A Feasibility Study of Taste & See: A Church Based Programme to Develop a Healthy Relationship with Food
Abstract
:1. Introduction
2. Aim
3. Objectives
- To determine how feasible it is to evaluate Taste & See within a UK church setting in preparation for developing a randomised controlled trial (RCT).
- To investigate change in physical, psychological and spiritual well-being in participants pre- and post-programme, and at six-month follow-up.
- To assess change in eating behaviour, nutritional intake and physical activity pre- and post-programme, and at six-month follow-up.
- To explore participant acceptability (fully reported elsewhere) and the facilitators’ experiences in delivering the intervention.
4. Methods
4.1. Design
4.2. Setting
4.3. Participants
“Of our 18 participants, 15 participants had a BMI greater than 25 kg/m2 with mean (SD) UE, CR, EE scores of 57 (19), 29 (20), and 67 (23) respectively. Three participants had a BMI between 18.5 and 25 kg/m2 with mean UE, CR, EE scores of 50 (20), 50 (28) and 43 (19) respectively.”
4.4. Facilitators
4.5. Ethical Approval
4.6. Intervention
- Scientific content of evidence-based dietetic practice,
- Activities designed for discussion in small groups of 3–4 participants to consider the application of these dietetic principles in their own lives,
- Biblical view on the issues raised,
- Opportunity, without obligation, to respond individually to spiritual content if participants wish to do so,
- Activity for the week to practice making health behaviour changes,
- Daily Bible reading and prayer material for those who want to engage with this.
4.7. Outcomes
- Anthropometric measures of height, weight, BMI, percentage body fat and blood pressure,
- Health-Related Quality of Life was measured by the five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) and the Quality of Life-Visual Analogue Scale (QoL-VAS) as measured by the European Quality of Life-5-Dimensions-5-Levels (EQ-5D-5L) [27].
- Physical activity as measured by the Stanford seven-day physical activity recall [32].
- Nutritional intake as measured by a seven-day food diary.
4.8. Sample Size
4.9. Data Analysis
5. Results
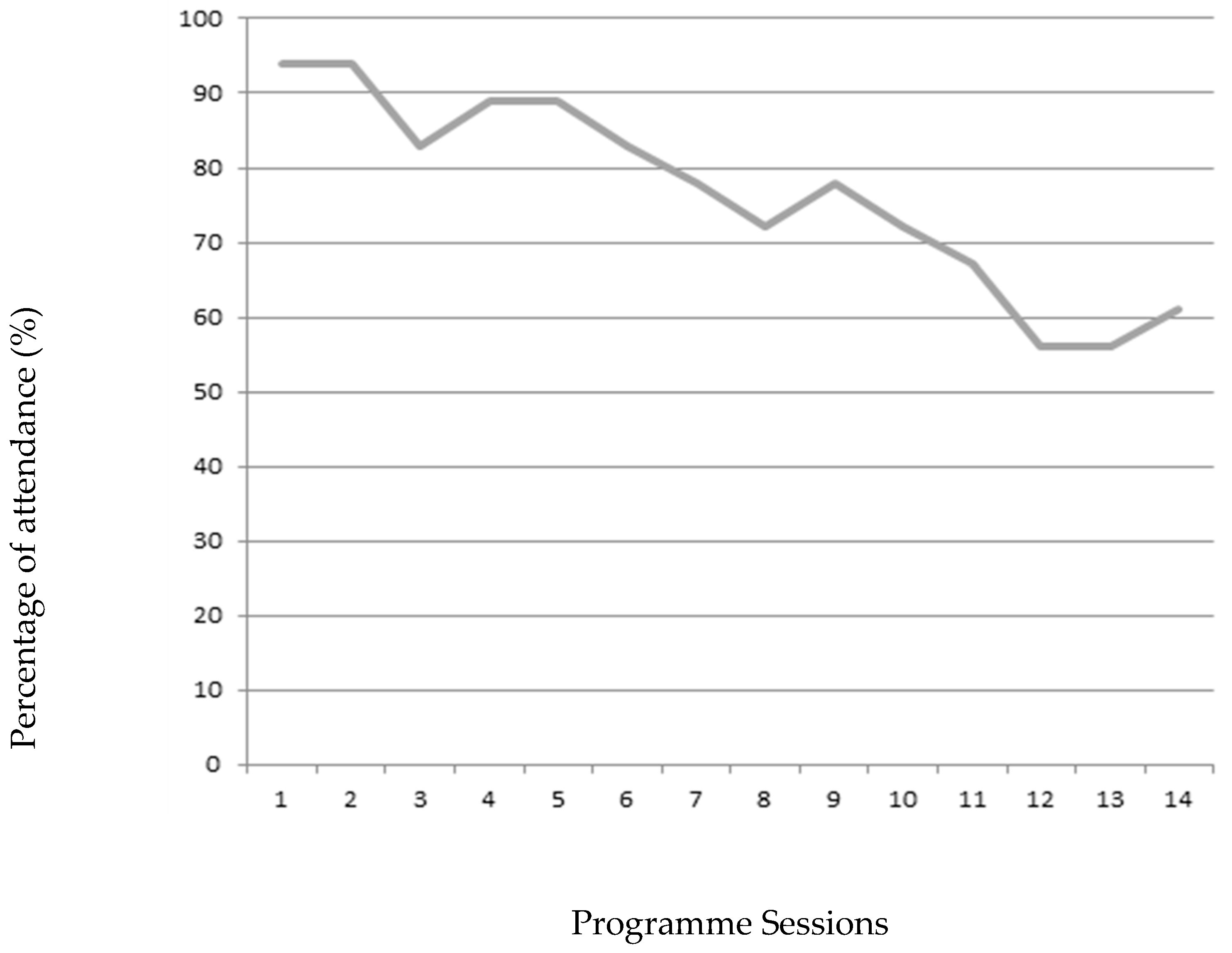
5.1. Participant Retention
5.2. Participant Demographic Details
5.3. Changes in Outcomes from Baseline to End of Intervention
5.4. Sustained and Un-Sustained Changes in Outcomes at Follow-Up
5.5. Facilitator Feasibility and Acceptability
5.5.1. Theme 1: Facilitating the Group Was Not Always Easy
“I think generally it would have been good to have some advice on…what the facilitators were supposed to do, what they were supposed to ask.”[Extract 1, Facilitator 1]
“A little bit more clarity [around] the role you wanted us to play. I think that would have been the most helpful. I mean all the stuff is in the book or hand-outs and we have them in advance and we can read through and understand that stuff, but what do we do with it? How do we actually put it into practice?”[Extract 2, Facilitator 2]
“What were the real objectives in that conversation? Was there a real objective or was it just an open time? If there were objectives, how are we going to get there… how much were we to be just somebody chatting within the group or [how much were we] actually pulling people towards an objective?[Extract 3, Facilitator 2]
“Yeah I was unsure what my role was, whether I’m supposed to be just part of it [and] encourage conversation or actually be the example setter or be the teacher.”[Extract 4, Facilitator 2]
“I think on one week I felt in reflection that I probably should have been more encouraging and practicing it than actually bringing my personal opinion.”[Extract 5, Facilitator 2]
5.5.2. Theme 2: Developing More Thorough Training Resources
“I was just thinking earlier about some difficult people. There was a difficult person in my group who I [found] difficult to manage because they weren’t allowing other people to speak. I really had to put in some more tactics for that group, but perhaps that goes back to the initial facilitators training.”[Extract 6, Facilitator 1]
