Influence of the Amount of Change in Quadriceps Tendon Young’s Modulus on Amount of Change in Walking Speed before and after Total Knee Arthroplasty
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Young’s Modulus of Quadriceps Tendon
2.3. Knee Circumference
2.4. Knee Joint ROM
2.5. Knee Joint Extension Strength
2.6. One-Leg Standing Time
2.7. Walking Parameters
2.8. Walking Pain
2.9. Activity Level
2.10. Statistical Analysis
3. Results
3.1. Physical Characteristics
3.2. Comparisons before and after TKA
3.3. The Amount of Change before and after TKA
3.4. Correlation Coefficient for Amounts of Change
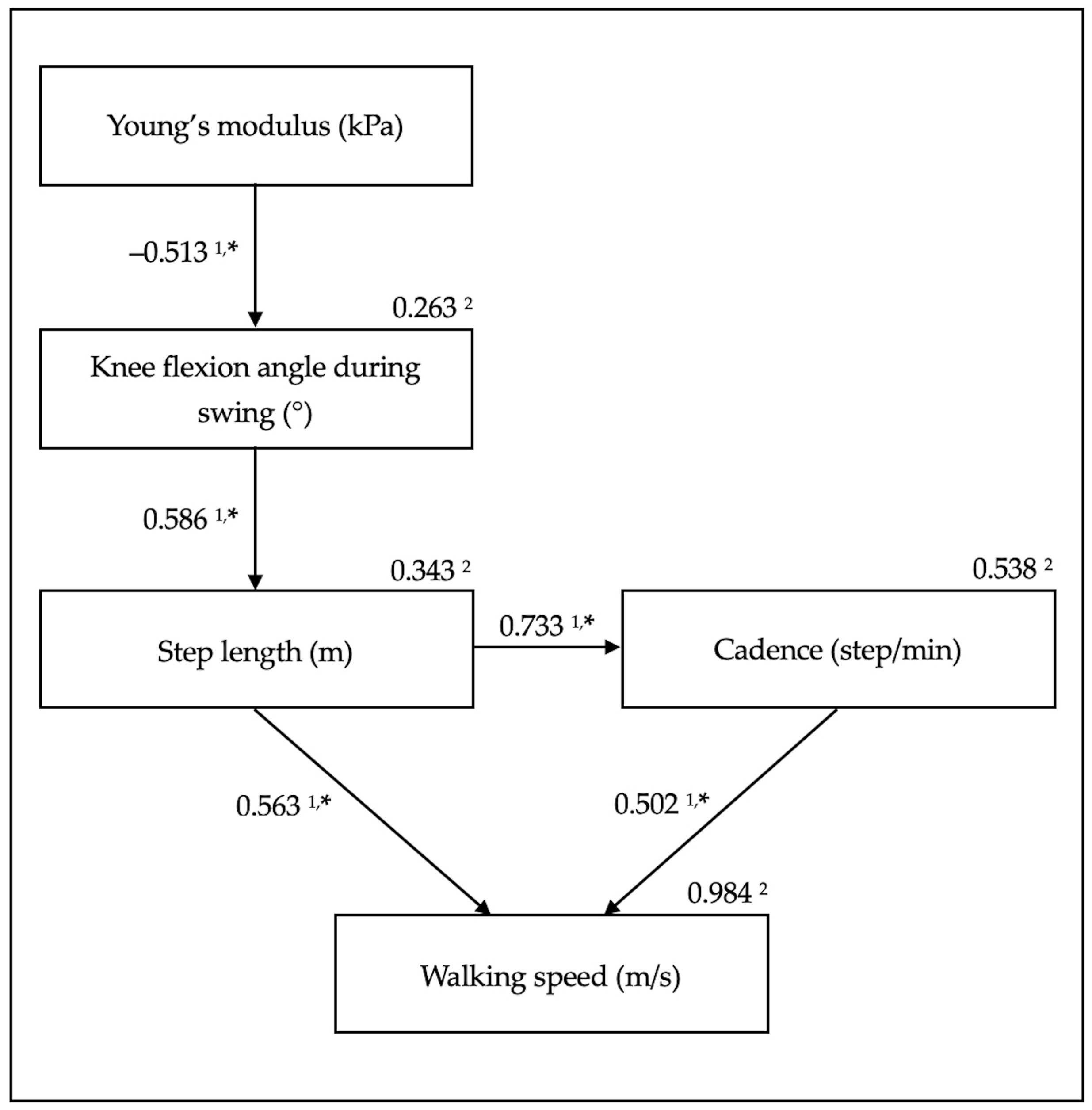
3.5. Path Analysis of the Amounts of Change
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Primorac, D.; Molnar, V.; Rod, E.; Jeleč, Ž.; Čukelj, F.; Matišić, V.; Vrdoljak, T.; Hudetz, D.; Hajsok, H.; Borić, I. Knee osteoarthritis: A review of pathogenesis and state-of-the-art non-operative therapeutic considerations. Genes 2020, 11, 854. [Google Scholar] [CrossRef] [PubMed]
- McAlindon, T.E.; Bannuru, R.R.; Sullivan, M.C.; Arden, N.K.; Berenbaum, F.; Bierma-Zeinstra, S.M.; Hawker, G.A.; Henrotin, Y.; Hunter, D.J.; Kawaguchi, H.; et al. OARSI for the non-surgical management of knee osteoarthritis. Osteoarthr. Cartil. 2014, 22, 363–388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Notarnicola, A.; Maccagnano, G.; Moretti, L.; Pesce, V.; Tafuri, S.; Fiore, A.; Moretti, B. Methylsulfonylmethane and bosewellic acids versus glucosamine sulfate in the treatment of knee arthritis: Randomized trial. Int. J. Immunopathol. Pharmacol. 2016, 29, 140–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Kan, G.A.; Rolland, Y.; Andrieu, S.; Bauer, J.; Beauchet, O.; Bonnefoy, M.; Cesari, M.; Donini, L.; Gillette-Guyonnet, S.; Inzitari, M.; et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J. Nutr. Health Aging 2009, 13, 881–889. [Google Scholar] [CrossRef]
- Hubley-Kozey, C.L.; Hill, N.A.; Rutherford, D.J.; Dunbar, M.J.; Stanish, W.D. Co-activation differences in lower limb muscles between asymptomatic controls and those with varying degrees of knee osteoarthritis during walking. Clin. Biomech. 2009, 24, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Abramoff, B.; Caldera, F.E. Osteoarthritis: Pathology, diagnosis, and treatment options. Med. Clin. N. Am. 2020, 104, 293–311. [Google Scholar] [CrossRef]
