Pharmacists as Interprofessional Collaborators and Leaders through Clinical Pathways
Abstract
:1. Introduction
2. Materials and Methods
2.1. Development of Pathway Team and Pharmacy Team
2.2. Perspectives of the Pharmacy Team
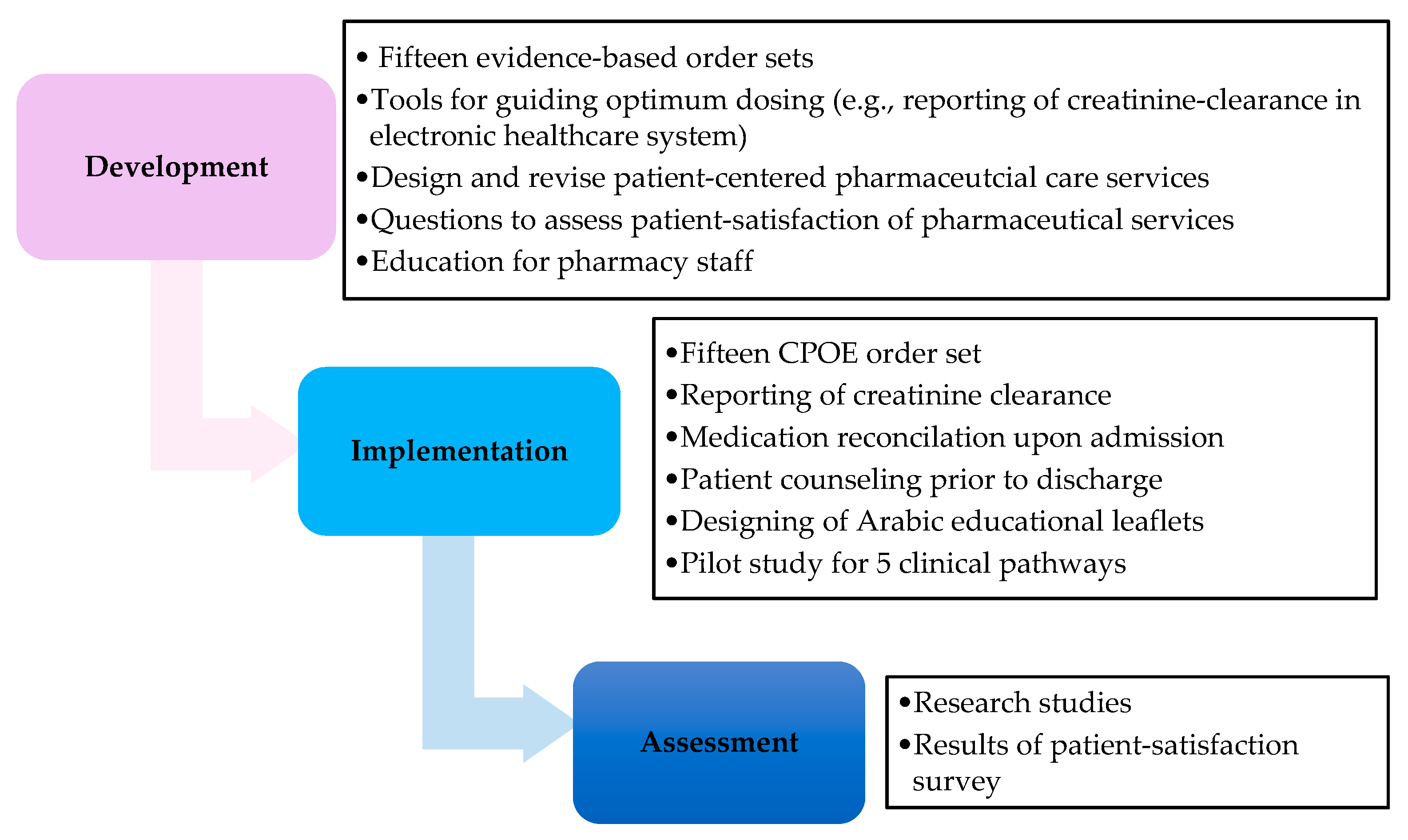
2.3. The Development Phase
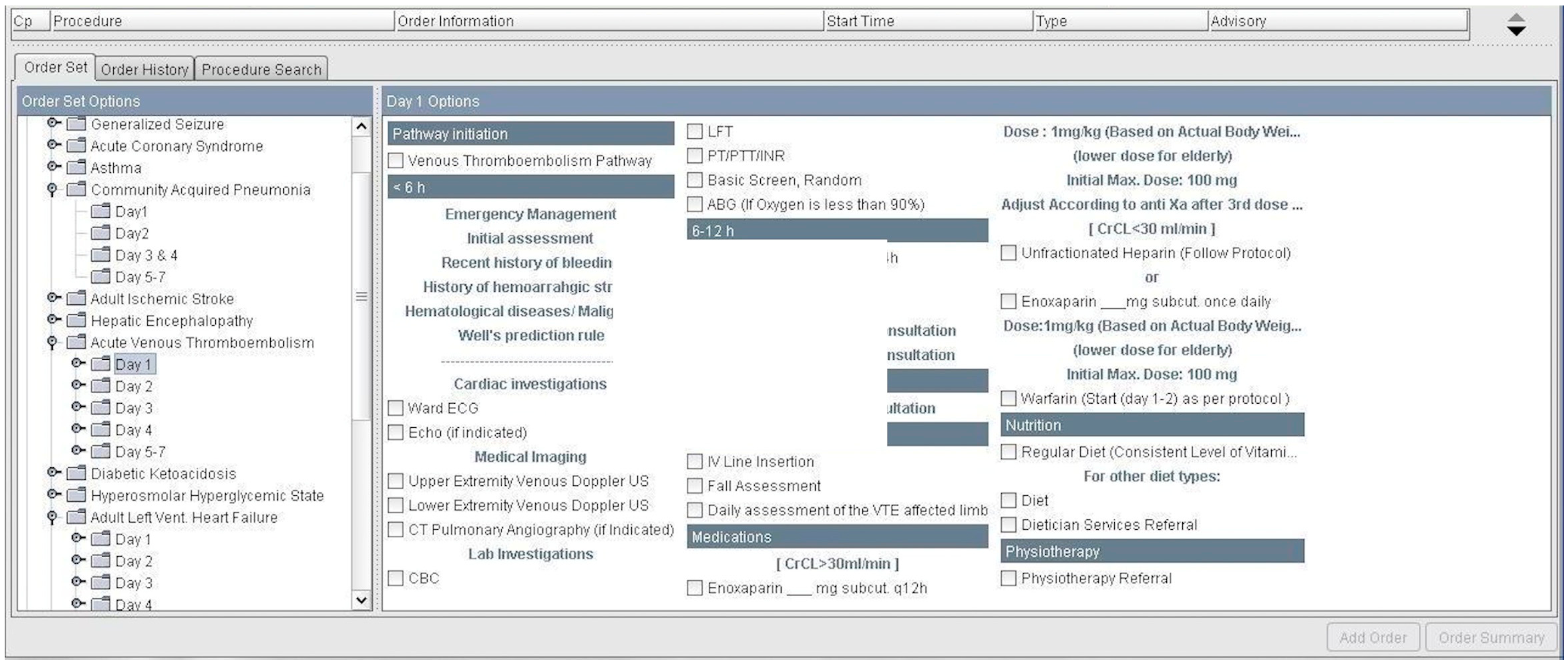
2.3.1. Order Sets
2.3.2. Patient-Centered Pharmaceutical Care Services
2.3.3. Tools
2.3.4. Research Opportunities
Statistical Analyses
Ethics
3. Results
3.1. Implementation
3.1.1. Order Sets
3.1.2. Patient-Centered Pharmaceutical Care Services
3.1.3. Tools
3.1.4. Research
3.2. Assessment
3.2.1. Pilot Study for Validation of Patient-Satisfaction Survey
3.2.2. Patient-Satisfaction Survey
3.2.3. Continuous Education
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Saseen, J.J.; Ripley, T.L.; Bondi, D.; Burke, J.M.; Cohen, L.J.; McBane, S.; McConnell, K.J.; Sackey, B.; Sanoski, C.; Simonyan, A.; et al. ACCP clinical pharmacist competencies. Pharmacotherapy 2017, 37, 630–636. [Google Scholar] [CrossRef] [PubMed]
- American Society of Health-System Pharmacists. ASHP guidelines on a standardized method for pharmaceutical care. Am. J. Health Syst. Pharm. 1996, 53, 1713–1716. [Google Scholar]
- Jaggers, L.D. Differentiation of critical pathways from other health care management tools. Am. J. Health Syst. Pharm. 1996, 53, 311–313. [Google Scholar] [PubMed]
- Petitta, A. Assessing the value of pharmacists’ health-systemwide services: Clinical pathways and treatment guidelines. Pharmacotherapy 2000, 20, 327s–332s. [Google Scholar] [CrossRef] [PubMed]
- Campbell, H.; Hotchkiss, R.; Bradshaw, N.; Porteous, M. Integrated care pathways. BMJ 1998, 316, 133–137. [Google Scholar] [CrossRef] [PubMed]
- European Pathway Association (EPA). Care Pathways. Available online: http://e-p-a.Org/care-pathways (accessed on 14 May 2016).