“I didn’t think people were going to have such massive issues. I thought it was basically well, just stop eating so much…but I’ve discovered it’s more complicated than that.”[Extract 7, Facilitator 1]
“Another thing I was thinking was having advice or information on the sorts of issues people are going to have…I had someone in my group who had eating disorder issues and I didn’t know and I didn’t know what to do about it...”[Extract 8, Facilitator 1]
“What I’m just wary of is going digging, which is what we were doing really and then digging something up that is a lot bigger. [We need to] make sure that [the] person is in a position where they can handle [it, and] take it to a counsellor.”[Extract 9, Facilitator 3]
“I think one of the challenges is staying completely non-judgemental, even if you think you’re [not] judging it’s easy to say something that someone else can then feel they’re being judged.”[Extract 10, Facilitator 3]
5.6. Participants’ Experience and Engagement
6. Discussion
6.1. Summary of Results
6.2. Strengths of the Study
6.3. Limitations of the Study
6.4. Consistency of Findings
7. Conclusions and Implications
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Gema Frühbeck, and Volkan Yumuk. “Obesity: A Gateway Disease with a Rising Prevalence.” Obesity Facts 7 (2014): 33–36. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Health Observatory (GHO) Data. Prevelance of Obesity Ages 18+. Geneva: WHO, 2016. [Google Scholar]
- World Health Organization. Interventions on Diet and Physical Activity: What Works: Summary Report. Geneva: WHO, 2009. [Google Scholar]
- Kristie Lancaster, Lori Carter-Edwards, Stephanie Grilo, Chwan Li Shen, and Antoinette Schoenthaler. “Obesity interventions in African American faith-based organizations: A systematic review.” Obesity Reviews 15 (2014): 159–76. [Google Scholar] [CrossRef] [PubMed]
- Shirley Timmons. “Review and evaluation of faith-based weight management interventions that target African American women.” Journal of Religion and Health 54 (2015): 798–809. [Google Scholar] [CrossRef] [PubMed]
- Deborah Lycett. “The Association of Religious Affiliation and Body Mass Index (BMI): An Analysis from the Health Survey for England.” Journal of Religion and Health 54 (2014): 1–19. [Google Scholar]
- Conrad Hackett, Phillip Connor, Marcin Stonawski, Vegard Skirbekk, M. Potancoková, and G. Abel. The Future of World Religions: Population Growth Projections, 2010–2050. Washington: Pew Research Center, 2015. [Google Scholar]
- Jeroen Barte, Nancy Ter Bogt, Rik Bogers, Pedro Teixeira, Bryan Blissmer, Trevor Mori, and Wanda Bemelmans. “Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review.” Obesity Reviews 11 (2010): 899–906. [Google Scholar] [CrossRef] [PubMed]
- Traci Mann, A. Janet Tomiyama, Erika Westling, Ann-Marie Lew, Barbra Samuels, and Jason Chatman. “Medicare’s Search for Effective Obesity Treatments: Diets are Not the Answer.” American Psychologist 62 (2007): 220–33. [Google Scholar] [PubMed]
- Julie Schaefer, and Amy Magnuson. “A review of interventions that promote eating by internal cues.” Journal of the Academy of Nutrition and Dietetics 114 (2014): 734–60. [Google Scholar] [CrossRef] [PubMed]
- Tracy L. Tylka. “Development and psychometric evaluation of a measure of intuitive eating.” Journal of Counseling Psychology 53 (2006): 226–40. [Google Scholar] [CrossRef]
- Tracy L. Tylka, and Ashley M. Kroon van Diest. “The Intuitive Eating Scale—2: Item Refinement and Psychometric Evaluation with College Women and Men.” Journal of Counseling Psychology 60 (2013): 137–53. [Google Scholar] [CrossRef] [PubMed]
- Nazanin Khasteganan, Deborah Lycett, Andy Turner, Amanda Farley, Nicola Lindson-Hawley, and Gill Furze. “Health, not weight loss, focused versus conventional weight loss programmes for cardiovascular risk factors: Protocol for a Cochrane Review.” Cochrane Database of Systematic Reviews 7 article CD011182. (2014). [Google Scholar]
