A 40-Day Journey to Better Health: Utilizing the DanielFast to Improve Health Outcomes in Urban Church-Based Settings
Abstract
:1. Introduction
Background
2. Materials and Methods
2.1. Design
2.2. Measures
2.3. Statistical Analyses
3. Results
3.1. Participant Demographics
3.2. Biometric Data
3.3. Blood Pressure Data by Church
3.4. SF-12 across Church and by Church
3.5. Food Choice
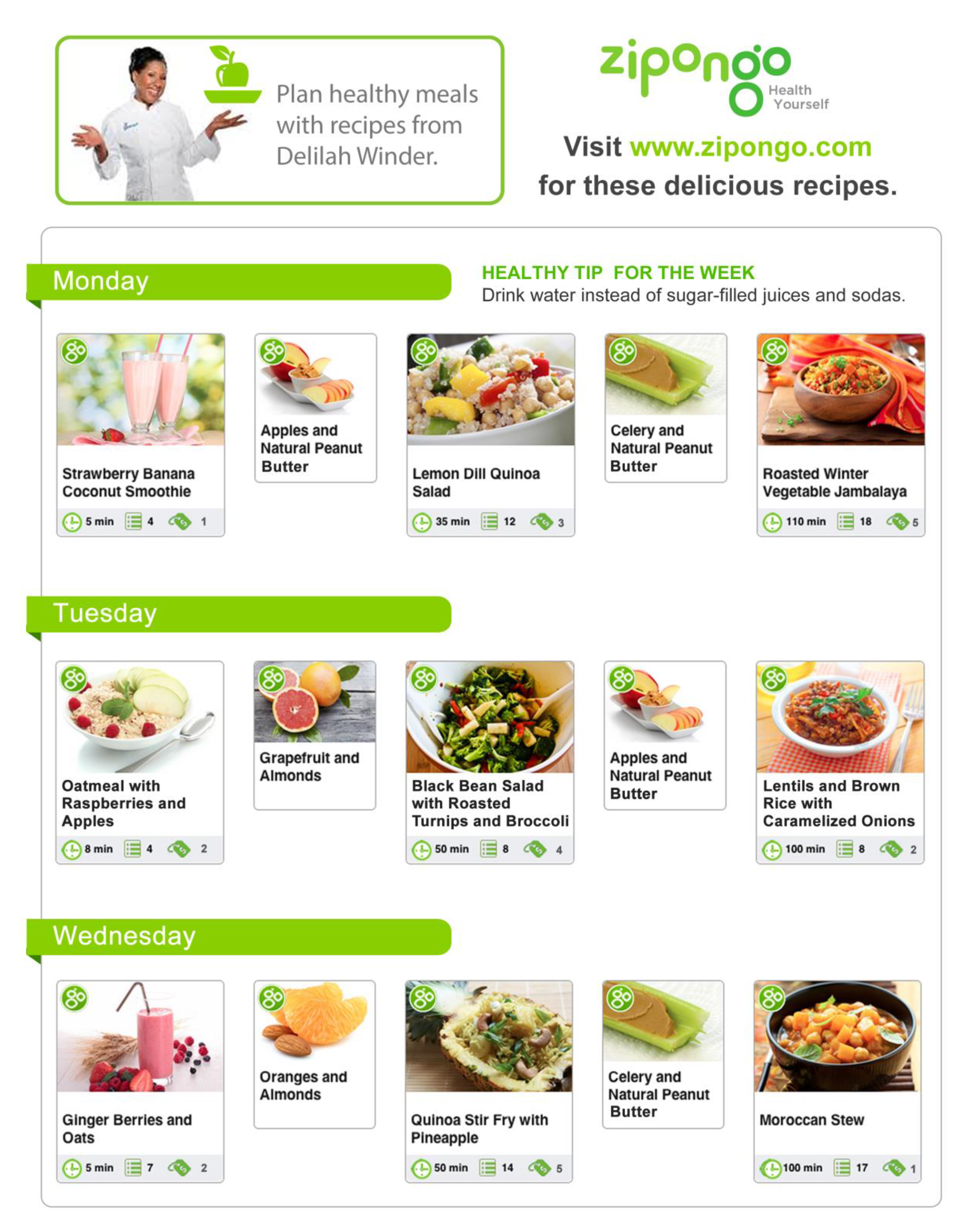
3.6. Zipongo: Digital Engagement for Healthier Eating
4. Discussion
4.1. Program Assessment
4.2. Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ward, B.W.; Schiller, J.S.; Goodman, R.A. Multiple Chronic Conditions Among US Adults: A 2012 Update. Prev. Chronic Dis. 2014, 11, E62. [Google Scholar] [CrossRef] [PubMed]
- Robert Wood Johnson Foundation Chronic Care: Making the Case for Ongoing Care. 2010. Available online: https://www.rwjf.org/en/library/research/2010/01/chroniccare.html (accessed on 23 June 2014).
