Strengthening the Referral System through Social Capital: A Qualitative Inquiry in Ghana
Abstract
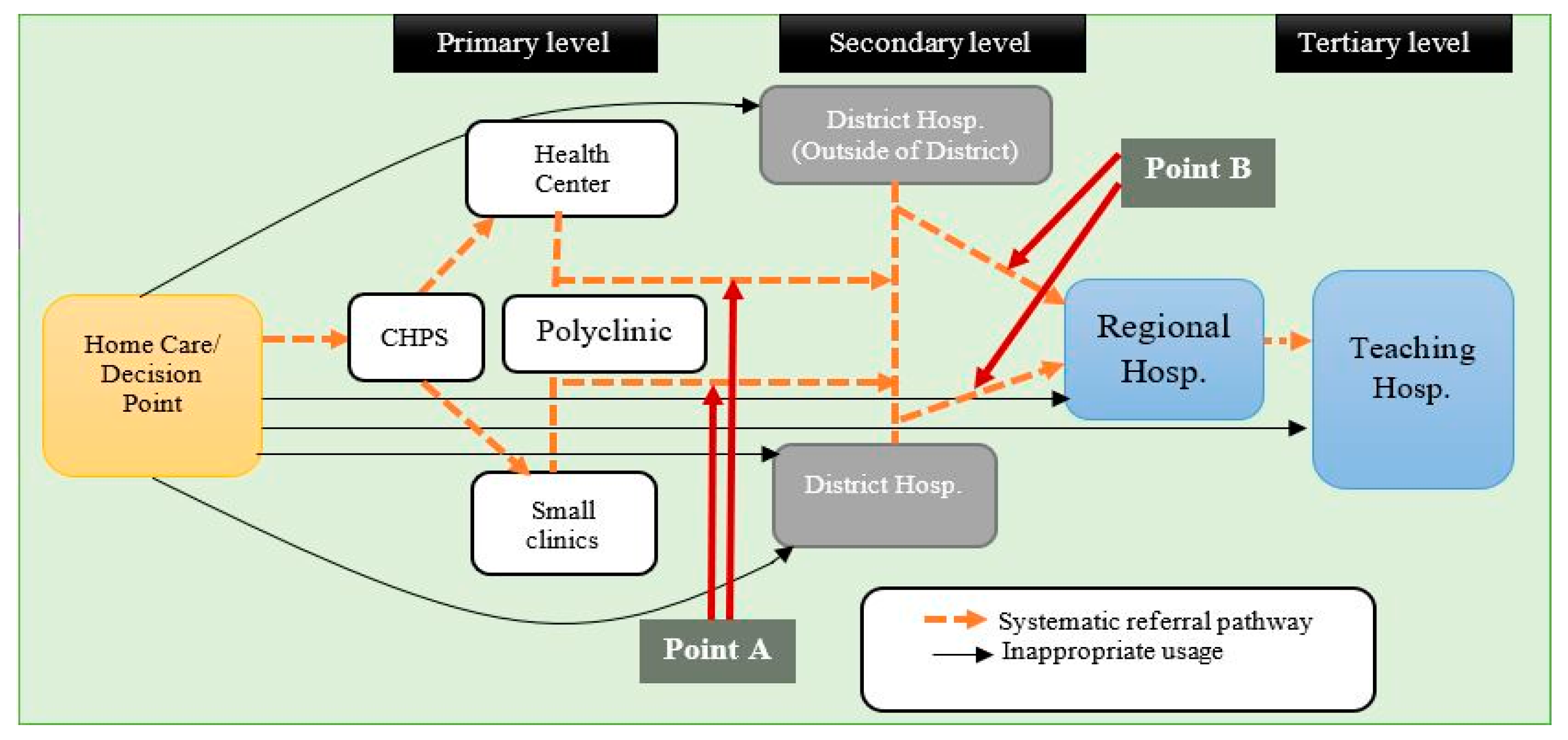
:1. Background
2. Methods
2.1. Study Design
2.2. Data Collection and Sampling
2.3. Data Analysis
3. Findings
…Some patients and their relatives occasionally resist referral. …Usually, the patients would say they are scared to go to a higher-level facility. …When you refer a patient to Komfo Anokye (tertiary hospital), they may eventually go, but first, they would insist that they want to stay here for the same treatment. …They consider that going to Komfo Anokye means that one has a serious ailment and is on the verge of dying. …We have to spend time to convince them of the fact that the receiving facility is better equipped to handle their situation. …Many do not understand the referral processes (Health officer 3, urban)
3.1. Bonding Social Capital Determined Choice of Health Facilities
I often ask for help on where to seek medical help. …I mostly discuss it with my friends. …when I am not feeling well, I just tell them about how I am feeling. Usually, one of them will either recommend drugs for me or direct me to a good health facility to seek medical care (Ibrah, 50 years, urban)
…When my child was sick, a lot of that happened. …Many people suggested different health centres to me. …Some asked me to go to Suntreso hospital [District hospital] …and Komfo Anokye [teaching hospital] …They went like …’This place is right, the new doctor is very good’. …Eventually, I took her to the Ejisu (District Hospital) for treatment. …It worked for me (Naa, 40 years, rural)
3.2. Linking Social Capital Persuaded People to Abandon the Referral Policy
…Every person needs to have a doctor or nurse as a friend so that in times of sickness, you can contact them for help. …I have a nurse as a friend …and I talk to her about my health. …She sometimes arranges for me to see specialist doctors at Komfo Anokye (tertiary hospital) (Akua, 42 years, urban)
3.3. Bridging Social Capital Protected Against Misuse of the Referral Policy
My child fell sick for a while after I gave birth. I was referred from Foase (secondary hospital) to KATH (tertiary hospital). …I decided to go, but I realised that I did not have enough money. …I used the little money on me to get blood tonics for the child, but her condition did not improve after a while. …Later, one of my friends led me to acquire a loan from someone she knew. …I was then able to take him to the KATH (Akua, 35 years, rural)
