Total Power Radiometer for Medical Sensor Applications Using Matched and Mismatched Noise Sources
Abstract
:1. Introduction
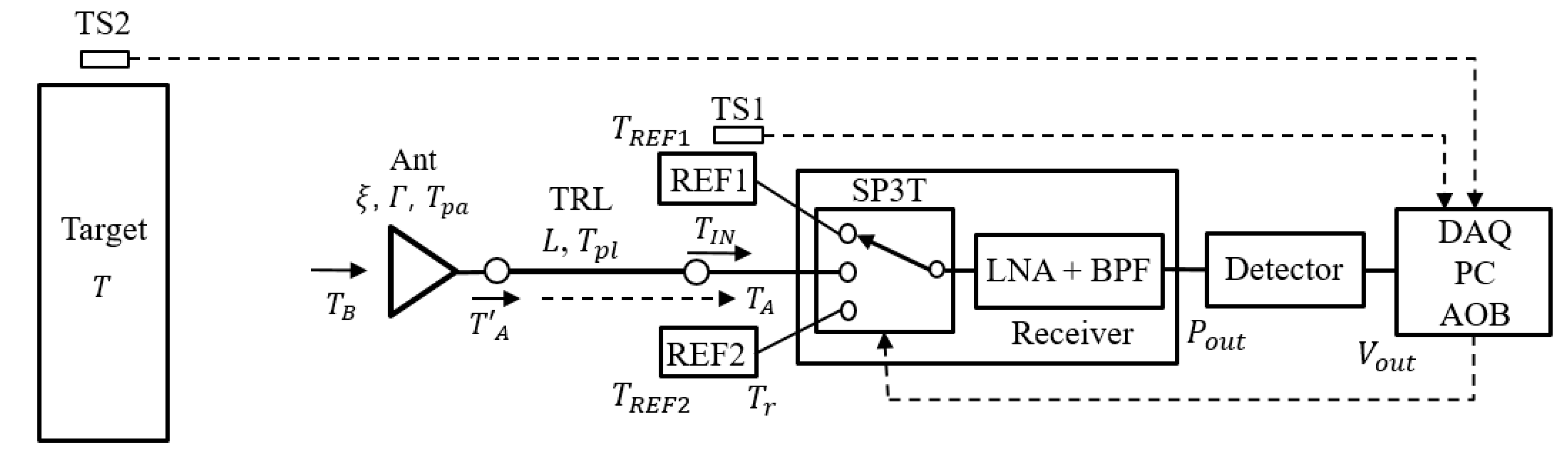
2. Design of Radiometer
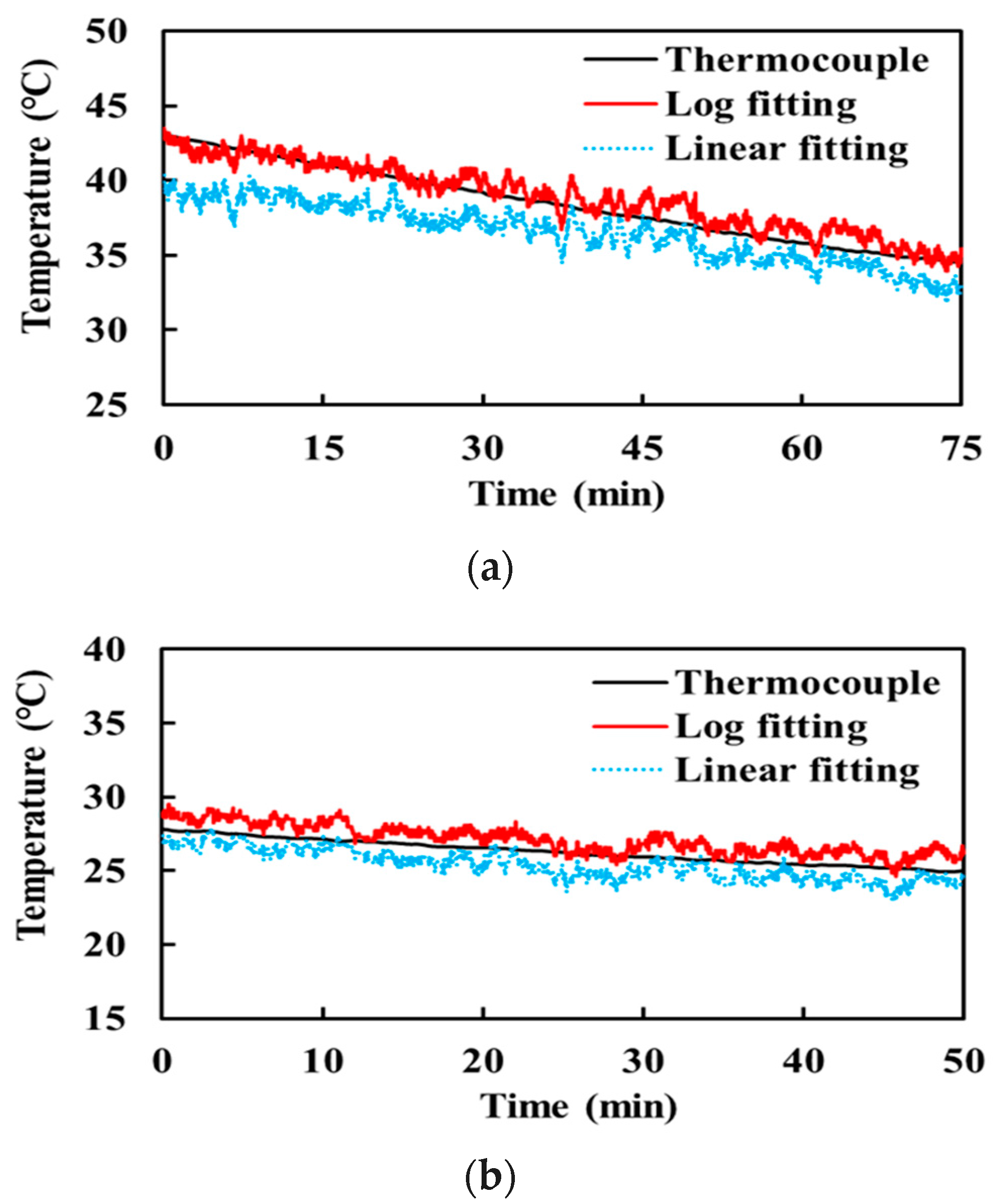
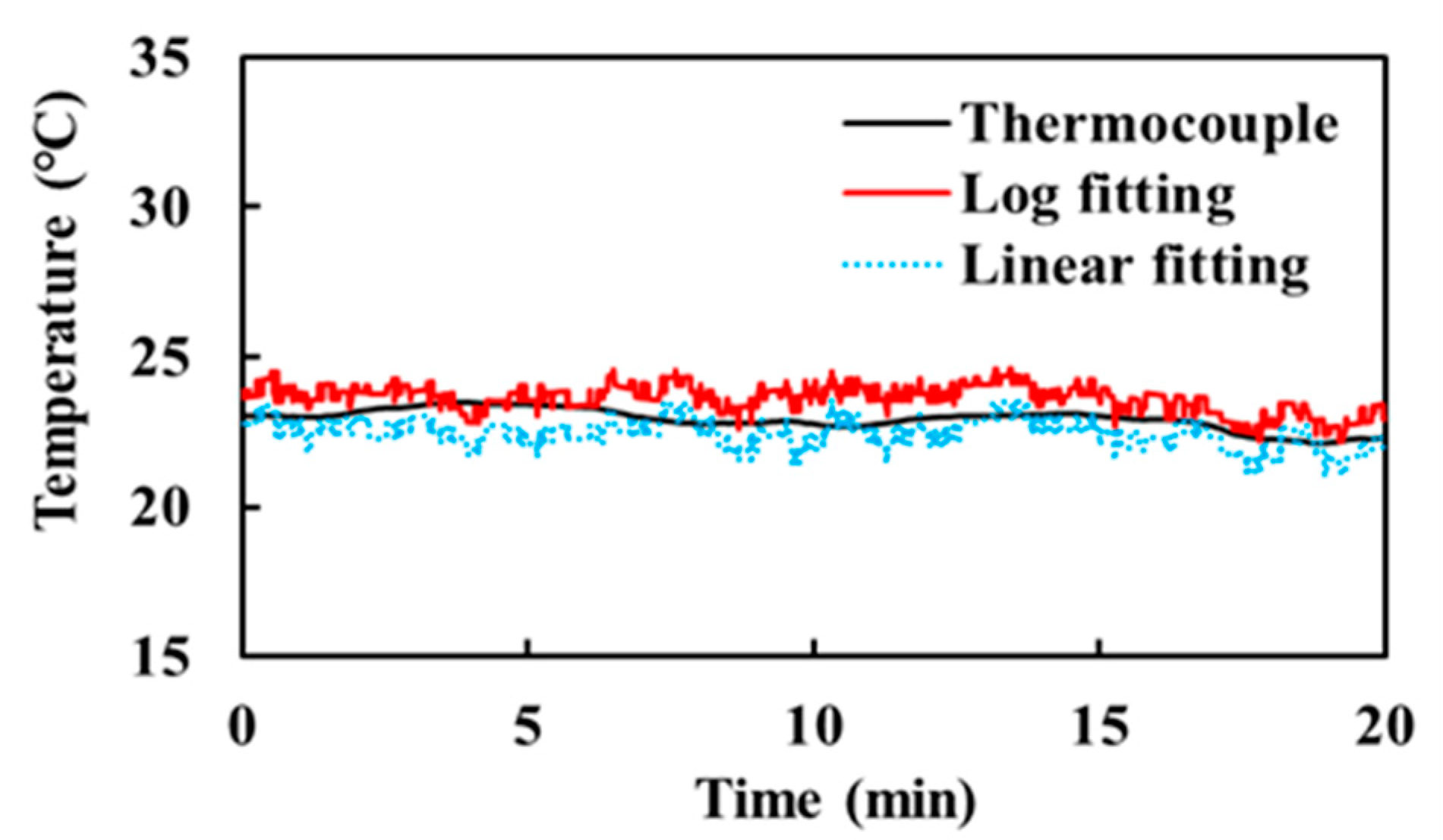
2.1. Radiometer with Two Reference Noise Sources
2.2. Two Reference Noise Sources
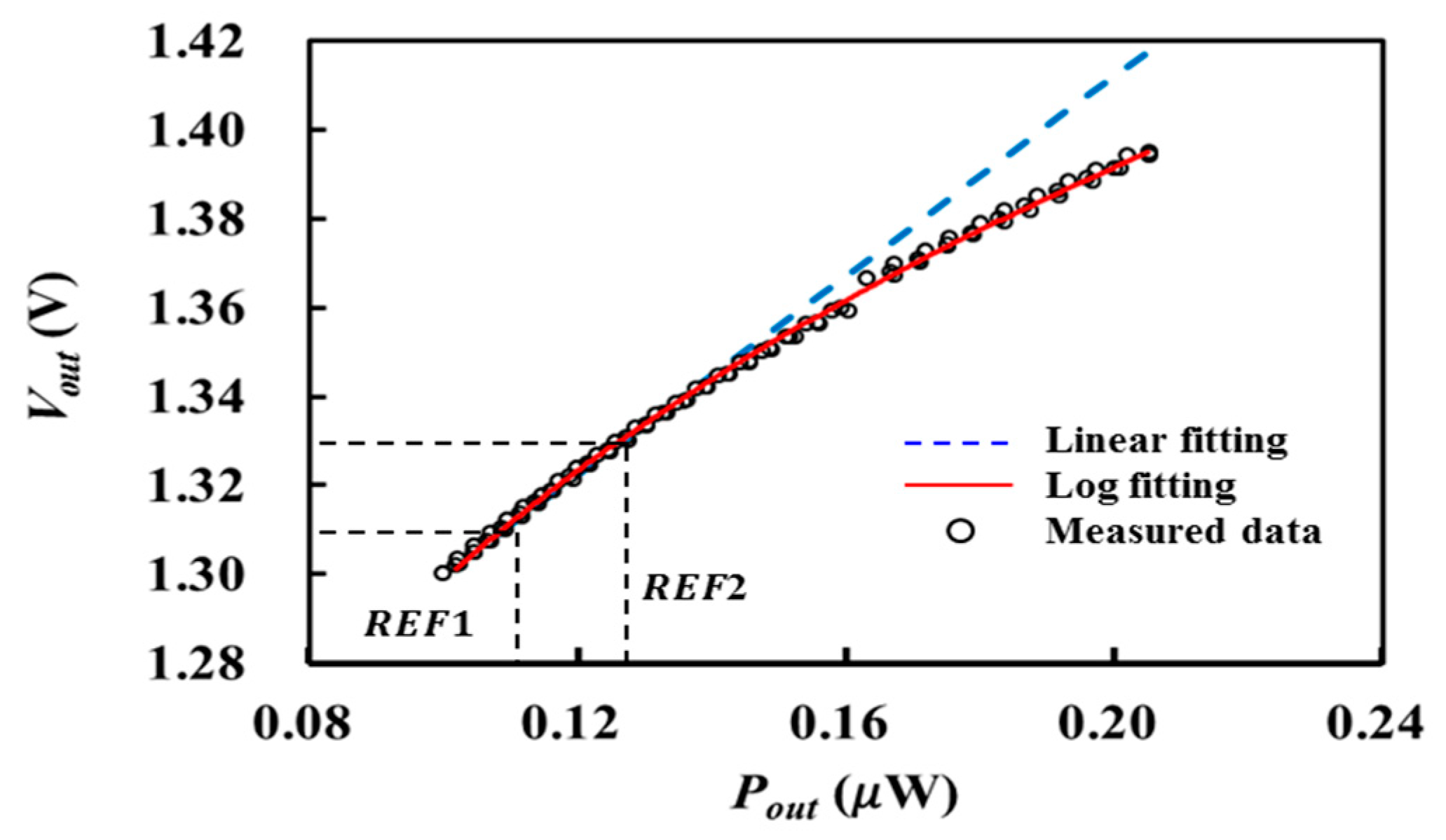
2.3. Logaritmic Detector
2.4. SP3T Switch Calibration
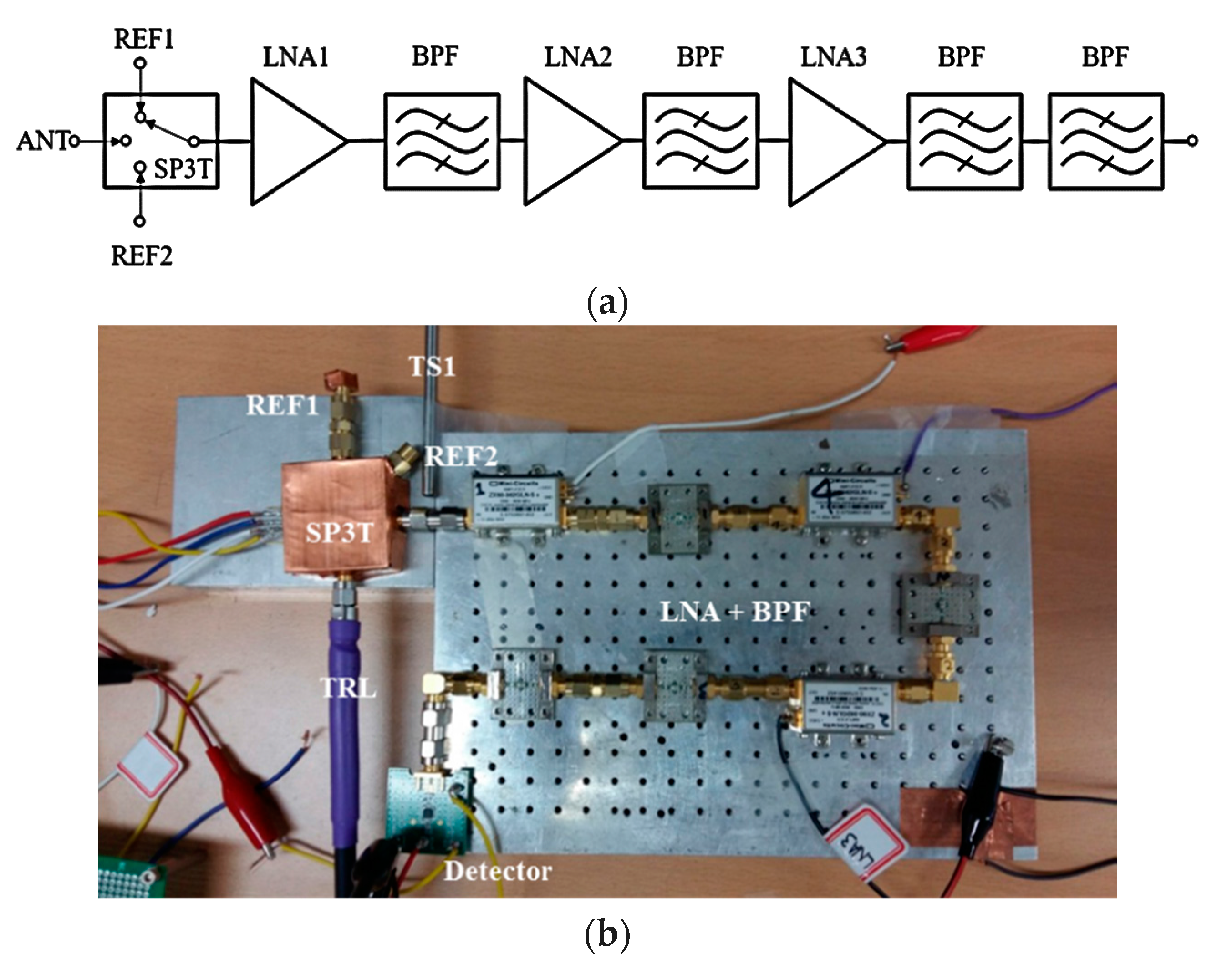
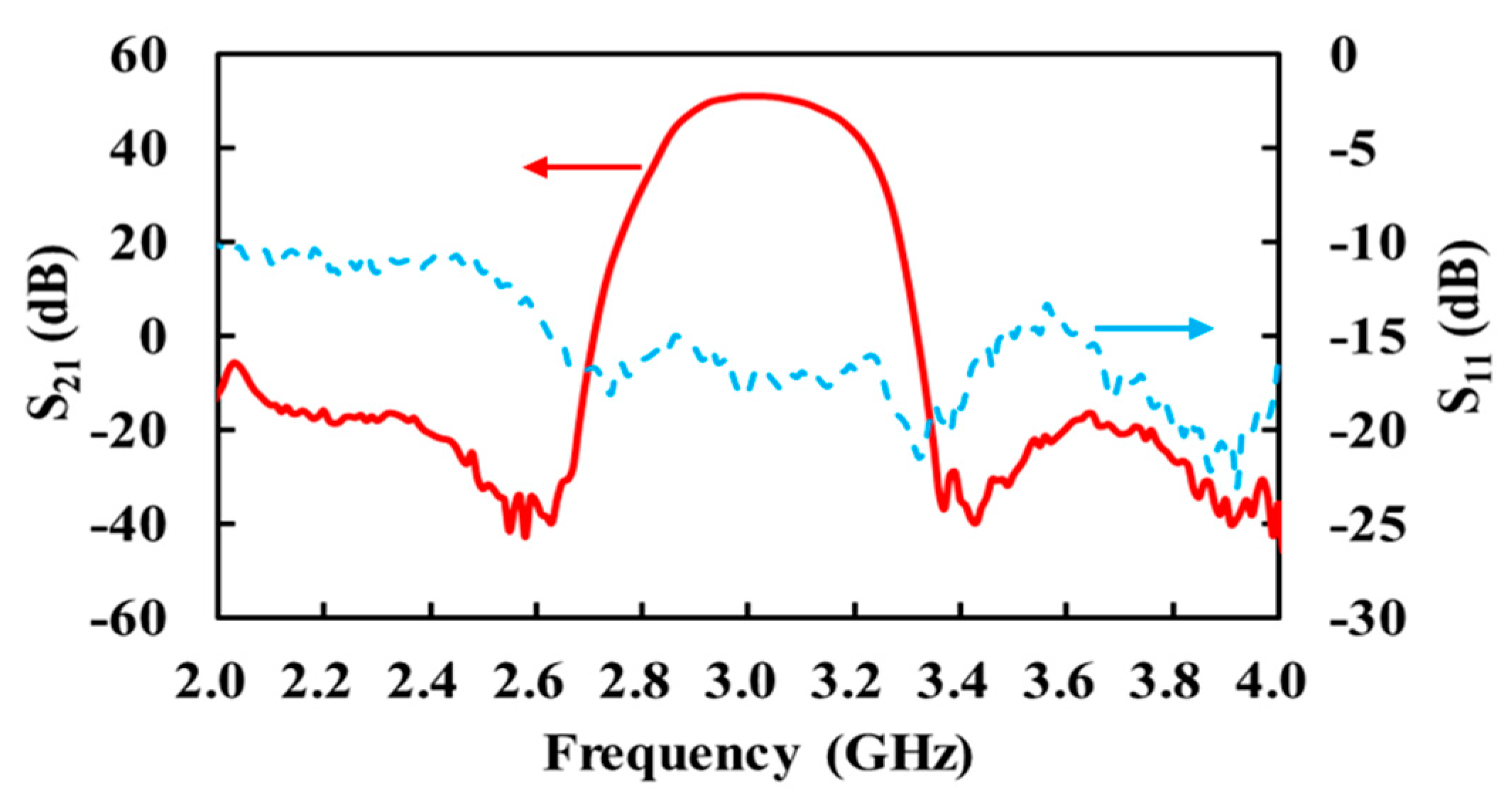
2.5. Receiver Design
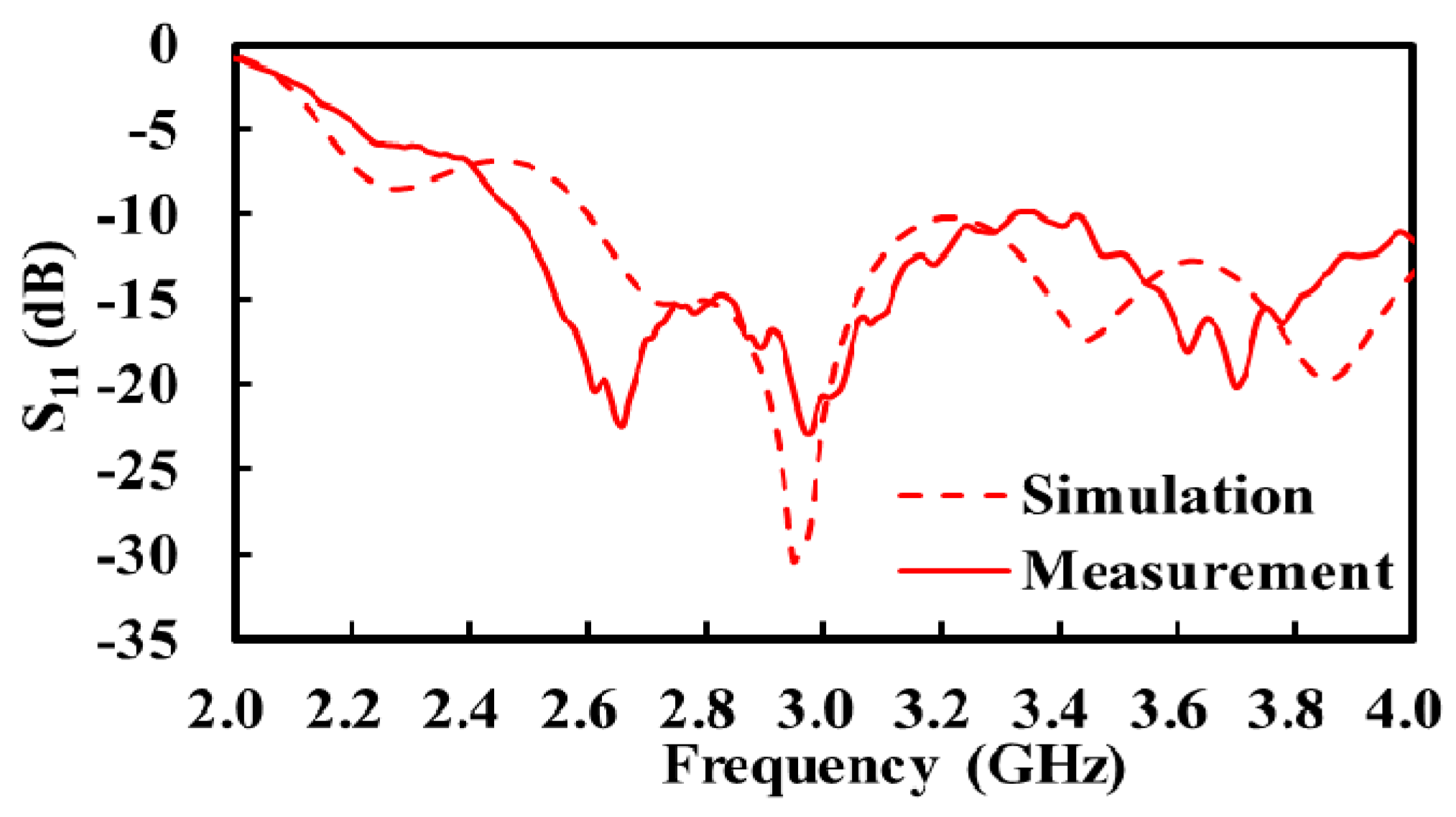
2.6. Antenna Design
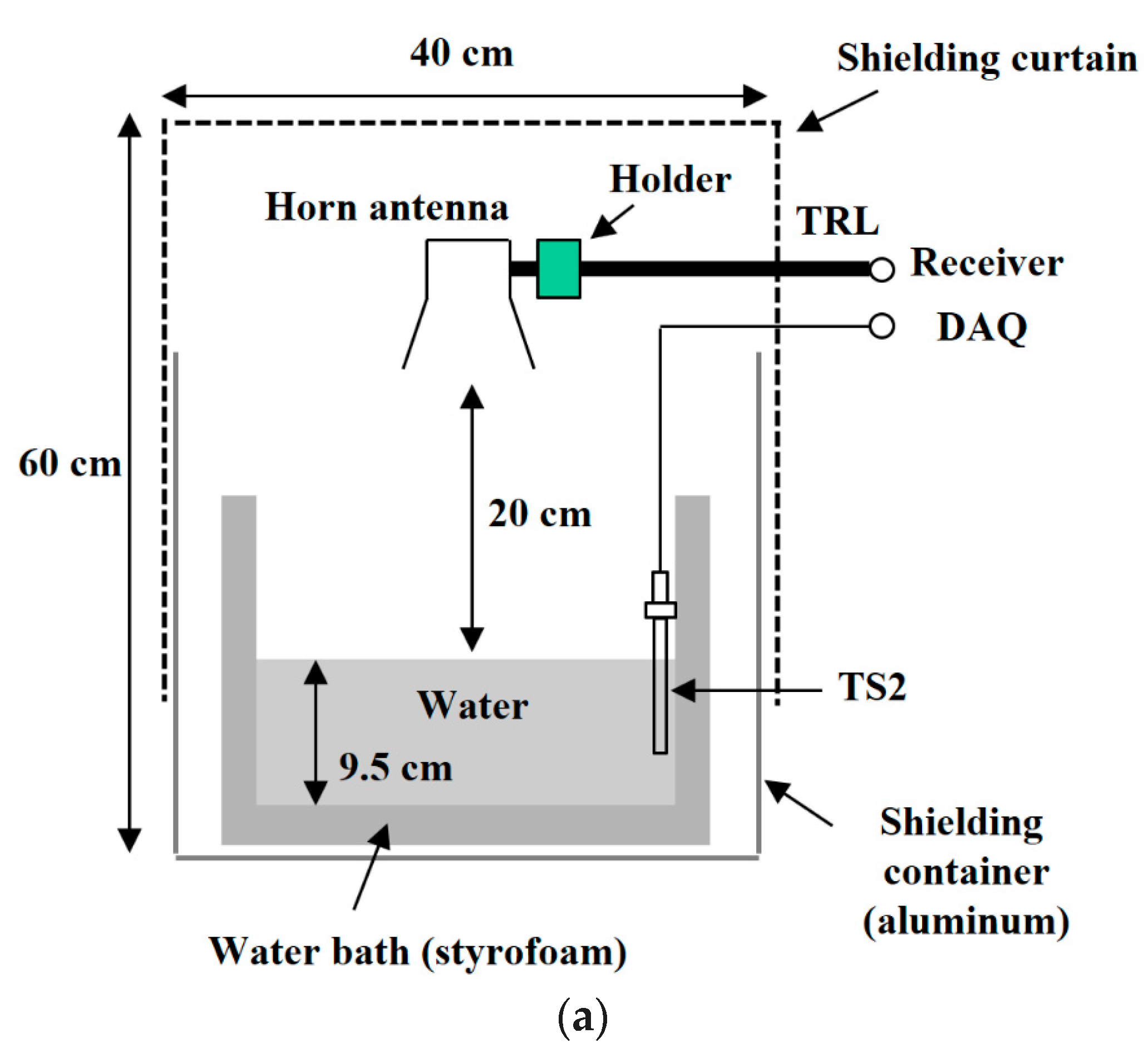
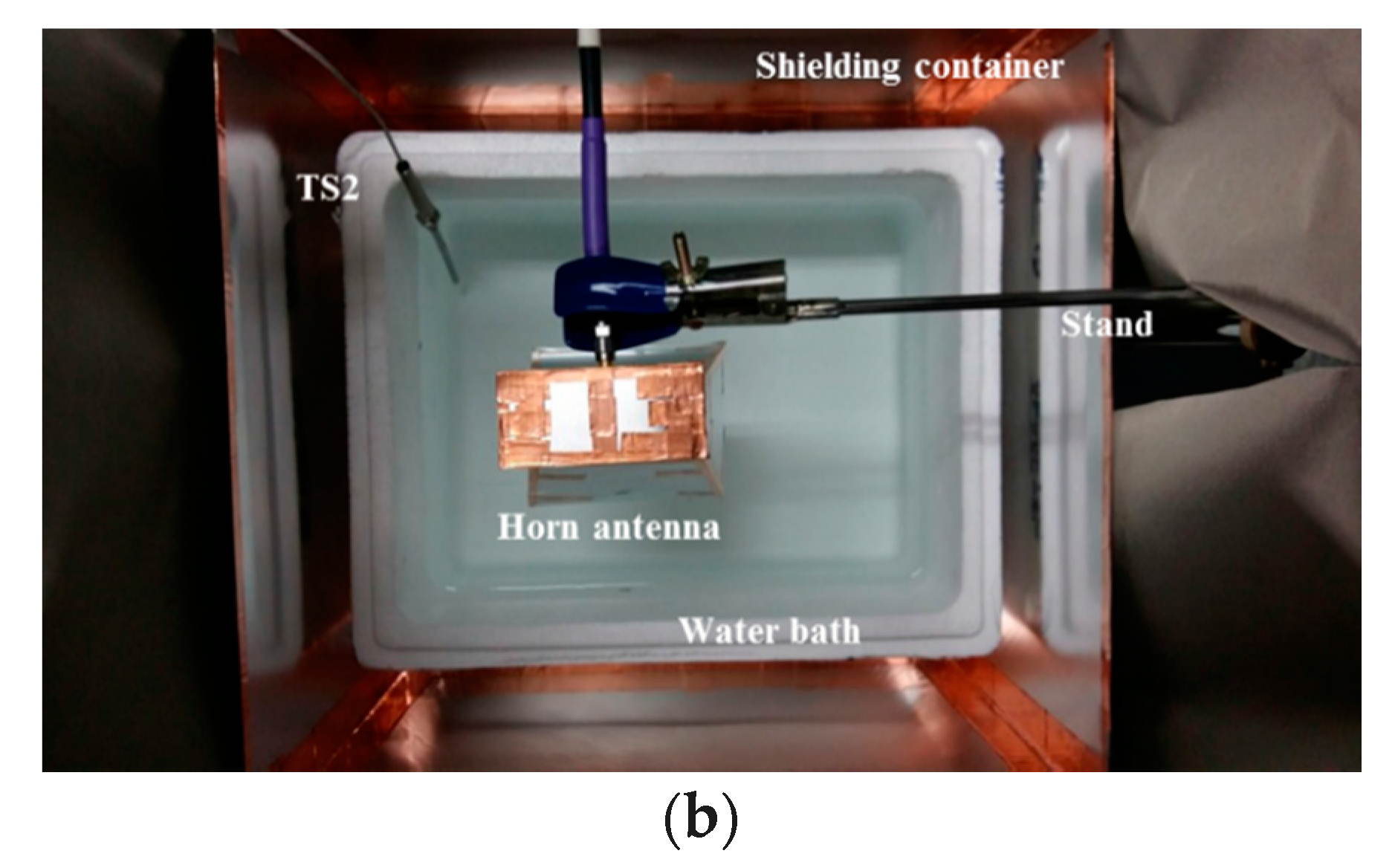
3. Temperature Measurement Setup
4. Temperature Measurement Result