- Notarnicola, A.; Maccagnano, G.; Fiore, A.; Spinarelli, A.; Montenegro, L.; Paoloni, M.; Pastore, F.; Tafuri, S.; Moretti, B. Baropodometry on patients after total knee arthroplasty. Musculoskelet. Surg. 2018, 102, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, Y.; Mizner, R.L.; Ramsey, D.K.; Snyder-Mackler, L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin. Biomech. 2008, 23, 320–328. [Google Scholar] [CrossRef] [Green Version]
- Casartelli, N.C.; Item-Glatthorn, J.F.; Bizzini, M.; Leunig, M.; Maffiuletti, N.A. Differences in gait characteristics between total hip, knee, and ankle arthroplasty: A six-month postoperative comparison. BMC Musculoskelet. Disord. 2013, 14, 176. [Google Scholar] [CrossRef] [Green Version]
- Pua, Y.H.; Seah, F.J.; Clark, R.A.; Lian-Li Poon, C.; Tan, J.W.; Chong, H.C. Factors associated with gait speed recovery after total knee arthroplasty: A longitudinal study. Semin. Arthritis Rheum. 2017, 46, 544–551. [Google Scholar] [CrossRef]
- Do, K.; Yim, J. Effects of muscle strengthening around the hip on pain, physical function, and gait in elderly patients with total knee arthroplasty: A randomized controlled trial. Healthcare 2020, 8, 489. [Google Scholar] [CrossRef]
- Ro, D.H.; Han, H.S.; Lee, D.Y.; Kim, S.H.; Kwak, Y.H.; Lee, M.C. Slow gait speed after bilateral total knee arthroplasty is associated with suboptimal improvement of knee biomechanics. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1671–1680. [Google Scholar] [CrossRef]
- Suh, M.J.; Kim, B.R.; Kim, S.R.; Han, E.Y.; Nam, K.W.; Lee, S.Y.; Park, Y.G.; Kim, W.B. Bilateral quadriceps muscle strength and pain correlate with gait speed and gait endurance early after unilateral total knee arthroplasty: A cross-sectional study. Am. J. Phys. Med. Rehabil. 2019, 98, 897–905. [Google Scholar] [CrossRef] [PubMed]
- Pua, Y.H.; Seah, F.J.; Seet, F.J.; Tan, J.W.; Liaw, J.S.; Chong, H.C. Sex differences and impact of body mass index on the time course of knee range of motion, knee strength, and gait speed after total knee arthroplasty. Arthritis Care Res. 2015, 67, 1397–1405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebihara, B.; Mutsuzaki, H.; Fukaya, T.; Iwai, K. Interpretation of causal relationship between quadriceps tendon Young’s modulus and gait speed by structural equation modeling in patients with severe knee osteoarthritis. J. Orthop. Surg. 2021, 29, 23094990211034003. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [Green Version]
- Bercoff, J. ShearWave Elastography. Available online: https://www.konicaminolta.jp/healthcare/products/us/aixplorer/pdf/whitepaper_swe_eng.pdf (accessed on 29 June 2021).