- Sandra M. Eldridge, Claire L. Chan, Michael J. Campbell, Christine M. Bond, Sally Hopewell, Lehana Thabane, and Gillian A. Lancaster. “CONSORT 2010 statement: Extension to randomised pilot and feasibility trials.” Pilot and Feasibility Studies 2 (2016): 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deborah Lycett, Riya Patel, Anne Coufopoulos, and Andy Turner. “Protocol of Taste and See: A Feasibility Study of a Church-Based, Healthy, Intuitive Eating Programme.” Religions 7 (2016): 41–54. [Google Scholar] [CrossRef]
- Jacinta Ashworth, and Ian Farthing. Churchgoing in the UK. A Research Report from Tearfund on Church Attendance in the UK. London: Tearfund, 2007. [Google Scholar]
- Natti Ronel, and Galit Libman. “Eating Disorders and Recovery: Lessons from Overeaters Anonymous.” Clinical Social Work Journal 31 (2003): 155–71. [Google Scholar] [CrossRef]
- ChurchCare. “Open and Sustainable.” 2012. Available online: Http://www.churchcare.co.uk/churches/open-sustainable (accessed on 8 January 2017).
- Jan Karlsson, Lars-Olof Persson, Lars Sjöström, and Marriane Sullivan. “Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects.” International Journal of Obesity Related Metabolic Disorder 24 (2000): 1715–25. [Google Scholar] [CrossRef]
- Jan Karlsson. “Three-Factor Eating Questionnaire Revised 21 items Scoring Instructions.” (Personal Correspondance).
- J. Cappelleri, A. G. Bushmakin, R. A. Gerber, N. K. Leidy, C. C. Sexton, M. R. Lowe, and J. Karlsson. “Psychometric analysis of the Three-Factor Eating Questionnaire-R21: Results from a large diverse sample of obese and non-obese participants.” International Journal of Obesity 33 (2009): 611–20. [Google Scholar] [CrossRef] [PubMed]
- A. Laurenius, I. Larsson, M. Bueter, K. J. Melanson, I. Bosaeus, H. Bertéus Forslund, H. Lönroth, L. Fändriks, and T. Olbers. “Changes in eating behaviour and meal pattern following Roux-en-Y gastric bypass.” International Journal of Obesity 36 (2012): 348–55. [Google Scholar] [CrossRef] [PubMed]
- Kjersti Karoline Danielsen, Mette Svendsen, Sverre Mæhlum, and Jorunn Sundgot-Borgen. “Changes in body composition, cardiovascular disease risk factors, and eating behavior after an intensive lifestyle intervention with high volume of physical activity in severely obese subjects: A prospective clinical controlled trial.” Journal of Obesity 2013 article 325464. (2013). [Google Scholar] [CrossRef] [PubMed]
- Ruth Tennant, Louise Hiller, Ruth Fishwick, Stephen Platt, Stephen Joseph, Scott Weich, Jane Parkinson, Jenny Secker, and Sarah Stewart-Brown. “The Warwick-Edinburgh mental well-being scale (WEMWBS): Development and UK validation.” Health and Quality of Life Outcomes 5 (2007): 63–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robert L. Spitzer, Kurt Kroenke, Janet B. W. Williams, and Bernd Löwe. “A brief measure for assessing generalized anxiety disorder: The GAD-7.” Archives of Internal Medicine 166 (2006): 1092–97. [Google Scholar] [CrossRef] [PubMed]
- Kurt Kroenke, and Robert L. Spitzer. “The PHQ-9: A new depression diagnostic and severity measure.” Psychiatric Annals 32 (2002): 509–21. [Google Scholar] [CrossRef]
- Michael Herdman, Claire Gudex, Andrew Lloyd, Bas Janssen, Paul Kind, David Parkin, Gouke Bonsel, and Xavier Badia. “Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L).” Quality of Life Research 20 (2011): 1727–36. [Google Scholar] [CrossRef] [PubMed]
- Raymond Paloutzian, and Craig Ellison. “Loneliness, spiritual well-being and the quality of life.” In Loneliness: A Sourcebook of Current Theory, Research and Therapy. Edited by Anne Peplau and Daniel Perlman. New York: Wiley, 1982, pp. 224–37. [Google Scholar]
- Rodger K. Bufford, Raymond F. Paloutzian, and Craig Ellison. “Norms for the spiritual well-being scale.” Journal of Psychology and Theology 19 (1991): 56–70. [Google Scholar]
- Rowatt Wade, and Lee Kirkpatrick. “Dimensions of attachment to God and their subsequent attachment to affect, religiosity, and personality constructs.” Journal for the Scientific Study of Religion 41 (2002): 637–51. [Google Scholar]
