Job Strain and Casual Blood Pressure Distribution: Looking beyond the Adjusted Mean and Taking Gender, Age, and Use of Antihypertensives into Account. Results from ELSA-Brasil
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Variables
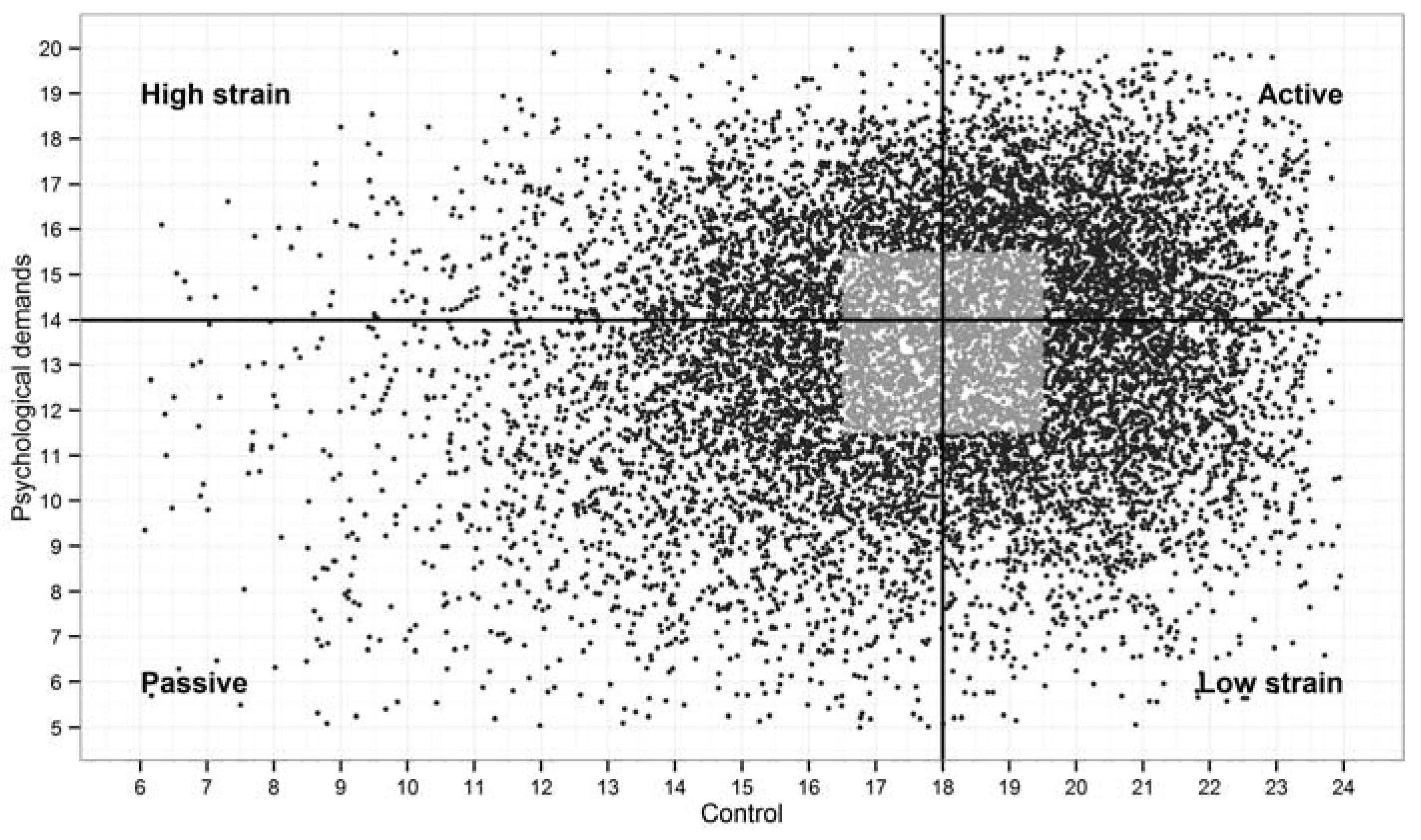
2.2.1. Job Strain
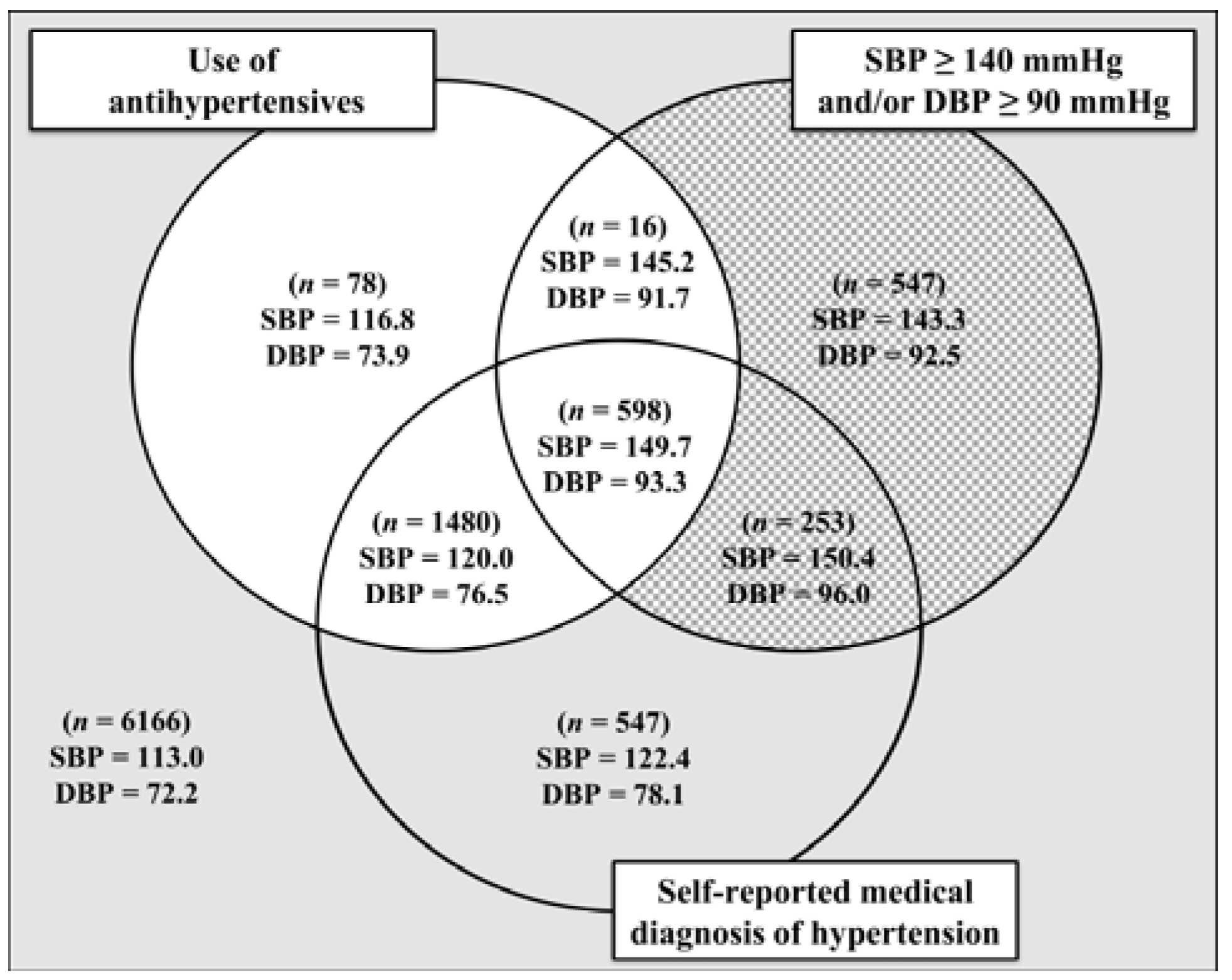
2.2.2. Casual Blood Pressure
2.2.3. Blood Pressure-Related Variables
2.2.4. Covariables
2.3. Statistical Analysis
3. Results
3.1. Job Strain
3.2. Casual Blood Pressure
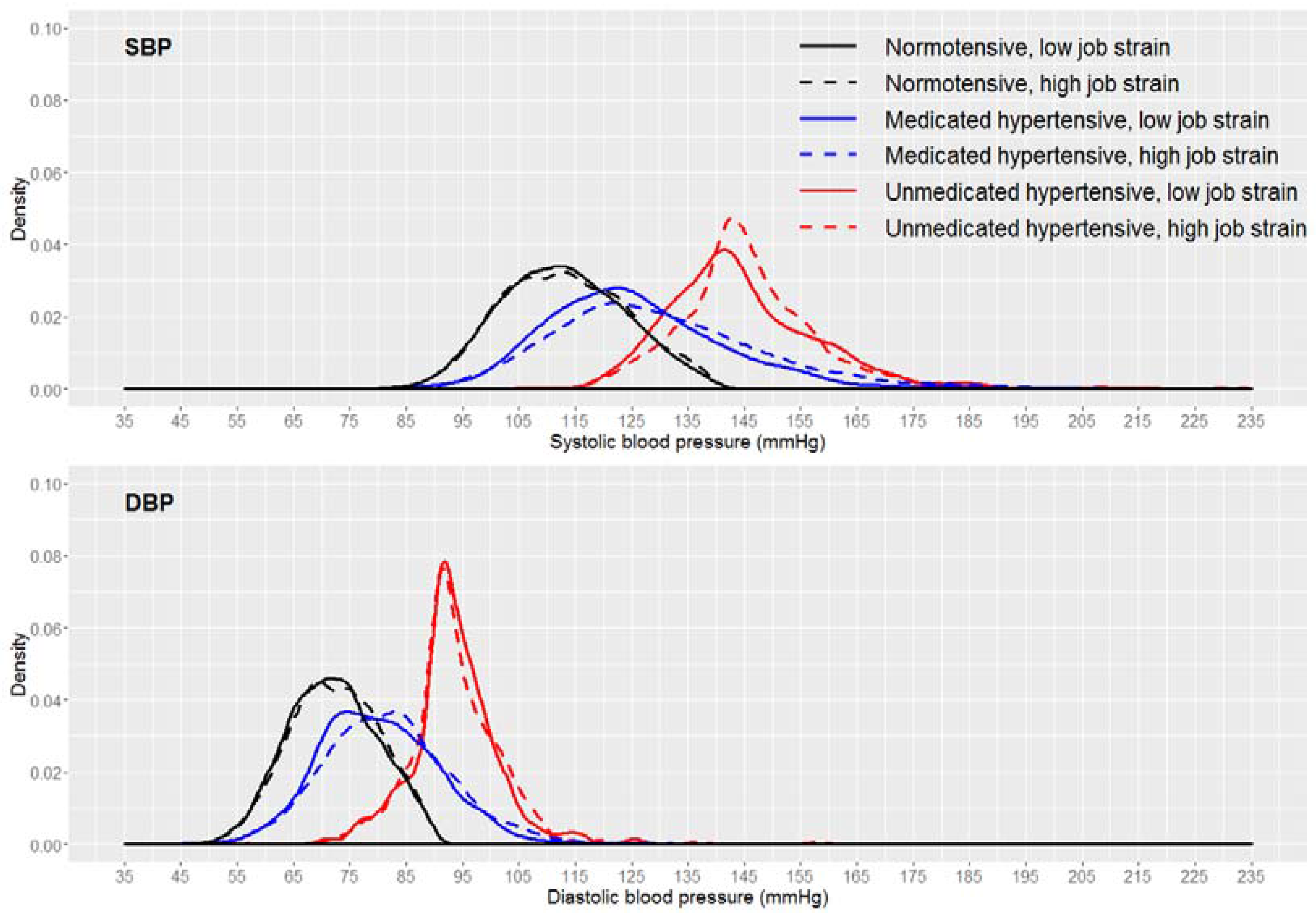
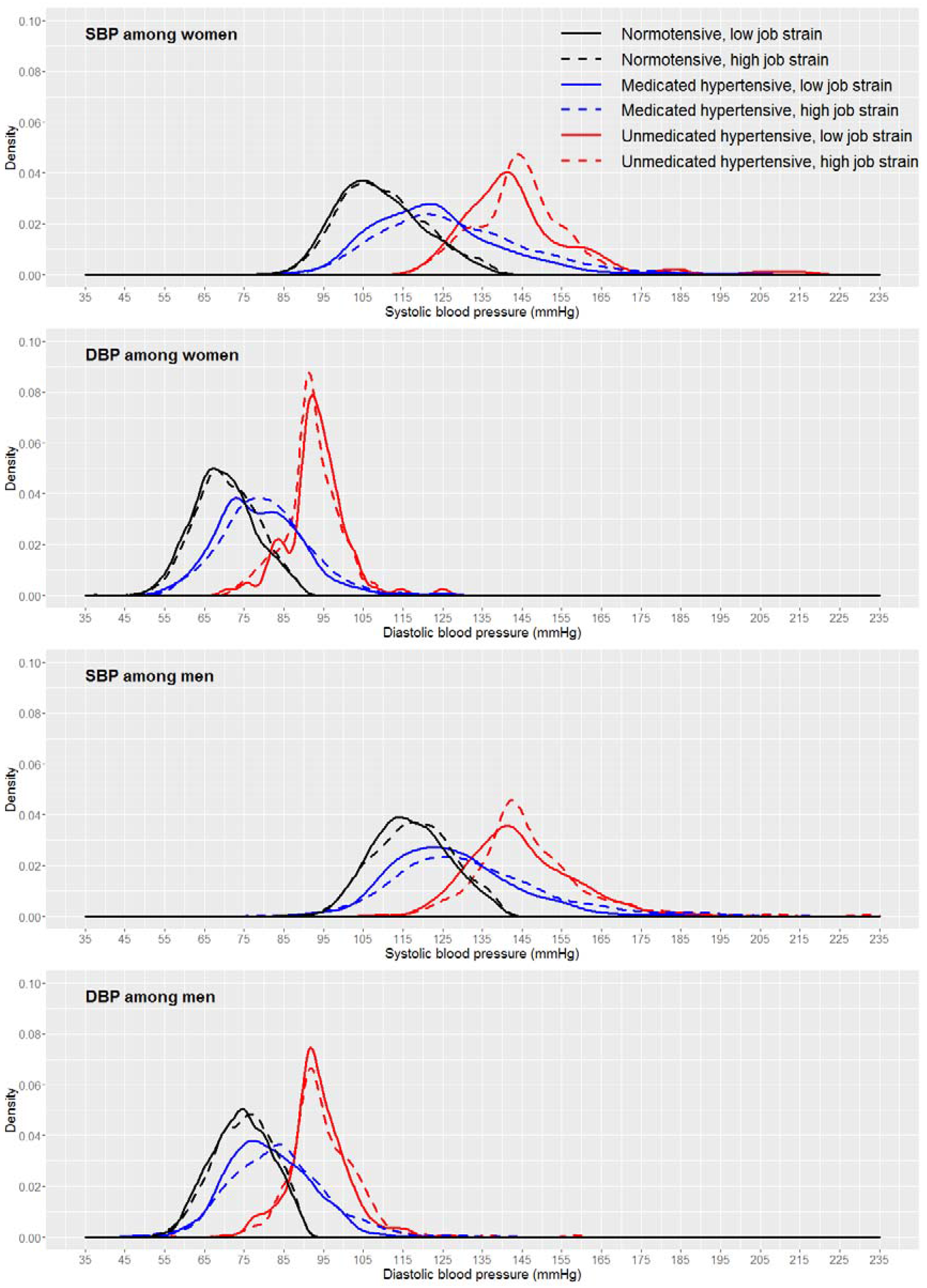
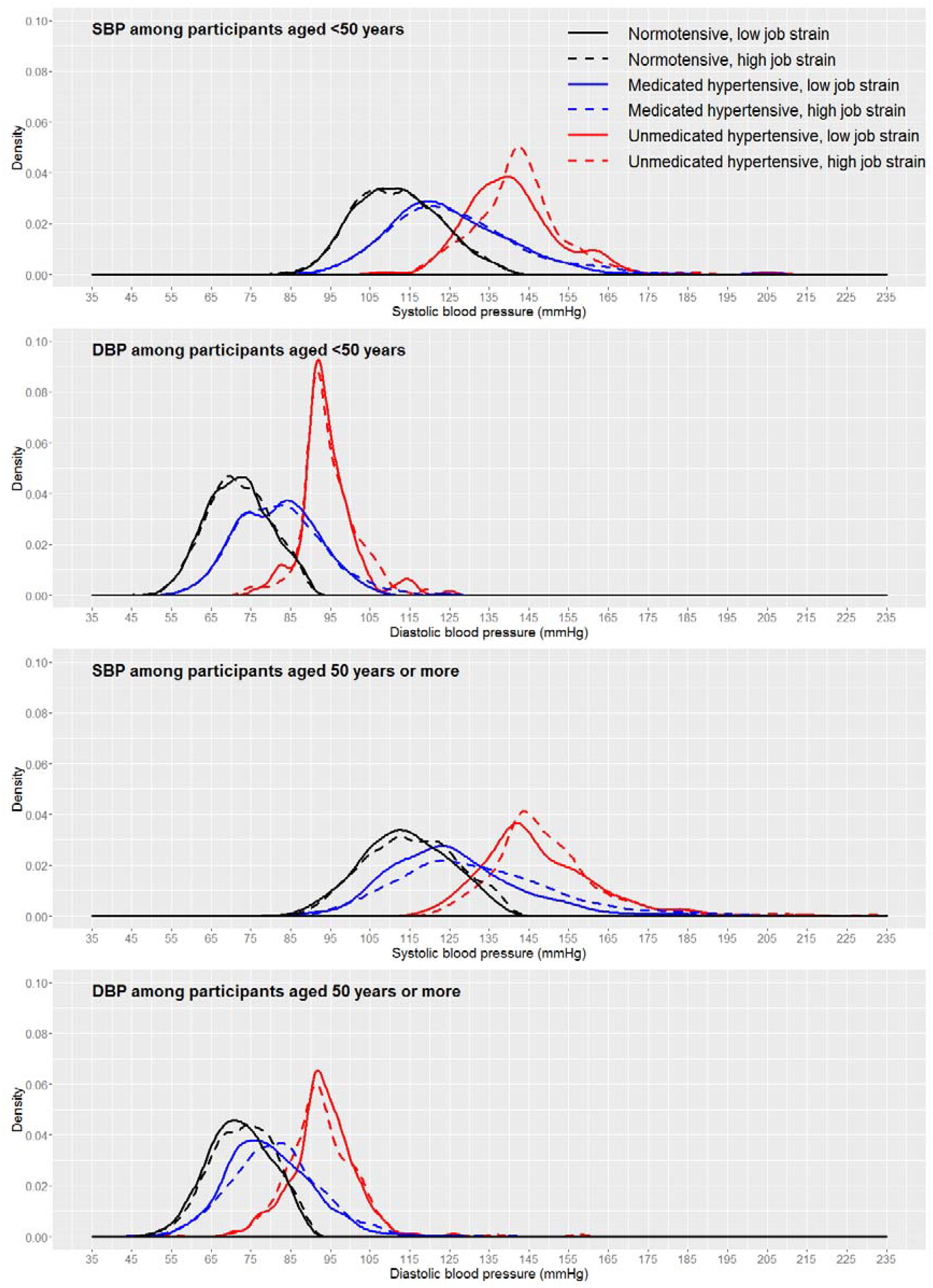
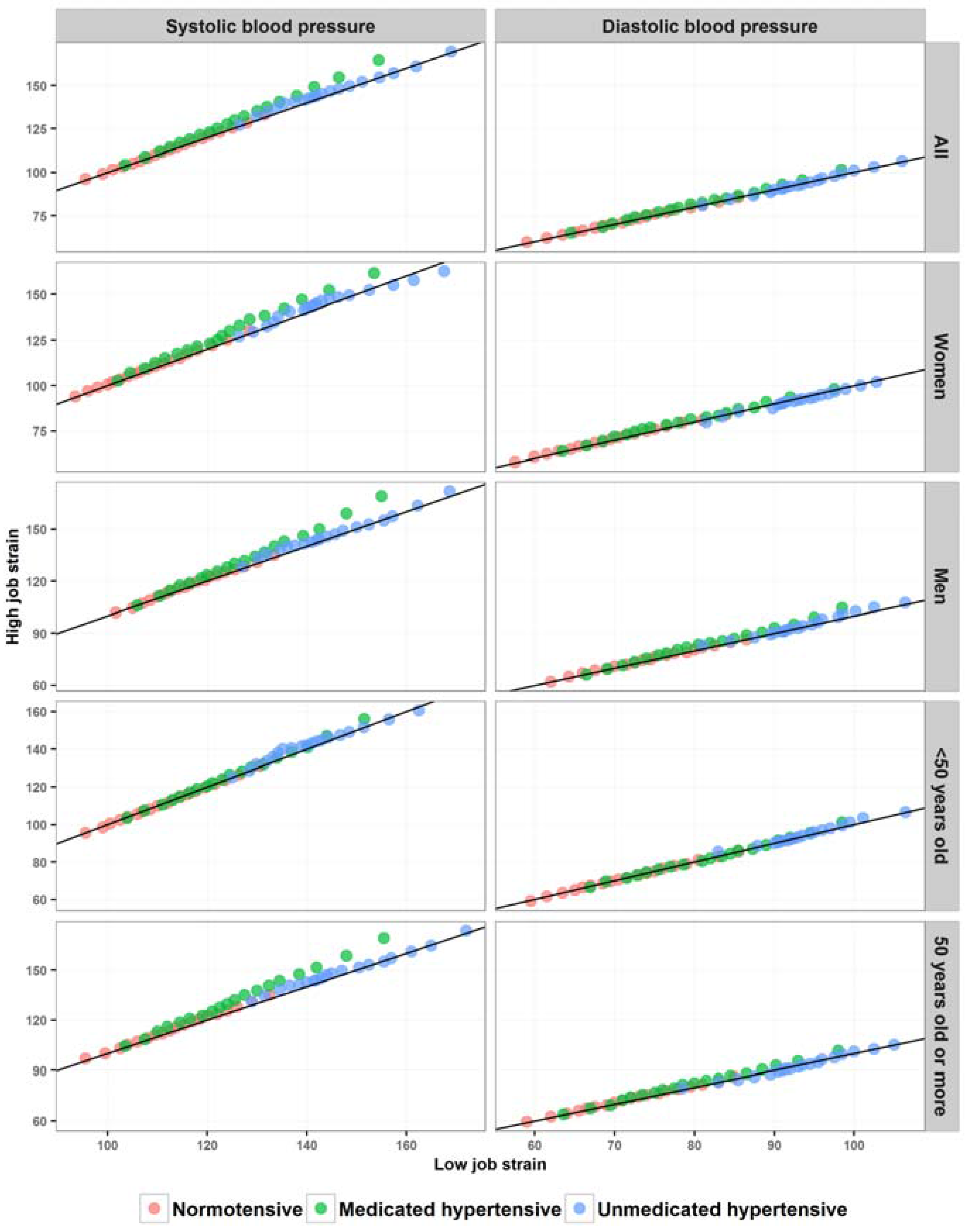
3.3. Relationship between Job Strain and Casual Blood Pressure Distribution
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Karasek, R.A. Job demands, job decision latitude, and mental strain: Implications for job redesign. Adm. Sci. Q. 1979, 24, 285–308. [Google Scholar] [CrossRef]
- Kivimäki, M.; Nyberg, S.T.; Batty, G.D.; Fransson, E.I.; Heikkila, K.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Casini, A.; et al. Job strain as a risk factor for coronary heart disease: A collaborative meta-analysis of individual participant data. Lancet 2012, 380, 1491–1497. [Google Scholar] [CrossRef]
- Torén, K.; Schiöler, L.; Giang, W.K.; Novak, M.; Söderberg, M.; Rosengren, A. A longitudinal general population-based study of job strain and risk for coronary heart disease and stroke in Swedish men. BMJ Open 2014, 4, e004355. [Google Scholar] [CrossRef] [PubMed]
- Babu, G.R.; Jotheeswaran, A.; Mahapatra, T.; Mahapatra, S.; Kumar, A.; Detels, R.; Pearce, N. Is hypertension associated with job strain? A meta-analysis of observational studies. Occup. Environ. Med. 2014, 71, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, I.B.; Shapiro, D.; Chicz-DeMet, A.; Guthrie, D. Ambulatory blood pressure, heart rate, and neuroendocrine responses in women nurses during work and off work days. Psychosom. Med. 1999, 61, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Cropley, M.; Griffith, J.; Kirschbaum, C. Job strain and anger expression predict early morning elevations in salivary cortisol. Psychosom. Med. 2000, 62, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Thomas, K.S.; Nelesen, R.A.; Ziegler, M.G.; Bardwell, W.A.; Dimsdale, J.E. Job strain, ethnicity, and sympathetic nervous system activity. Hypertension 2004, 44, 891–896. [Google Scholar] [CrossRef] [PubMed]
- Nomura, K.; Nakao, M.; Tsurugano, S.; Takeuchi, T.; Inoue, M.; Shinozaki, Y.; Yano, E. Job stress and healthy behavior among male Japanese office workers. Am. J. Ind. Med. 2010, 53, 1128–1134. [Google Scholar] [CrossRef] [PubMed]
