ECG Signal De-noising and Baseline Wander Correction Based on CEEMDAN and Wavelet Threshold
Abstract
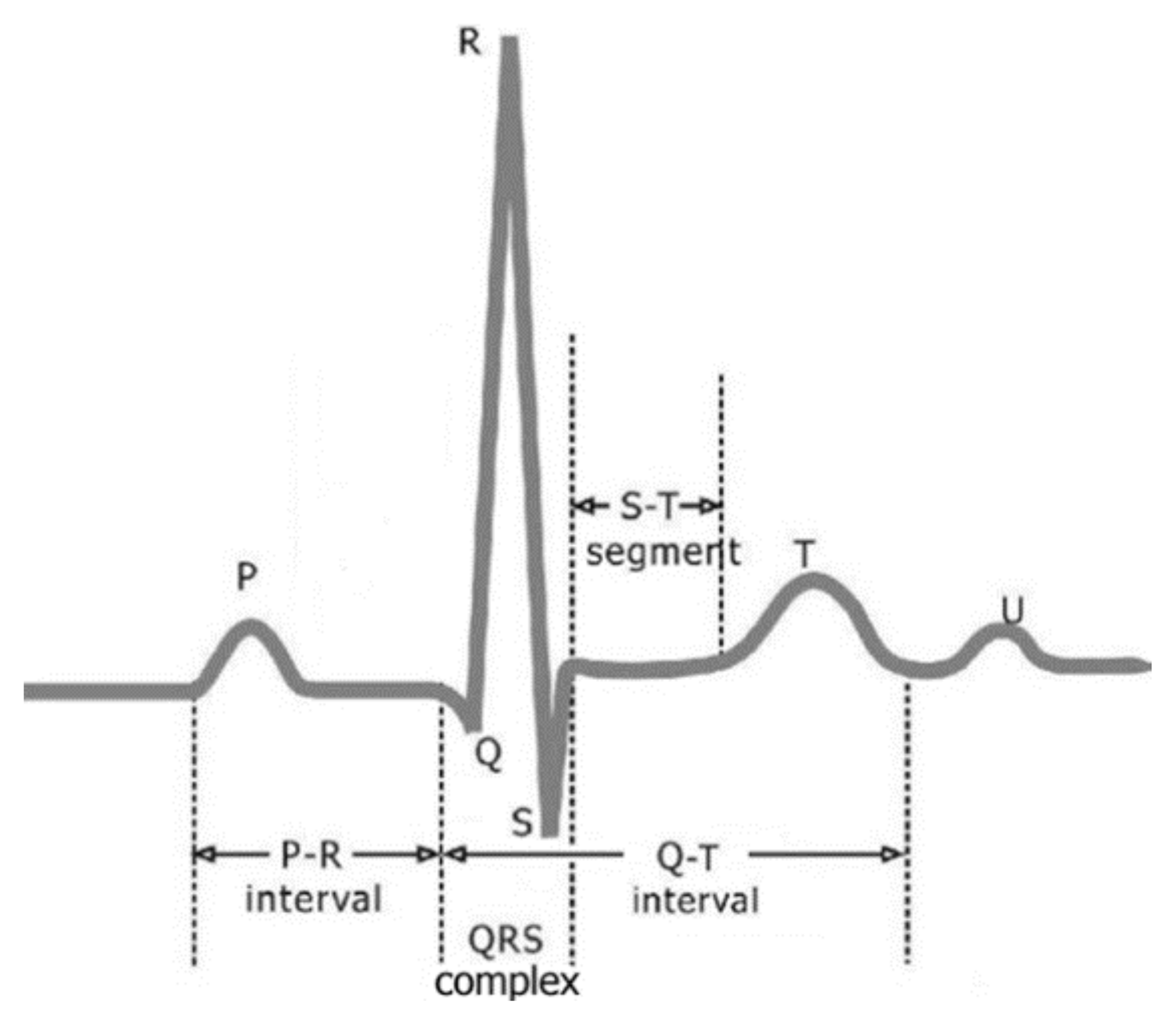
:1. Introduction
2. Basic Principle
2.1. EMD, EEMD, CEEMDAN Algorithm
- Step 1.
- Find all extreme points (both minima and maxima) in the test signal s(t).
- Step 2.
- Use the cubic spline interpolation between maxima (minima) to obtain the upper (lower) envelope u0(t) (d0(t)).
- Step 3.
- Compute the mean envelope,
- Step 4.
- Subtract the mean envelope from s(t) to obtain,
- Step 5.
- If h1(t) follows the criteria of the IMF, then it is the IMF1, otherwise h1(t) is considered as the data of the sifting process, and repeat steps 1 to 4. Thus a new function h11(t) is obtained. This process will be repeated until either h1k(t) follows the criteria of IMF or a certain termination condition (generally standard deviation criteria) is met.
- Step 6.
- Subtract the IMF1 from s(t) to obtain the residue,
- Step 7.