- Ebihara, B.; Mutsuzaki, H.; Fukaya, T. Relationships between quadriceps tendon elasticity and knee flexion angle in young healthy adults. Medicina 2019, 55, 53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peltz, C.D.; Haladik, J.A.; Divine, G.; Siegal, D.; van Holsbeeck, M.; Bey, M.J. ShearWave elastography: Repeatability for measurement of tendon stiffness. Skeletal. Radiol. 2013, 42, 1151–1156. [Google Scholar] [CrossRef] [PubMed]
- Kot, B.C.; Zhang, Z.J.; Lee, A.W.; Leung, V.Y.; Fu, S.N. Elastic modulus of muscle and tendon with shear wave ultrasound elastography: Variations with different technical settings. PLoS ONE 2012, 7, e44348. [Google Scholar] [CrossRef] [Green Version]
- Belkhiria, C.; De Marco, G.; Driss, T. Effects of verbal encouragement on force and electromyographic activations during exercise. J. Sports Med. Phys. Fit. 2018, 58, 750–757. [Google Scholar] [CrossRef]
- Spinoso, D.H.; Bellei, N.C.; Marques, N.R.; Navega, M.T. Quadriceps muscle weakness influences the gait pattern in women with knee osteoarthritis. Adv. Rheumatol. 2018, 58, 26. [Google Scholar] [CrossRef]
- Katoh, M.; Yamasaki, H. Test-retest reliability of isometric leg muscle strength measurements made using a hand-held dynamometer restrained by a belt: Comparisons during between sessions. J. Phys. Ther. Sci. 2009, 21, 239–243. [Google Scholar] [CrossRef] [Green Version]
- Harato, K.; Kobayashi, S.; Kojima, I.; Sakurai, A.; Tanikawa, H.; Niki, Y. Factors affecting one-leg standing time in patients with end-stage knee osteoarthritis and the age-related recovery process following total knee arthroplasty. J. Orthop. Surg. Res. 2017, 12, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joyce, C.R.; Zutshi, D.W.; Hrubes, V.; Mason, R.M. Comparison of fixed interval and visual analogue scales for rating chronic pain. Eur. J. Clin. Pharmacol. 1975, 8, 415–420. [Google Scholar] [CrossRef]
- Okuda, M.; Omokawa, S.; Okahashi, K.; Akahane, M.; Tanaka, Y. Validity and reliability of the Japanese Orthopaedic Association score for osteoarthritic knees. J. Orthop. Sci. 2012, 17, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, E.; Tsuda, E.; Yamamoto, Y.; Meada, S.; Otsuka, H.; Ishibashi, Y. Relationship between patient-based outcome score and conventional objective outcome scales in post-operative total knee arthroplasty patients. Int. Orthop. 2014, 38, 373–378. [Google Scholar] [CrossRef] [Green Version]
- Wright, S. Path coefficients and path regressions: Alternative or complementary concepts? Biometrics 1960, 16, 189–202. [Google Scholar] [CrossRef]
- Wright, S. The treatment of reciprocal interaction, with or without lag, in path analysis. Biometrics 1960, 16, 423–445. [Google Scholar] [CrossRef]
- Zhang, Y.; Ye, L.Y.; Liu, H.X.; Wen, H. Quadriceps tendon pie-crusting release of stiff knees in total knee arthroplasty. J. Orthop. Sci. 2015, 20, 669–674. [Google Scholar] [CrossRef]
