Non-Responsive Feeding Practices, Unhealthy Eating Behaviors, and Risk of Child Overweight and Obesity in Southeast Asia: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction and Data Synthesis
2.4. Quality Assessment of Included Studies
3. Results
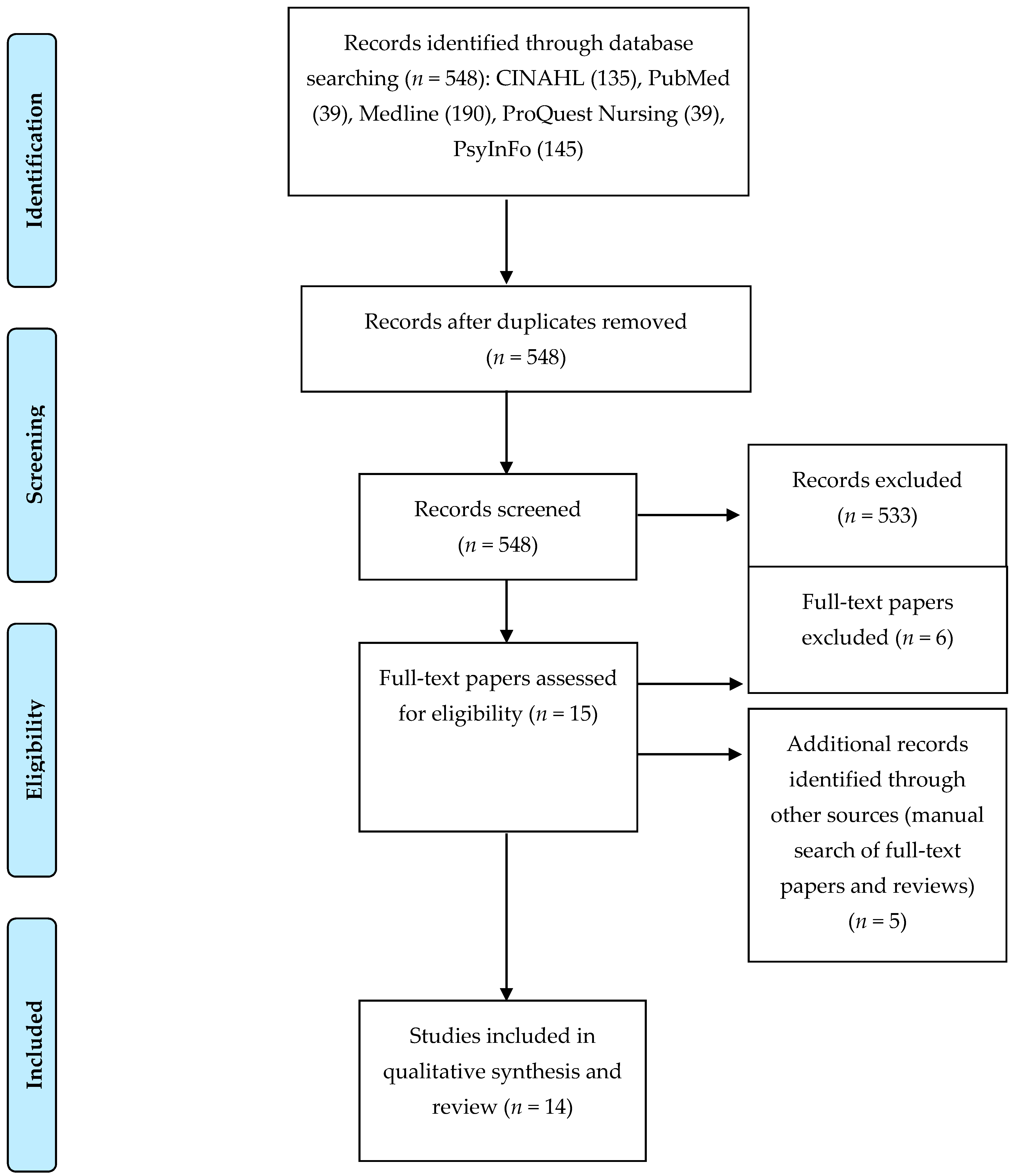
3.1. Search
3.2. Summary of Included Studies
3.2.1. Studies with Preschool-Age Children
Breastfeeding Initiation and Duration
Non-Responsive Feeding Practices
Unhealthy Eating Habits
3.2.2. Studies with School-Age Children
Breastfeeding Initiation and Duration
Non-Responsive Feeding Practices
Unhealthy Eating Habits
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- De Onis, M.; Blössner, M.; Borghi, E. Global prevalence and trends of overweight and obesity among preschool children. Am. J. Clin. Nutr. 2010, 92, 1257–1264. [Google Scholar] [CrossRef] [PubMed]
- ASEAN; UNICEF; WHO. Regional Report on Nutrition Security in ASEAN. Available online: https://www.unicef.org/eapro/Regional_Report_on_Nutrition_Security_in_ASEAN_(Volume_2).pdf (accessed on 25 February 2017).
