Understanding Ebola Virus Transmission
Abstract
:1. Introduction
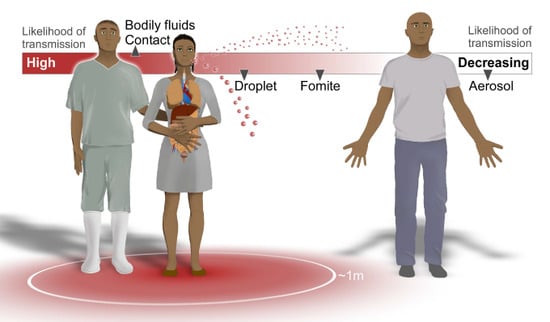
| Mode of transmission | Consensus likelihood of occurring | Known | Unknown |
|---|---|---|---|
| Airborne/Aerosol (small droplet/droplet nuclei) | Unlikely from epidemiology of disease | EBOV can be aerosolized mechanically and cause lethal disease in non-human primates at low concentrations [2,3] | Ability of the virus to become airborne through respiratory tract in humans and animals |
| Outbreaks contained without airborne precautions in the affected population [4] | Airborne stability of EBOV in tropical climates | ||
| EBOV detected after 90 min in experimental small aerosols [5] | Whether AGPs produce EBOV aerosols that cause transmission | ||
| Fomite | Less likely from environmental sampling | Virus found in dried blood [6] | EBOV stability in tropical climates and on surfaces |
| Persists on glass and in the dark for 5.9 days [7] | |||
| Droplet (large droplet) | Likely from epidemiology and experiments | EBOV found in stool, semen, saliva, breast milk [6] | Whether infectious fluids are formed into droplets by humans |
| Accidental infections in non-human primates, possibly from power washing [8,9] | |||
| Range of droplets containing EBOV | |||
| EBOV infections without direct contact [10] | |||
| Bodily fluids contact | Very likely from epidemiology and experimental data | Sharing needles and handling the deceased or sick are high risk factors [11] | How much virus is shed in different fluids |

2. Potential Routes of EBOV Transmission
2.1. Airborne/Aerosol
2.2. Droplet
2.3. Fomites and Environmental Stability
2.4. Contact with Bodily Fluids
3. Why Experiments Are Necessary
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Outbreaks Chronology: Ebola Virus Disease. Available online: http://www.cdc.gov/vhf/ebola/outbreaks/history/chronology.html (accessed on 21 November 2014).
- Reed, D.S.; Lackemeyer, M.G.; Garza, N.L.; Sullivan, L.J.; Nichols, D.K. Aerosol exposure to Zaire ebolavirus in three nonhuman primate species: Differences in disease course and clinical pathology. Microbes Infect. 2011, 13, 930–936. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.; Jaax, N.; White, J.; Jahrling, P. Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus. Int. J Exp. Pathol. 1995, 76, 227. [Google Scholar] [PubMed]
- Borio, L.; Inglesby, T.; Peters, C.J.; Schmaljohn, A.L.; Hughes, J.; Jahrling, P.; Ksiazek, T.; Johnson, K.; Meyerhoff, A.; O’Toole, T.; et al. Hemorrhagic fever viruses as biological weapons: Medical and public health management. JAMA 2002, 287, 2391–2405. [Google Scholar] [CrossRef] [PubMed]
- Piercy, T.; Smither, S.; Steward, J.; Eastaugh, L.; Lever, M. The survival of filoviruses in liquids, on solid substrates and in a dynamic aerosol. J. Appl. Microbiol. 2010, 109, 1531–1539. [Google Scholar] [PubMed]
- Bausch, D.G.; Towner, J.S.; Dowell, S.F.; Kaducu, F.; Lukwiya, M.; Sanchez, A.; Nichol, S.T.; Ksiazek, T.G.; Rollin, P.E. Assessment of the risk of Ebola virus transmission from bodily fluids and fomites. J. Infect. Dis. 2007, 196 (Suppl. 2), S142–S147. [Google Scholar]
- Sagripanti, J.L.; Rom, A.M.; Holland, L.E. Persistence in darkness of virulent alphaviruses, Ebola virus, and Lassa virus deposited on solid surfaces. Arch. Virol. 2010, 155, 2035–2039. [Google Scholar] [CrossRef] [PubMed]
- Jaax, N.; Jahrling, P.; Geisbert, T.; Geisbert, J.; Steele, K.; McKee, K.; Nagley, D.; Johnson, E.; Jaax, G.; Peters, C. Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory. Lancet 1995, 346, 1669–1671. [Google Scholar] [CrossRef] [PubMed]
- Weingartl, H.M.; Embury-Hyatt, C.; Nfon, C.; Leung, A.; Smith, G.; Kobinger, G. Transmission of Ebola virus from pigs to non-human primates. Sci. Rep. 2012, 2, 811. [Google Scholar] [CrossRef] [PubMed]
- Roels, T.; Bloom, A.; Buffington, J.; Muhungu, G.; Mac Kenzie, W.; Khan, A.; Ndambi, R.; Noah, D.; Rolka, H.; Peters, C. Ebola hemorrhagic fever, Kikwit, Democratic Republic of the Congo, 1995: Risk factors for patients without a reported exposure. J. Infect. Dis. 1999, 179 (Suppl. 1), S92–S97. [Google Scholar] [CrossRef]
- Dowell, S.F.; Mukunu, R.; Ksiazek, T.G.; Khan, A.S.; Rollin, P.E.; Peters, C. Transmission of Ebola hemorrhagic fever: A study of risk factors in family members, Kikwit, Democratic Republic of the Congo, 1995. J. Infect. Dis. 1999, 179 (Suppl. 1), S87–S91. [Google Scholar] [CrossRef]
- Jaax, N.K.; Davis, K.; Geisbert, T.J.; Vogel, P.; Jaax, G.P.; Topper, M.; Jahrling, P.B. Lethal experimental infection of rhesus monkeys with Ebola-Zaire (Mayinga) virus by the oral and conjunctival route of exposure. Arch. Pathol. Lab. Med. 1996, 120, 140–155. [Google Scholar]
- Centers for Disease Control and Prevention. Transmission: Ebola Virus Disease. Available online: http://www.cdc.gov/vhf/ebola/transmission/ (accessed on 21 November 2014).