- Johns Hopkins Bloomberg, School of Public Health. Centers for Disease Control and Prevention C. NCHS Data on Obesity. 2013. Available online: http://www.cdc.gov/nchs/data/factsheets/factsheet_obesity.htm (accessed on 23 June 2014).
- Go, A.S.; Mozaffarian, D.; Roger, V.L.; Benjamin, E.J.; Berry, J.D.; Blaha, M.J.; Dai, S.; Ford, E.S.; Fox, C.S.; Franco, S.; et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2014 update: A report from the American Heart Association. Circulation 2014, 129, e28. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, E.A.; Trogdon, J.G.; Cohen, J.W.; Dietz, W. Annual medical spending attributable to obesity: Payer-and service-specific estimates. Health Aff. 2009, 28, W822–W831. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention National Diabetes Statistics Report. Available online: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf (accessed on 1 November 2017).
- Field, A.E.; Coakley, E.H.; Must, A.; Spadano, J.L.; Laird, N.; Dietz, W.H.; Rimm, E.; Colditz, G.A. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch. Intern. Med. 2001, 161, 1581–1586. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Chronic Disease Prevention and Health Promotion: Racial and Ethnic Approaches to Community Health (REACH). Available online: https://www.cdc.gov/chronicdisease/resources/publications/aag/reach.htm (accessed on 29 November 2016).
- Centers for Disease Control and Prevention: Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. Available online: https://www.cdc.gov/nchs/products/databriefs/db288.htm (accessed on 1 November 2017).
- Centers for Disease Control and Prevention Vital Signs: African American Health. Available online: https://www.cdc.gov/vitalsigns/aahealth/index.html (accessed on 3 July 2017).
- Philadelphia Department of Public Health. Community Health Assessment, Philadelphia, PA. In Health; Philadelphia Department of Public Health: Philadelphia, PA, USA, 2013. Available online: http://www.phila.gov/health/pdfs/chareport_52114_final.pdf (accessed on 15 May 2014).
- The Daniel Fast. Available online: http://www.daniel-fast.com/ (accessed on 23 June 2014).
