Diagnosed but Not Undiagnosed Diabetes Is Associated with Depression in Rural Areas
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Data Collection
2.3. Definitions
2.4. Measuring Depression Symptoms
2.5. Statistical Analysis
3. Results
3.1. Basic Characteristics of the Study Population
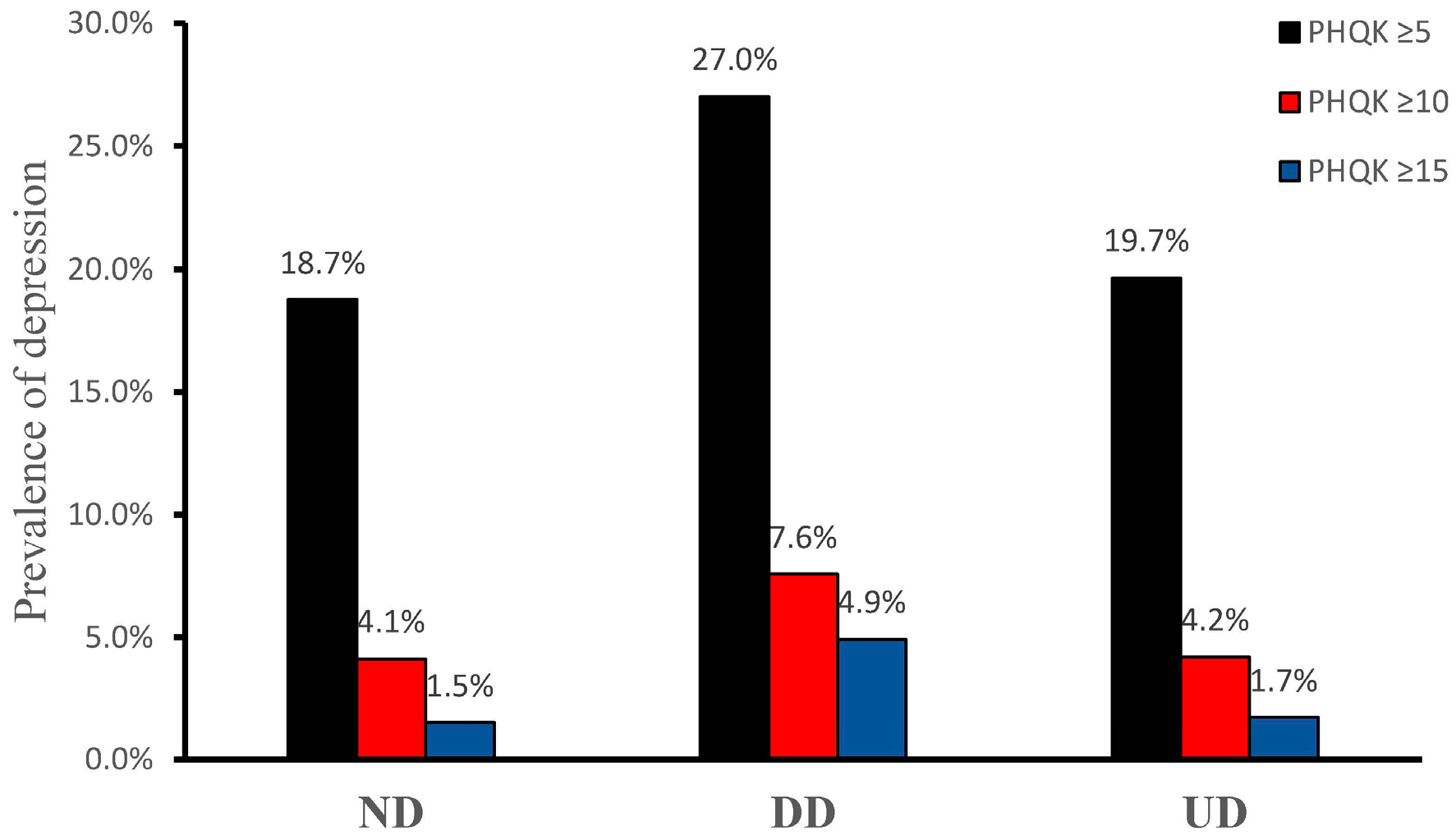
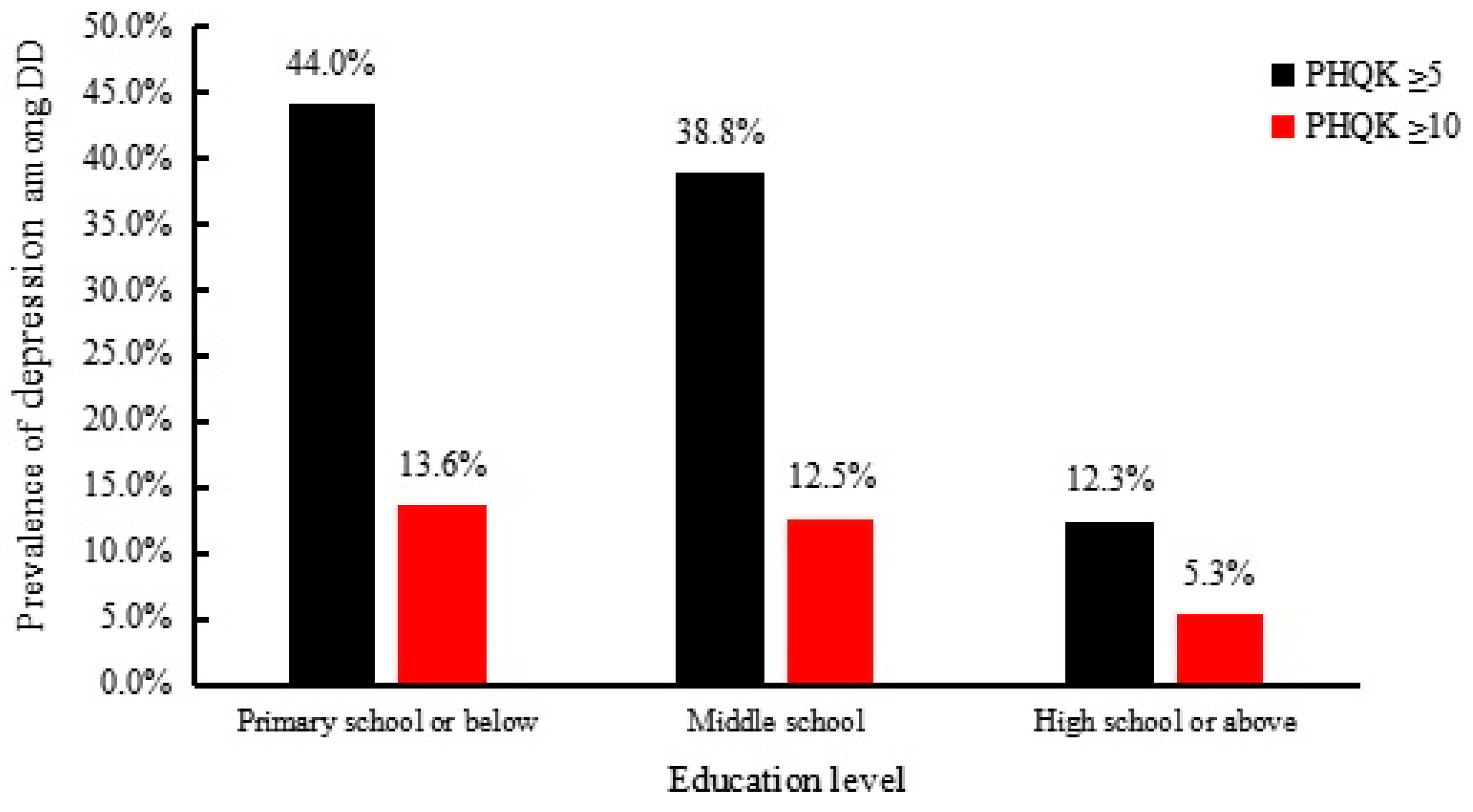
3.2. Prevalence of Depression
3.3. Results from Multivariate Logistic Regression Analyses
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Zhang, X.; Bullard, K.M.; Cotch, M.F.; Wilson, M.R.; Rovner, B.W.; McGwin, G. Association between depression and functional vision loss in persons 20 years of age or older in the United States, NHANES 2005–2008. JAMA Ophthalmol. 2013, 131, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Kan, C.; Silva, N.; Golden, S.H.; Rajala, U.; Timonen, M.; Stahl, D.; Ismail, K. A systematic review and meta-analysis of the association between depression and insulin resistance. Diabetes Care 2013, 36, 480–489. [Google Scholar] [CrossRef] [PubMed]
- Laake, J.P.; Stahl, D.; Amiel, S.A. The association between depressive symptoms and systemic inflammation in people with type 2 diabetes: Findings from the South London Diabetes Study. Diabetes Care 2014, 37, 2186–2192. [Google Scholar] [CrossRef] [PubMed]
- Katon, W.; Lyles, C.R.; Parker, M.M. Association of depression with increased risk of dementia in patients with type 2 diabetes: The Diabetes and Aging Study. Arch. Gen. Psychiatr. 2012, 69, 410–417. [Google Scholar] [PubMed]
- Mommersteeg, P.M.C.; Herr, R.; Pouwer, F. The association between diabetes and an episode of depressive symptoms in the 2002 World Health Survey: An analysis of 231,797 individuals from 47 countries. Diabet. Med. 2013, 30, e208–e214. [Google Scholar] [CrossRef] [PubMed]
- Look AHEAD Research Group. Impact of intensive lifestyle intervention on depression and health-related quality of life in type 2 diabetes: The Look AHEAD Trial. Diabetes Care 2014, 37, 1544–1553. [Google Scholar]
