Establishing a Pharmacy-Based Patient Registry System: A Pilot Study for Evaluating Pharmacist Intervention for Patients with Long-Term Medication Use
Abstract
:1. Introduction
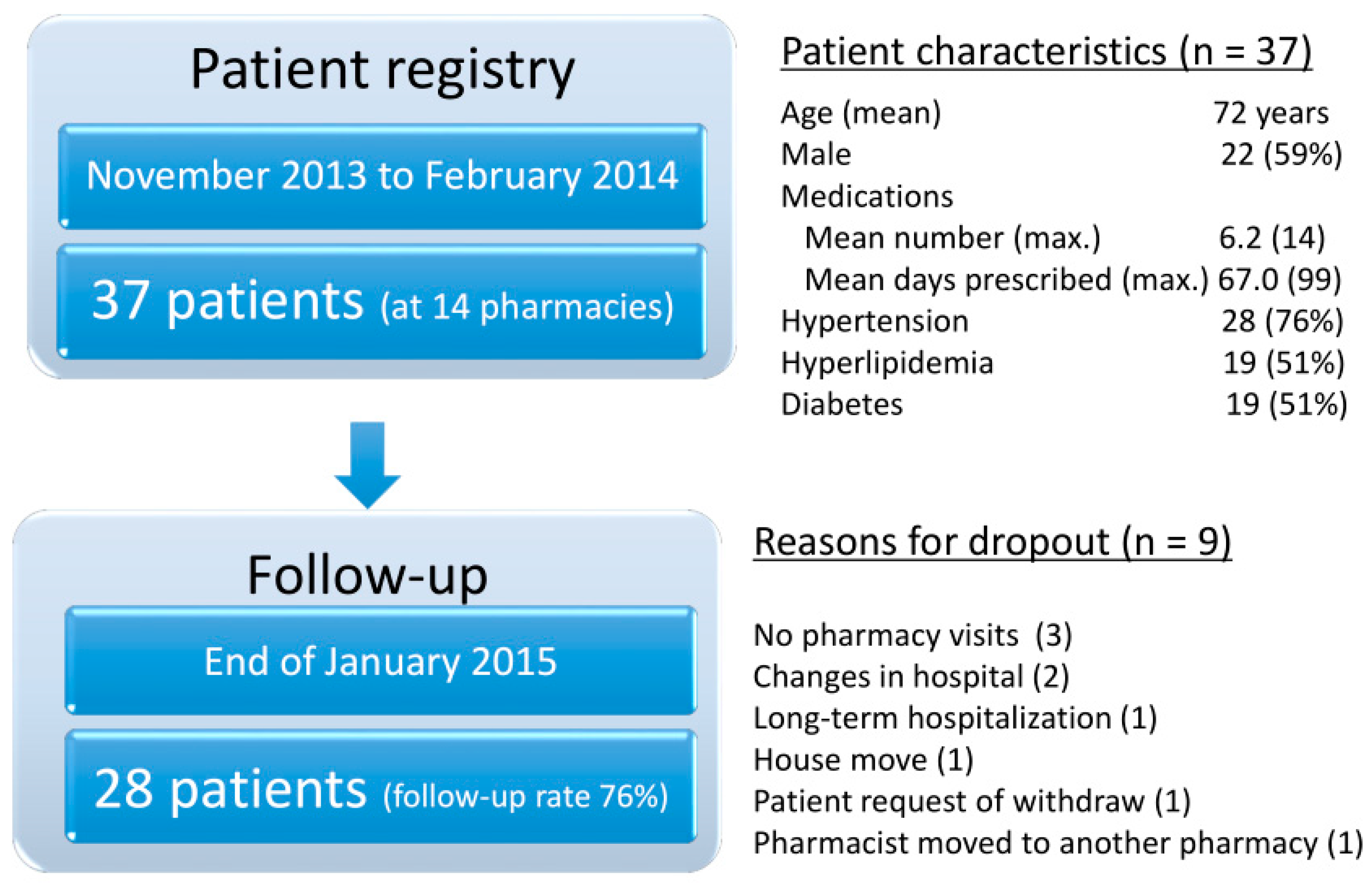
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Disclosure
Appendix A. Data Collection at the Initial and Follow-Up Assessments
- Patient’s ID (automatically assigned at registration)
- Age and sex
- Clinical conditions for long-term medication use
- Date of informed consent
- Contact information if needed
- List of all medications used by the patient (not only dispensed medication at the pharmacy, but also those dispensed at different pharmacies)
- Treatment history
- Other conditions not for long-term medication use
- Lab results (blood pressure, lipid, HbA1c, etc.)