- Liu, H.X.; Wen, H.; Hu, Y.Z.; Yu, H.C.; Pan, X.Y. Percutaneous quadriceps tendon pie-crusting release of extension contracture of the knee. Orthop. Traumatol. Surg. Res. 2014, 100, 333–335. [Google Scholar] [CrossRef] [Green Version]
- Ebihara, B.; Fukaya, T.; Mutsuzaki, H. Relationship between Quadriceps Tendon Young’s Modulus and Maximum Knee Flexion Angle in the Swing Phase of Gait in Patients with Severe Knee Osteoarthritis. Medicina 2020, 56, 437. [Google Scholar] [CrossRef] [PubMed]
- Sekiya, N.; Nagasaki, H.; Ito, H.; Furuna, T. The invariant relationship between step length and step rate during free walking. J. Hum. Mov. Stud. 1996, 30, 241–257. [Google Scholar]
- Wadugodapitiya, S.; Sakamoto, M.; Suzuki, S.; Morise, Y.; Kobayashi, K. In vivo stiffness assessment of patellar and quadriceps tendons by strain ultrasound elastography. Biomed. Mater. Eng. 2021, 32, 257–266. [Google Scholar] [CrossRef]
- Xu, J.; Hug, F.; Fu, S.N. Stiffness of individual quadriceps muscle assessed using ultrasound shear wave elastography during passive stretching. J. Sport Health Sci. 2018, 7, 245–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lima, K.M.M.E.; Costa Júnior, J.F.S.; Pereira, W.C.A.; Oliveira, L.F. Assessment of the mechanical properties of the muscle-tendon unit by supersonic shear wave imaging elastography: A review. Ultrasonography 2018, 37, 3–15. [Google Scholar] [CrossRef]
| Characteristics | Pre-TKA (n = 16) |
|---|---|
| Age (years) | 74.0 (64.5–75.8) 2 |
| Sex (men/women) | 3/13 |
| Height (m) | 1.52 ± 0.07 1 |
| Body weight (kg) | 60.8 ± 11.4 1 |
| FTA (°) | 180.0 (177.3–182.8) 2 |
| KL grade (3/4) | 4/12 |
| Measurement Item | Pre-TKA (n = 16) | Post-TKA (n = 16) | p-Value | Effect Size |
|---|---|---|---|---|
| Body weight (kg) | 60.8 ± 11.4 1 | 61.4 ± 12.1 1 | 0.320 3 | 0.05 5 |
| BMI (kg/m2) | 26.2 ± 4.3 1 | 26.5 ± 4.3 1 | 0.368 3 | 0.07 5 |
| FTA (°) | 180.0 (177.3–182.8) 2 | 173.9 ± 3.7 1 | 0.007 4,* | 0.68 6 |
| Young’s modulus (kPa) | 306.0 ± 121.5 1 | 250.1 ± 106.9 1 | 0.125 3 | 0.49 5 |
| Knee circumference (cm) | 39.1 ± 3.3 1 | 38.7 ± 3.5 1 | 0.281 3 | 0.12 5 |
| Passive knee flexion angle (°) | 129.1 ± 12.6 1 | 131.2 ± 11.7 1 | 0.409 3 | 0.17 5 |
| Active knee flexion angle (°) | 121.8 ± 12.7 1 | 120.9 ± 8.1 1 | 0.761 3 | 0.09 5 |
| Knee extension torque (Nm) | 66.9 ± 20.0 1 | 81.0 ± 18.6 1 | 0.003 3,* | 0.73 5 |
| Knee extension torque/weight ratio (Nm/kg) | 1.12 ± 0.34 1 | 1.35 ± 0.34 1 | 0.007 3,* | 0.68 5 |
| One-leg standing time (s) | 9.1 (2.9–28.1) 2 | 8.0 (3.9–36.1) 2 | 0.301 4 | 0.26 6 |
| Knee flexion angle during swing (°) | 58.7 (51.9–64.3) 2 | 60.5 ± 5.0 1 | 0.187 4 | 0.33 6 |
| Step length (m) | 0.49 ± 0.10 1 | 0.53 ± 0.07 1 | 0.016 3,* | 0.46 5 |
| Cadence (step/min) | 110.3 ± 16.0 1 | 121.5 ± 10.7 1 | 0.007 3,* | 0.82 5 |
| Walking speed (m/s) | 0.91 ± 0.26 1 | 1.07 ± 0.17 1 | 0.006 3,* | 0.73 5 |
| Walking pain (points) | 29.9 ± 24.6 1 | 0.0 (0.0–0.0) 2 | 0.002 4,* | 0.77 6 |
| JOA score (points) | 64.1 ± 10.5 1 | 85.0 ± 7.7 1 | <0.001 3,* | 2.27 5 |
| Measurement Item | Amount of Change (n = 16) |
|---|---|
| Body weight (kg) | 0.6 ± 2.5 1 |