- Mezuk, B.; Chen, Y.; Yu, C. Depression, anxiety, and prevalent diabetes in the Chinese population: Findings from the China Kadoorie Biobank of 0.5 million people. J. Psychosom. Res. 2013, 75, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Olvera, R.L.; Fisher-Hoch, S.P.; Williamson, D.E. Depression in Mexican Americans with diagnosed and undiagnosed diabetes. Psychol. Med. 2016, 46, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Collins, P.Y.; Insel, T.R.; Chockalingam, A. Grand challenges in global mental health: Integration in research, policy, and practice. PLoS Med. 2013, 10, e1001434. [Google Scholar] [CrossRef] [PubMed]
- Mathias, K.; Kermode, M.; San Sebastian, M. Under the banyan tree-exclusion and inclusion of people with mental disorders in rural North India. BMC Public Health 2015, 15, 446. [Google Scholar] [CrossRef] [PubMed]
- Mendenhall, E.; Norris, S.A.; Shidhaye, R. Depression and type 2 diabetes in low-and middle-income countries: A systematic review. Diabetes Res. Clin. Pract. 2014, 103, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Leone, T.; Coast, E.; Narayanan, S. Diabetes and depression comorbidity and socio-economic status in low and middle income countries (LMICs): A mapping of the evidence. Glob. Health 2012, 8, 39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, G.Z.; Guo, L.; Wang, X.Z.; Song, H.J.; Li, Z.; Wang, J.; Sun, Y.X. Prevalence of atrial fibrillation and its risk factors in rural China: A cross-sectional study. Int. J. Cardiol. 2015, 26, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Sun, G.Z.; Li, Z.; Guo, L. High prevalence of dyslipidemia and associated risk factors among rural Chinese adults. Lipids Health Dis. 2014, 13, 189. [Google Scholar] [CrossRef] [PubMed]
- Hu, G.; Tuomilehto, J.; Silventoinen, K.; Barengo, N.; Jousilahti, P. Joint effects of physical activity, body mass index, waist circumference and waist-to-hip ratio with the risk of cardiovascular disease among middle-aged Finnish men and women. Eur. Heart J. 2004, 25, 2212–2219. [Google Scholar] [CrossRef] [PubMed]
- Panagiotakos, D.B.; Pitsavos, C.; Chrysohoou, C. Epidemiology of overweight and obesity in a Greek adult population: The ATTICA Study. Obes. Res. 2004, 12, 1914–1920. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.M.; Lee, J.S.; Lee, J. Prevalence of Diabetes and Impaired Fasting Glucose in Korea Korean National Health and Nutrition Survey 2001. Diabetes Care 2006, 29, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.; Sun, Z.; Zheng, L. Prevalence of Diabetes and Impaired Fasting Glucose in Hypertensive Adults in Rural China: Far from Leveling-Off. Int. J. Environ. Res. Public Health 2015, 12, 14764–14779. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Kroenke, K.; Herzog, W. Measuring depression outcome with a brief self-report instrument: Sensitivity to change of the Patient Health Questionnaire (PHQ-9). J. Affect. Disord. 2004, 81, 61–66. [Google Scholar] [CrossRef]
- Pignone, M.P.; Gaynes, B.N.; Rushton, J.L. Screening for depression in adults: A summary of the evidence for the US Preventive Services Task Force. Ann. Intern. Med. 2002, 136, 765–776. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; Text Revision; DSM-IV-TR; American Psychiatric Association: Washington, DC, USA, 2001; p. 85. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. Gen. Hosp. Psychiatry 2010, 32, 345–359. [Google Scholar] [CrossRef] [PubMed]
- Needham, B.L.; Mezuk, B.; Bareis, N. Depression, anxiety and telomere length in young adults: Evidence from the National Health and Nutrition Examination Survey. Mol. Psychiatry 2015, 20, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Magnan, E.M.; Palta, M.; Mahoney, J.E. The relationship of individual comorbid chronic conditions to diabetes care quality. BMJ Open Diabetes Res. Care 2015, 3, e000080. [Google Scholar] [CrossRef] [PubMed]
- Loucks, E.B.; Gilman, S.E.; Howe, C.J. Education and Coronary Heart Disease Risk Potential Mechanisms Such as Literacy, Perceived Constraints, and Depressive Symptoms. Health Educ. Behav. 2015, 42, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Niles, A.N.; Dour, H.J.; Stanton, A.L. Anxiety and depressive symptoms and medical illness among adults with anxiety disorders. J. Psychosom. Res. 2015, 78, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Ford, E.S.; Zhao, G. Association between diagnosed diabetes and serious psychological distress among US adults: The Behavioral Risk Factor Surveillance System. Int. J. Public Health 2009, 54, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Xu, X.; Hall, J.J. Differences in depression between unknown diabetes and known diabetes: Results from China health and retirement longitudinal study. Int. Psychogeriatr. 2016, 28, 1191–1199. [Google Scholar] [CrossRef] [PubMed]
