Vitamin D Intake and Status in 12-Month-Old Infants at 63–66° N
Abstract
:1. Introduction
2. Experimental Section
2.1. Subjects
2.2. Dietary Assessment

2.3. Blood Sampling and Biochemical Analyses
2.4. Statistical Analyses
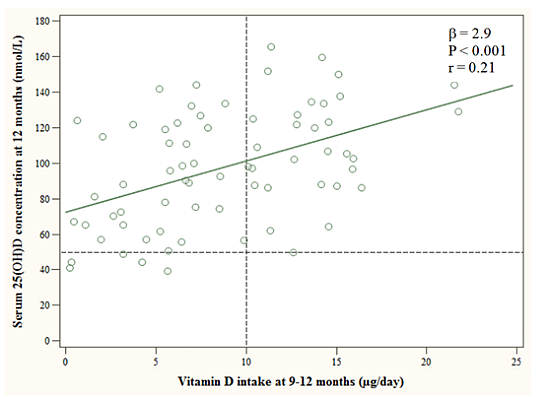
3. Results

| Variables | n (%) | Vitamin D Intake (μg/day) | 25(OH)D (nmol/L) |
|---|---|---|---|
| All | 76 (100) | 8.8 ± 5.2 | 98.1 ± 32.2 |
| Boys | 39 (51) | 8.6 ± 5.7 | 96.6 ± 34.3 |
| Girls | 37 (49) | 8.9 ± 4.6 | 99.7 ± 30.3 |
| Vitamin D sources at 9–12 months a | |||
| “No or irregular” | 20 (26) | 2.5 ± 1.9 | 76.8 ± 27.1 |
| “Fortified” | 17 (22) | 6.5 ± 2.2 | 100.0 ± 31.4 |
| “Supplement” | 14 (18) | 8.8 ± 2.7 | 104.6 ± 37.0 |
| “Combined” | 25 (33) | 14.3 ± 3.0 | 110.3 ± 26.6 |
| Partially breastfed at 12 months | |||
| No | 62 (82) | 8.7 ± 5.0 | 97.7 ± 32.7 |
| Yes | 14 (18) | 9.1 ± 6.0 | 101.9 ± 31.5 |
| Season of blood sample collection | |||
| Winter/Spring | 33 (43) | 8.1 ± 4.9 | 94.4 ± 31.6 |
| Summer/Autumn | 43 (57) | 9.2 ± 5.4 | 101.0 ± 32.8 |
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Turner, A.G.; Anderson, P.H.; Morris, H.A. Vitamin D and bone health. Scand. J. Clin. Lab. Investig. 2012, 243, 65–72. [Google Scholar]
- Moreno, L.A.; Valtuena, J.; Perez-Lopez, F.; Gonzalez-Gross, M. Health effects related to low vitamin D concentrations: Beyond bone metabolism. Ann. Nutr. Metab. 2011, 59, 22–27. [Google Scholar] [CrossRef]
- Lamberg-Allardt, C.; Brustad, M.; Meyer, H.E.; Steingrimsdottir, L. Vitamin D—A systematic literature review for the 5th edition of the Nordic Nutrition Recommendations. Food Nutr. Res. 2013, 57. [Google Scholar] [CrossRef] [Green Version]
- Engelsen, O.; Brustad, M.; Aksnes, L.; Lund, E. Daily duration of vitamin D synthesis in human skin with relation to latitude, total ozone, altitude, ground cover, aerosols and cloud thickness. Photochem. Photobiol. 2005, 81, 1287–1290. [Google Scholar] [CrossRef]
- Thiele, D.K.; Senti, J.L.; Anderson, C.M. Maternal vitamin D supplementation to meet the needs of the breastfed infant: A systematic review. J. Hum. Lact. 2013, 29, 163–170. [Google Scholar] [CrossRef]
- EFSA Panel on Dietetic Products Nutrition and Allergies (NDA). Scientific opinion on the tolerable upper intake level of vitamin D. EFSA J. 2012, 10. [Google Scholar] [CrossRef]
- Nordic Council of Ministers. Nordic Nutrition Recommendations 2012—Integrating Nutrition and Physical Activity; Nordic Council of Ministers: Copenhagen, Denmark, 2014. [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D; The National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Thorsdottir, I.; Atladottir, H.; Palsson, G. Infant Nutrition in Iceland 1995–2000; Unit for Nutrition Research: Reykjavik, Iceland, 2000. [Google Scholar]
- Thorsdottir, I.; Thorisdottir, A.V.; Palsson, G. Infant Nutrition in Iceland 2005–2007; Unit for Nutrition Research: Reykjavik, Iceland, 2008. [Google Scholar]
- Gunnarsdottir, I.; Eysteinsdottir, T.; Thorsdottir, I. Diet for Preschool Children age 3 and 5 Years old in Iceland 2007; Unit for Nutrition Research and Public Health Institue of Iceland: Reykjavik, Iceland, 2008. [Google Scholar]
- Kristinsdottir, H.; Jonasdottir, S.; Bjornsson, S.; Ludvigsson, P. Rickets in a child. Laeknabladid 2011, 97, 477–480. [Google Scholar]
- Thorisdottir, A.V.; Thorsdottir, I.; Palsson, G.I. Nutrition and iron status of 1-year olds following a revision in infant dietary recommendations. Anemia 2011, 2011. [Google Scholar] [CrossRef]
- Matis Ltd.—Icelandic Food and Biotech R & D. Food Composition Tables. ISGEM (The Icelandic Food Composition Database); Matis Ltd.—Icelandic Food and Biotech R & D: Reykjavik, Iceland, 2008. Available online: http://www.matis.is/ISGEM/en/ (accessed on 7 February 2014).