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Gakidou, E. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Angkurawaranon, C.; Jiraporncharoen, W.; Chenthanakij, B.; Doyle, P.; Nitsch, D. Urban environments and obesity in Southeast Asia: A systematic review, meta-analysis and meta-regression. PLoS ONE 2014, 9, e113547. [Google Scholar] [CrossRef] [PubMed]
- Lipoeto, N.I.; Lin, K.G.; Angeles-Agdeppa, I. Food consumption patterns and nutrition transition in South-East Asia. Public Health Nutr. 2013, 16, 1637–1643. [Google Scholar] [CrossRef] [PubMed]
- Barbara, W.A. Introduction to Southeast Asia. Available online: http://asiasociety.org/education/introduction-southeast-asia (accessed on 25 March 2017).
- Birch, L.L. Learning to eat: Behavioral and psychological aspects. Nestle Nutr. Inst. Workshop Ser. 2016, 85, 125–134. [Google Scholar] [PubMed]
- Lindsay, A.C.; Sussner, K.M.; Kim, J.; Gortmaker, S. The role of parents in preventing childhood obesity. Future Child. 2016, 1, 169–186. [Google Scholar] [CrossRef]
- Sleddens, S.F.; Gerards, S.M.; Thijs, C.; De Vries, N.K.; Kremers, S.P. General parenting, childhood overweight and obesity-inducing behaviors: A review. Int. J. Pediatr. Obes. 2011, 6 (Suppl. 3), e12–e27. [Google Scholar] [CrossRef] [PubMed]
- Vollmer, R.L.; Mobley, A.R. Parenting styles, feeding styles, and their influence on child obesogenic behaviors and body weight: A review. Appetite 2013, 71, 232–241. [Google Scholar] [CrossRef] [PubMed]
- Anzman, S.L.; Rollins, B.Y.; Birch, L.L. Parental influence on children’s early eating environments and obesity risk: Implications for prevention. Int. J. Obes. 2010, 34, 1116–1124. [Google Scholar] [CrossRef] [PubMed]
- Shloim, N.; Edelson, L.R.; Martin, N.; Hetherington, M.M. Parenting styles, feeding styles, feeding practices and weight status in 4–12 year-old children: A systematic review of the literature. Front. Psychol. 2015, 6, 1849. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Huffman, S.L. Nutrition in pregnancy and early childhood and associations with obesity in developing countries. Matern. Child Nutr. 2013, 9 (Suppl. 1), 105–119. [Google Scholar] [CrossRef] [PubMed]
- Weng, S.F.; Redsell, S.A.; Swift, J.A.; Yang, M.; Glazebrook, C.P. Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch. Dis. Child. 2012, 97, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Hancox, R.J.; Stewart, A.W.; Braithwaite, I.; Beasley, R.; Murphy, R.; Mitchell, E.A. ISAAC Phase Three Study Group. Association between breastfeeding and body mass index at age 6–7 years in an international survey. Pediatr. Obes. 2015, 10, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Van der Willik, E.M.; Vrijkotte, T.G.; Altenburg, T.M.; Gademan, M.G.; Kist-van Holthe, J. Exclusively breastfed overweight infants are at the same risk of childhood overweight as formula fed overweight infants. Arch. Dis. Child. 2015, 100, 932–937. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.; Story, M. A review of snacking patterns among children and adolescents: What are the implications of snacking for weight status? Child. Obes. 2013, 9, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Taillie, L.S.; Wang, D.; Popkin, B.M. Snacking is longitudinally associated with declines in body mass index z scores for overweight children, but increases for underweight children. J. Nutr. 2016, 146, 1268–1275. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Matheson, B.E.; Rhee, K.E.; Peterson, C.B.; Rydell, S.; Boutelle, K.N. Parental control and overconsumption of snack foods in overweight and obese children. Appetite 2016, 100, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Webber, L.; Hill, C.; Saxton, J.; Van Jaarsveld, C.H.; Wardle, J. Eating behaviour and weight in children. Int. J. Obes. 2009, 33, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Svensson, V.; Lundborg, L.; Cao, Y.; Nowicka, P.; Marcus, C.; Sobko, T. Obesity related eating behaviour patterns in Swedish preschool children and association with age, gender, relative weight and parental weight-factorial validation of the Children’s Eating Behaviour Questionnaire. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 134. [Google Scholar] [CrossRef] [PubMed]