| BMI (kg/m2) | 0.2 ± 1.0 1 |
| FTA (°) | −5.1 ± 5.9 1 |
| Young’s modulus (kPa) | −55.9 ± 137.4 1 |
| Knee circumference (cm) | −0.4 ± 1.5 1 |
| Passive knee flexion angle (°) | 5.5 (−8.5–10.8) 2 |
| Active knee flexion angle (°) | −0.8 ± 10.5 1 |
| Knee extension torque (Nm) | 14.1 ± 16.3 1 |
| Knee extension torque/weight ratio (Nm/kg) | 0.16 (−0.03–0.36) 2 |
| One-leg standing time (s) | 0.4 (−2.7–12.2) 2 |
| Knee flexion angle during swing (°) | 0.9 (−0.8–7.1) 2 |
| Step length (m) | 0.04 ± 0.06 1 |
| Cadence (step/min) | 6.0 (0.9–18.8) 2 |
| Walking speed (m/s) | 0.16 ± 0.20 1 |
| Walking pain (points) | −28.6 ± 25.2 1 |
| JOA score (points) | 20 (11.25–28.75) 2 |
| Young’s Modulus | Knee Flexion Angle during Swing | Step Length | Cadence | Walking Speed | |
|---|---|---|---|---|---|
| Correlation coefficient | |||||
| Body weight (kg) | 0.408 1 | −0.568 2,* | −0.203 1 | −0.339 2 | −0.071 1 |
| BMI (kg/m2) | 0.433 1 | −0.594 2,* | −0.186 1 | −0.353 2 | −0.073 1 |
| FTA (°) | 0.497 1 | −0.195 2 | −0.144 1 | −0.437 2 | −0.357 1 |
| Young’s modulus (kPa) | - | −0.594 2,* | −0.196 1 | −0.465 2 | −0.285 1 |
| Knee circumference (cm) | 0.230 1 | −0.439 2 | −0.425 1 | −0.222 2 | −0.210 1 |
| Passive knee flexion angle (°) | −0.124 2 | −0.103 2 | 0.121 2 | 0.310 2 | 0.296 2 |
| Active knee flexion angle (°) | −0.085 1 | 0.028 2 | 0.161 1 | 0.249 2 | 0.211 1 |
| Knee extension torque (Nm) | 0.263 1 | −0.085 2 | 0.423 1 | 0.344 2 | 0.433 1 |
| Knee extension torque/weight ratio (Nm/kg) | 0.091 2 | 0.047 2 | 0.504 2,* | 0.374 2 | 0.557 2,* |
| One-leg standing time (s) | 0.368 2 | −0.274 2 | 0.062 2 | −0.053 2 | 0.071 2 |
| Knee flexion angle during swing (°) | −0.594 2,* | - | 0.499 2,* | 0.553 2,* | 0.457 2 |
| Step length (m) | −0.196 1 | 0.499 2,* | - | 0.711 2,* | 0.931 1,* |
| Cadence (step/min) | −0.465 2 | 0.553 2,* | 0.711 2,* | - | 0.878 2,* |
| Walking speed (m/s) | −0.285 1 | 0.457 2 | 0.931 1,* | 0.878 2,* | - |
| Walking pain (points) | 0.329 1 | −0.188 2 | −0.100 1 | −0.218 2 | −0.096 1 |
| JOA score (points) | −0.443 2 | 0.659 2,* | 0.279 2 | 0.327 2 | 0.283 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ebihara, B.; Mutsuzaki, H.; Fukaya, T.; Iwai, K. Influence of the Amount of Change in Quadriceps Tendon Young’s Modulus on Amount of Change in Walking Speed before and after Total Knee Arthroplasty. Medicina 2021, 57, 1329. https://doi.org/10.3390/medicina57121329
Ebihara B, Mutsuzaki H, Fukaya T, Iwai K. Influence of the Amount of Change in Quadriceps Tendon Young’s Modulus on Amount of Change in Walking Speed before and after Total Knee Arthroplasty. Medicina. 2021; 57(12):1329. https://doi.org/10.3390/medicina57121329
Chicago/Turabian StyleEbihara, Bungo, Hirotaka Mutsuzaki, Takashi Fukaya, and Koichi Iwai. 2021. "Influence of the Amount of Change in Quadriceps Tendon Young’s Modulus on Amount of Change in Walking Speed before and after Total Knee Arthroplasty" Medicina 57, no. 12: 1329. https://doi.org/10.3390/medicina57121329