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Bonds, Q.; Gerig, J.; Weller, T.M.; Herzig, P. Towards core body temperature measurement via close proximity radiometric sensing. IEEE Sens. J. 2012, 12, 519–526. [Google Scholar] [CrossRef]
- Ojica, S.; Iftemie, A. Thermographic Studies in Vivo and in Vitro for Detection of Tumor Structures Using Microwave Radiometry. In Proceedings of the 2013 IEEE International Symposium on Advanced Topics in Electrical Engineering, Bucharest, Romania, 23–25 May 2013; pp. 1–4. [Google Scholar]
- Klemetsen, O. Design and Evaluation of a Medical Microwave Radiometer for Observing Temperature Gradients Subcutaneously in the Human Body. Ph.D. Thesis, University of Tromsø, Tromsø, Norway, 2011. [Google Scholar]
- Ulaby, F.T.; Long, D.G. Microwave Radar and Radiometric Remote Sensing; University of Michigan Press: Ann Arbor, MI, USA, 2014. [Google Scholar]
- Sirizi, M.; Jones, W.L. Measurement of Atmospheric Noise Emission during Heavy Rain Events Using a C-band Radiometer. In Proceedings of the 2012 IEEE Southeast Conference, Orlando, FL, USA, 15–18 March 2012; pp. 1–4. [Google Scholar]
- Susek, W. Thermal microwave radiation for subsurface absolute temperature measurement. ACTA Phys. Pol. A 2010, 118, 1246–1249. [Google Scholar] [CrossRef]
- Colliander, A.; Ruokokoski, L.; Suomela, J.; Veijola, K.; Kettunen, J.; Kangas, V.; Aalto, A.; Levander, M.; Greus, H.; Hallikainen, M.T. Development and calibration of SMOS reference radiometer. IEEE Trans. Geosci. Remote Sens. 2007, 45, 1967–1977. [Google Scholar] [CrossRef]
- Klemetsen, O.; Birkelund, Y.; Jacobsen, S.K.; Maccarini, P.F.; Stauffer, P.R. Design of medical radiometer front-end for improved performance. Prog. Electromagn. Res. B 2011, 27, 289–306. [Google Scholar] [CrossRef]