…When someone is referred to Foase (District hospital), and there is no car immediately, the men in the community organise themselves to carry the person to the hospital if he or she is not able to find a car after waiting for a while. …If the men do not help, then the patient would have to wait until the next day. …However, in all the cases that I have witnessed here, people were always ready to help once the patients and their families expressed the willingness to honour the referral (Health officer 2, rural)
3.4. Social Norms and Adherence to the Referral Policy
Some time ago, a woman in labour had complications at the CHPS compound at Sanyeneso No.3. …The attendant handled the case, but she encountered some complications. …The patient had a retained placenta. …The nurse immediately asked those who brought the woman to the clinic to take her to another hospital. …She gave them a referral note as well. …Instead of taking her to the hospital, they took the patient home and asked her to blow air into a bottle to force her placenta out. …There is a perception that blowing air forcefully into a bottle could pressure out the placenta in such situations. She bled profusely and died eventually (Health officer 2, rural).
The people know we do not treat such cases (diseases attributed to spiritual causes) here, so they take to the fetish priest for (spiritual) treatment. …Sometimes, the fetish priest consults us for assistance when he feels that the patient could use orthodox medical care whiles he continues with his spiritual work. …He sometimes asks us to treat his clients with wounds and severe cuts at his premises. …The relatives of the sick only consider our services if the fetish priest recommends it (Health officer 1, rural)
3.5. Trust Influenced Adherence to the Referral Policy
I always used to attend antenatal and postnatal services at Ejisu hospital, but now I use the clinic in the community (CHPS compound). …This is the only time I am using this facility (CHPS compound). ...This time, when I first realised that I was pregnant, I asked my sister-in-law who has been using the clinic here. …She told me the service is the same as that of Ejisu. …That was when I decided to visit this clinic (CHPS) (Naa, 40 years, rural).
Yes, I live here (Fori), but I go to Abuk (a place at the other end of the city) for healthcare. …I used to visit one clinic (a primary level facility) here, but I stopped. …Everyone in my house uses a facility at Abuk (secondary level facility), and none of them has ever complained about anything, so I decided to go there as well. …I felt that the facility at Abuk may be better than the one here (Victor, 32 years, urban).