- Daniels, L.A.; Mallan, K.M.; Battistutta, D.; Nicholson, J.M.; Meedeniya, J.E.; Bayer, J.K.; Magarey, A. Child eating behavior outcomes of an early feeding intervention to reduce risk indicators for child obesity: The NOURISH RCT. Obesity (Silver Spring) 2014, 22, E104–E111. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- Dieu, H.T.T.; Dibley, M.J.; Sibbritt, D.; Hanh, T.T.M. Prevalence of overweight and obesity in preschool children and associated socio-demographic factors in Ho Chi Minh City, Vietnam. Int. J. Pediatr. Obes. 2007, 2, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Huynh, D.T.; Dibley, M.J.; Sibbritt, D.; Tran, H.T.; Le, Q.T. Influence of contextual and individual level risk factors on adiposity in a preschool child cohort in Ho Chi Minh City, Vietnam. Int. J. Pediatr. Obes 2011, 6, e487–e500. [Google Scholar] [CrossRef] [PubMed]
- Thongbai, W.; Fongkaew, W.; Kennedy, C.M.; Aree, P.; Patumanond, J. Risk factors contributing to overweight among preschool children. Pac. Rim Int. J. Nurs. Res. 2011, 1, 13–27. [Google Scholar]
- Do, L.M.; Eriksson, B.; Tran, T.K.; Petzold, M.; Ascher, H. Feeding of preschool children in Vietnam: A study of parents’ practices and associated factors. BMC Nutr. 2015, 1, 16. [Google Scholar] [CrossRef]
- Do, L.M.; Tran, T.K.; Eriksson, B.; Petzold, M.; Nguyen, C.T.; Ascher, H. Preschool overweight and obesity in urban and rural Vietnam: Differences in prevalence and associated factors. Glob. Health Action 2015, 8, 28615. [Google Scholar] [CrossRef] [PubMed]
- Aziz, M.F.A.; Devi, N.M. Nutritional status and eating practices among children aged 4–6 years old in selected urban and rural kindergarten in Selangor, Malaysia. Asian J. Clin. Nutr. 2012, 4, 116–131. [Google Scholar] [CrossRef]
- Sabanayagam, C.; Shankar, A.; Chong, Y.S.; Wong, T.Y.; Saw, S.M. Breast-feeding and overweight in Singapore school children. Pediatr. Int. 2009, 51, 650–656. [Google Scholar] [CrossRef] [PubMed]
- Yamborisut, U.; Kosulwat, V.; Chittchang, U.; Wimonpeerapattana, W.; Suthutvoravut, U. Factors associated with dual form of malnutrition in school children in Nakhon Pathom and Bangkok. J. Med. Assoc. Thail. 2006, 89, 1012–1023. [Google Scholar]
- Zaini, M.Z.A.; Lim, C.T.; Low, W.Y.; Harun, F. Factors affecting nutritional status of Malaysian primary school children. Asia Pac. J. Public Health 2005, 17, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Serene, T.E.; Shamarina, S.; Mohd, N.M. Familial and socio-environmental predictors of overweight and obesity among primary school children in Selangor and Kuala Lumpur. Malays. J. Nutr. 2011, 17, 151–162. [Google Scholar] [PubMed]
- Wan, A.M.; Norazawati, A.K.; Lee, Y.Y. Overweight and obesity among Malay primary school children in Kota Bharu, Kelantan: Parental beliefs, attitudes and child feeding practices. Malays. J. Nutr. 2012, 18, 27–36. [Google Scholar] [PubMed]
- Tay, C.W.; Chin, Y.S.; Lee, S.T.; Khouw, I.; Poh, B.K. Association of eating behavior with nutritional status and body composition in primary school-aged children. Asia Pac. J. Public Health 2016, 28, 47S–58S. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Suarez, C.B.; Lee-Pineda, K.; Caralipio, N.D.; Grimmer-Somers, K.; Sibug, E.O.; Velasco, Z.F. Is what Filipino children eat between meals associated with body mass index? Asia Pac. J. Public Health 2015, 27, NP650–NP661. [Google Scholar] [CrossRef] [PubMed]
- Soo, K.L.; Wan, A.M.; Abdul, M.H.; Lee, Y.Y. Dietary practices among overweight and obese Chinese children in Kota Bharu, Kelantan. Malays. J. Nutr. 2011, 17, 87–95. [Google Scholar] [PubMed]
- Vereecken, C.A.; Keukelier, E.; Maes, L. Influence of mother’s educational level on food parenting practices and food habits of young children. Appetite 2004, 43, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Guthrie, C.A.; Sanderson, S.; Rapoport, L. Development of the Children’s Eating Behaviour Questionnaire. J. Child. Psychol. Psychiatry 2002, 42, 963–970. [Google Scholar] [CrossRef]