- Heikkilä, K.; Nyberg, S.T.; Fransson, E.I.; Alfredsson, L.; De Bacquer, D.; Bjorner, J.B.; Bonenfant, S.; Borritz, M.; Burr, H.; Clays, E.; et al. Job strain and alcohol intake: A collaborative meta-analysis of individual-participant data from 140,000 men and women. PLoS ONE 2012, 7, e40101. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, S.T.; Fransson, E.I.; Heikkilä, K.; Alfredsson, L.; Casini, A.; Clays, E.; De Bacquer, D.; Dragano, N.; Erbel, R.; Ferrie, J.E.; et al. Job strain and cardiovascular disease risk factors: Meta-Analysis of individual-participant data from 47,000 men and women. PLoS ONE 2013, 8, e67323. [Google Scholar] [CrossRef] [PubMed]
- Gilbert-Ouimet, M.; Trudel, X.; Brisson, C.; Milot, A.; Vézina, M. Adverse effects of psychosocial work factors on blood pressure: Systematic review of studies on demand-control-support and effort-reward imbalance models. Scand. J. Work Environ. Health 2014, 40, 109–132. [Google Scholar] [CrossRef]
- Markovitz, J.H.; Matthews, K.A.; Whooley, M.; Lewis, C.E.; Greenlund, K.J. Increases in job strain are associated with incident hypertension in the CARDIA Study. Ann. Behav. Med. 2004, 28, 4–9. [Google Scholar] [CrossRef]
- Landsbergis, P.A.; Dobson, M.; Koutsouras, G.; Schnall, P. Job strain and ambulatory blood pressure: A meta-analysis and systematic review. Am. J. Public Health 2013, 103, e61–e71. [Google Scholar] [CrossRef] [PubMed]
- Fauvel, J.P.; M’Pio, I.; Quelin, P.; Rigaud, J.-P.; Laville, M.; Ducher, M. Neither perceived job stress nor individual cardiovascular reactivity predict high blood pressure. Hypertension 2003, 42, 1112–1116. [Google Scholar] [CrossRef] [PubMed]
- Kivimäki, M.; Head, J.; Ferrie, J.E.; Shipley, M.J.; Steptoe, A.; Vahtera, J.; Marmot, M.G. Hypertension is not the link between job strain and coronary heart disease in the Whitehall II study. Am. J. Hypertens. 2007, 20, 1146–1153. [Google Scholar]
- Chikani, V.; Reding, D.; Gunderson, P.; McCarty, C.A. Psychosocial work characteristics predict cardiovascular disease risk factors and health functioning in rural women: The Wisconsin Rural Women’s Health Study. J. Rural Health 2005, 21, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Fornari, C.; Ferrario, M.; Menni, C.; Sega, R.; Facchetti, R.; Cesana, G.C. Biological consequences of stress: Conflicting findings on the association between job strain and blood pressure. Ergonomics 2007, 50, 1717–1726. [Google Scholar] [CrossRef] [PubMed]