No, personally I do not share my health issues with other people except it is something that overwhelms me. I do not usually ask anybody about where to seek medical attention. …I only open up to discuss my health issues with people I consider as trustworthy and knowledgeable (Faust, 38 years, rural).
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Gros, J.-G. Healthcare Policy in Africa: Institutions and Politics from Colonialism to the Present; Rowman and Littlefield: Lanham, MD, USA, 2016. [Google Scholar]
- Saleh, K. The Health Sector in Ghana: A Comprehensive Assessment; The World Bank: Washington, DC, USA, 2013. [Google Scholar]
- Gyapong, J.; Garshong, B.; Akazili, J.; Aikins, M.; Agyepong, I.; Nyonator, F. Critical Analysis of Ghana’s Health System: With a Focus on Equity Challenges and the National Health Insurance; University of Cape Town (UCT): Cape Town, South Africa, 2007. [Google Scholar]
- Abor, P.A.; Abekah-Nkrumah, G.; Abor, J. An examination of hospital governance in Ghana. Leadersh. Health Serv. 2008, 21, 47–60. [Google Scholar] [CrossRef]
- GHS. Ghana Health Service 2014 Annual Report; Ghana Health Service: Accra, Ghana, 2015. [Google Scholar]
- GHS. Quality Assurance Strategy Plan for Ghana Health Service 2007–2011; Ghana Health Service: Accra, Ghana, 2007. [Google Scholar]
- MoH. Referral Policy and Guidelines; Ministry of Health (MoH), Ghana: Accra, Ghana, 2012.
- WHO. Management of Health Facilities: Referral Systems. Available online: http://www.who.int/management/facility/referral/en/ (accessed on 15 May 2017).
- BASICS II; GHS. The Status of Referrals in Three Districts in Ghana: Analysis of Referral Pathways for Children under Five; The Basic Support for Institutionalizing Child Survival Project (BASICS II) for the United States Agency for International Development, and Ghana Health Service: Arlington, VA, USA, 2003. [Google Scholar]
- Awoonor-Williams, J.K.; Bailey, P.E.; Yeji, F.; Adongo, A.E.; Baffoe, P.; Williams, A.; Mercer, S. Conducting an audit to improve the facilitation of emergency maternal and newborn referral in northern Ghana. Glob. Public Health 2015, 10, 1118–1133. [Google Scholar] [CrossRef] [PubMed]
- Nanyonjo, A.; Bagorogoza, B.; Kasteng, F.; Ayebale, G.; Makumbi, F.; Tomson, G.; Källander, K. Estimating the cost of referral and willingness to pay for referral to higher-level health facilities: A case series study from an integrated community case management programme in Uganda. BMC Health Serv. Res. 2015, 15, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hongoro, C.; Musonza, T.G.; Macq, J.; Anozie, A. A qualitative assessment of the referral system at district level in Zimbabwe: Implications on efficiency and effective delivery of health services. Cent. Afr. J. Med. 1998, 44, 93–97. [Google Scholar] [PubMed]
- Abimbola, S.; Ukwaja, K.N.; Onyedum, C.C.; Negin, J.; Jan, S.; Martiniuk, A.L.C. Transaction costs of access to health care: Implications of the care-seeking pathways of tuberculosis patients for health system governance in Nigeria. Glob. Public Health 2015, 10, 1060–1077. [Google Scholar] [CrossRef] [PubMed]
- Phillips, D.R. Health and Health Care in the Third World; Longman Group UK Limited: London, UK, 1990. [Google Scholar]
- Halpern, D. Social Capital; Polity Press: Cambridge, UK, 2005. [Google Scholar]
- Putland, C.; Baum, F.; Ziersch, A.; Arthurson, K.; Pomagalska, D. Enabling pathways to health equity: Developing a framework for implementing social capital in practice. BMC Public Health 2013, 13, 517. [Google Scholar] [CrossRef] [PubMed]