- Birch, L.L.; Fisher, J.O.; Markey, C.N.; GrimmThomas, K.; Sawyer, R.; Johnson, S.L. Confirmatory factor analysis of the Child Feeding Questionnaire: A measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite 2001, 36, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Horta, B.L.; Loret de Mola, C.; Victora, C.G. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 30–37. [Google Scholar] [CrossRef] [PubMed]
- De la Hunty, A.; Gibson, S.; Ashwell, M. Does regular breakfast cereal consumption help children and adolescents stay slimmer? A systematic review and meta-analysis. Obes. Facts 2013, 6, 70–85. [Google Scholar] [CrossRef] [PubMed]
- Karatzi, K.; Moschonis, G.; Choupi, E.; Manios, Y.; Healthy Growth Study Group. Late-night overeating is associated with smaller breakfast, breakfast skipping, and obesity in children: The Healthy Growth Study. Nutrition 2017, 33, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Coppinger, T.; Jeanes, Y.M.; Hardwick, J.; Reeves, S. Body mass, frequency of eating and breakfast consumption in 9–13-year-olds. J. Hum. Nutr. Diet. 2012, 25, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, R.F.; Paxton, S.J.; Massey, R.; Campbell, K.J.; Wertheim, E.H.; Skouteris, H.; Gibbons, K. Maternal feeding practices predict weight gain and obesogenic eating behaviors in young children: A prospective study. Int. J. Behav. Nutr. Phys. Act. 2013, 18, 10. [Google Scholar] [CrossRef] [PubMed]
- Boots, S.B.; Tiggemann, M.; Corsini, N.; Mattiske, J. Managing young children’s snack food intake. The role of parenting style and feeding strategies. Appetite 2015, 92, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.I.; Miller, J.M.; Watts, A.W.; Story, M.T.; Neumark-Sztainer, D.R. Adolescent Snacking Behaviors Are Associated with Dietary Intake and Weight Status. J. Nutr. 2016, 146, 1348–1355. [Google Scholar] [CrossRef] [PubMed]
- Zakrzewski, J.K.; Gillison, F.B.; Cumming, S.; Church, T.S.; Katzmarzyk, P.T.; Broyles, S.T.; Standage, M. Associations between breakfast frequency and adiposity indicators in children from 12 countries. Int. J. Obes. 2015, 5, S80–S88. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes. Rev. 2013, 14, 606–619. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Broyles, S.T.; Champagne, C.M.; Chaput, J.P.; Fogelholm, M.; Hu, G.; Kuriyan, R.; Kurpad, A.; Lambert, E.V.; Maia, J.; et al. Relationship between soft drink consumption and obesity in 9–11 years old children in a multi-national study. Nutrients 2016, 30, 770. [Google Scholar] [CrossRef] [PubMed]
- Tschann, J.M.; Martinez, S.M.; Penilla, C.; Gregorich, S.E.; Pasch, L.A.; de Groat, C.L.; Flores, E.; Deardorff, J.; Greenspan, L.C.; Butte, N.F.; et al. Parental feeding practices and child weight status in Mexican American families: A longitudinal analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 66. [Google Scholar] [CrossRef] [PubMed]
- Gubbels, J.S.; Kremers, S.P.; Stafleu, A.; de Vries, S.I.; Goldbohm, R.A.; Dagnelie, P.C.; Thijs, C. Association between parenting practices and children’s dietary intake, activity behavior and development of body mass index: The KOALA Birth Cohort Study. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 18. [Google Scholar] [CrossRef] [PubMed]
| Studies | Items | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| #1 | #2 | #3 | #4 | #5 | #6 | #7 | #8 | #9 | #10 | Total | |
| Dieu et al. [25] | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Huynh et al. [26] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 8 |
| Thongbai et al. [27] | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 7 |
| Do et al. [28] | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 8 |
| Do et al. [29] | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 8 |
| Aziz et al. [30] | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 7 |
| Sabanayagam et al. [31] | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 7 |
| Yamborisut et al. [32] | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 6 |