- Treat the residual as a new signal, repeat steps 1 to 6, and other IMFs such as IMF2, IMF3, …, IMFN can be obtained, until becomes either a constant, a monotonic slope, or a function with only one extremum. After the EMD decomposition, the original signal s(t) can be expressed as,where N is the number of IMFs, and is the final residue.
- Step 1.
- The Gaussian white noise with zero mean and unit variance is added to the original signal , to obtain a new signal,
- Step 2.
- For every i = 1, …, I, decompose each by EMD, to obtain IMFik, where k = 1, …, N denote the number of IMFs.
- Step 3.
- Average IMFik, to obtain EEMD mode,
- Step 1.
- For every i = 1,…, I, decompose each by EMD, until its first mode, and define the first CEEMDAN mode as,
- Step 2.
- At the first stage (j = 1), calculate the first residue,
- Step 3.
- For every i = 1, …, I, decompose each by EMD, until its first mode, and define the second CEEMDAN mode as,
- Step 4.
- For j = 2, 3, …, N, calculate the j-th residue,
- Step 5.
- For every i = 1, …, I, decompose each by EMD, until its first mode, and define the (j + 1)-th CEEMDAN mode as,
- Step 6.
- Go to step 4 for the next j.
2.2. Improved Wavelet Threshold Function
3. ECG Signal De-Noising Procedure
3.1. Flowchart of ECG Signal De-Noising
3.2. Random Noise Suppression in the ECG Signal
3.3. ECG Baseline Wander Correction
4. ECG Signal De-Noising Results
4.1. Synthetic Noisy ECG Signal De-Noising Results
4.2. Real ECG Signal De-Noising Results
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Brady, W.J.; Hudson, K.B.; Naples, R.; Sudhir, A.; Mitchell, S.H.; Ferguson, J.D. The ECG in Prehospital Emergency Care; Wiley Blackwell Publishing Ltd.: Hoboken, NJ, USA, 2013. [Google Scholar]
- Raka, A.G.; Naik, G.R.; Chai, R. Computational Algorithms Underlying the Time-Based Detection of Sudden Cardiac Arrest via Electrocardiographic Markers. Appl. Sci. 2017, 7, 954. [Google Scholar] [CrossRef]
- Peng, Y.; Wang, X.; Guo, L.; Wang, Y.; Deng, Q. An Efficient Network Coding-Based Fault-Tolerant Mechanism in WBAN for Smart Healthcare Monitoring Systems. Appl. Sci. 2017, 7, 817. [Google Scholar] [CrossRef]
- Weder, M.; Hegemann, D.; Amberg, M.; Hess, M.; Boesel, L.F.; Abächerli, R.; Meyer, V.R.; Rossi, R.M. Embroidered Electrode with Silver/Titanium Coating for Long-Term ECG Monitoring. Sensors 2015, 15, 1750–1759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abtahi, F.; Snäll, J.; Aslamy, B.; Abtahi, S.; Seoane, F.; Lindecrantz, K. Biosignal PI, an Affordable Open-Source ECG and Respiration Measurement System. Sensors 2015, 15, 93–109. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-H.; de Beeck, M.O.; Vanderheyden, L.; Carrette, E.; Mihajlović, V.; Vanstreels, K.; Grundlehner, B.; Gadeyne, S.; Boon, P.; Van Hoof, C. Soft, Comfortable Polymer Dry Electrodes for High Quality ECG and EEG Recording. Sensors 2014, 14, 23758–23780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laguna, P.; Jan, R.; Caminal, P. Automatic detection of wave boundaries in multilead ECG signals: Validation with the cse database. Comput. Biomed. Res. 1994, 27, 45–60. [Google Scholar] [CrossRef] [PubMed]
- Stridh, M.; Sornmo, L. Spatiotemporal QRST cancellation techniques for analysis of atrial fibrillation: Methods and performance. In Proceedings of the Computers in Cardiology, Cleveland, OH, USA, 13–16 September 1998. [Google Scholar]
- De Chazal, P.; O’Dwyer, M.; Reilly, R.B. Automatic classification of heartbeats using ECG morphology and heartbeat interval features. IEEE Trans. Bio-Med. Eng. 2004, 51, 1196–1206. [Google Scholar] [CrossRef] [PubMed]
- Rubel, P.; Fayn, J.; Mohsen, N.; Girard, P. New methods of quantitative assessment of the extent and significance of serial ECG changes of the repolarization phase. J. Electrocardiol. 1988, 21, S177–S181. [Google Scholar] [CrossRef]
- Guo, X.; Shen, C.; Chen, L. Deep Fault Recognizer: An Integrated Model to De-noise and Extract Features for Fault Diagnosis in Rotating Machinery. Appl. Sci. 2017, 7, 41. [Google Scholar] [CrossRef]
- Al-Tmeme, A.; Woo, W.L.; Dlay, S.S.; Gao, B. Underdetermined convolutive source separation using gem-mu with variational approximated optimum model order nmf2d. IEEE/ACM Trans. Audio Speech Lang. Process. 2017, 25, 35–49. [Google Scholar] [CrossRef]