- Jeff Levin, and Berton H. Kaplan. “The sorokin multidimensional inventory of love experience (SMILE): Development, validation, and religious determinants.” Review of Religious Research 51 (2010): 380–401. [Google Scholar]
- James F. Sallis, William L. Haskell, Peter D. Wood, Stephen P. Fortmann, Todd Rogers, Steven N. Blair, and Ralph S. Paffenbarger. “Physical activity assessment methodology in the Five City Project.” American Journal of Epidemiology 121 (1985): 91–106. [Google Scholar] [CrossRef] [PubMed]
- Riya Patel, Deborah Lycett, Anne Coufopoulos, and Andy Turner. “Moving forward in their journey: Participant’s experience of Taste & See: A church-based programme to develop a healthy relationship with food.” Religions 8 article 14. (2017). [Google Scholar]
- Virginia Braun, and Victoria Clarke. “Using thematic analysis in psychology.” Qualitative Research in Psychology 1 (2006): 77–101. [Google Scholar] [CrossRef]
- Dale A. Schoeller. “How accurate is self-reported dietary energy intake? ” Nutrition Reviews 48 (1990): 373–79. [Google Scholar] [CrossRef] [PubMed]
- Janet A. Tooze, Susan M. Krebs-Smith, Richard P. Troiano, and Amy F. Subar. “The accuracy of the Goldberg method for classifying misreporters of energy intake on a food frequency questionnaire and 24-h recalls: Comparison with doubly labeled water.” European Journal of Clinical Nutrition 66 (2012): 569–76. [Google Scholar] [CrossRef] [PubMed]
- Sunita Dodani, and Jeremy Fields. “Implementation of the fit body and soul, a church-based life style program for diabetes prevention in high-risk African Americans a feasibility study.” The Diabetes Educator 36 (2010): 465–72. [Google Scholar] [CrossRef] [PubMed]
- Karen Hye-cheon Kim Yeary, Carol Cornell, Jerome Turner, Page Moore, Zoran Bursac, Elaine Prewitt, and Delia Smith West. “Feasibility of an evidence-based weight loss intervention for a faith-based, rural, African American population.” Preventing Chronic Disease 8 (2011): 1–12. [Google Scholar]
- Carolyn Murrock, and Faye Gary. “Culturally specific dance to reduce obesity in African American women.” Health Promotion Practice 11 (2010): 465–73. [Google Scholar] [CrossRef] [PubMed]
- Ken Resnicow, Alice Jackson, Dhana Blissett, Terry Wang, Frances McCarty, Simone Rahotep, and Santhi Periasamy. “Results of the healthy body healthy spirit trial.” Health Psychology 24 (2005): 339–48. [Google Scholar] [CrossRef] [PubMed]
- Sara Wilcox, Allen Parrott, Meghan Baruth, Marilyn Laken, Margaret Condrasky, Ruth Saunders, Marsha Dowda, Rebecca Evans, Cheryl Addy, Tatiana Warren, and et al. “The Faith, Activity, and Nutrition program: A randomized controlled trial in African-American churches.” American Journal of Preventive Medicine 44 (2013): 122–31. [Google Scholar] [CrossRef] [PubMed]
- Dawn Clifford, Amy Ozier, Joanna Bundros, Jeffrey Moore, Anna Kreiser, and Michelle Neyman Morris. “Impact of non-diet approaches on attitudes, behaviors, and health outcomes: A systematic review.” Journal of Nutrition Education and Behavior 47 (2015): 143–55. [Google Scholar] [CrossRef] [PubMed]
- Marie-Pierre Gagnon-Girouard, Catherine Bégin, Véronique Provencher, Angelo Tremblay, Lyne Mongeau, Sonia Boivin, and Simone Lemieux. “Psychological impact of a ‘Health-at-Every-Size’ intervention on weight-preoccupied overweight/obese women.” Journal of Obesity 2010 (2010): 1–13. [Google Scholar] [CrossRef] [PubMed]
- Laurel Mellin, Mary Croughan-Minihane, and Larry Dickey. “The Solution Method: 2-year trends in weight, blood pressure, exercise, depression, and functioning of adults trained in development skills.” Journal of the American Dietetic Association 97 (1997): 1133–38. [Google Scholar] [CrossRef]
- P. Roughan, E. Seddon, and J. Vernon-Roberts. “Long-term effects of a psychologically based group programme for women preoccupied with body weight and eating behaviour.” International Journal of Obesity 14 (1990): 135–47. [Google Scholar] [PubMed]