- Mezuk, B.; Kershaw, K.N.; Hudson, D.; Lim, K.A.; Ratliff, S. Job strain, workplace discrimination, and hypertension among older workers: The Health and Retirement Study. Race Soc. Probl. 2011, 3, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Netterstrom, B. Job strain and hypertension. Occup. Environ. Med. 2014, 71, 157–158. [Google Scholar] [CrossRef] [PubMed]
- Landsbergis, P.A.; Schnall, P.L.; Warren, K.; Pickering, T.G.; Schwartz, J.E. Association between ambulatory blood pressure and alternative formulations of job strain. Scand. J. Work Environ. Health 1994, 20, 349–363. [Google Scholar] [CrossRef] [PubMed]
- De Alves, M.G.M.; Hökerberg, Y.H.M.; Faerstein, E. Trends and diversity in the empirical use of Karasek’s demand-control model (job strain): A systematic review. Rev. Bras. Epidemiol. 2013, 16, 125–136. [Google Scholar]
- Lewington, S.; Clarke, R.; Qizilbash, N.; Peto, R.; Collins, R.; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002, 360, 1903–1913. [Google Scholar] [PubMed]
- Hu, B.; Liu, X.; Yin, S.; Fan, H.; Feng, F.; Yuan, J. Effects of psychological stress on hypertension in middle-aged Chinese: A cross-sectional study. PLoS ONE 2015, 10, e0129163. [Google Scholar] [CrossRef] [PubMed]
- Bakhshi, E.; McArdle, B.; Mohammad, K.; Seifi, B.; Biglarian, A. Let continuous outcome variables remain continuous. Comput. Math. Methods Med. 2012, 2012, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.G.; Royston, P. The cost of dichotomising continuous variables. BMJ 2006, 332, 1080. [Google Scholar] [CrossRef] [PubMed]
- Naggara, O.; Raymond, J.; Guilbert, F.; Roy, D.; Weill, A.; Altman, D.G. Analysis by categorizing or dichotomizing continuous variables is inadvisable: An example from the natural history of unruptured aneurysms. Am. J. Neuroradiol. 2011, 32, 437–440. [Google Scholar] [CrossRef] [PubMed]
- Dawson, N.V.; Weiss, R. Dichotomizing continuous variables in statistical analysis: A practice to avoid. Med. Decis. Mak. 2012, 32, 225–226. [Google Scholar] [CrossRef] [PubMed]
- Landsbergis, P.A.; Schnall, P.L.; Pickering, T.G.; Warren, K.; Schwartz, J.E. Lower socioeconomic status among men in relation to the association between job strain and blood pressure. Scand. J. Work Environ. Health 2003, 29, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Guimont, C.; Brisson, C.; Dagenais, G.R.; Milot, A.; Vézina, M.; Mâsse, B.; Moisan, J.; Laflamme, N.; Blanchette, C. Effects of job strain on blood pressure: A prospective study of male and female white-collar workers. Am. J. Public Health 2006, 96, 1436–1443. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, A.; Kayaba, K.; Tsutsumi, K.; Igarashi, M.; Jichi Medical School Cohort Study Group. Association between job strain and prevalence of hypertension: A cross sectional analysis in a Japanese working population with a wide range of occupations: The Jichi Medical School cohort study. Occup. Environ. Med. 2001, 58, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Aquino, E.M.L.; Barreto, S.M.; Bensenor, I.M.; Carvalho, M.S.; Chor, D.; Duncan, B.B.; Lotufo, P.A.; Mill, J.G.; Molina, M.D.C.; Mota, E.L.A.; et al. Brazilian Longitudinal Study of Adult Health (ELSA-Brasil): Objectives and design. Am. J. Epidemiol. 2012, 175, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Aquino, E.M.L.; Araujo, M.J.; da Conceição C Almeida, M.; Conceição, P.; de Andrade, C.R.; Cade, N.V.; Carvalho, M.S.; de Figueiredo, R.C.; de Jesus M da Fonseca, M.; Giatti, L.; et al. Participants recruitment in ELSA-Brasil (Brazilian Longitudinal Study for Adult Health). Rev. Saúde Pública 2013, 47, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.I.; Duncan, B.B.; Mill, J.G.; Lotufo, P.A.; Chor, D.; Barreto, S.M.; Aquino, E.M.L.; Passos, V.M.A.; Matos, S.M.A.; Molina, M.C.B.; et al. Cohort profile: Longitudinal Study of Adult Health (ELSA-Brasil). Int. J. Epidemiol. 2015, 44, 68–75. [Google Scholar] [CrossRef]
- De Mello Alves, M.G.; Chor, D.; Faerstein, E.; de S Lopes, C.; Werneck, G.L. Short version of the “job stress scale”: A Portuguese-language adaptation. Rev. Saúde Pública 2004, 38, 164–171. [Google Scholar]
- Theorell, T.; Perski, A.; Akerstedt, T.; Sigala, F.; Ahlberg-Hulten, G.; Svensson, J.; Eneroth, P. Changes in job strain in relation to changes in physiological state. A longitudinal study. Scand. J. Work Environ. Health 1988, 14, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Griep, R.H.; Rotenberg, L.; Vasconcellos, A.G.G.; Landsbergis, P.; Comaru, C.M.; Alves, M.G.M. The psychometric properties of demand-control and effort-reward imbalance scales among Brazilian nurses. Int. Arch. Occup. Environ. Health 2009, 82, 1163–1172. [Google Scholar] [CrossRef]
- Hökerberg, Y.H.M.; Aguiar, O.B.; Reichenheim, M.; Faerstein, E.; Valente, J.G.; de Fonseca, M.J.; Passos, S.R.L. Dimensional structure of the demand control support questionnaire: A Brazilian context. Int. Arch. Occup. Environ. Health 2010, 83, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Mill, J.G.; Pinto, K.; Griep, R.H.; Goulart, A.; Foppa, M.; Lotufo, P.A.; Maestri, M.K.; Ribeiro, A.L.; Andreao, R.V.; Dantas, E.M.; et al. Medical assessments and measurements in ELSA-Brasil. Rev. Saúde Pública 2013, 47, 54–62. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2015; ISBN 3-900051-07-0. [Google Scholar]