- Thorisdottir, A.V.; Gunnarsdottir, I.; Thorsdottir, I. Revised infant dietary recommendations: The impact of maternal education and other parental factors on adherence rates in Iceland. Acta Paediatr. 2013, 102, 143–148. [Google Scholar] [CrossRef]
- Misra, M.; Pacaud, D.; Petryk, A.; Collett-Solberg, P.F.; Kappy, M. Vitamin D deficiency in children and its management: Review of current knowledge and recommendations. Pediatrics 2008, 122, 398–417. [Google Scholar] [CrossRef]
- Braegger, C.; Campoy, C.; Colomb, V.; Decsi, T.; Domellof, M.; Fewtrell, M.; Hojsak, I.; Mihatsch, W.; Molgaard, C.; Shamir, R.; et al. Vitamin D in the healthy European paediatric population. J. Pediatr. Gastroenterol. Nutr. 2013, 56, 692–701. [Google Scholar] [CrossRef]
- Ostergard, M.; Arnberg, K.; Michaelsen, K.F.; Madsen, A.L.; Krarup, H.; Trolle, E.; Molgaard, C. Vitamin D status in infants: Relation to nutrition and season. Eur. J. Clin. Nutr. 2011, 65, 657–660. [Google Scholar] [CrossRef]
- Holvik, K.; Brunvand, L.; Brustad, M.; Meyer, H.E. Vitamin D Status in the Norwegian Population. In Solar Radiation and Human Health; Bjertness, E., Ed.; The Norwegian Academy of Science and Letters: Oslo, Norway, 2008; pp. 216–228. [Google Scholar]
- Viljakainen, H.T.; Korhonen, T.; Hytinantti, T.; Laitinen, E.K.; Andersson, S.; Makitie, O.; Lamberg-Allardt, C. Maternal vitamin D status affects bone growth in early childhood—A prospective cohort study. Osteoporos. Int. 2011, 22, 883–891. [Google Scholar] [CrossRef]
- Directorate of Health and Centre of Development. Infant and Children Care. Guidelines on Health Protection of Children 0–5 Years, 3rd ed.; Directorate of Health: Reykjavik, Iceland, 2013. [Google Scholar]
- Statistics Iceland. Population by Municipality, Age and Sex 1 December 1997–2013. Statistics, Population (Online); Statistics Iceland: Reykjavik, Iceland, 2013. Available online: http://www.statice.is/ (accessed on 12 March 2014).
- Vieth, R. Implications for 25-hydroxyvitamin D testing of public health policies about the benefits and risks of vitamin D fortification and supplementation. Scand. J. Clin. Lab. Investig. Suppl. 2012, 243, 144–153. [Google Scholar]
- The Public Health Institute of Iceland. Recommendations on Diet and Nutrients for Adults and Children from Two Years of Age; Booklet: Reykjavik, Iceland, 2006. [Google Scholar]
- Nielsen, A.; Michaelsen, K.F.; Holm, L. Parental concerns about complementary feeding: Differences according to interviews with mothers with children of 7 and 13 months of age. Eur. J. Clin. Nutr. 2013, 67, 1157–1162. [Google Scholar] [CrossRef]
- Kyttala, P.; Erkkola, M.; Kronberg-Kippila, C.; Tapanainen, H.; Veijola, R.; Simell, O.; Knip, M.; Virtanen, S.M. Food consumption and nutrient intake in Finnish 1–6-year-old children. Public Health Nutr. 2010, 13, 947–956. [Google Scholar] [CrossRef]
- Kristjansdottir, A.G.; Thorsdottir, I. Adherence to food-based dietary guidelines and evaluation of nutrient intake in 7-year-old children. Public Health Nutr. 2009, 12, 1999–2008. [Google Scholar] [CrossRef]
- Thorsdottir, I.; Gunnarsdottir, I. The Diet of Icelandic 9- and 15-Year-Old Children and Adolescents; Unit for Nutrition Research and Public Health Institute of Iceland: Reykjavik, Iceland, 2006. [Google Scholar]
- Thorgeirsdottir, H.; Valgeirsdottir, H.; Gunnarsdottir, I.; Gisladottir, E.; Gunnarsdottir, B.E.; Thorsdottir, I.; Stefansdottir, J.; Steingrimsdottir, L. The Diet of Icelanders—Results from a National Nutrition Survey 2010–2011; Directorate of Health, the Icelandic Food and Veterinary Authority, Unit for Nutrition Research: Reykjavik, Iceland, 2011. [Google Scholar]
