Current Updates on Involvement of Artificial Intelligence and Machine Learning in Semen Analysis
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
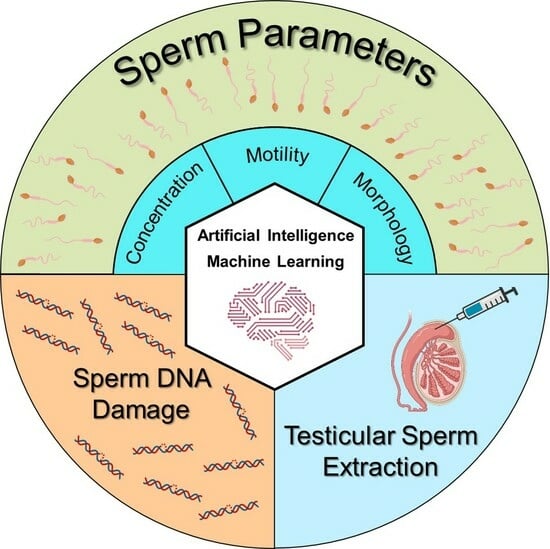
4.1. AI in Evaluation of Sperm Concentration or Total Count
4.2. AI in Evaluation of Sperm Motility
4.3. AI in Evaluation of Sperm Morphology
4.4. AI in Evaluation of Sperm DNA Integrity or Damage
4.5. AI in Predicting Outcome of TESE
| Studies | Dataset/Sample | Algorithm or Model | Performance or Outcomes |
|---|---|---|---|
| Bachelot et al., 2023 [53] | Semen | DNN | RF model: detected AUC = 0.90, sensitivity = 100%, specificity = 69.2% |
| Lee et al., 2022 [58] | Semen | CNN | For dissociated micro-TESE samples doped with an abundant quantity of sperm obtained: PPV = 84.0%, sensitivity = 72.7%, F1-score = 77.9% For dissociated micro-TESE samples doped with rare sperm obtained: PPV = 84.4%, sensitivity = 86.1%, F1-score = 85.2% |
| Wu et al., 2021 [57] | Semen | DNN | Obtained mean average precision (mAP) = 0.741, average recall (AR) = 0.376 |
| Zeadna et al., 2020 [54] | Semen | GBTs | Detected AUC = 0.8, sensitivity = 91%, specificity = 25% |
| Ramasamy et al., 2013 [56] | Semen | ANN | Achieved ROC = 0.641, accuracy = 59.4% |
| Samli and Dogan 2004 [55] | Semen | ANN | Prediction accuracy = 80.80% |
4.6. Strengths, Weaknesses, Opportunities, Threats (SWOT) Analysis of AI in Semen Analysis and Andrology Procedures
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zegers-Hochschild, F.; Adamson, G.D.; Dyer, S.; Racowsky, C.; de Mouzon, J.; Sokol, R.; Rienzi, L.; Sunde, A.; Schmidt, L.; Cooke, I.D.; et al. The International Glossary on Infertility and Fertility Care, 2017. Fertil. Steril. 2017, 108, 393–406. [Google Scholar] [CrossRef]
- World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Agarwal, A.; Baskaran, S.; Parekh, N.; Cho, C.L.; Henkel, R.; Vij, S.; Arafa, M.; Panner Selvam, M.K.; Shah, R. Male infertility. Lancet 2021, 397, 319–333. [Google Scholar] [CrossRef]
- Sikka, S.C.; Hellstrom, W.J. Current updates on laboratory techniques for the diagnosis of male reproductive failure. Asian J. Androl. 2016, 18, 392–401. [Google Scholar] [CrossRef]
- Niederberger, C.; Pellicer, A.; Cohen, J.; Gardner, D.K.; Palermo, G.D.; O’Neill, C.L.; Chow, S.; Rosenwaks, Z.; Cobo, A.; Swain, J.E.; et al. Forty years of IVF. Fertil. Steril. 2018, 110, 185–324.e185. [Google Scholar] [CrossRef]
- Keel, B.A. How reliable are results from the semen analysis? Fertil. Steril. 2004, 82, 41–44. [Google Scholar] [CrossRef]
- Finelli, R.; Leisegang, K.; Tumallapalli, S.; Henkel, R.; Agarwal, A. The validity and reliability of computer-aided semen analyzers in performing semen analysis: A systematic review. Transl. Androl. Urol. 2021, 10, 3069–3079. [Google Scholar] [CrossRef]
- Busnatu, Ș.; Niculescu, A.G.; Bolocan, A.; Petrescu, G.E.D.; Păduraru, D.N.; Năstasă, I.; Lupușoru, M.; Geantă, M.; Andronic, O.; Grumezescu, A.M.; et al. Clinical Applications of Artificial Intelligence-An Updated Overview. J. Clin. Med. 2022, 11, 2265. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, M.J.; Javed, Z.; Sadia, H.; Qureshi, I.A.; Irshad, A.; Ahmed, R.; Malik, K.; Raza, S.; Abbas, A.; Pezzani, R.; et al. Clinical applications of artificial intelligence and machine learning in cancer diagnosis: Looking into the future. Cancer Cell Int. 2021, 21, 270. [Google Scholar] [CrossRef] [PubMed]