- Bloomer, R.J.; Kabir, M.M.; Trepanowski, J.F.; Canale, R.E.; Farney, T.M. A 21 day Daniel Fast improves selected biomarkers of antioxidant status and oxidative stress in men and women. Nutr. Metab. 2011, 8, 17. [Google Scholar] [CrossRef] [PubMed]
- Bloomer, R.; Kabir, M.M.; Canale, R.E.; Trepanowski, J.F.; Marshall, K.E.; Farney, T.M.; Hammond, K.G. Effect of a 21 day Daniel Fast on metabolic and cardiovascular disease risk factors in men and women. Lipids Health Dis. 2010, 9, 94. [Google Scholar] [CrossRef] [PubMed]
- Alleman, R.J.; Harvey, I.C.; Farney, T.M.; Bloomer, R.J. Both a traditional and modified Daniel Fast improve the cardio-metabolic profile in men and women. Lipids Health Dis. 2013, 12, 114. [Google Scholar] [CrossRef] [PubMed]
- Bloomer, R.J.; Gunnels, T.A.; Schriefer, J.M. Comparison of a Restricted and Unrestricted Vegan Diet Plan with a Restricted Omnivorous Diet Plan on Health-Specific Measures. Healthcare 2015, 3, 544–555. [Google Scholar] [CrossRef] [PubMed]
- Trepanowski, J.F.; Bloomer, R.J. The impact of religious fasting on human health. BMC Nutr. 2010, 9. [Google Scholar] [CrossRef] [PubMed]
- Gerber, B.S.; Stolley, M.R.; Thompson, A.L.; Sharp, L.K.; Fitzgibbon, M.L. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: A feasibility study. Health Inform. J. 2009, 15, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, D.M.; Levine, E.L.; Askew, S.; Foley, P.; Bennett, G.G. Daily text messaging for weight control among racial and ethnic minority women: Randomized controlled pilot study. J. Med. Internet Res. 2013, 15. [Google Scholar] [CrossRef]
- Patrick, K.; Raab, F.; Adams, M.A.; Dillon, L.; Zabinski, M.; Rock, C.; Griswold, W.; Norman, G. A text message–based intervention for weight loss: Randomized controlled trial. J. Med. Internet Res. 2009, 11. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Grossman, R.M.; Pinski, R.B.; Patterson, T.L.; Nader, P.R. The development of scales to measure social support for diet and exercise behaviors. Prev. Med. 1987, 16, 825–836. [Google Scholar] [CrossRef]
- Brownson, R.C.; Riley, P.; Bruce, T.A. Demonstration projects in community-based prevention. JPHMP 1998, 4, 66. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Pollard, T.M.; Wardle, J. Development of a measure of the motives underlying the selection of food: The food choice questionnaire. Appetite 1995, 25, 267–284. [Google Scholar] [CrossRef] [PubMed]
- Blomain, E.S.; Dirhan, D.A.; Valentino, M.A.; Kim, G.W.; Waldman, S.A. Mechanisms of Weight Regain following Weight Loss. ISRN Obes. 2013, 2013. [Google Scholar] [CrossRef] [PubMed]
- Burke, L.E.; Wang, J.; Sevick, M.A. Self-monitoring in weight loss: A systematic review of the literature. J. Am. Diet. Assoc. 2011, 111, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.R.; Phelan, S. Long-term weight loss maintenance. Am. J. Clin. Nutr. 2005, 82, 222S–225S. [Google Scholar] [CrossRef] [PubMed]
| Pre-Test Mean (SD) | Post-Test Mean (SD) | df | T-Score | p-Value | |
|---|---|---|---|---|---|
| Weight (lbs) | 210.00 (52.00) | 206.10 (51.96) | 60 | 2.93 | 0.005 * |
| Waist circumference (in) | 41.50 (6.69) | 40.80 (6.38) | 61 | 1.83 | 0.07 |
| BMI (kg/m2) | 34.84 (7.32) | 34.52 (7.56) | 61 | 1.35 | 0.18 |
| Total Cholesterol (mg/dL) | 171.7 (12.02) | 158.8 (30.60) | 62 | 5.17 | 0.0001 * |
| Glucose (mg/dL) | 126.95 (51.30) | 117.60 (35.88) | 61 | 1.81 | 0.071 |