- Gunnarsdottir, I.; Helgadottir, H.; Thorisdottir, B.; Thorsdottir, I. Diet of six-year-old Icelandic children—National dietary survey 2011–2012. Laeknabladid 2013, 99, 17–23. [Google Scholar]
- Steingrimsdottir, L.; Gunnarsson, O.; Indridason, O.S.; Franzson, L.; Sigurdsson, G. Relationship between serum parathyroid hormone levels, vitamin D sufficiency, and calcium intake. JAMA 2005, 294, 2336–2341. [Google Scholar] [CrossRef]
- Gunnarsson, O.; Indriethason, O.S.; Franzson, L.; Halldorsdottir, E.; Sigurethsson, G. Vitamin-D homeostasis amongst adult Icelandic population. Laeknabladid 2004, 90, 29–36. [Google Scholar]
- Bjarnadottir, A.; Kristjansdottir, A.G.; Hrafnkelsson, H.; Johannsson, E.; Magnusson, K.T.; Thorsdottir, I. Insufficient autumn vitamin-D intake and low vitamin-D status in 7-year-old Icelandic children. Public Health Nutr. 2014. [Google Scholar] [CrossRef]
- Hower, J.; Knoll, A.; Ritzenthaler, K.L.; Steiner, C.; Berwind, R. Vitamin D fortification of growing up milk prevents decrease of serum 25-hydroxyvitamin D concentrations during winter: A clinical intervention study in Germany. Eur J. Pediatr. 2013, 172, 1597–1605. [Google Scholar] [CrossRef]
- Dawodu, A.; Akinbi, H. Vitamin D nutrition in pregnancy: Current opinion. Int. J. Women’s Health 2013, 5, 333–343. [Google Scholar] [CrossRef]
- Janssen, M.J.; Wielders, J.P.; Bekker, C.C.; Boesten, L.S.; Buijs, M.M.; Heijboer, A.C.; van der Horst, F.A.; Loupatty, F.J.; van den Ouweland, J.M. Multicenter comparison study of current methods to measure 25-hydroxyvitamin D in serum. Steroids 2012, 77, 1366–1372. [Google Scholar] [CrossRef]
- Singh, R.J.; Taylor, R.L.; Reddy, G.S.; Grebe, S.K. C-3 epimers can account for a significant proportion of total circulating 25-hydroxyvitamin D in infants, complicating accurate measurement and interpretation of vitamin D status. J. Clin. Endocrinol. Metab. 2006, 91, 3055–3061. [Google Scholar] [CrossRef]
- Stepman, H.C.; Vanderroost, A.; Stockl, D.; Thienpont, L.M. Full-scan mass spectral evidence for 3-epi-25-hydroxyvitamin D(3) in serum of infants and adults. Clin. Chem. Lab. Med. 2011, 49, 253–256. [Google Scholar]
- Madar, A.A.; Stene, L.C.; Meyer, H.E. Vitamin D status among immigrant mothers from Pakistan, Turkey and Somalia and their infants attending child health clinics in Norway. Br. J. Nutr. 2009, 101, 1052–1058. [Google Scholar] [CrossRef]
- Holmlund-Suila, E.; Koskivirta, P.; Metso, T.; Andersson, S.; Makitie, O.; Viljakainen, H.T. Vitamin D deficiency in children with a chronic illness-seasonal and age-related variations in serum 25-hydroxy Vitamin D concentrations. PLoS One 2013, 8, e60856. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Thorisdottir, B.; Gunnarsdottir, I.; Steingrimsdottir, L.; Palsson, G.I.; Thorsdottir, I. Vitamin D Intake and Status in 12-Month-Old Infants at 63–66° N. Nutrients 2014, 6, 1182-1193. https://doi.org/10.3390/nu6031182
Thorisdottir B, Gunnarsdottir I, Steingrimsdottir L, Palsson GI, Thorsdottir I. Vitamin D Intake and Status in 12-Month-Old Infants at 63–66° N. Nutrients. 2014; 6(3):1182-1193. https://doi.org/10.3390/nu6031182
Chicago/Turabian StyleThorisdottir, Birna, Ingibjorg Gunnarsdottir, Laufey Steingrimsdottir, Gestur I. Palsson, and Inga Thorsdottir. 2014. "Vitamin D Intake and Status in 12-Month-Old Infants at 63–66° N" Nutrients 6, no. 3: 1182-1193. https://doi.org/10.3390/nu6031182