| Zaini et al. [33] | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 6 |
| Serene et al. [34] | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 8 |
| Wan et al. [35] | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| Tay et al. [36] | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| Gonzalez-Suarez et al. [37] | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 7 |
| Soo et al. [38] | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Characteristics | No. of Studies |
|---|---|
| Total Number of Studies Selected | 14 |
| Publication Dates | |
| 2000–2005 | 1 |
| 2006–2011 | 7 |
| 2012–2016 | 6 |
| Study Design | |
| Cohort/longitudinal | 2 |
| Case-Control | 1 |
| Cross-sectional | 11 |
| Age Group | |
| Preschool-age (2–5 years) | 6 |
| School-age (6–12 years) | 8 |
| Southeast Asian Countries Represented | |
| Malaysia | 6 |
| Thailand | 2 |
| Singapore | 1 |
| Vietnam | 4 |
| The Philippines | 1 |
| Assessment of Parental Feeding Practices and Eating Behaviors Used | |
| Children’s Eating Behavior Questionnaire (CEBQ) | 2 |
| Child Feeding Questionnaire (CFQ) | 3 |
| Other (i.e., Food Frequency Questionnaire, food record, 24-h recall) | 9 |
| Classification of Child Overweight and Obesity Used | |
| International Obesity Task Force definition | 4 |
| World Health Organization (WHO) standard | 7 |
| National standard (Thailand) | 2 |
| Asian population standard | 1 |
| Author (Year) Country | Sample’s Characteristics and Study Design | Study Aim(s) | Measures of Feeding Practices and Eating Behaviors | Measures of Overweight and Obesity | Main Findings |
|---|---|---|---|---|---|
| Preschool-Age Children | |||||
| Dieu et al. (2007); Vietnam [25] | n = 670 preschool-aged children (4–5 years) in the kindergarten system: 49.6% boys, 50.4% girls. Children’s mean age = 56.2 months Cross-sectional | To assess the magnitude of overweight and obesity, and identify associated socio-demographic factors in a population of preschool-aged children in the kindergarten system of Vietnam’s largest city. | Breast-feeding was defined as being breastfed at any time. Breastfeeding duration was measured in months using an interviewer-administered, pre-coded questionnaire. | Height and weight were measured using standard methods and used to calculate child’s body mass index (BMI) using age- and sex-specific BMI cutoff points proposed by International Obesity Task Force (IOTF) | The odds of being obese significantly decreased by 5% for each additional month of breastfeeding. However, the association between breastfeeding duration was not significant after controlling for confounding factors. |
| Huynh et al. (2011); Vietnam [26] | n = 526 children aged 4–5 years in urban preschools 49% boys and 51% girls. Longitudinal | To identify risk factors associated with obesity at the community and family environment levels, and to identify individual parental and child characteristics associated with changes in adiposity indicators over a one-year period. | Interviewer-administered food frequency questionnaire (FFQ). | Height and weight were measured using standard methods and used to calculate child’s BMI using cutoff points for overweight in Asian populations (of >23 kg/m2) | Breast-feeding was associated with reduced risk of child obesity. The protective effect of breast-feeding appeared to be more obvious in boys than in girls (reduced BMI in boys by 0.05 units). |
| Thongbai et al. (2011); Thailand [27] | n = 615 primary caregivers of 102 overweight children (cases) and 513 normal-weight children (controls) age 3 to 5 years old. Case-control | To investigate family environmental factor as determinants of overweight among preschool children. | The Food Parenting Practices [39] were used to measure the primary caregivers’ food practices and frequency of being (a) permissive, (b) authoritarian, and (c) authoritative. The Children’s Eating Behavior Questionnaire (CEBQ) [40] to measure—food responsiveness, enjoyment of food, emotional overeating, desire to drink, satiety responsiveness, slowness in eating, emotional under-eating, and food fussiness. | Height and weight were measured using the standard methods. Child nutritional status was classified by using a Ministry of Public Health growth reference for two- to seven-year-old Thais. | Three maternal feeding practices were associated with child overweight (low pressure, low encouragement through material reward, and low negotiation) without adjusting for confounding factors. Low maternal pressure was associated with child overweight adjusting for confounding factors. |