- Kumar, Y.; Koul, A.; Singla, R.; Ijaz, M.F. Artificial intelligence in disease diagnosis: A systematic literature review, synthesizing framework and future research agenda. J. Ambient. Intell. Humaniz. Comput. 2023, 14, 8459–8486. [Google Scholar] [CrossRef] [PubMed]
- Keenan, T.D.L.; Clemons, T.E.; Domalpally, A.; Elman, M.J.; Havilio, M.; Agrón, E.; Benyamini, G.; Chew, E.Y. Retinal Specialist versus Artificial Intelligence Detection of Retinal Fluid from OCT: Age-Related Eye Disease Study 2: 10-Year Follow-On Study. Ophthalmology 2021, 128, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Pan, W.; Jin, L.; Li, Y.; Geng, Y.; Gao, C.; Chen, G.; Wang, H.; Ma, D.; Liao, S. Artificial intelligence in reproductive medicine. Reproduction 2019, 158, R139–R154. [Google Scholar] [CrossRef]
- Smith, K.P.; Wang, H.; Durant, T.J.; Mathison, B.A.; Sharp, S.E.; Kirby, J.E.; Long, S.W.; Rhoads, D.D. Applications of artificial intelligence in clinical microbiology diagnostic testing. Clin. Microbiol. Newsl. 2020, 42, 61–70. [Google Scholar] [CrossRef]
- Rabbani, N.; Kim, G.Y.E.; Suarez, C.J.; Chen, J.H. Applications of machine learning in routine laboratory medicine: Current state and future directions. Clin. Biochem. 2022, 103, 1–7. [Google Scholar] [CrossRef]
- Delipetrev, B.; Tsinaraki, C.; Kostić, U. AI Watch Historical Evolution of Artificial Intelligence; Joint Research: Ispra, Italy, 2018. [Google Scholar]
- Punjani, N.; Kang, C.; Lee, R.K.; Goldstein, M.; Li, P.S. Technological Advancements in Male Infertility Microsurgery. J. Clin. Med. 2021, 10, 4259. [Google Scholar] [CrossRef] [PubMed]
- Santi, D.; Spaggiari, G.; Casonati, A.; Casarini, L.; Grassi, R.; Vecchi, B.; Roli, L.; De Santis, M.C.; Orlando, G.; Gravotta, E.; et al. Multilevel approach to male fertility by machine learning highlights a hidden link between haematological and spermatogenetic cells. Andrology 2020, 8, 1021–1029. [Google Scholar] [CrossRef]
- Zhou, M.; Yao, T.; Li, J.; Hui, H.; Fan, W.; Guan, Y.; Zhang, A.; Xu, B. Preliminary prediction of semen quality based on modifiable lifestyle factors by using the XGBoost algorithm. Front. Med. 2022, 9, 811890. [Google Scholar] [CrossRef] [PubMed]
- Ghasemian, F.; Bahadori, M.H.; Hosseini Kolkooh, S.Z.; Esmaeili, M. Using Deep Learning Algorithm: The Study of Sperm Head Vacuoles and Its Correlation with Protamine mRNA Ratio. Cell J. 2022, 24, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Dubey, V.; Popova, D.; Ahmad, A.; Acharya, G.; Basnet, P.; Mehta, D.S.; Ahluwalia, B.S. Partially spatially coherent digital holographic microscopy and machine learning for quantitative analysis of human spermatozoa under oxidative stress condition. Sci. Rep. 2019, 9, 3564. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Kumar, K.V.; Reddy, B.R.; Krishna, K.S. Comparison of different methods for assessing sperm concentration in infertility workup: A review. Int. J. Med. Med. Sci. 2013, 5, 396–400. [Google Scholar]