- Hipp, R.; Abel, E.; Weber, R.J. A primer on clinical pathways. Hosp. Pharm. 2016, 51, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Kinsman, L.; Rotter, T.; James, E.; Snow, P.; Willis, J. What is a clinical pathway? Development of a definition to inform the debate. BMC Med. 2010, 8, 31. [Google Scholar] [CrossRef] [PubMed]
- Rotter, T.; Kinsman, L.; James, E.; Machotta, A.; Willis, J.; Snow, P.; Kugler, J. The effects of clinical pathways on professional practice, patient outcomes, length of stay, and hospital costs: Cochrane systematic review and meta-analysis. Eval. Health Prof. 2012, 35, 3–27. [Google Scholar] [CrossRef] [PubMed]
- Rotter, T.; Kugler, J.; Koch, R.; Gothe, H.; Twork, S.; van Oostrum, J.; Steyerberg, E. A systematic review and meta-analysis of the effects of clinical pathways on length of stay, hospital costs and patient outcomes. BMC Health Serv. Res. 2008, 8, 265. [Google Scholar] [CrossRef] [PubMed]
- Kirk, J.K.; Michael, K.A.; Markowsky, S.J.; Restino, M.R.; Zarowitz, B.J. Critical pathways: The time is here for pharmacist involvement. American college of clinical pharmacy. Pharmacotherapy 1996, 16, 723–733. [Google Scholar] [PubMed]
- American Society of Health-System Pharmacists. ASHP guidelines on the pharmacist’s role in the development, implementation, and assessment of critical pathways. Am. J. Health Syst. Pharm. 2004, 61, 939–945. [Google Scholar]
- Dobesh, P.P.; Bosso, J.; Wortman, S.; Dager, W.E.; Karpiuk, E.L.; Ma, Q.; Zarowitz, B.J. Critical pathways: The role of pharmacy today and tomorrow. Pharmacotherapy 2006, 26, 1358–1368. [Google Scholar] [CrossRef] [PubMed]
- American Society of Health-System Pharmacists. ASHP–SHM joint statement on hospitalist–pharmacist collaboration. Am. J. Health Syst. Pharm. 2008, 65, 260–263. [Google Scholar]
- Institute for Safe Medication Practices. ISMP Develops Guidelines for Standard Order Sets. Available online: http://www.Ismp.Org/newsletters/acutecare/articles/20100311.Asp (accessed on 3 February 2018).
- Best Possible Medication History Interview Guide. Available online: https://www.Ismp-canada.Org/download/medrec/shn_medcard_09_en.Pdf (accessed on 14 February 2018).
- American Society of Health-System Pharmacists. ASHP statement on the pharmacist’s role in medication reconciliation. Am. J. Health Syst. Pharm. 2013, 70, 453–456. [Google Scholar]
- Maclean, L.G. Patient consultation in the cycle of patient care. In Pharmacy Practice Manual: A Guide to the Clinical Experience, 3rd ed.; Stein, S.M., Ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2010; pp. 566–577. [Google Scholar]
- American Society of Health-System Pharmacists. ASHP guidelines on pharmacist-conducted patient education and counseling. Am. J. Health Syst. Pharm. 1997, 54, 431–434. [Google Scholar]
- Fields, W.; Tedeschi, C.; Foltz, J.; Myers, T.; Heaney, K.; Bosak, K.; Rizos, A.; Snyder, R. Reducing preventable medication safety events by recognizing renal risk. Clin. Nurse Spec. 2008, 22, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, A.L.; Henriksen, D.P.; Marinakis, C.; Hellebek, A.; Birn, H.; Nybo, M.; Sondergaard, J.; Nymark, A.; Pedersen, C. Drug dosing in patients with renal insufficiency in a hospital setting using electronic prescribing and automated reporting of estimated glomerular filtration rate. Basic Clin. Pharmacol. Toxicol. 2014, 114, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Ismail, S.; Khalil, M.; Hafez, J.; Yusuf, O.; Thomson, J.; Sidiqui, M.; Quadri, K.M. The Genesis of the Champ-Path: Pragmatic rcts Methodology. PPCR 2017, 3. Available online: http://ppcr.org/journal/index.php/ppcrjournal/article/view/66 (accessed on 1 February 2018).