| Do et al. (2015); Vietnam [28] | n = 2677 children (rural 1313; urban 1364), aged 3–6 years. Cross-sectional | To describe the use of parental non-responsive feeding practices (i.e., restriction, pressure to eat, and monitoring of child food intake). To identify associations between the parental feeding practices and children’s diet and BMI. | The Child Feeding Questionnaire (CFQ) [41] was used to assess parental attitudes, beliefs and practices related to feeding children. Children’s diet question was used to assess children’s level of food consumption including (1) amount of food and (2) fatty food, sweets and snacks consumption. | Height and weight were measured using standard methods and used to calculate child’s BMI. | Child’s BMI and the mother’s perception of the child’s weight was negatively associated with pressure to eat and positively associated with monitoring. Restriction was positively associated with mother’s perception of the child’s weight. High consumption of fatty foods, sweets, and snacks was associated with high restriction and monitoring in rural areas and high restriction and pressure to eat but low monitoring in urban areas. The amount of food consumed was negatively associated with pressure to eat in rural areas, but positively associated with monitoring in urban areas. |
| Do et al. (2015); Vietnam [29] | n = 2677 children (rural 1313; urban 1364), aged 3–6 years. Cross-sectional | To estimate prevalence of overweight and obesity for preschool children in both urban and rural areas and to identify risk factors of overweight and obesity among children. | Structured questionnaires included amount of food, food consumption, fast eating, irregular snacks, outdoor physical activity, indoor physical activity, sedentary time, family economy, mother’s education, household size, watching food advertisements, and snack availability. These questionnaires were used to assess child eating habits and lifestyle by interviewing parents or caregivers. | Height and weight were measured using standard methods and used to calculate child’s BMI. Overweight and obesity were defined using World Health Organization (WHO) standards. | In urban areas, overweight or obesity in children were significantly associated with age, large amounts of food, fast eating, and indoor activity. In rural areas, overweight or obesity in children was significantly associated with age, frequent consumption of fatty, and mothers watching food advertisements on television (TV). |
| Aziz et al. (2012); Malaysia [30] | n = 142 children (urban 100; rural 42): aged 4–6 years, 45.8%; 52.8% boys and 47.2% girls. Cross-sectional | To compare and investigate the relationship between the nutritional status and eating practice. | Parental feeding practices questions were used to measure parental feeding practices. Children’s dietary habit questions and the three-day diet record were used to assess children’s diet intake. | Height and weight were measured using standard methods and used to calculate child’s BMI, which was used to determine weight status using the WHO and Centers for Disease Control and Prevention (CDC) 2000 growth chart as a reference. | There were significant differences in nutrient intake between children in rural and urban areas. Children’s BMI had a positive relationship with fast food intake (r = 0.274, p < 0.05) and eating out (r = 0.207, p < 0.05) |
| School-Age Children | |||||