- Sheryl Tanco, Wolfgang Linden, and Tracey Earle. “Well-being and morbid obesity in women: A controlled therapy evaluation.” International Journal of Eating Disorders 23 (1988): 325–39. [Google Scholar] [CrossRef]
- Véronique Provencher, Catherine Bégin, Angelo Tremblay, Lyne Mongeau, Louise Corneau, Sylvie Dodin, Sonia Boivin, and Simone Lemieux. “Health-at-every-size and eating behaviors: 1-year follow-up results of a size acceptance intervention.” Journal of the American Dietetic Association 109 (2009): 1854–61. [Google Scholar] [CrossRef] [PubMed]
- Vicky Leblanc, Véronique Provencher, Catherine Bégin, Louise Corneau, Angelo Tremblay, and Simone Lemieux. “Impact of a Health-At-Every-Size intervention on changes in dietary intakes and eating patterns in premenopausal overweight women: Results of a randomized trial.” Clinical Nutrition 31 (2012): 481–88. [Google Scholar] [CrossRef] [PubMed]
- Renee Cole, and Tanya Horacek. “Effectiveness of the My Body Knows When intuitive-eating pilot program.” American Journal of Health Behavior 34 (2010): 286–97. [Google Scholar] [CrossRef] [PubMed]
- L. Rapoport, M. Clark, and J. Wardle. “Evaluation of a modified cognitive-behavioural programme for weight management.” International Journal of Obesity 24 (2000): 1726–37. [Google Scholar] [CrossRef] [PubMed]
- Tracy Sbrocco, Randall C. Nedegaard, Jay M. Stone, and Evelyn L. Lewis. “Behavioral choice treatment promotes continuing weight loss: Preliminary results of a cognitive–behavioral decision-based treatment for obesity.” Journal of Consulting and Clinical Psychology 67 (1999): 260–66. [Google Scholar] [CrossRef] [PubMed]
- Y. Ma, B. C. Olendzki, W. Li, A. R. Hafner, D. Chiriboga, J. R. Hebert, M. Campbell, M. Sarnie, and I. S. Ockene. “Seasonal variation in food intake, physical activity, and body weight in a predominantly overweight population.” European Journal of Clinical Nutrition 60 (2006): 519–28. [Google Scholar] [CrossRef] [PubMed]
- Betty M. Kennedy, Sahasporn Paeratakul, Catherine M. Champagne, Donna H. Ryan, David W. Harsha, Bernestine McGee, Glenda Johnson, and Farzad Deyhim. “A Pilot church-based weight loss program for African-American adults using church members as health educators: A comparison of individual and group intervention.” Ethnicity & Disease 15 (2005): 373–78. [Google Scholar]
- Judith Z. Goldfinger, Guedy Arniella, Judith Wylie-Rosett, and Carol R. Horowitz. “Project HEAL: Peer education leads to weight loss in Harlem.” Journal of Health Care for the Poor and Underserved 19 (2008): 180–92. [Google Scholar] [CrossRef] [PubMed]
- Karen Hye-cheon Kim, Laura Linnan, Marci Kramish Campbell, Christine Brooks, Harold G. Koenig, and Christopher Wiesen. “The WORD (wholeness, oneness, righteousness, deliverance): A faith-based weight-loss program utilizing a community-based participatory research approach.” Health Education & Behavior 35 (2008): 634–50. [Google Scholar] [CrossRef] [PubMed]
- Nina Van Dyke, and Eric J. Drinkwater. “Review article relationships between intuitive eating and health indicators: Literature review.” Public Health Nutrition 17 (2014): 1757–66. [Google Scholar] [CrossRef] [PubMed]
- Lauren J. Bruce, and Lina A. Ricciardelli. “A systematic review of the psychosocial correlates of intuitive eating among adult women.” Appetite 96 (2016): 454–72. [Google Scholar] [CrossRef] [PubMed]
- Jeanne Dalen, Bruce W. Smith, Brian M. Shelley, Anita Lee Sloan, Lisa Leahigh, and Debbie Begay. “Pilot study: Mindful Eating and Living (MEAL): Weight, eating behavior, and psychological outcomes associated with a mindfulness-based intervention for people with obesity.” Complementary Therapies in Medicine 18 (2010): 260–64. [Google Scholar] [CrossRef] [PubMed]
- Jean Kristeller, Ruth Q. Wolever, and Virgil Sheets. “Mindfulness-based eating awareness training (MB-EAT) for binge eating: A randomized clinical trial.” Mindfulness 5 (2014): 282–97. [Google Scholar] [CrossRef]