- Goodberlet, M.A.; Mead, J.B. Two-load radiometer precision and accuracy. IEEE Trans. Geosci. Remote Sens. 2006, 44, 58–67. [Google Scholar] [CrossRef]
- Popovic, Z.; Momenroodaki, P.; Scheeler, R. Toward wearable wireless thermometers for internal body temperature measurements. IEEE Commun. Mag. 2014, 52, 118–125. [Google Scholar] [CrossRef]
- Kaisti, M.; Altti, M.; Poutanen, T. Uncertainty of radiometer calibration loads and its impact on radiometric measurements. IEEE Trans. Microw. Theory Technol. 2014, 62, 2435–2446. [Google Scholar] [CrossRef]
- Robert, S.; Zoya, P. A 1.4 GHz MMIC Active Cold Noise Source. In Proceedings of the 2013 IEEE Compound Semiconductor Integrated Circuit Symposium, Monterey, CA, USA, 13–16 October 2013; pp. 1–4. [Google Scholar]
- Robert, S. A Microwave Radiometer for Internal Body Temperature Measurement. Ph.D. Thesis, University of Colorado Boulder, Boulder, CO, USA, 2013. [Google Scholar]
- Li, Y.; Lang, L.; Li, Q.; Liu, S.; Gui, L. A Novel Dicke Microwave Radiometer without Temperature Control for Reference Match Load. In Proceedings of the 2016 IEEE International Conference on Microwave and Millimeter Wave Technology, Beijing, China, 5–8 June 2016; pp. 880–882. [Google Scholar]
- Tofighi, M.; Pardeshi, J.; Maicke, B. Microwave System and Methods for Combined Heating and Radiometric Sensing for Blood Perfusion Measurement of Tissue. In Proceedings of the 2016 IEEE MTT-s International Microwave Symposium, San Francisco, CA, USA, 22–27 May 2016; pp. 1–4. [Google Scholar]
- Chae, C.; Kwon, J.; Kim, Y. A study of compensation for temporal and spatial physical temperature variation in total power radiometers. IEEE Sens. J. 2012, 12, 2306–2312. [Google Scholar] [CrossRef]
