerbach, S.; Völk, M. Chest radiography with a flat-panel detector: Image quality with dose reduction after copper filtration. Radiology 2005, 237, 691–700. [Google Scholar] [CrossRef] [PubMed]
- Shrimpton, P.C.; Jones, D.G.; Wall, B.F. The influence of tube filtration and potential on patient dose during X-ray examinations. Phys. Med. Biol. 1988, 33, 1205–1212. [Google Scholar] [CrossRef] [PubMed]
- Hata, A.; Yamada, Y.; Tanaka, R.; Nishino, M.; Hida, K.; Hino, T.; Ueyama, M.; Yanagawa, M.; Kamitani, T.; Kurosaki, A. Dynamic Chest X-ray Using a Flat-Panel Detector System: Technique and Applications. Korean J. Radiol. 2021, 22, 634–651. [Google Scholar] [CrossRef] [PubMed]
- Berfer, M.J.; Motz, J.W. X-rays from thick tungsten targets irradiated by 500–50 keV electrons. Sci. Direct 2004, 226, 324–344. [Google Scholar]
- Yamaguchi, C.; Yamamoto, T.; Terada, H.; Akisada, M. Effect of tungsten absorption edge filter on diagnostic X-ray spectra, image quality and absorbed dose to the patient. Phys. Med. Biol. 1983, 28, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y. A study on the reduction of exposure dose and contrast improvement by use of heavy elements filter. J. Orient. Technol. 2000, 23, 91–96. [Google Scholar]
- Chu, J.C.; Galvin, J.M.; Lockett, P.; Bloch, P. Use of a tungsten filter to improve beam uniformity. Med. Phys. 1981, 8, 520–522. [Google Scholar] [CrossRef]
- Nagel, H.D. Comparison of performance characteristics of conventional and K-edge filters in general diagnostic radiology. Phys. Med. Biol. 1989, 34, 1269–1287. [Google Scholar] [CrossRef] [Green Version]
- Kim, G.S.; Kim, S.C. Comparison of image quality and effective dose by additional filtration on digital chest tomosynthesis. J. Radiol. Sci. Technol. 2015, 38, 347–353. [Google Scholar] [CrossRef]
- Atkins, H.L.; Fairchild, R.G.; Robertson, J.S.; Greenberg, D. Effect of absorption edge filters on diagnostic X-ray spectra. Radiol. 1975, 115, 431–437. [Google Scholar] [CrossRef] [PubMed]
- McParland, B.J.; Boyd, M.M. X-ray image intensifier performance and patient doses for combinations of supplemental beam filters and vascular contrast agents. Phys. Med. Biol. 2001, 46, 227–244. [Google Scholar] [CrossRef] [PubMed]
- Nagel, H.D. Limitation in the determination of total filtration of X-ray tube assemblies. Phys. Med. Biol. 1988, 33, 271–289. [Google Scholar] [CrossRef] [PubMed]
- Toroi, P.; Zanca, F.; Young, K.C.; Ongeval, C.; Marchal, G.; Bosmans, G.H. Experimental investigation on the choice of the tungsten/rhodium anode/filter combination for an amorphous selenium-based digital mammography system. Eur. Radiol. 2007, 17, 2368–2375. [Google Scholar] [CrossRef]
- Onnasch, D.G.W.; Schemm, A.; Kramer, H. Optimization of radiographic parameters for paediatric cardiac angiography. Br. J. Radiol. 2004, 77, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Jennings, R.J. A method for comparing beam-hardening filter materials for diagnostic radiology. Med. Phys. 1988, 15, 588–599. [Google Scholar] [CrossRef] [PubMed]
- Koedooder, K.; Venema, H.W. Filter materials for dose reduction in screen-film radiography. Phys. Med. Biol. 1986, 31, 585–600. [Google Scholar] [CrossRef] [PubMed]
- Yakoumakis, E.; Dimitriadis, A.; Makri, T.; Karlatira, M.; Karavasilis, E.; Gialousis, G. Verification of radiation dose calculations during pediatric cystourethrography examinations using MCNP5 and PCXMC 2.0 Monte Carlo codes. Radiat. Prot. Dosim. 2013, 157, 355–362. [Google Scholar] [CrossRef]
- Brosi, P.; Stuessi, A.; Verdun, F.R.; Vock, P.; Wolf, R. Copper filtration in pediatric digital X-ray imaging: Its impact on image quality and dose. Radiol. Phys. Technol. 2011, 4, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Tapiovaara, M.; Siiskonen, T. PCXMC, a Monte Carlo program for calculating patient doses in medical X-ray examinations. Radiat. Prot. Dosim. 2008, 40, 49. [Google Scholar]