- Pehr Granqvist, and Lee Kirkpatrick. “Religion, spirituality and attachment.” In APA Handbook of Psychology, Religion and Spirituality. Edited by Kenneth Pargament, Julie Exline and James Jones. Washington: American Psychological Association, 2013, pp. 139–55. [Google Scholar]
- Kristin J. Homan, and Brianna N. Cavanaugh. “Perceived relationship with God fosters positive body image in college women.” Journal of Health Psychology 18 (2013): 1529–39. [Google Scholar] [CrossRef] [PubMed]
- Kristin J. Homan, and Chris J. Boyatzis. “The protective role of attachment to God against eating disorder risk factors: Concurrent and prospective evidence.” Eating Disorders 18 (2010): 239–58. [Google Scholar] [CrossRef] [PubMed]

| Session | Scientific Principle | Biblical Principle |
|---|---|---|
| Session 1: Your Relationship with Food To develop an awareness of self, of eating habits and of a God who cares about this. | The holistic aspects of eating The evidence for addressing the spiritual in weight management. | We are physical and spiritual beings. God loves us and wants to be involved in our lives |
| Session 2: What dietary rules do you follow? To introduce intuitive eating versus dietary restriction. | The diet and weight regain cycle The evidence for finding what approach suits you The evidence for intuitive eating | Freedom with responsibility. “Everything permissible but not everything is beneficial.” |
| Session 3: Are you really hungry? To identify hunger and fullness. | Hormonal regulation of appetite What is a healthy diet? | Created by God. A time for everything. |
| Session 4: Enjoying food again: To feel free to enjoy food. | Evidence for eating attentively, reducing distractions, mindful eating exercise. | The blessings of God, he loves to give us good gifts |
| Session 5: Why else do we eat? To understand impulsive responses to feel happier, to feel less bored, to reduce stress. | Dopamine pathway | The reality of life in an imperfect world Why things went wrong. |
| Session 6: What can we do instead? To identify ways to tackle boredom, stress and low mood. | Evidence-based physical activity and relaxation suggestions | Spiritual coping. Hope in difficult times. |
| Session 7: Leaving the past behind To identify past hurts or habits that still influence our relationship with food today, to find healing in forgiveness. | Evidence of the impact of adverse child events Evidence for forgiveness | ‘Forgive us as we forgive others’ |
| Session 8: You are loved and you are lovely To understand the truth of who you are. | Body congruence Tips to build self-esteem | God’s love and acceptance |
| Session 9: Moving forward To consolidate new attitudes and behaviours, to identify specific aspects of healthy living to work on. | Goal setting Habit formation Tips and ideas for a healthy lifestyle | New creation, with God’s spirit at work within us |
| Session 10: Pressing on/The future To equip participants to be able to continue the Taste and See principles without weekly support. | Identifying and planning for lapses Evidence for behaviour change maintenance | Pressing on and managing failure |
| Mean | SD | Min | Max | ||
| Age (Years) | 47.3 | 14.8 | 19 | 72 | |
| BMI | 33.10 | 7.95 | 22.2 | 52.8 | |
| N (% Frequency) | |||||
| BMI category: | Healthy (BMI: 18.5–24.9 kg/m2) and high TFEQ | 3 (17) | |||
| Overweight (BMI: 25–29.9 kg/m2) | 4 (22) | ||||
| Obese (BMI: 30–39.9 kg/m2) | 8 (44) | ||||
| Morbidly Obese (BMI>40 kg/m2) | 3 (17) | ||||
| Sex: | Male | 3 (17) | |||
| Female | 15 (83) | ||||
| Ethnicity: | White | 16 (88) | |||
| Black | 1 (6) | ||||
| Asian | 1(6) | ||||
| Religion: | Christian | 16 (88) | |||
| Sikh | 1 (6) | ||||
| Spiritual, but not religious | 1 (6) | ||||
| Outcomes: | Baseline | 3 Months (End of Intervention) | 9 Months (6-Month Follow-Up) | Mean Change Baseline—3 Months | SE | 95% CI for Mean Difference | Mean Change from 3–9 Months | SE | 95% CI for Mean Difference | Mean Change Baseline—9 Months | SE | 95% CI for Mean Difference | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| Weight (kg) | 89.2 | 18.9 | 87.6 | 18.9 | 89.1 | 19.1 | −1.6 | 0.6 | −3.2 | 0.1 | 1.5 | 0.7 | −0.3 | 3.2 | −0.10 | 0.6 | −1.7 | 1.5 |