- Meurs, M.; Roest, A.M.; Wolffenbuttel, B.H. Association of Depressive and Anxiety Disorders With Diagnosed Versus Undiagnosed Diabetes: An Epidemiological Study of 90,686 Participants. Psychosom. Med. 2015, 78, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Magliano, D.J.; Zimmet, P.Z. The worldwide epidemiology of type 2 diabetes mellitus—Present and future perspectives. Nat. Rev. Endocrinol. 2012, 8, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Trento, M.; Charrier, L.; Salassa, M. Depression, anxiety and cognitive function in patients with type 2 diabetes: An 8-year prospective observational study. Acta Diabetol. 2015, 52, 1157–1166. [Google Scholar] [CrossRef] [PubMed]
| Variables | ND (n = 10,310) | DD (n = 529) | UD (n = 692) | p-Value |
|---|---|---|---|---|
| Age (year) | 53.4 ± 10.6 | 58.4 ± 9.0 | 57.0 ± 10.1 | <0.01 |
| Male gender | 4799 (46.5) | 186 (35.2) | 349 (50.4) | <0.01 |
| Female gender | 5511 (53.5) | 343 (64.8) | 343 (49.6) | |
| Marital status | ||||
| Married | 9465 (91.8) | 479 (90.5) | 618 (89.3) | 0.01 |
| Single | 185 (1.8) | 5 (0.9) | 11 (1.6) | |
| Widowed | 660 (6.4) | 45 (8.5) | 63 (9.1) | |
| Race of Han | 9764 (94.7) | 505 (95.5) | 649 (93.8) | 0.42 |
| others | 546 (5.3) | 24 (4.5) | 43 (6.2) | |
| Education | <0.01 | |||
| primary school or below | 5021 (48.7) | 322 (60.9) | 400 (57.8) | |
| middle school | 4297 (41.7) | 153 (28.9) | 244 (35.3) | |
| high school or above | 992 (9.6) | 54 (10.2) | 48 (6.9) | |
| Family income (CNY/year) | ||||
| ≤5000 | 1258 (12.2) | 74 (14.0) | 98 (14.2) | 0.39 |
| 5000–20,000 | 5625 (54.6) | 285 (53.9) | 378 (54.6) | |
| >20,000 | 3427 (33.2) | 170 (32.1) | 216 (31.2) | |
| Smoking | 3687 (35.8) | 108 (20.4) | 264 (38.2) | <0.01 |
| Drinking | 2328 (22.6) | 63 (11.9) | 197 (28.5) | <0.01 |
| Physical activity | 1.00 | |||
| Low | 3076 (29.8) | 156 (29.5) | 205 (29.6) | |
| Moderate | 6653 (64.5) | 343 (64.8) | 449 (64.9) | |
| High | 581 (5.6) | 30 (5.7) | 38 (5.5) | |
| BMI (kg/m2) | 24.6 ± 3.6 | 26.2 ± 3.6 | 26.2 ± 3.8 | <0.01 |
| Sleep duration (h/d) | 7.3 ± 1.9 | 7.1 ± 2.1 | 7.3 ± 2.7 | 0.09 |
| Diet score | 2.3 ± 1.1 | 2.0 ± 1.1 | 2.3 ± 1.1 | <0.01 |