- Treatment conditions (one-pack doses, number of clinics used, etc.)
- Living environments related to treatment (living alone, job, home care, etc.)
- Potential problems reported by patient
- Potential concerns identified by pharmacist
- Preferred methods for follow-up contacts
- Others
- Date of contacts
- Method for monitoring (telephone or visit)
- Changes in medications
- Patient reported adherence or number of medications not used
- Reason for not taking medications as instructed
- Conditional changes (if any)
- Lab results (reported by patients)
- Pharmacist advice given to patients
- Next appointment dates
References
- Abe, S. Japan’s strategy for global health diplomacy: Why it matters. Lancet 2013, 382, 915–916. [Google Scholar] [CrossRef]
- Organisation for Economic Co-operation and Development (OECD). OECD Reviews of Health Care Quality: Japan–Assessment and Recommendations; OECD: Paris, France, 2014. [Google Scholar]
- Nomura, H.; Nakayama, T. The Japanese healthcare system: The issue is to solve the “tragedy of the commons” without making another. BMJ 2005, 331, 648–649. [Google Scholar] [CrossRef] [PubMed]
- Cabinet Office, Government of Japan. General Overview and Examples of the Regulatory Reform Council’s Second Report of Recommendations—Health and Medical Field. Available online: http://www8.cao.go.jp/kisei-kaikaku/english/index-en.html (accessed on 27 October 2017). (In Japanese)
- Ministry of Health, Labour and Welfare. Unused Drugs and Split Dispensing (as a Document Used in Central Social Insurance Medical Council on 22 July 2015). Available online: http://www.mhlw.go.jp/stf/shingi2/0000092094.html (accessed on 27 October 2017). (In Japanese)
- Koyanagi, K.; Kubot, T.; Kobayashi, D.; Kihara, T.; Yoshid, T.; Miisho, T.; Saito, Y.; Uchigoshi, H.; Takaki, J.; Seo, T.; et al. SETSUYAKU-BAG Campaign—Investigation of leftover drugs retained by outpatients and promotion of proper reuse leftover drugs to reduce medical expenses. Yakugak. Zasshi 2013, 133, 1215–1221. [Google Scholar] [CrossRef]
- Nakamura, K.; Urano, K.; Tanaka, M.; Nishiguchi, K.; Sakai, Y.; Katano, T.; Nabekura, T.; Yamamura, K.; Kunimasa, J. The Reduction Impact in Medical Expenses of Pharmaceutical Inquiries on Leftover Medicines at a Community Pharmacy. Jpn. J. Pharm. Health Care Sci. 2014, 40, 522–529. [Google Scholar] [CrossRef]
- Onda, M.; Imai, H.; Kasuga, M.; Yasuda, M.; Shimomura, M.; Okamoto, N.; Takada, Y.; Nanaumi, Y.; Tanaka, Y.; Arakawa, Y. Examining the effect of pharmacists’ visits to housebound patients on the elimination of unused drugs. Jpn. J. Drug. Inform. 2015, 17, 21–33. [Google Scholar]
- Japan Pharmaceutical Association. Study on the Effect of Pharmacist Drug Management for Elderly Patients at Home. Report March 2008. Available online: http://www.nichiyaku.or.jp/action/wp-content/uploads/2008/06/19kourei_hukuyaku1.pdf (accessed on 27 October 2017). (In Japanese).