| Sabanayagam et al. (2009); Singapore [31] | n = 797 school children aged 10–12; 49% girls and 51% boys. Longitudinal | To evaluate the association between breastfeeding and overweight and obesity. | Parents completed an interviewer- administered survey that assessed whether the participating child was ever breast-fed, duration of breastfeeding and type of breastfeeding. Breastfeeding was dichotomized (yes/no). Breastfeeding duration was categorized into two groups (≤3 months, >3 months). Type of breastfeeding was defined as exclusive (fed no food other than breast milk); mostly (breast milk and non-formula supplements such as water, sweetened water or juices); or partly (breast milk supplemented with formula milk or other complementary foods). | Height and weight were measured using standard methods and used to calculate child’s BMI using the IOTF cutoff points to determine weight status. | There were no significant associations between breastfeeding status (yes/no), duration of breastfeeding ≤3 months, >3 months) and type of breastfeeding and overweight and/or obesity for the cohort and by sex. |
| Yamborisut et al. (2006); Thailand [32] | n = 199 children aged 6–10. Mean age was 8.2 years. Cross-sectional | To examine the influence of family characteristics and maternal feeding practices on eating behaviors, food consumption, and nutritional status of children. | Used an FFQ and 24-h food recall to assess the food consumption patterns of the children for two days. | Height and weight were measured using standard methods and used to classify child’s nutritional status using weight-for-height Z score (WHZ). The Thai growth reference was used to classify weight status. | Maternal control over the consumption of high caloric food and large amounts of food consumed by the children was associated with childhood obesity. Compared to normal-weight children, a higher proportion of obese children were not breastfed. |
| Zaini et al. (2005); Malaysia [33] | n = 1405 students aged 9–10 years old. Mean age 9.68 years old. Cross-sectional | To examine factors affecting the nutritional status of the sample. | Questionnaire administered to students, with confirmation by mothers whenever possible. Dietary practices assessed included having breakfast, regularity of having the three main meals, types, and quantities of each food item consumed during each meal in a typical day, and the frequency of eating fast food. | Height and weight were measured using standard methods and used to calculate child’s BMI; the IOTF standard was used to classify weight status. | There was association between the proportion of students who were breastfed for more than six months and classified as overweight and obese and the proportion of students who were breastfed for less than six months and classified as overweight and obese (21.9% vs. 20.4%). Students who consumed fast food more 4+/week were more likely to be overweight/obese (24%) than those who consumed fast food less <4/week (20%). |
| Serene et al. (2011); Malaysia [34] | n = 1430 Children ages 9–12 years. Mean age for children was 10.3+/−0.8 years. Cross-sectional | To explore the association between familial and socio-environmental factors and childhood obesity. | The CFQ [41] was used to monitor parental feeding strategies and ideas (perceived parent weight, perceived child weight, perceived responsibility, concern about child’s weight, and restriction and pressure to eat). | Height and weight were measured using standard methods and used to calculate the child’s BMI, which was used to determine the weight status using the WHO growth reference for children aged 5–19 years of age. | Pressure to eat showed a reverse association with child’s risk of overweight and obesity. |
| Wan et al. (2012); Malaysia [35] | n = 175 children aged 7–8 years old. Mean age of children was 7.4+/−0.5 years. Cross-sectional | To examine the association between parental children feeding practices and child’s weight status. | Used the CFQ [41] to measure several practices including perceived weight status, food restriction and pressure to eat. | Height and weight were measured using standard methods and used to calculate child’s BMI using the BMI-for-age WHO Growth chart as standard reference. | Perception of child’s weight, perceived parental weight, and food restriction factors were positively associated with the child’s BMI, whereas pressure to eat was negatively associated with child’s BMI. |