- Klemetsen, O.; Jacobsen, S. Improved radiometric performance attained by an elliptical microwave antenna with suction. IEEE Trans. Biomed. Eng. 2012, 59, 263–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pozar, D.M. Microwave Engineering, 4th ed.; Wiley: New York, NY, USA, 2012. [Google Scholar]
- Momenroodaki, P.; Popovic, Z.; Scheeler, R. A 1.4-GHz Radiometer for Internal Body Temperature Measurements. In Proceedings of the 2015 IEEE European Microwave Conference, Paris, France, 7–10 September 2015; pp. 694–697. [Google Scholar]
- Arthur, R.M.; Straube, W.L.; Trobaugh, J.W.; Moros, E.G. Non-invasive estimation of hyperthermia temperatures with ultrasound. Int. J. Hyperth. 2005, 21, 589–600. [Google Scholar] [CrossRef] [PubMed]
- Sugiura, T.; Hirata, H.; Hand, J.W.; Van Leeuwen, J.M.M.; Mizushina, S. Five-band microwave radiometer system for noninvasive brain temperature measurement in newborn babies: Phantom experiment and confidence interval. Radio Sci. 2011, 46. [Google Scholar] [CrossRef]
- Chae, C.; Kwon, J.; Kim, Y. Ka-band total power radiometer and temperature control system for calibration of spatial temperature distribution. IEEE Sens. J. 2010, 10, 1555–1556. [Google Scholar] [CrossRef]
- Jacobsen, S.; Klemetsen, O. Improved detectability in medical microwave radio-thermometers as obtained by active antennas. IEEE Trans. Biomed. Eng. 2008, 55, 2778–2785. [Google Scholar] [CrossRef] [PubMed]
- Skou, N.; Sobjaerg, S.S.; Balling, J. Performance Measurements on Active Cold Loads for Radiometer Calibration. In Proceedings of the 2007 IEEE International Geoscience and Remote Sensing Symposium, Barcelona, Spain, 23–28 July 2007; pp. 2431–2434. [Google Scholar]