| Systolic BP (mm/Hg) | 134.59 (19.16) | 130.92 (19.05) | 62 | 1.64 | 0.11 |
| Diastolic BP (mm/Hg) | 83.03 (10.56) | 82.76 (10.51) | 62 | 0.18 | 0.86 |
| SF-12 Domain | Pre-Test Mean (SD) | Post-Test Mean (SD) | df | T-Score | p-Value |
|---|---|---|---|---|---|
| Physical functioning | 61.46 (37.58) | 67.71 (36.47) | 23 | 0.97 | 0.34 |
| Role physical | 72.92 (44.18) | 77.08 (38.95) | 23 | 0.46 | 0.65 |
| Bodily pain | 73.95 (30.82) | 78.13 (28.85) | 23 | 0.7 | 0.49 |
| General health | 48.95 (20.16) | 46.88 (16.99) | 23 | −0.49 | 1 |
| Social functioning | 69.79 (33.77) | 83.33 (27.25) | 23 | 3 | 0.01 * |
| Role emotional | 68.75 (43.77) | 77.08 (36.05) | 23 | 1.16 | 0.26 |
| Mental health | 70.00 (22.26) | 79.17 (21.45) | 23 | 2.65 | 0.01 * |
| Vitality | 52.50 (24.18) | 65.00 (23.77) | 23 | 2.33 | 0.03 * |
| FCQ Dimension | Pre-Test Mean (SD) | Post-Test Mean (SD) | df | T-Score | p-Value |
|---|---|---|---|---|---|
| Natural content | 3.04 (0.75) | 3.32 (0.62) | 59 | 3.12 | 0.003 * |
| Convenience | 3.30 (0.68) | 3.17 (0.63) | 59 | 2.18 | 0.03 * |
| Familiarity | 2.66 (0.91) | 2.44 (0.95) | 59 | −2.62 | 0.01 * |
| Weight control | 3.25 (0.83) | 3.47 (0.57) | 58 | 2.02 | 0.048 * |
| Ethical concern | 2.51 (1.05) | 2.60 (0.91) | 59 | 0.8 | 0.43 |
| Price | 3.24 (0.74) | 3.13 (0.76) | 59 | −1.3 | 0.2 |
| Mood | 2.95 (0.90) | 2.83 (0.95) | 59 | 1.15 | 0.26 |
| Sensory appeal | 3.30 (0.67) | 3.26 (0.68) | 59 | −0.061 | 0.54 |
| Health | 3.27 (0.73) | 3.40 (0.62) | 59 | −1.52 | 0.13 |
| Healthy Tips and Recipe Responses |
| “Good information for me to know. Thank you” |
| “I luv [sic] the daily tips pls [sic] cont [sic] thank you” |
| “Soup was delicious, great using veg [sic] stock” |
| “I am enjoying the recipes. They are easy and quick to make. I have a new appreciation for beans. Please keep them coming. I like new dishes. Thanks!” |
| Responses Indicating Behavior Change |
| “I made some soup and I ate lots of salad last week. No meat!!!” |
| “I made ur [sic] wonderful meals. My favorite so far is the black bean chili and lentil/sweet potato” |
| “eating more healthier, made spagetti [sic] squash and califlower [sic]with parsnips blended together instead of mash potatoes topped with veggie chee[se]” [sic] |
| “Thank u [sic] for the Healthy meals!!!!! I m [sic] on day 3 eating veggies Just loving it. Thank u [sic]again” |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vaughn, N.A.; Brown, D.; Reyes, B.O.; Wyatt, C.; Arnold, K.T.; Dalianis, E.; Kalksma, P.J.; Roth, C.; Langheier, J.; Pajil-Battle, M.; et al. A 40-Day Journey to Better Health: Utilizing the DanielFast to Improve Health Outcomes in Urban Church-Based Settings. Healthcare 2018, 6, 25. https://doi.org/10.3390/healthcare6010025
Vaughn NA, Brown D, Reyes BO, Wyatt C, Arnold KT, Dalianis E, Kalksma PJ, Roth C, Langheier J, Pajil-Battle M, et al. A 40-Day Journey to Better Health: Utilizing the DanielFast to Improve Health Outcomes in Urban Church-Based Settings. Healthcare. 2018; 6(1):25. https://doi.org/10.3390/healthcare6010025
Chicago/Turabian StyleVaughn, Nicole A., Darryl Brown, Beatriz O. Reyes, Crystal Wyatt, Kimberly T. Arnold, Elizabeth Dalianis, Paula J. Kalksma, Caryn Roth, Jason Langheier, Maria Pajil-Battle, and et al. 2018. "A 40-Day Journey to Better Health: Utilizing the DanielFast to Improve Health Outcomes in Urban Church-Based Settings" Healthcare 6, no. 1: 25. https://doi.org/10.3390/healthcare6010025