- Lesani, A.; Kazemnejad, S.; Moghimi Zand, M.; Azadi, M.; Jafari, H.; Mofrad, M.R.K.; Nosrati, R. Quantification of human sperm concentration using machine learning-based spectrophotometry. Comput. Biol. Med. 2020, 127, 104061. [Google Scholar] [CrossRef]
- Amann, R.P.; Katz, D.F. Reflections on CASA after 25 years. J. Androl. 2004, 25, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Girela, J.L.; Gil, D.; Johnsson, M.; Gomez-Torres, M.J.; De Juan, J. Semen parameters can be predicted from environmental factors and lifestyle using artificial intelligence methods. Biol. Reprod. 2013, 88, 99. [Google Scholar] [CrossRef] [PubMed]
- Ory, J.; Tradewell, M.B.; Blankstein, U.; Lima, T.F.; Nackeeran, S.; Gonzalez, D.C.; Nwefo, E.; Moryousef, J.; Madhusoodanan, V.; Lau, S.; et al. Artificial Intelligence Based Machine Learning Models Predict Sperm Parameter Upgrading after Varicocele Repair: A Multi-Institutional Analysis. World J. Mens. Health 2022, 40, 618–626. [Google Scholar] [CrossRef] [PubMed]
- Tsai, V.F.; Zhuang, B.; Pong, Y.H.; Hsieh, J.T.; Chang, H.C. Web- and Artificial Intelligence-Based Image Recognition For Sperm Motility Analysis: Verification Study. JMIR Med. Inform. 2020, 8, e20031. [Google Scholar] [CrossRef]
- Cherouveim, P.; Velmahos, C.; Bormann, C.L. Artificial Intelligence (AI) for Sperm Selection—A Systematic Review. Fertil. Steril. 2023, 120, 24–31. [Google Scholar] [CrossRef]
- Goodson, S.G.; White, S.; Stevans, A.M.; Bhat, S.; Kao, C.Y.; Jaworski, S.; Marlowe, T.R.; Kohlmeier, M.; McMillan, L.; Zeisel, S.H.; et al. CASAnova: A multiclass support vector machine model for the classification of human sperm motility patterns. Biol. Reprod. 2017, 97, 698–708. [Google Scholar] [CrossRef]
- Agarwal, A.; Henkel, R.; Huang, C.C.; Lee, M.S. Automation of human semen analysis using a novel artificial intelligence optical microscopic technology. Andrologia 2019, 51, e13440. [Google Scholar] [CrossRef]
- Hicks, S.A.; Andersen, J.M.; Witczak, O.; Thambawita, V.; Halvorsen, P.; Hammer, H.L.; Haugen, T.B.; Riegler, M.A. Machine Learning-Based Analysis of Sperm Videos and Participant Data for Male Fertility Prediction. Sci. Rep. 2019, 9, 16770. [Google Scholar] [CrossRef]
- Ottl, S.; Amiriparian, S.; Gerczuk, M.; Schuller, B.W. motilitAI: A machine learning framework for automatic prediction of human sperm motility. iScience 2022, 25, 104644. [Google Scholar] [CrossRef]
- Somasundaram, D.; Nirmala, M. Faster region convolutional neural network and semen tracking algorithm for sperm analysis. Comput. Methods Programs Biomed. 2021, 200, 105918. [Google Scholar] [CrossRef]
- Valiuškaitė, V.; Raudonis, V.; Maskeliūnas, R.; Damaševičius, R.; Krilavičius, T. Deep Learning Based Evaluation of Spermatozoid Motility for Artificial Insemination. Sensors 2020, 21, 72. [Google Scholar] [CrossRef]
- Marín, R.; Chang, V. Impact of transfer learning for human sperm segmentation using deep learning. Comput. Biol. Med. 2021, 136, 104687. [Google Scholar] [CrossRef]
- Yüzkat, M.; Ilhan, H.O.; Aydin, N. Multi-model CNN fusion for sperm morphology analysis. Comput. Biol. Med. 2021, 137, 104790. [Google Scholar] [CrossRef]
- Shaker, F.; Monadjemi, S.A.; Naghsh-Nilchi, A.R. Automatic detection and segmentation of sperm head, acrosome and nucleus in microscopic images of human semen smears. Comput. Methods Programs Biomed. 2016, 132, 11–20. [Google Scholar] [CrossRef]