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis; Springer Science & Business Media: New York, NY, USA, 2009. [Google Scholar]
- Karasek, R.; Choi, B.; Ostergren, P.-O.; Ferrario, M.; De Smet, P. Testing two methods to create comparable scale scores between the Job Content Questionnaire (JCQ) and JCQ-like questionnaires in the European JACE Study. Int. J. Behav. Med. 2007, 14, 189–201. [Google Scholar] [CrossRef] [PubMed]
- Drew, J.H.; Glen, A.G.; Leemis, L.M. Computing the cumulative distribution function of the Kolmogorov-Smirnov statistic. Comput. Stat. Data Anal. 2000, 34, 1–15. [Google Scholar] [CrossRef]
- Beyerlein, A. Quantile regression-opportunities and challenges from a user’s perspective. Am. J. Epidemiol. 2014, 180, 330–331. [Google Scholar] [CrossRef] [PubMed]
- Ducher, M.; Cerutti, C.; Chatellier, G.; Fauvel, J.-P. Is high job strain associated with hypertension genesis? Am. J. Hypertens. 2006, 19, 694–700. [Google Scholar] [CrossRef] [PubMed]
- Everson, S.A.; Lynch, J.W.; Chesney, M.A.; Kaplan, G.A.; Goldberg, D.E.; Shade, S.B.; Cohen, R.D.; Salonen, R.; Salonen, J.T. Interaction of workplace demands and cardiovascular reactivity in progression of carotid atherosclerosis: Population based study. BMJ 1997, 314, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Fredrikson, M.; Matthews, K.A. Cardiovascular responses to behavioral stress and hypertension: A meta-analytic review. Ann. Behav. Med. 1990, 12, 30–39. [Google Scholar] [CrossRef]
- Porta, M.; Vineis, P.; Bolúmar, F. The current deconstruction of paradoxes: One sign of the ongoing methodological “revolution”. Eur. J. Epidemiol. 2015, 30, 1079–1087. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.E.; Pickering, T.G.; Landsbergis, P.A. Work-related stress and blood pressure: Current theoretical models and considerations from a behavioral medicine perspective. J. Occup. Health Psychol. 1996, 1, 287–310. [Google Scholar] [CrossRef] [PubMed]
- Theorell, T. Family history of hypertension—An individual trait interacting with spontaneously occurring job stressors. Scand. J. Work Environ. Health 1990, 16 (Suppl. 1), 74–79. [Google Scholar] [CrossRef] [PubMed]
- Westerlund, H.; Gustafsson, P.E.; Theorell, T.; Janlert, U.; Hammarström, A. Social adversity in adolescence increases the physiological vulnerability to job strain in adulthood: A prospective population-based study. PLoS ONE 2012, 7, e35967. [Google Scholar] [CrossRef] [PubMed]