| Body Fat (%) | 44.3 | 9.5 | 41.4 | 13.8 | 43.9 | 9.5 | −2.9 | 2.2 | −8.8 | 3.1 | 2.6 | 2.4 | −3.9 | 9.1 | −0.3 | 0.8 | −2.5 | 1.9 |
| Body Mass Index | 33.11 | 7.90 | 32.60 | 8.00 | 33.10 | 8.10 | −0.60 * | 0.20 | −1.10 | −0.002 | 0.6 | 0.2 | −0.1 | 1.2 | 0.02 | 0.20 | −0.60 | 0.60 |
| Systolic Blood Pressure | 124 | 16 | 127 | 18 | 123 | 17 | 2 | 3 | −5 | 11 | −4 | 3 | −11 | 4 | −1 | 2 | −6 | 4 |
| Diastolic Blood Pressure | 81 | 10 | 82 | 10 | 81 | 10 | 1 | 3 | −6 | 8 | −0.6 | 2 | −6 | 5 | 0.4 | 2 | −4 | 5 |
| EQ-5D5LL: Self-Care | 1.0 | 0.0 | 1.0 | 0.0 | 1.0 | 0.0 | 0.0 | 0.0 | 0.0 | |||||||||
| EQ-5D5L: Usual Activities | 1.3 | 0.8 | 1.3 | 0.6 | 1.3 | 0.7 | 0.0 | 0.2 | −0.4 | 0.4 | 0.0 | 0.1 | −0.2 | 0.2 | 0.0 | 0.1 | −0.3 | 0.3 |
| EQ-5D5L: Pain/Discomfort | 1.9 | 0.8 | 1.6 | 0.8 | 1.7 | 0.8 | −0.3 * | 0.1 | −0.03 | −0.6 | 0.1 | 0.1 | −0.2 | 0.4 | −0.2 | 0.1 | −0.5 | 0.1 |
| EQ-5D5L: Anxiety/Depression | 1.6 | 0.7 | 1.5 | 0.9 | 1.4 | 0.9 | −0.1 | 0.1 | −0.3 | 0.2 | −0.1 | 0.1 | −0.3 | 0.2 | −0.1 | 0.1 | −0.4 | 0.2 |
| EQ-5D5L: Mobility | 1.3 | 0.7 | 1.4 | 0.7 | 1.4 | 0.7 | 0.1 | 0.1 | −0.2 | 0.3 | 0.001 | 0.1 | −0.2 | 0.2 | 0.1 | 0.1 | −0.2 | 0.3 |
| EQ-5D5L: QoL-VAS | 61.0 | 19.0 | 72.0 | 16.2 | 68.0 | 13.5 | 11.7 * | 3.7 | 1.9 | 21.6 | −4.3 | 3.2 | −12.9 | 4.3 | 7.4 | 3.8 | −2.5 | 17.4 |
| TFEQ: Uncontrolled Eating | 56.0 | 18.8 | 39.5 | 19.8 | 42.6 | 21.5 | −16.5 * | 3.7 | −26.2 | −6.7 | 3.1 | 3.6 | −6.4 | 12.5 | −13.4 * | 4.5 | −25.3 | −1.4 |
| TFEQ: Emotional Eating | 62.7 | 23.5 | 43.2 | 23.5 | 45.9 | 22.6 | −19.4 * | 3.8 | −29.4 | −9.5 | 2.8 | 4.1 | −8.2 | 13.8 | −16.7 * | 3.6 | −26.3 | −7.1 |
| TFEQ: Cognitive Restrained Eating | 32.4 | 22.7 | 43.5 | 22.5 | 42.6 | 18.5 | 11.1 * | 3.8 | 0.9 | 21.3 | −1 | 5.5 | −16 | 13 | 10.2 | 4.9 | −2.7 | 23.1 |
| Intuitive Eating (IE) Total | 2.5 | 0.5 | 3.1 | 0.6 | 2.9 | 0.6 | 0.6 * | 0.1 | 0.3 | 0.9 | −0.2 | 0.1 | −0.4 | 0.2 | 0.5 * | 0.1 | 0.2 | 0.8 |
| IE: Unconditional Permission to Eat | 3.0 | 0.9 | 3.2 | 0.7 | 3.1 | 0.6 | 0.2 | 0.2 | −0.3 | 0.7 | −0.1 | 0.1 | −0.4 | 0.3 | 0.1 | 0.2 | −0.5 | 0.7 |
| IE: Reliance on Hunger Cues | 2.0 | 0.8 | 3 | 0.9 | 2.8 | 1.09 | 1.1 * | 0.2 | 0.6 | 1.5 | −0.2 | 0.2 | −0.8 | 0.3 | 0.8 * | 0.2 | 0.2 | 1.4 |
| IE: Body Food Choice Congruence | 3.0 | 0.9 | 3.4 | 0.9 | 3.4 | 0.9 | 0.4 | 0.2 | −0.1 | 0.9 | 0.02 | 0.2 | −0.5 | 0.6 | 0.4 * | 0.1 | 0.7 | 0.8 |
| WEMBS: Mental Well-Being | 45.6 | 6.1 | 52.3 | 5.5 | 49.4 | 7.1 | 6.7 * | 1.3 | 3.4 | 10.04 | −2.8 | 1.4 | −6.5 | 0.8 | 3.9 * | 1.5 | 0.01 | 7.8 |
| GAD-7: Anxiety | 7.5 | 4.4 | 3.3 | 2.8 | 5.8 | 5.5 | −4.1 * | 0.9 | −6.5 | −1.6 | 2.4 | 1.1 | −0.4 | 5.3 | −1.6 * | 0.6 | −3.2 | −0.02 |
| PHQ-9: Depression | 6.6 | 5.2 | 3.6 | 2.9 | 5.9 | 5.1 | −3 * | 0.9 | −5.3 | −0.7 | 2.4 | 0.9 | −0.1 | 4.8 | −0.6 | 0.9 | −2.9 | 1.8 |
| Spiritual Well-Being Scale Total | 93.3 | 15.1 | 98.1 | 13.2 | 96.2 | 13.7 | 4.8 | 2.8 | −2.6 | 12.1 | −1.9 | 2.8 | −9.3 | 5.5 | 2.9 | 2.2 | −2.9 | 8.7 |
| SWBS: Religious Well-Being | 48.9 | 12.1 | 49.7 | 8.2 | 49.2 | 10.6 | 0.8 | 1.8 | −4.03 | 5.6 | −0.5 | 1.9 | −5.4 | 4.4 | 0.3 | 1.2 | −2.8 | 3.4 |
| SWBS: Existential Well-Being | 44.4 | 5.7 | 48.4 | 5.8 | 47 | 6.2 | 4.0 | 1.7 | −0.4 | 8.4 | −1.4 | 1.6 | −5.7 | 2.9 | 2.6 | 1.5 | −1.3 | 6.5 |
| SMILE: Religious Love | 17.7 | 3.6 | 18.1 | 2.3 | 17.9 | 3.9 | 0.4 | 0.5 | −0.9 | 1.7 | −0.2 | 0.6 | −1.7 | 1.3 | 0.2 | 0.2 | −0.3 | 0.6 |
| ATG: Avoidant | 2.4 | 1.4 | 2.0 | 1.1 | 2.3 | 1.4 | −0.4 | 0.2 | −0.9 | 0.1 | 0.3 | 0.2 | −0.3 | 0.8 | −0.1 | 0.2 | −0.6 | 0.3 |
| ATG: Anxious | 2.9 | 1.3 | 2.6 | 1.3 | 3.2 | 1.4 | −0.4 | 0.3 | −1.0 | 0.3 | 0.6 | 0.3 | −0.1 | 1.3 | 0.3 | 0.3 | −0.6 | 1.1 |
| Energy Expenditure (Kcal) | 3173 | 711 | 3079 | 744 | 3158 | 642 | −93 | 43 | −208 | 22 | 78 | 68 | −101 | 258 | −14 | 59 | −172 | 143 |