- Chang, V.; Garcia, A.; Hitschfeld, N.; Härtel, S. Gold-standard for computer-assisted morphological sperm analysis. Comput. Biol. Med. 2017, 83, 143–150. [Google Scholar] [CrossRef]
- Javadi, S.; Mirroshandel, S.A. A novel deep learning method for automatic assessment of human sperm images. Comput. Biol. Med. 2019, 109, 182–194. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Kishi, H.; Murakata, S.; Hayashi, Y.; Hattori, T.; Nakazawa, S.; Mori, Y.; Hidaka, M.; Kasahara, Y.; Kusuhara, A.; et al. A new deep-learning model using YOLOv3 to support sperm selection during intracytoplasmic sperm injection procedure. Reprod. Med. Biol. 2022, 21, e12454. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, A.; Miahi, E.; Mirroshandel, S.A. Effect of deep transfer and multi-task learning on sperm abnormality detection. Comput. Biol. Med. 2021, 128, 104121. [Google Scholar] [CrossRef] [PubMed]
- Nygate, Y.N.; Levi, M.; Mirsky, S.K.; Turko, N.A.; Rubin, M.; Barnea, I.; Dardikman-Yoffe, G.; Haifler, M.; Shalev, A.; Shaked, N.T. Holographic virtual staining of individual biological cells. Proc. Natl. Acad. Sci. USA 2020, 117, 9223–9231. [Google Scholar] [CrossRef] [PubMed]
- Movahed, R.A.; Mohammadi, E.; Orooji, M. Automatic segmentation of Sperm’s parts in microscopic images of human semen smears using concatenated learning approaches. Comput. Biol. Med. 2019, 109, 242–253. [Google Scholar] [CrossRef]
- Riordon, J.; McCallum, C.; Sinton, D. Deep learning for the classification of human sperm. Comput. Biol. Med. 2019, 111, 103342. [Google Scholar] [CrossRef] [PubMed]
- Mirsky, S.K.; Barnea, I.; Levi, M.; Greenspan, H.; Shaked, N.T. Automated analysis of individual sperm cells using stain-free interferometric phase microscopy and machine learning. Cytometry A 2017, 91, 893–900. [Google Scholar] [CrossRef] [PubMed]
- Shaker, F.; Monadjemi, S.A.; Alirezaie, J.; Naghsh-Nilchi, A.R. A dictionary learning approach for human sperm heads classification. Comput. Biol. Med. 2017, 91, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, I.; Mustafa, G.; Ma, J. Deep Learning-Based Morphological Classification of Human Sperm Heads. Diagnostics 2020, 10, 325. [Google Scholar] [CrossRef] [PubMed]
- Evenson, D.P. The Sperm Chromatin Structure Assay (SCSA®) and other sperm DNA fragmentation tests for evaluation of sperm nuclear DNA integrity as related to fertility. Anim. Reprod. Sci. 2016, 169, 56–75. [Google Scholar] [CrossRef] [PubMed]
- McCallum, C.; Riordon, J.; Wang, Y.; Kong, T.; You, J.B.; Sanner, S.; Lagunov, A.; Hannam, T.G.; Jarvi, K.; Sinton, D. Deep learning-based selection of human sperm with high DNA integrity. Commun. Biol. 2019, 2, 250. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Karna, K.K.; Kaiyal, R.S.; Cannarella, R.; Lundy, S.D.; Vij, S.C.; Agarwal, A. Novel sperm chromatin dispersion test with artificial intelligence-aided halo evaluation: A comparison study with existing modalities. Andrology 2023, 11, 1581–1592. [Google Scholar] [CrossRef]
- Noy, L.; Barnea, I.; Mirsky, S.K.; Kamber, D.; Levi, M.; Shaked, N.T. Sperm-cell DNA fragmentation prediction using label-free quantitative phase imaging and deep learning. Cytometry A 2023, 103, 470–478. [Google Scholar] [CrossRef]