- Chor, D.; Pinho Ribeiro, A.L.; Sá Carvalho, M.; Duncan, B.B.; Andrade Lotufo, P.; Araújo Nobre, A.; de Aquino, E.M.L.L.; Schmidt, M.I.; Griep, R.H.; Molina, M.D.C.B.; et al. Prevalence, awareness, treatment and influence of socioeconomic variables on control of high blood pressure: Results of the ELSA-Brasil study. PLoS ONE 2015, 10, e0127382. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D.M.; Evans, J.C.; Larson, M.G.; O’Donnell, C.J.; Roccella, E.J.; Levy, D. Differential control of systolic and diastolic blood pressure factors associated with lack of blood pressure control in the community. Hypertension 2000, 36, 594–599. [Google Scholar] [CrossRef] [PubMed]
- Muntner, P.; Gu, D.; Wu, X.; Duan, X.; Wenqi, G.; Whelton, P.K.; He, J. Factors associated with hypertension awareness, treatment, and control in a representative sample of the Chinese population. Hypertension 2004, 43, 578–585. [Google Scholar] [CrossRef] [PubMed]
- Courvoisier, D.S.; Perneger, T.V. Validation of alternative formulations of job strain. J. Occup. Health 2010, 52, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Karasek, R.; Baker, D.; Marxer, F.; Ahlbom, A.; Theorell, T. Job Decision latitude, job demands, and cardiovascular disease: A prospective study of Swedish men. Am. J. Public Health 1981, 71, 694. [Google Scholar] [CrossRef] [PubMed]
- Griep, R.H.; Rotenberg, L.; Landsbergis, P.; Vasconcellos-Silva, P.R. Combined use of job stress models and self-rated health in nursing. Rev. Saúde Pública 2011, 45, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Stansfeld, S.A.; Shipley, M.J.; Head, J.; Fuhrer, R. Repeated job strain and the risk of depression: Longitudinal analyses from the Whitehall II study. Am. J. Public Health 2012, 102, 2360–2366. [Google Scholar] [CrossRef] [PubMed]
- Sznajder, K.K.; Harlow, S.D.; Burgard, S.A.; Wang, Y.; Han, C.; Liu, J. Gynecologic pain related to occupational stress among female factory workers in Tianjin, China. Int. J. Occup. Environ. Health 2014, 20, 33–45. [Google Scholar] [CrossRef] [PubMed]
- Schnall, P.L.; Landsbergis, P.A.; Pickering, T.G.; Schwartz, J.E. Perceived job stress, job strain, and hypertension. Am. J. Public Health 1994, 84, 320–321. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.V.; Hall, E.M. Job strain, work place social support, and cardiovascular disease: A cross-sectional study of a random sample of the Swedish working population. Am. J. Public Health 1988, 78, 1336–1342. [Google Scholar] [CrossRef] [PubMed]