- Centers for Disease Control and Prevention. Review of Human-to-Human Transmission of Ebola Virus: Ebola (Ebola Virus Disease). Available online: http://www.cdc.gov/vhf/ebola/transmission/human-transmission.html (accessed on 21 November 2014).
- Tellier, R. Aerosol transmission of influenza A virus: A review of new studies. J. R. Soc. Interface 2009, 6 (Suppl. 6), S783–S790. [Google Scholar] [CrossRef]
- Tang, J.W.; Li, Y.; Eames, I.; Chan, P.K.; Ridgway, G.L. Factors involved in the aerosol transmission of infection and control of ventilation in healthcare premises. J. Hosp. Infect. 2006, 64, 100–114. [Google Scholar] [CrossRef] [PubMed]
- Martines, R.B.; Ng, D.L.; Greer, P.W.; Rollin, P.E.; Zaki, S.R. Tissue and cellular tropism, pathology and pathogenesis of Ebola and Marburg viruses. J. Pathol. 2015, 235, 153–174. [Google Scholar] [CrossRef] [PubMed]
- Alimonti, J.; Leung, A.; Jones, S.; Gren, J.; Qiu, X.; Fernando, L.; Balcewich, B.; Wong, G.; Stroher, U.; Grolla, A.; et al. Evaluation of transmission risks associated with in vivo replication of several high containment pathogens in a biosafety level 4 laboratory. Sci. Rep. 2014, 4, 5824. [Google Scholar] [CrossRef] [PubMed]
- Johnson, G.R.; Morawska, L.; Ristovski, Z.D.; Hargreaves, M.; Mengersen, K.; Chao, C.Y.H.; Wan, M.P.; Li, Y.; Xie, X.; Katoshevski, D.; et al. Modality of human expired aerosol size distributions. J. Aerosol. Sci. 2011, 42, 839–851. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Guidance on Personal Protective Equipment To Be Used by Healthcare Workers during Management of Patients with Ebola Virus Disease in U.S. Hospitals, Including Procedures for Putting On (Donning) and Removing (Doffing): Ebola (Ebola Virus Disease). Available online: http://www.cdc.gov/vhf/ebola/healthcare-us/ppe/guidance.html (accessed on 21 January 2015).
- Bosch, A. Human enteric viruses in the water environment: A minireview. Int. Microbiol. 2010, 1, 191–196. [Google Scholar]
- Sobsey, M.D.; Meschke, J.S. Virus Survival in the Environment with Special Attention to Survival in Sewage Droplets and Other Environmental Media of Fecal or Respiratory Origin; World Health Organization: Geneva, Switzerland, 2003; p. 70. [Google Scholar]
- Kawaoka, Y. How Ebola virus infects cells. N. Engl. J. Med. 2005, 352, 2645–2646. [Google Scholar] [CrossRef] [PubMed]
- Casson, L.W.; Ritter, M.O.; Cossentino, L.M.; Gupta, P. Survival and recovery of seeded HIV in water and wastewater. Water Environ. Res. 1997, 69, 174–179. [Google Scholar] [CrossRef]
- WHO/International Study Team. Ebola haemorrhagic fever in Zaire, 1976. Bull. World Health Organ. 1978, 56, 271–293. [Google Scholar]
- Tarantola, A.; Abiteboul, D.; Rachline, A. Infection risks following accidental exposure to blood or body fluids in health care workers: A review of pathogens transmitted in published cases. Am. J. Infect. Control. 2006, 34, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Towner, J.S.; Rollin, P.E.; Bausch, D.G.; Sanchez, A.; Crary, S.M.; Vincent, M.; Lee, W.F.; Spiropoulou, C.F.; Ksiazek, T.G.; Lukwiya, M. Rapid diagnosis of Ebola hemorrhagic fever by reverse transcription-PCR in an outbreak setting and assessment of patient viral load as a predictor of outcome. J. Virol. 2004, 78, 4330–4341. [Google Scholar] [CrossRef] [PubMed]
- Leroy, E.; Baize, S.; Volchkov, V.; Fisher-Hoch, S.; Georges-Courbot, M.; Lansoud-Soukate, J.; Capron, M.; Debre, P.; McCormick, J.; Georges, A. Human asymptomatic Ebola infection and strong inflammatory response. Lancet 2000, 355, 2210–2215. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Judson, S.; Prescott, J.; Munster, V. Understanding Ebola Virus Transmission. Viruses 2015, 7, 511-521. https://doi.org/10.3390/v7020511
Judson S, Prescott J, Munster V. Understanding Ebola Virus Transmission. Viruses. 2015; 7(2):511-521. https://doi.org/10.3390/v7020511
Chicago/Turabian StyleJudson, Seth, Joseph Prescott, and Vincent Munster. 2015. "Understanding Ebola Virus Transmission" Viruses 7, no. 2: 511-521. https://doi.org/10.3390/v7020511