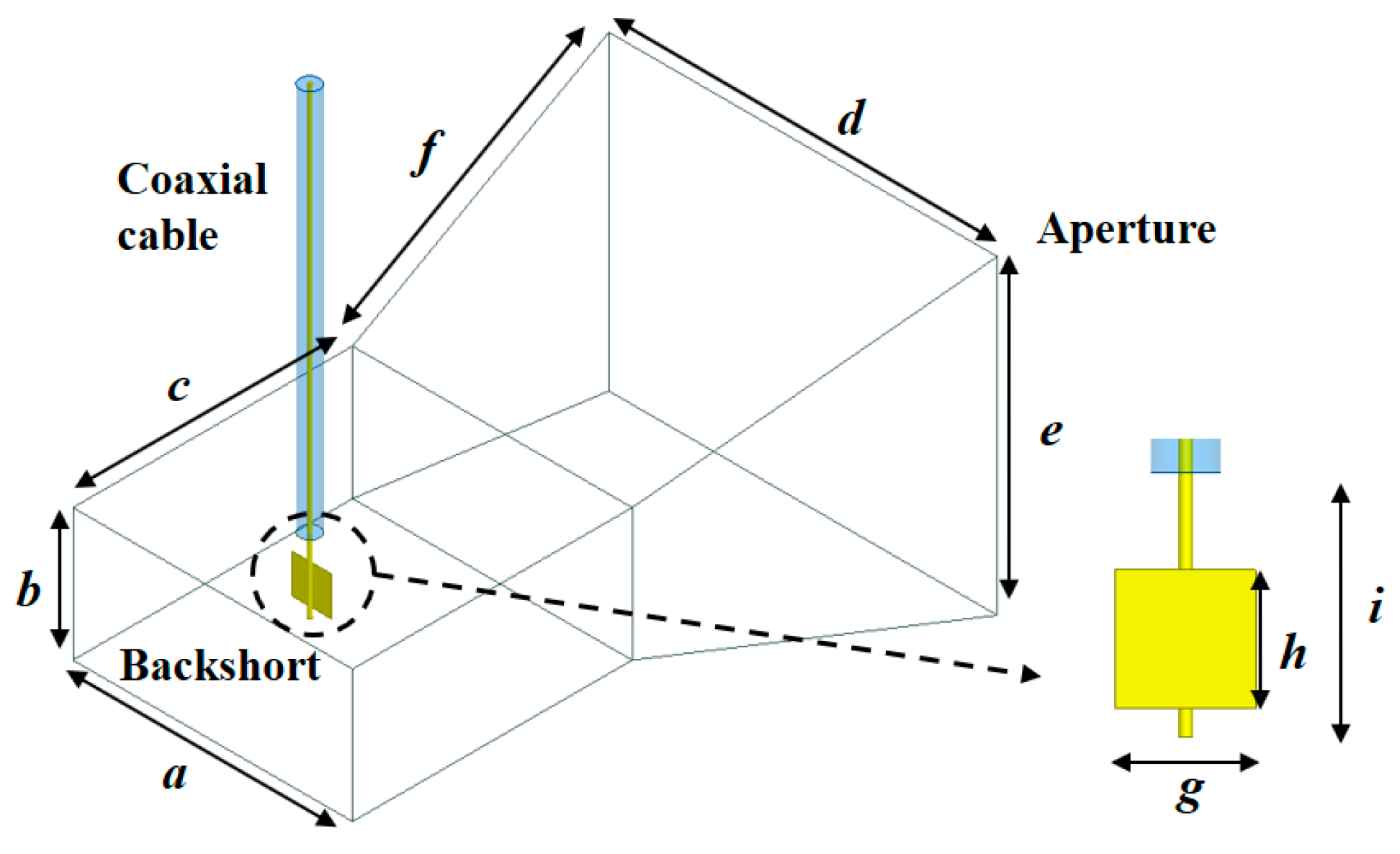
| a | b | c | d | e | f | g | h | i | |
|---|---|---|---|---|---|---|---|---|---|
| Length (mm) | 72 | 34 | 72 | 100 | 80 | 102.6 | 10 | 10 | 19 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, W.; Jeong, J. Total Power Radiometer for Medical Sensor Applications Using Matched and Mismatched Noise Sources. Sensors 2017, 17, 2105. https://doi.org/10.3390/s17092105
Park W, Jeong J. Total Power Radiometer for Medical Sensor Applications Using Matched and Mismatched Noise Sources. Sensors. 2017; 17(9):2105. https://doi.org/10.3390/s17092105
Chicago/Turabian StylePark, Woojin, and Jinho Jeong. 2017. "Total Power Radiometer for Medical Sensor Applications Using Matched and Mismatched Noise Sources" Sensors 17, no. 9: 2105. https://doi.org/10.3390/s17092105