- Elliott, R.A.; Barber, N.; Clifford, S.; Horne, R.; Hartley, E. The cost effectiveness of a telephone-based pharmacy advisory service to improve adherence to newly prescribed medicines. Pharm. World Sci. 2008, 30, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Nitta, M.; Hara, K.; Watanabe, F.; Akagawa, K.; Kurata, N.; Kamei, M. Community pharmacists provided telephone treatment support for patients who received long-term prescribed medication. Integr. Pharm. Res. Pract. 2016, 5, 27–32. [Google Scholar] [PubMed]
- Ministry of Health, Labour and Welfare 2015: Kanjanotameno Yakkyokubijon (as a Document, “a Vision of Community Pharmacy for Patients” on 23 October 2015). Available online: http://www.mhlw.go.jp/file/04-Houdouhappyou-11121000-Iyakushokuhinkyoku-Soumuka/vision_1.pdf (accessed on 27 October 2017). (In Japanese)
- Donabedian, A. Evaluating the quality of medical care. Milbank Mem. Fund Q. 1966, 44, 166–206. [Google Scholar] [CrossRef]
- Pharmacist Intermediate Intervention Study (PIIS). Available online: http://piis.skr.jp/public.health/home.html (accessed on 25 January 2018). (In Japanese).
- Japanese Society for Applied Therapeutics. Available online: http://www.applied-therapeutics.org (accessed on 25 January 2018). (In Japanese).
- Alliance of Pharmacy Executives. Available online: http://yakukeiren.com (accessed on 25 January 2018). (In Japanese).

| Category | Potential Problems | Pharmacist Intervention (Suggestion or Recommendation) | Patient Outcomes |
|---|---|---|---|
| 1. Medication Use | |||
| Forget to take medicine when eating out | Keep some tablets in the bag constantly | Adherence was improved. | |
| Forget to take medicine when busy with work | Put the medicine in a conspicuous place Notice that the medicine could be taken also before eating | Adherence was improved. | |
| 2. Concerns | |||
| High blood sugar level despite efforts | Wait for the result of the next health check-up, and consider the possibility of hyperglycemia after a meal, as the current average blood sugar level is still better than before | The blood sugar level fell to the normal range on the next measurement. | |
| Blood pressure variation (low in the morning and high in the night) | Receive counseling from the family doctor | Concern disappeared after hearing that it was not necessary to mind this. | |
| 3. Physical Complaint | |||
| Chest ache after exercise | Get medical consultation for angina pectoris fear | The patient underwent detailed examination and was diagnosed and operated on for angina pectoris. | |
| Dizziness | Drink more water or tea because of possible side effect | Dizziness disappeared after several weeks. | |
| 4. Others | |||
| No interest in the results of the health check | Promote health education | The patient became interested in the value of health check-ups (e.g., purchased books); motivation to receive medical treatment increased. | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akazawa, M.; Mikami, A.; Tamura, Y.; Yanagi, N.; Yamamura, S.; Ogata, H. Establishing a Pharmacy-Based Patient Registry System: A Pilot Study for Evaluating Pharmacist Intervention for Patients with Long-Term Medication Use. Pharmacy 2018, 6, 12. https://doi.org/10.3390/pharmacy6010012
Akazawa M, Mikami A, Tamura Y, Yanagi N, Yamamura S, Ogata H. Establishing a Pharmacy-Based Patient Registry System: A Pilot Study for Evaluating Pharmacist Intervention for Patients with Long-Term Medication Use. Pharmacy. 2018; 6(1):12. https://doi.org/10.3390/pharmacy6010012
Chicago/Turabian StyleAkazawa, Manabu, Akiko Mikami, Yuri Tamura, Natsuyo Yanagi, Shinichi Yamamura, and Hiroyasu Ogata. 2018. "Establishing a Pharmacy-Based Patient Registry System: A Pilot Study for Evaluating Pharmacist Intervention for Patients with Long-Term Medication Use" Pharmacy 6, no. 1: 12. https://doi.org/10.3390/pharmacy6010012