| History of hypertension | ||||
| no | 8269 (80.2) | 258 (48.8) | 445 (64.3) | 0.39 |
| yes | 2041 (19.8) | 271 (51.2) | 247 (35.7) | |
| History of heart disease a | ||||
| no | 9374 (90.9) | 509 (96.2) | 641 (92.6) | <0.01 |
| yes | 936 (9.1) | 20 (3.8) | 51 (7.4) | |
| History of stroke | ||||
| no | 9724 (94.3) | 514 (97.2) | 659 (95.2) | 0.01 |
| yes | 586 (5.7) | 15 (2.8) | 33 (4.8) | |
| History of renal disease | ||||
| no | 7730 (75.0) | 380 (71.8) | 522 (75.4) | 0.25 |
| yes | 2580 (25.0) | 149 (28.2) | 170 (24.6) | |
| Medication used b | ||||
| no | 6778 (65.7) | 429 (81.1) | 521 (75.3) | <0.01 |
| yes | 3532 (34.3) | 100 (18.9) | 171 (24.7) | |
| PHQ-9 score | 2.9 ± 3.6 | 4.6 ± 4.7 | 3.0 ± 3.7 | <0.01 |
| Model | Variables | PHQK ≥ 5 | PHQK ≥ 10 | ||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||
| Model 1 | ND | 1.00 (reference) | 1.00 (reference) | ||||
| DD | 1.70 | 1.412.04 | <0.01 | 1.89 | 1.43–2.49 | <0.01 | |
| UD | 1.01 | 0.84–1.21 | 0.95 | 0.96 | 0.69–1.34 | 0.81 | |
| Model 2 | ND | 1.00 (reference) | 1.00 (reference) | ||||
| DD | 1.68 | 1.38–2.03 | <0.01 | 1.93 | 1.45–2.57 | <0.01 | |
| UD | 1.00 | 0.83–1.20 | 0.97 | 0.96 | 0.69–1.34 | 0.80 | |
| Model 3 | ND | 1.00 (reference) | 1.00 (reference) | ||||
| DD | 1.75 | 1.43–2.12 | <0.01 | 1.94 | 1.44–2.61 | <0.01 | |
| UD | 1.06 | 0.88–1.27 | 0.56 | 0.99 | 0.71–1.40 | 0.96 | |
| Model 4 | ND | 1.00 (reference) | 1.00 (reference) | ||||
| DD | 1.62 | 1.32–1.98 | <0.01 | 1.70 | 1.25–2.31 | 0.00 | |
| UD | 1.04 | 0.86–1.25 | 0.71 | 0.92 | 0.65–1.31 | 0.66 | |
| Variable | PHQ ≥ 5 | PHQ ≥ 10 | ||||
|---|---|---|---|---|---|---|
| p-Value | OR | 95% CI | p-Value | OR | 95% CI | |
| Age (year) | 0.86 | 1.00 | 0.98–1.03 | 0.29 | 1.02 | 0.98–1.06 |
| Male gender | 0.37 | 1.27 | 0.76–2.12 | 0.13 | 1.87 | 0.83–4.25 |
| Race of Han | 0.72 | 1.19 | 0.47–3.02 | 0.72 | 1.27 | 0.34–4.82 |
| Marital status | ||||||
| Married | 0.40 | 1.00 (reference) | 0.97 | 1.00 (reference) | ||
| Single | 0.54 | 0.80 | 0.40–1.62 | 0.81 | 1.12 | 0.43–2.92 |
| Widowed | 0.19 | 0.20 | 0.02–2.16 | 1.00 | 0.00 | 0 |
| Family income (CNY/year) | ||||||
| ≤5000 | 0.22 | 1.00 (reference) | 0.33 | 1.00 (reference) | ||