- Wang, Y.; Riordon, J.; Kong, T.; Xu, Y.; Nguyen, B.; Zhong, J.; You, J.B.; Lagunov, A.; Hannam, T.G.; Jarvi, K.; et al. Prediction of DNA Integrity from Morphological Parameters Using a Single-Sperm DNA Fragmentation Index Assay. Adv. Sci. 2019, 6, 1900712. [Google Scholar] [CrossRef]
- Bachelot, G.; Dhombres, F.; Sermondade, N.; Haj Hamid, R.; Berthaut, I.; Frydman, V.; Prades, M.; Kolanska, K.; Selleret, L.; Mathieu-D’Argent, E.; et al. A Machine Learning Approach for the Prediction of Testicular Sperm Extraction in Nonobstructive Azoospermia: Algorithm Development and Validation Study. J. Med. Internet Res. 2023, 25, e44047. [Google Scholar] [CrossRef] [PubMed]
- Zeadna, A.; Khateeb, N.; Rokach, L.; Lior, Y.; Har-Vardi, I.; Harlev, A.; Huleihel, M.; Lunenfeld, E.; Levitas, E. Prediction of sperm extraction in non-obstructive azoospermia patients: A machine-learning perspective. Hum. Reprod. 2020, 35, 1505–1514. [Google Scholar] [CrossRef]
- Samli, M.M.; Dogan, I. An artificial neural network for predicting the presence of spermatozoa in the testes of men with nonobstructive azoospermia. J. Urol. 2004, 171, 2354–2357. [Google Scholar] [CrossRef]
- Ramasamy, R.; Padilla, W.O.; Osterberg, E.C.; Srivastava, A.; Reifsnyder, J.E.; Niederberger, C.; Schlegel, P.N. A comparison of models for predicting sperm retrieval before microdissection testicular sperm extraction in men with nonobstructive azoospermia. J. Urol. 2013, 189, 638–642. [Google Scholar] [CrossRef]
- Wu, D.J.; Badamjav, O.; Reddy, V.V.; Eisenberg, M.; Behr, B. A preliminary study of sperm identification in microdissection testicular sperm extraction samples with deep convolutional neural networks. Asian J. Androl. 2021, 23, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Witherspoon, L.; Robinson, M.; Lee, J.H.; Duffy, S.P.; Flannigan, R.; Ma, H. Automated rare sperm identification from low-magnification microscopy images of dissociated microsurgical testicular sperm extraction samples using deep learning. Fertil. Steril. 2022, 118, 90–99. [Google Scholar] [CrossRef] [PubMed]


| Studies | Dataset/Sample | Algorithm or Model | Performance or Outcomes |
|---|---|---|---|
| Ory et al., 2022 [26] | Semen | Logistic regression, SVM and RF | Good predictive accuracy with AUC = 0.72 |
| Lesani et al., 2020 [23] | Semen | FSNN, SPNN | Prediction accuracy: SPNN = 86%, FSNN = 93% |
| Tsai et al., 2020 [27] | Semen | Image recognition algorithm | AI algorithm vs. manual analysis: sperm concentration (r = 0.65, p < 0.001), motile sperm concentration (r = 0.84, p < 0.001) |
| Girela et al., 2013 [25] | Semen | ANN | Accuracy = 90%, sensitivity = 95.45%, specificity = 50%, PPV = 93.33%, NPV= 60% |
| Studies | Dataset/Sample | Algorithm or Model | Performance or Outcomes |
|---|---|---|---|
| Ottl et al., 2022 [32] | VISEM | SVR, MLP, CNN, RNN | Mean absolute error (MAE): SVR = 9.29, MLP = 9.50, CNN = 9.22, RNN = 9.86 |
| Somasundaram and Nirmala 2021 [33] | Semen | THMA | Accuracy = 97.37%, with minimum execution time of 1.12 s. |
| Tsai et al., 2020 [27] | Semen | Bemaner AI algorithm | AI algorithm vs. manual analysis: r = 0.90, p < 0.001 |
| Valiuškaitė et al., 2020 [34] | VISEM | CNN | MAE for predicted sperm motility = 2.92 |