- Portela, L.; Rotenberg, L.; Almeida, A.; Landsbergis, P.; Griep, R. The influence of domestic overload on the association between job strain and ambulatory blood pressure among female nursing workers. Int. J. Environ. Res. Public. Health 2013, 10, 6397–6408. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T.; et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef] [PubMed]
- Strandberg, T.E.; Pitkala, K. What is the most important component of blood pressure: Systolic, diastolic or pulse pressure? Curr. Opin. Nephrol. Hypertens. 2003, 12, 293–297. [Google Scholar] [CrossRef] [PubMed]
- Ohlin, B.; Berglund, G.; Rosvall, M.; Nilsson, P. Job strain in men, but not in women, predicts a significant rise in blood pressure after 6.5 years of follow-up. J. Hypertens. 2007, 25, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Trudel, X.; Brisson, C.; Milot, A.; Masse, B.; Vézina, M. Psychosocial work environment and ambulatory blood pressure: Independent and combined effect of demand-control and effort-reward imbalance models. Occup. Environ. Med. 2013, 70, 815–822. [Google Scholar] [CrossRef] [PubMed]
- Gilbert-Ouimet, M.; Brisson, C.; Vézina, M.; Milot, A.; Blanchette, C. Repeated exposure to effort–reward imbalance, increased blood pressure, and hypertension incidence among white-collar workers. J. Psychosom. Res. 2012, 72, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Landsbergis, P.A.; Schnall, P.L.; Belkic, K.L.; Schwartz, J.E.; Baker, D.; Pickering, T.G. Work conditions and masked (hidden) hypertension–insights into the global epidemic of hypertension. Scand. J. Work Environ. Health 2008, 34, 41. [Google Scholar]
| Variables | n (%) or Mean (SD) |
|---|---|
| Age (years) | 49.3 (7.4) |
| Gender (%) | |
| Women | 4704 (52.1) |
| Men | 4319 (47.9) |
| Colour/race (%) | |
| White | 4589 (51.4) |
| Brown | 2624 (29.4) |
| Black | 1414 (15.9) |
| Yellow | 210 (2.4) |
| Indigenous | 84 (0.9) |
| Education (%) | |
| <Secondary complete | 1018 (11.3) |
| Secondary complete | 3163 (35.0) |
| Undergraduate complete | 1363 (15.1) |
| Postgraduate | 3479 (38.6) |
| Job strain scores (units) | |
| Job control | 17.8 (3.3) |
| Psychological job demands | 13.3 (3.1) |
| BP levels (mmHg) | |
| SBP | 119.5 (16.7) |
| DBP | 76.2 (11.0) |
| Use of antihypertensives (%) | |
| Yes | 2172 (24.1) |
| No | 6851 (75.9) |
| Group | K-S Statistic (D) 1 | Mean Difference 2 and 95% CI (mmHg) | ||||
|---|---|---|---|---|---|---|
| SBP | DBP | SBP | DBP | |||
| All (n = 9023) | ||||||
| Normotensive | 0.03 | 0.03 | 0.39 | (−0.17, 0.94) | 0.42 * | (0.02, 0.82) |