- Ogden, J.; Morrison, K.; Hardee, K. Social capital to strengthen health policy and health systems. Health Policy Plan. 2013. [Google Scholar] [CrossRef] [PubMed]
- Lin, N. Social Capital: Critical Concepts in the Social Sciences; Lin, N., Ed.; Routledge: London, UK, 2011; Volume I. [Google Scholar]
- Bourdieu, P. The Forms of Capital. In Handbook of Theory and Research for the Sociology of Education; Richardson, G., Ed.; Greenwood Press: New York, NY, USA, 1986. [Google Scholar]
- Putnam, R.D. Tuning In, Tuning Out: The Strange Disappearance of Social Capital in America. Political Sci. Politics 1995, 28, 664–683. [Google Scholar] [CrossRef]
- Harpham, T. The measurement of community social capital through surveys. In Social Capital and Health; Kawachi, I., Subramanian, S.V., Kim, D., Eds.; Springer: New York, NY, USA, 2008; pp. 51–62. [Google Scholar]
- Ostrom, E. Social Capital: A Fad or a Fundamental Concept? In Social Capital: A Multifaceted Perspective; Dasgupta, P., Serageldin, I., Eds.; World Bank: Washington, DC, USA, 2000; pp. 172–214. [Google Scholar]
- Edwards, B.; Foley, M. Civil society and social capital beyond Putnam. Am. Behav. Sci. 1998, 42, 124–132. [Google Scholar] [CrossRef]
- Van Vugt, M.; Hart, C.M. Social identity as social glue: The origins of group loyalty. J. Personal. Soc. Psychol. 2004, 86, 585–598. [Google Scholar] [CrossRef] [PubMed]
- Freidson, E. Client control and medical practice. Am. J. Sociol. 1960, 654, 374–382. [Google Scholar] [CrossRef]
- Freidson, E. Patient’s View of Medical Practice; Russel Sage: New York, NY, USA, 1961. [Google Scholar]
- Clarke, A. The Sociology of Healthcare; Pearson Education Limited: Essex, UK, 2010. [Google Scholar]
- Nettleton, S. The Sociology of Health and Illness; Polity Press: Cambridge, UK, 2013. [Google Scholar]
- Murray, S.F.; Pearson, S.C. Maternity referral systems in developing countries: Current knowledge and future research needs. Soc. Sci. Med. 2006, 62, 2205–2215. [Google Scholar] [CrossRef] [PubMed]
- Sakeah, E.; McCloskey, L.; Bernstein, J.; Yeboah-Antwi, K.; Mills, S.; Doctor, H.V. Is there any role for community involvement in the community-based health planning and services skilled delivery program in rural Ghana? BMC Health Serv. Res. 2014, 14, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Aikins, A.D.-G. Healer shopping in Africa: New evidence from rural-urban qualitative study of Ghanaian diabetes experiences. BMJ 2005, 331, 737. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aryeetey, R.N.O.; Aikins, M.; Gyeke-Dako, P.; Adongo, P.B. Pathways utilised for antenatal health seeking among women in the Ga East District, Ghana. Ghana Med. J. 2015, 49, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Bakare, M.O. Pathway to care: First points of contact and sources of referral among children and adolescent patients seen at neuropsychiatric hospital in south-eastern Nigeria. Niger. J. Med. 2013, 22, 52–56. [Google Scholar] [PubMed]
- Sheikh, M.R.; Ali, S.Z.; Hussain, A.; Shehzadi, R.; Afzal, M.M. Measurement of social capital as an indicator of community-based initiatives (CBI) in the Islamic Republic of Iran. J. Health Organ. Manag. 2009, 23, 429–441. [Google Scholar] [CrossRef] [PubMed]
- Bryman, A. Social Research Methods, 4th ed.; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Angen, M.J. Evaluating interpretive inquiry: Reviewing the validity debate and opening the dialogue. Qual. Health Res. 2000, 10, 378–395. [Google Scholar] [CrossRef] [PubMed]