| 5000–20,000 | 0.31 | 0.75 | 0.42–1.31 | 0.50 | 0.78 | 0.37–1.62 |
| >20,000 | 0.09 | 0.58 | 0.31–1.09 | 0.15 | 0.53 | 0.22–1.26 |
| Education | ||||||
| High school or above | 0.01 | 1.00 (reference) | 0.60 | 1.00 (reference) | ||
| Primary school or below | 0.00 | 3.94 | 1.65–9.45 | 0.48 | 1.58 | 0.44–5.71 |
| Middle school | 0.00 | 3.93 | 1.62–9.56 | 0.33 | 1.91 | 0.52–7.10 |
| BMI (kg/m2) | 0.24 | 0.97 | 0.91–1.02 | 0.53 | 0.97 | 0.90–1.06 |
| Diet score | 0.01 | 0.80 | 0.67–0.95 | 0.03 | 0.75 | 0.58–0.97 |
| Family history of diabetes | 0.55 | 0.89 | 0.59–1.32 | 0.48 | 0.80 | 0.44–1.47 |
| Smoking | 0.03 | 1.75 | 1.05–2.94 | 0.26 | 1.55 | 0.72–3.36 |
| Drinking | 0.98 | 0.99 | 0.50–1.96 | 0.83 | 1.14 | 0.37–3.54 |
| Totalsleep | 0.00 | 0.85 | 0.76–0.94 | 0.07 | 0.87 | 0.76–1.01 |
| Physical activity | ||||||
| Low | 0.77 | 1.00 (reference) | 0.46 | 1.00 (reference) | ||
| Moderate | 0.50 | 0.86 | 0.57–1.32 | 0.84 | 1.07 | 0.58–1.97 |
| High | 0.98 | 1.01 | 0.43–2.40 | 0.26 | 0.40 | 0.08–1.97 |
| History of heart disease a | 0.77 | 1.08 | 0.65–1.79 | 0.69 | 1.16 | 0.56–2.38 |
| History of stroke | 0.48 | 0.77 | 0.37–1.60 | 0.34 | 0.54 | 0.15–1.92 |
| Medication used b | 0.36 | 0.77 | 0.45–1.34 | 0.14 | 0.50 | 0.20–1.27 |
| History of hypertension | 0.71 | 1.08 | 0.72–1.62 | 0.78 | 1.09 | 0.60–1.98 |
| History of renal disease | 0.42 | 1.19 | 0.78–1.83 | 0.87 | 1.05 | 0.57–1.93 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Z.; Guo, X.; Jiang, H.; Sun, G.; Sun, Y.; Abraham, M.R. Diagnosed but Not Undiagnosed Diabetes Is Associated with Depression in Rural Areas. Int. J. Environ. Res. Public Health 2016, 13, 1136. https://doi.org/10.3390/ijerph13111136
Li Z, Guo X, Jiang H, Sun G, Sun Y, Abraham MR. Diagnosed but Not Undiagnosed Diabetes Is Associated with Depression in Rural Areas. International Journal of Environmental Research and Public Health. 2016; 13(11):1136. https://doi.org/10.3390/ijerph13111136
Chicago/Turabian StyleLi, Zhao, Xiaofan Guo, Hongkun Jiang, Guozhe Sun, Yingxian Sun, and Maria Roselle Abraham. 2016. "Diagnosed but Not Undiagnosed Diabetes Is Associated with Depression in Rural Areas" International Journal of Environmental Research and Public Health 13, no. 11: 1136. https://doi.org/10.3390/ijerph13111136