| Tay et al. (2016); Malaysia [36] | n = 1782 children aged 7–12 years old; 48.6% boys and 51.4% girls. Cross-sectional | To determine the association between eating behaviors and BMI, BMI-for-age Z-score (BAZ), waist circumference (WC), and percentage body fat (%BF) as indicators of nutritional status and body composition the sample. | The CEBQ [40] to measure - food responsiveness, enjoyment of food, emotional overeating, desire to drink, satiety responsiveness, slowness in eating, emotional under-eating, and food fussiness. | Height and weight were measured using standard methods and used to calculate the child’s BMI using the WHO growth standards. WC was measured using standard methods. %BF was measured by bioelectrical impedance. | Food responsiveness was positively associated with body adiposity for both sexes. Desire to drink was positively associated with BMI and WC for girls. Satiety responsiveness was negatively associated with body adiposity in both sexes except for %BF of boys. Slowness in eating was negatively associated with WC in girls. Emotional under-eating was negatively associated with the body adiposity (BMI) of boys. |
| Gonzalez-Suarez et al. (2015); The Philippines [37] | n = 396 elementary school students aged 10–12 years old. Cross-sectional. | To assess the associations between snacking (e.g., time, frequency, amount, type of snacks) and risk of overweight and obesity. | Data about mid-morning, mid-afternoon (both at school during the week), and nighttime snacks were collected using an interviewer-administered 24-h food recall. | Height and weight were measured using standard methods and used to calculate the child’s BMI. The IOTF’s gender- and age-specific cutoff points were used to determine weight status. | The odds of being overweight were associated with high total snack servings of 2.12. The odds of being obese (both males and females) were associated with calories obtained from snacking. |
| Soo et al. (2011); Malaysia [38] | n = 278 urban Chinese primary school children aged 10–12; 51.8% boys and 48.2% girls. Cross-sectional | To assess the relationship between nutritional statuses and dietary habits among sample. | Dietary habits were assessed using a three-day food record. Children were asked to record the type of foods, quantity, and portion size of all food consumed. | Height and weight were measured using standard methods and used to calculate the child’s BMI, which was used to determine the weight status using the WHO BMI-for-age growth chart as a reference. | Children classified as obese skipped breakfast more frequently than those classified as having a normal weight group. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cristina Lindsay, A.; Sitthisongkram, S.; Greaney, M.L.; Wallington, S.F.; Ruengdej, P. Non-Responsive Feeding Practices, Unhealthy Eating Behaviors, and Risk of Child Overweight and Obesity in Southeast Asia: A Systematic Review. Int. J. Environ. Res. Public Health 2017, 14, 436. https://doi.org/10.3390/ijerph14040436
Cristina Lindsay A, Sitthisongkram S, Greaney ML, Wallington SF, Ruengdej P. Non-Responsive Feeding Practices, Unhealthy Eating Behaviors, and Risk of Child Overweight and Obesity in Southeast Asia: A Systematic Review. International Journal of Environmental Research and Public Health. 2017; 14(4):436. https://doi.org/10.3390/ijerph14040436
Chicago/Turabian StyleCristina Lindsay, Ana, Somporn Sitthisongkram, Mary L. Greaney, Sherrie F. Wallington, and Praewrapee Ruengdej. 2017. "Non-Responsive Feeding Practices, Unhealthy Eating Behaviors, and Risk of Child Overweight and Obesity in Southeast Asia: A Systematic Review" International Journal of Environmental Research and Public Health 14, no. 4: 436. https://doi.org/10.3390/ijerph14040436