- Ansah, E.K.; Gyapong, M.; Narh-Bana, S.; Bart-Plange, C.; Whitty, C.J.M. Factors influencing choice of care-seeking for acute fever comparing private chemical shops with health centres and hospitals in Ghana: A study using case–control methodology. Malar. J. 2016, 15, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Febir, L.G.; Asante, K.P.; Afari-Asiedu, S.; Abokyi, L.N.; Kwarteng, A.; Ogutu, B.; Gyapong, M.; Owusu-Agyei, S. Seeking treatment for uncomplicated malaria: Experiences from the Kintampo districts of Ghana. Malar. J. 2016, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Turkson, P.K. Perceived Quality of Healthcare Delivery in a Rural District of Ghana. Ghana Malar. J. 2009, 43, 65–70. [Google Scholar] [CrossRef]
- Gupta, M.L.; Aborigo, R.A.; Adongo, P.B.; Rominski, S.; Hodgson, A.; Engmann, C.M.; Moyer, C.A. Grandmothers as gatekeepers? The role of grandmothers in influencing health-seeking for mothers and newborns in rural northern Ghana. Glob. Public Health 2015, 10, 1078–1091. [Google Scholar] [PubMed]
- Misztal, B. Trust in Modern Societies: The Search for the Bases of Social Order; John Wiley & Sons: New York, NY, USA, 2013. [Google Scholar]
- Song, L.; Chang, T.-Y. Do resources of network members help in help seeking? Social capital and health information search. Soc. Netw. 2012, 34, 658–669. [Google Scholar]
- Asampong, E.; Dwuma-Badu, K.; Stephens, J.; Srigboh, R.; Neitzel, R.; Basu, N.; Fobil, J.N. Health seeking behaviours among electronic waste workers in Ghana. BMC Public Health 2015, 15, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Schieber, G.; Cashin, C.; Saleh, K.; Lavado, R. Health Financing in Ghana; The World Bank: Washington, DC, USA, 2012. [Google Scholar]
- Rostila, M. Social Capital and Health Inequality in European Welfare States; Palgrave Macmillan UK: New York, NY, USA, 2013. [Google Scholar]
| Characteristic | Urban (n = 28) | Rural (n =51) | Overall (n = 79) | |||
|---|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | Frequency | Percentage | |
| Sex | ||||||
| Male | 13 | 46.43 | 24 | 47.06 | 37 | 46.84 |
| Female | 15 | 53.57 | 27 | 52.94 | 42 | 53.16 |
| Age | ||||||
| 18–24 | 5 | 17.85 | 7 | 13.72 | 12 | 15.19 |
| 25–34 | 8 | 28.57 | 14 | 27.45 | 22 | 27.85 |
| 35–44 | 8 | 28.57 | 12 | 23.53 | 20 | 25.32 |
| 45–59 | 3 | 10.71 | 12 | 23.53 | 15 | 18.99 |
| 60+ | 4 | 14.29 | 6 | 11.76 | 10 | 12.65 |
| Educational Attainment | ||||||
| Never been to school | 4 | 14.29 | 12 | 23.53 | 16 | 20.25 |
| Primary school | 7 | 25 | 12 | 23.53 | 19 | 24.05 |
| Junior High Sch. | 10 | 35.71 | 14 | 27.45 | 24 | 30.38 |
| Senior High Sch. | 4 | 14.29 | 9 | 17.65 | 13 | 16.46 |
| Tertiary Level | 3 | 10.71 | 4 | 7.84 | 7 | 8.86 |
| Total | 28 | 100 | 51 | 100 | 79 | 100 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amoah, P.A.; Phillips, D.R. Strengthening the Referral System through Social Capital: A Qualitative Inquiry in Ghana. Healthcare 2017, 5, 80. https://doi.org/10.3390/healthcare5040080
Amoah PA, Phillips DR. Strengthening the Referral System through Social Capital: A Qualitative Inquiry in Ghana. Healthcare. 2017; 5(4):80. https://doi.org/10.3390/healthcare5040080
Chicago/Turabian StyleAmoah, Padmore Adusei, and David R. Phillips. 2017. "Strengthening the Referral System through Social Capital: A Qualitative Inquiry in Ghana" Healthcare 5, no. 4: 80. https://doi.org/10.3390/healthcare5040080