- Almalki, A.H.; Ismail, S.E.; Qureshi, M.A.; Abunijem, Z.; Balla, M.E.; Karsou, S.; Qureshi, R.A.; Ahmad, A.; AlSulami, S.; Khalil, M.; et al. A pragmatic randomized controlled trial comparing pathway-based versus usual care in community-acquired acute kidney injury. Saudi J. Kidney Dis Transpl. 2017, 28, 1282–1292. [Google Scholar] [CrossRef] [PubMed]
- Okumura, L.M.; Rotta, I.; Correr, C.J. Assessment of pharmacist-led patient counseling in randomized controlled trials: A systematic review. Int. J. Clin. Pharm. 2014, 36, 882–891. [Google Scholar] [CrossRef] [PubMed]
- Abdulghani, K.H.; Aseeri, M.A.; Mahmoud, A.; Abulezz, R. The impact of pharmacist-led medication reconciliation during admission at tertiary care hospital. Int. J. Clin. Pharm. 2017. [Google Scholar] [CrossRef] [PubMed]
- Mekonnen, A.B.; McLachlan, A.J.; Brien, J.A. Effectiveness of pharmacist-led medication reconciliation programmes on clinical outcomes at hospital transitions: A systematic review and meta-analysis. BMJ Open 2016, 6, e010003. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, K.E.; Zwarenstein, M.; Oxman, A.D.; Treweek, S.; Furberg, C.D.; Altman, D.G.; Tunis, S.; Bergel, E.; Harvey, I.; Magid, D.J.; et al. A pragmatic-explanatory continuum indicator summary (precis): A tool to help trial designers. CMAJ 2009, 180, E47–E57. [Google Scholar] [CrossRef] [PubMed]
- Zwarenstein, M.; Treweek, S.; Gagnier, J.J.; Altman, D.G.; Tunis, S.; Haynes, B.; Oxman, A.D.; Moher, D. Improving the reporting of pragmatic trials: An extension of the consort statement. BMJ 2008, 337, a2390. [Google Scholar] [CrossRef] [PubMed]
- Bridges, D.R.; Davidson, R.A.; Odegard, P.S.; Maki, I.V.; Tomkowiak, J. Interprofessional collaboration: Three best practice models of interprofessional education. Med. Educ. Online 2011, 16, 95–106. [Google Scholar] [CrossRef] [PubMed]
|
| Pharmaceutical Care (الرعاية الصيدلانية) | Responses | ||||
|---|---|---|---|---|---|
| 1 Did the Pharmacist review your home medication within 24 h of admission? هل راجع الصيدلي أدويتك الخاصة بك التى تتناولها بالمنزل خلال 24 ساعة من تنويمك؟ | Yes ( نعم ) □ | No ( لا ) □ | |||
| 2 Did you receive counseling by the Pharmacist on your medications before discharge? هل حصلت على معلومات خاصة بادويتك من الصيدلي قبل خروجك من المستشفى؟ | Yes ( نعم ) □ | No ( لا ) □ | |||
 |  |  |  |  | |
| Excellent | Very Good | Good | Poor | Unsatisfactory | |
| ممتا ز | جيد جدا | جيد | ضعيف | غير مقبول | |
| 3 How would you describe the process of reviewing your home medication with the Pharmacist upon admission? كيف تصف طريقة مراجعة أدويتك الخاصة مع الصيدلي عند التنويم؟ | □ | □ | □ | □ | □ |
| 4 How would you best describe your level of understanding about your medications based on the educational information you received from your pharmacist before discharge? كيف تصف مستوى فهمك للأدوية الخاصة بك حسب التعليمات التي تلقيتها من الصيدلي قبل خروجك من المستشفى؟ | □ | □ | □ | □ | □ |
| 5 How would you best describe the overall performance of the pharmaceutical services provided during your stay in hospital? كيف تصف الأداء العام للخدمات الصيدلانية المقدمة خلال إقامتك في المستشفى؟ | □ | □ | □ | □ | □ |
| Pharmaceutical Care | الرعاية الصيدلانية | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | Did the Pharmacist review your home medications? | Yes | □ | نعم | هل راجع الصيدلي أدويتك التى تتناولها بالمنزل؟ | ١ـ | ||