| Goodson et al., 2017 [29] | Semen | SVM | Accuracy = 89.9% |
| Girela et al., 2013 [25] | Semen | ANN | Accuracy = 82%, sensitivity = 89.29%, specificity = 43.75%, PPV = 89.29%, NPV = 43.75% |
| Studies | Dataset/Sample | Algorithm or Model | Performance or Outcomes |
|---|---|---|---|
| Sato et al., 2022 [40] | JSD | DL | Abnormal sperm: sensitivity = 0.881 and PPV = 0.853 Normal sperm: sensitivity = 0.794 and PPV = 0.689 |
| Abbasi et al., 2021 [41] | MHSMA | DTL DMTL | Detection accuracy: head = 84.0%, acrosome = 80.66%, and vacuole = 94.0% |
| Marín and Chang 2021 [35] | SCIAN-SpermSegGS | DL, U-Net, and Mask-RCNN | Dice coefficient using U-net with transfer learning: head = 0.96, acrosome = 0.94, and nucleus = 0.95 |
| Nygate et al., 2020 [42] | Semen | DL, HoloStain | Virtual (holostain) vs. chemical staining: structural similarity (SSIM) = 0.85 ± 0.03 |
| Valiuškaitė et al., 2020 [34] | VISEM | CNN | Accuracy of sperm head detection = 91.77% |
| Dubey et al., 2019 [20] | Semen | SVM | Accuracy = 89.93%, sensitivity = 91.18%, and specificity = 88.61% |
| Javadi and Mirroshandel 2019 [39] | MHSMA | DL | Detection accuracy: acrosome = 76.67%, head = 77.00%, vacuole = 91.33% |
| Movahed et al., 2019 [43] | SCIAN | CNN and SVM | Dice coefficient: head = 0.90, axial filament = 0.77, acrosome = 0.77, nucleus = 0.78, tail = 0.75, and mid-piece = 0.64 |
| Riordon et al., 2019 [44] | HuSHeM and SCIAN | Deep-CNN, VGG16 | Increased true positive rate: HuSHeM dataset = 94.1%, SCIAN dataset = 62% |
| Mirsky et al., 2017 [45] | Semen | SVM | Good accuracy with AUC = 89.59% |
| Shaker et al., 2017 [46] | SCIAN and HuSHeM | Dictionary learning | Detection accuracy: HuSeM dataset = 92%, SCIAN dataset = 62% |
| Shaker et al., 2016 [37] | Semen | Tail point algorithm | Dice coefficient accuracy: heads = 92%, acrosome = 84%, nucleus = 87%, and tail = 96% |
| Studies | Dataset/Sample | Algorithm or Model | Performance or Outcomes |
|---|---|---|---|
| Kuroda et al., 2023 [50] | Semen | CNN | AI algorithm vs. manual scoring (r = 0.97, p < 0.001) |
| Noy et al., 2023 [51] | Semen | MobileNet CNN | Prediction accuracy = 90%, sensitivity = 0.93, specificity = 0.9 |
| McCallum et al., 2019 [49] | Semen | Deep CNN | Sperm cell image vs. DNA quality (bivariate correlation ~0.43) |
| Wang et al., 2019 [52] | Semen | Logistic regression | Test accuracy = 82.7% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panner Selvam, M.K.; Moharana, A.K.; Baskaran, S.; Finelli, R.; Hudnall, M.C.; Sikka, S.C. Current Updates on Involvement of Artificial Intelligence and Machine Learning in Semen Analysis. Medicina 2024, 60, 279. https://doi.org/10.3390/medicina60020279
Panner Selvam MK, Moharana AK, Baskaran S, Finelli R, Hudnall MC, Sikka SC. Current Updates on Involvement of Artificial Intelligence and Machine Learning in Semen Analysis. Medicina. 2024; 60(2):279. https://doi.org/10.3390/medicina60020279
Chicago/Turabian StylePanner Selvam, Manesh Kumar, Ajaya Kumar Moharana, Saradha Baskaran, Renata Finelli, Matthew C. Hudnall, and Suresh C. Sikka. 2024. "Current Updates on Involvement of Artificial Intelligence and Machine Learning in Semen Analysis" Medicina 60, no. 2: 279. https://doi.org/10.3390/medicina60020279