- Smans, K.; Struelens, L.; Smet, M.; Bosmans, H.; Vanhavere, H.F. Cu filtration for dose reduction in neonatal chest imaging. Radiat. Prot. Dosim. 2010, 139, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Iramina, H.; Hamaguchi, T.; Nakamura, M.; Minzowaki, T.; Kanno, I. Metal artifact reduction by filter-based dual-energy cone-beam computed tomography on a bench-top micro-CBCT system: Concept and demonstration. J. Radiat. Res. 2018, 59, 511–520. [Google Scholar] [CrossRef]
- Borrego, D.; Lowe, E.M.; Kitahara, C.M.; Lee, C. Assessment of PCXMC for patients with different body size in chest and abdominal X-ray examinations: A Monte Carlo simulation study. Phys. Med. Biol. 2018, 63, 065015. [Google Scholar] [CrossRef]
- International Commission on Radiological Protection. The 2007 Recommendations of the International Commission on Radiological Protection; ICRP Publication 103: Oxford, UK, 2007. [Google Scholar]
- Aichinger, H.; Dierker, J.; Joite-Barfuß, S.; Säbel, M. Radiation Exposure and Image Quality in X-ray Diagnostic Radiology; Springer: Berlin/Heidelberg, Germany, 2004. [Google Scholar]
- Dobbins, J.T.; Samei, E.; Chotas, H.J.; Warp, R.J.; Baydush, A.H.; Floyd, C.E., Jr.; Ravin, C.E. Chest radiography: Optimization of X-ray spectrum for cesium iodide-amorphous silicon flat-panel detector. Radiology 2003, 226, 221–230. [Google Scholar] [CrossRef]
- Kim, S.H.; Choi, J.H. Analysis of effectiveness of spectrum of energy and image quality evaluation by aluminium filter in the added compound filtration. J. Radiol. Sci. Technol. 2015, 38, 187–197. [Google Scholar] [CrossRef]
- Doyle, P.; Martin, C.J.; Gentle, D. Application of contrast-to-noise ratio in optimizing beam quality for digital chest radiography: Comparison of experimental measurements and theoretical simulations. Phys. Med. Biol. 2006, 51, 2953–2970. [Google Scholar] [CrossRef] [PubMed]
- Regano, L.J.; Sutton, R.A. Radiation dose reduction in diagnostic X-ray procedures. Phys. Med. Biol. 1992, 37, 1773–1788. [Google Scholar] [CrossRef] [PubMed]
- Park, H.S.; Kim, Y.S.; Kim, S.T.; Park, O.S.; Jeon, C.W.; Kim, H.J. Survey of technical parameters for pediatric chest X-ray imaging by using effective DQE and dose. Korean Soc. Med. Phys. 2011, 22, 163–171. [Google Scholar]




| Filter Material | K-Edge (keV) | Equivalent Thickness (mm) (Effective Energy (keV)) | |||
|---|---|---|---|---|---|
| This Work (70 keV) | Nagel, H (30 keV) | Jennings (65 keV) | Koedooder/Venema (70 keV) | ||
| Aluminium (Al) | 0.56 | 6.1 | 7.1 | 7.2 | 5.77 |
| Coppper (Cu) | 8.98 | 0.2 | 0.2 | 0.2 | 0.2 |
| Molybdenum (Mo) | 20 | 0.076 | 0.076 | ||
| Tungsten (W) | 69.5 | 0.045 | 0.046 | 0.046 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, E.; Muroi, K.; Koike, T.; Kim, J. Dose Reduction and Image Quality Optimization of Pediatric Chest Radiography Using a Tungsten Filter. Bioengineering 2022, 9, 583. https://doi.org/10.3390/bioengineering9100583
Kim E, Muroi K, Koike T, Kim J. Dose Reduction and Image Quality Optimization of Pediatric Chest Radiography Using a Tungsten Filter. Bioengineering. 2022; 9(10):583. https://doi.org/10.3390/bioengineering9100583
Chicago/Turabian StyleKim, Eunhye, Kenzo Muroi, Takahisa Koike, and Jungmin Kim. 2022. "Dose Reduction and Image Quality Optimization of Pediatric Chest Radiography Using a Tungsten Filter" Bioengineering 9, no. 10: 583. https://doi.org/10.3390/bioengineering9100583
APA StyleKim, E., Muroi, K., Koike, T., & Kim, J. (2022). Dose Reduction and Image Quality Optimization of Pediatric Chest Radiography Using a Tungsten Filter. Bioengineering, 9(10), 583. https://doi.org/10.3390/bioengineering9100583