| No | □ | لا | ||||||
 |  |  |  |  | ||||
| جيد جدا | جيدا | محايد | ضعيف | ضعيف جدا | ||||
| Very Good | Good | Neutral | Poor | Very Poor | ||||
| 2 | How would you rate the process of reviewing your home medication with the Pharmacist upon admission? | □ | □ | □ | □ | □ | ما هو تقييمك لطريقة مراجعة أدويتك مع الصيدلي عند دخولك في المستشفى؟ | ٢ـ |
| Did not Review | □ | لم يراجع أدويتي | ||||||
| 3 | Has the pharmacist counseled you on the medications, which you will be taking home with you? | Yes | □ | نعم | هل نصحك الصيدلي عن الأدوية التي ستأخذ معك إلى المنزل؟ | ٣ـ | ||
| No | □ | لا | ||||||
| Not Applicable | □ | لا ينطبق | ||||||
| (Discharged after-hours) | ||||||||
 |  |  |  |  | ٤ـ | |||
| فهمت تماما | فهمت كثيرا | فهمت نوعا ما | فهمت قليلا | لم أفهم | ||||
| Completely understood | Understood a lot | Understood somewhat | Understood a little | Did not understand | ||||
| 4 | How would you rate your level of understanding about your medications based on the educational information you received from your pharmacist before discharge? | □ | □ | □ | □ | □ | ما هو تقييمك لمستوى فهمك للأدوية الخاصة بك حسب التعليمات التي تلقيتها من الصيدلي قبل خروجك من المستشفى؟ | -٥ |
| No Information | □ | لم أتلق أي معلومات | ||||||
 |  |  |  |  | ||||
| جيد جيد جدا | جيد ا | محايد | ضعيف | ضعيف جدا | ||||
| Very Good | Good | Neutral | Poor | Very Poor | ||||
| 5 | How would you rate the overall performance of the pharmaceutical services provided during your stay in hospital? | □ | □ | □ | □ | □ | ما هو تقييمك عموما للخدمات الصيدلية المقدمة خلال إقامتك في المستشفى؟ | ٦ـ |
| Questions | Responses | Proportions n/N (%) | 95% Confidence Intervals | |
|---|---|---|---|---|
| Medication Reconciliation upon admission | ||||
| 1 | Received medication reconciliation by pharmacist | Yes | 119/166 (71.7) | 64.8–78.6 |
| 2 | Evaluation of Medication reconciliation by pharmacist | Did not review | 49/159 (30.8) | 23.6–38.0 |
| Poor a | 20/159 (12.6) | 7.4–17.8 | ||
| Good b | 90/159 (56.6) | 48.9–64.3 | ||
| Patient counseling before discharge | ||||
| 3 | Received counseling by pharmacist | Yes | 102/147 (69.4) | 62.0–76.8 |
| Not applicable c | 28/147 (19.0) | 12.7–25.3 | ||
| 4 | Level of understanding about medications based on counseling by pharmacist | No information provided | 14/145 (9.7) | 4.9–14.5 |
| Poor understanding d | 5/145 (3.4) | 0.5–6.3 | ||
| Good understanding e | 126/145 (86.9) | 81.4–92.4 | ||
| Overall performance of Pharmaceutical Services | ||||
| 5 | Evaluation of overall performance of the pharmaceutical services provided | Poor a | 38/144 (26.4) | 19.2–33.6 |
| Good b | 106/144 (73.6) | 66.4–80.8 | ||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ismail, S.; Osman, M.; Abulezz, R.; Alhamdan, H.; Quadri, K.H.M. Pharmacists as Interprofessional Collaborators and Leaders through Clinical Pathways. Pharmacy 2018, 6, 24. https://doi.org/10.3390/pharmacy6010024
Ismail S, Osman M, Abulezz R, Alhamdan H, Quadri KHM. Pharmacists as Interprofessional Collaborators and Leaders through Clinical Pathways. Pharmacy. 2018; 6(1):24. https://doi.org/10.3390/pharmacy6010024
Chicago/Turabian StyleIsmail, Sherine, Mohamed Osman, Rayf Abulezz, Hani Alhamdan, and K. H. Mujtaba Quadri. 2018. "Pharmacists as Interprofessional Collaborators and Leaders through Clinical Pathways" Pharmacy 6, no. 1: 24. https://doi.org/10.3390/pharmacy6010024