| Medicated hypertensive | 0.11 *** | 0.07 * | 4.30 *** | (2.81, 5.78) | 1.52 ** | (0.60, 2.45) |
| Unmedicated hypertensive | 0.12 ** | 0.04 | 1.47 | (−0.44, 3.38) | 0.08 | (−1.05, 1.21) |
| Women (n = 4704) | ||||||
| Normotensive | 0.04 | 0.06 ** | 1.01 ** | (0.28, 1.73) | 0.86 ** | (0.33, 1.39) |
| Medicated hypertensive | 0.14 *** | 0.11 ** | 4.44 *** | (2.29, 6.59) | 1.25 | (−0.07, 2.57) |
| Unmedicated hypertensive | 0.18 * | 0.12 | 0.12 | (−3.44, 3.68) | −1.36 | (−3.19, 0.47) |
| Men (n = 4319) | ||||||
| Normotensive | 0.06 * | 0.05 | 0.96 * | (0.22, 1.70) | 0.61 * | (0.04, 1.18) |
| Medicated hypertensive | 0.12 *** | 0.11 ** | 5.13 *** | (3.04, 7.21) | 2.44 *** | (1.11, 3.77) |
| Unmedicated hypertensive | 0.12 * | 0.08 | 2.39 * | (0.04, 4.73) | 1.05 | (−0.41, 2.50) |
| <50 years old (n = 4731) | ||||||
| Normotensive | 0.02 | 0.02 | −0.16 | (−0.85, 0.53) | 0.12 | (−0.39, 0.63) |
| Medicated hypertensive | 0.05 | 0.04 | 1.00 | (−1.39, 3.38) | 0.42 | (−1.17, 2.00) |
| Unmedicated hypertensive | 0.14 | 0.05 | 1.31 | (−1.20, 3.82) | 0.34 | (−1.17, 1.85) |
| 50 years old or more (n = 4292) | ||||||
| Normotensive | 0.07 ** | 0.07 * | 1.52 ** | (0.61, 2.43) | 0.95 ** | (0.31, 1.60) |
| Medicated hypertensive | 0.16 *** | 0.09 ** | 6.19 *** | (4.32, 8.06) | 1.86 ** | (0.72, 3.00) |
| Unmedicated hypertensive | 0.15 * | 0.08 | 2.24 | (−0.43, 4.91) | −0.27 | (−1.91, 1.37) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juvanhol, L.L.; Melo, E.C.P.; Carvalho, M.S.; Chor, D.; Mill, J.G.; Griep, R.H. Job Strain and Casual Blood Pressure Distribution: Looking beyond the Adjusted Mean and Taking Gender, Age, and Use of Antihypertensives into Account. Results from ELSA-Brasil. Int. J. Environ. Res. Public Health 2017, 14, 451. https://doi.org/10.3390/ijerph14040451
Juvanhol LL, Melo ECP, Carvalho MS, Chor D, Mill JG, Griep RH. Job Strain and Casual Blood Pressure Distribution: Looking beyond the Adjusted Mean and Taking Gender, Age, and Use of Antihypertensives into Account. Results from ELSA-Brasil. International Journal of Environmental Research and Public Health. 2017; 14(4):451. https://doi.org/10.3390/ijerph14040451
Chicago/Turabian StyleJuvanhol, Leidjaira Lopes, Enirtes Caetano Prates Melo, Marilia Sá Carvalho, Dóra Chor, José Geraldo Mill, and Rosane Härter Griep. 2017. "Job Strain and Casual Blood Pressure Distribution: Looking beyond the Adjusted Mean and Taking Gender, Age, and Use of Antihypertensives into Account. Results from ELSA-Brasil" International Journal of Environmental Research and Public Health 14, no. 4: 451. https://doi.org/10.3390/ijerph14040451