| Energy intake (Kcal) | 2131 | 1278 | 1713 | 551 | 2018 | 1311 | −418 | 370 | −1415 | 580 | 304.7 | 383 | −728 | 1337 | −112 | 71 | −304 | 79 |
| Energy (-Alcohol) (Kcal) | 2150 | 1271 | 1711 | 546 | 2056 | 1301 | −439 | 366 | −1426 | 549 | 345 | 378 | −674 | 1365 | −93 | 69 | −281 | 94 |
| Protein (g) | 67.0 | 12.7 | 66 | 16.2 | 69.1 | 13.5 | −1.0 | 2.4 | −7.6 | 5.5 | 3.1 | 2.7 | −4.2 | 10.5 | 2.1 | 1.3 | −1.4 | 5.6 |
| Carbohydrate (g) | 211 | 51 | 202 | 56 | 204 | 47 | −9 | 6 | −25 | 7 | 1 | 12 | −31 | 33 | −8 | 10 | −35 | 20 |
| Polysaccharides (g) | 101 | 33 | 105 | 31 | 121 | 37 | 4 | 7 | −13 | 22 | 16 | 9 | −10 | 40 | 20 | 9 | −4 | 43 |
| Mono and Disaccharides(g) | 88 | 36 | 81 | 35 | 77 | 26 | −7 | 4 | −17 | 3 | −4 | 7 | −23 | 14 | −11 | 6 | −28 | 5 |
| Fibre (g) | 18.0 | 6.2 | 15.7 | 8.1 | 16.8 | 7.5 | −2.3 | 1.4 | −6.1 | 1.5 | 1 | 2 | −4 | 6 | −1.2 | 1.04 | −3.4 | 1.6 |
| Fat (g) | 71.5 | 26.2 | 64.2 | 32.5 | 61.3 | 24.3 | −7.3 | 5.9 | −23.1 | 8.5 | −3 | 7 | −23 | 17 | −10.2 | 4.8 | −23.1 | 2.7 |
| Saturated Fatty acids (g) | 26.8 | 10.9 | 24.4 | 12.6 | 21.7 | 7.9 | −2.4 | 2.2 | −8.4 | 3.6 | −3 | 3 | −11 | 6 | −5.1 | 2.1 | −10.6 | 0.4 |
| Mono-unsaturated fat (g) | 23.4 | 9.3 | 21.1 | 11.6 | 20.2 | 8.6 | −2.3 | 2 | −7.8 | 3.1 | −1 | 3 | −9 | 7 | −3.2 | 2.04 | −8.7 | 2.3 |
| Poly-unsaturated fat (g) | 10.5 | 3.9 | 9.6 | 4.9 | 10.6 | 4.2 | −0.9 | 0.8 | −3.1 | 1.3 | 1 | 1 | −1 | 4 | 0.2 | 0.7 | −1.7 | 2.1 |
| Sodium (mg) | 1894 | 484 | 1658 | 761 | 1851 | 618 | −236 | 139 | −611 | 138 | 193 | 161 | −239 | 625 | −43 | 113 | −349 | 263 |
| Salt Equivalence (g) | 4.7 | 1.2 | 4.2 | 1.9 | 4.6 | 1.5 | −0.6 | 0.4 | −1.5 | 0.4 | 0.5 | 0.4 | −0.6 | 1.5 | −0.1 | 0.3 | −0.9 | 0.7 |
| Calcium (mg) | 709 | 195 | 631 | 264.1 | 675 | 210 | −77 | 60 | −240 | 86 | 43 | 72 | −152 | 238 | −34 | 33 | −122 | 55 |
| Codes | Sub-themes | Final Theme |
|---|---|---|
| Advice on how to facilitate Purpose of facilitation not explained What should facilitators ask? Should I keep conversation open? Should they be encouraging conversation or applying? Intervention tools Not enough clearness on role Am I the teacher? | What does the facilitator role entail? | Theme 1: Facilitating was not always easy. |
| Should I be living the programme? Example setter or participant? Brought my own opinion Expressing concern Still my opinion It’s difficult Which way is right? I took what I wanted | Challenges related to balancing both the roles of facilitator and participant | |
| How to manage difficult people Dominant people taking over, not letting others speak Help to make sure everyone can talk | Support managing difficult and dominant people | Theme 2: Developing more thorough training resources |
| Managing unexpected issues Unexpected issues not related to weight Managing the range of different things Unexpected spiritual issues People have real problems Serious problem, not expecting this | More advice on the range of issues that can arise | |
| Uncertain of role parameters How much detail should be pulled out from participants? Training around group discussion boundaries Should I try answer all questions? Should personal opinions be given? Trying not to judge people Digging something up We might not handle it We’re not equipped to address it Staying non-judgemental | More advice about boundaries to ensure beneficence |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patel, R.; Lycett, D.; Coufopoulos, A.; Turner, A. A Feasibility Study of Taste & See: A Church Based Programme to Develop a Healthy Relationship with Food. Religions 2017, 8, 29. https://doi.org/10.3390/rel8020029
Patel R, Lycett D, Coufopoulos A, Turner A. A Feasibility Study of Taste & See: A Church Based Programme to Develop a Healthy Relationship with Food. Religions. 2017; 8(2):29. https://doi.org/10.3390/rel8020029
Chicago/Turabian StylePatel, Riya, Deborah Lycett, Anne Coufopoulos, and Andy Turner. 2017. "A Feasibility Study of Taste & See: A Church Based Programme to Develop a Healthy Relationship with Food" Religions 8, no. 2: 29. https://doi.org/10.3390/rel8020029