- Al-Nima, R.R.O.; Abdullah, M.A.M.; Al-Kaltakchi, M.T.S.; Dlay, S.S.; Woo, W.L.; Chambers, J.A. Finger texture biometric verification exploiting multi-scale sobel angles local binary pattern features and score-based fusion. Dig. Signal Process. 2017, 70, 178–189. [Google Scholar] [CrossRef]
- Wang, A.D.; Liu, L.; Wei, Q. An adaptive morphologic filter applied to ECG de-noising and extraction of r peak at real-time. AASRI Procedia 2012, 1, 474–479. [Google Scholar]
- Agostinelli, A.; Sbrollini, A.; Giuliani, C.; Fioretti, S.; Nardo, F.D.; Burattini, L. Segmented beat modulation method for electrocardiogram estimation from noisy recordings. Med. Eng. Phys. 2016, 38, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Ren, A.; Du, Z.; Li, J.; Hu, F.; Yang, X.; Abbas, H. Adaptive Interference Cancellation of ECG Signals. Sensors 2017, 17, 942. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.L.P.; Woo, W.L.; Dlay, S.S. Enhanced wavelet transformation for feature extraction in highly variated ECG signal. In Proceedings of the 2nd IET International Conference on Intelligent Signal Processing 2015 (ISP), London, UK, 1–2 December 2015. [Google Scholar]
- Mallat, S. A Wavelet Tour of Signal Processing. In A Wavelet Tour of Signal Processing, 2nd ed.; Academic Press: London, UK, 1999; pp. 83–85. [Google Scholar]
- Donoho, D.L. De-noising by soft-thresholding. IEEE Trans. Inf. Theory 2002, 41, 613–627. [Google Scholar] [CrossRef]
- Yi, T.-H.; Li, H.-N.; Zhao, X.-Y. Noise Smoothing for Structural Vibration Test Signals Using an Improved Wavelet Thresholding Technique. Sensors 2012, 12, 11205–11220. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.N.; Tiwari, A.K. Optimal selection of wavelet basis function applied to ECG signal denoising. Dig. Signal Process. 2006, 16, 275–287. [Google Scholar] [CrossRef]
- Liu, X.; Qiao, L.; Yang, J.; Dong, B.; Wang, H. An improved wavelet threshold algorithm for ECG denoising. J. Biomed. Eng. 2014, 31, 511. [Google Scholar]
- Das, A.; Nirmala, S.R.; Medhi, J.P. ECG denoising based on probability of wavelet coefficients. In Proceedings of the 2015 International Symposium on Advanced Computing and Communication (ISACC), Silchar, India, 14–15 September 2015. [Google Scholar]
- Chen, S.W.; Chen, Y.H. Hardware design and implementation of a wavelet de-noising procedure for medical signal preprocessing. Sensors 2015, 15, 26396–26414. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Wang, Z.; Tan, C.; Si, L.; Liu, X. A novel de-noising method for an acoustic-based system through empirical mode decomposition and an improved fruit fly optimization algorithm. Appl. Sci. 2017, 7, 215. [Google Scholar] [CrossRef]
- Lv, Y.; Yuan, R.; Song, G. Multivariate empirical mode decomposition and its application to fault diagnosis of rolling bearing. Mech. Syst. Signal Process. 2016, 81, 219–234. [Google Scholar] [CrossRef]
- Zhao, X.; Li, M.; Song, G.; Xu, J. Hierarchical ensemble-based data fusion for structural health monitoring. Smart Mater. Struct. 2010, 19. [Google Scholar] [CrossRef]
- Blanco-Velasco, M.; Weng, B.; Barner, K.E. ECG signal de-noising and baseline wander correction based on the empirical mode decomposition. Comput. Biol. Med. 2008, 38, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Singh, O.; Sunkaria, R.K. Ecg signal de-noising based on empirical mode decomposition and moving average filter. Int. J. Med. Eng. Inf. 2013, 6, 1–6. [Google Scholar]
- Kabir, M.A.; Shahnaz, C. Denoising of ECG signals based on noise reduction algorithms in EMD and wavelet domains. Biomed. Signal Process. Control 2012, 7, 481–489. [Google Scholar] [CrossRef]
- Wu, Z.H.; Huang, N.E. Ensemble empirical mode decomposition: A noise-assisted data analysis method. Adv. Adapt. Data Anal. 2009, 1. [Google Scholar] [CrossRef]
- Zhao, Z.; Yang, L.; Chen, D.; Luo, Y. A Human ECG Identification System Based on Ensemble Empirical Mode Decomposition. Sensors 2013, 13, 6832–6864. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.-M. Arrhythmia ECG Noise Reduction by Ensemble Empirical Mode Decomposition. Sensors 2010, 10, 6063–6080. [Google Scholar] [CrossRef] [PubMed]
- Ye, L.L.; Yang, D.; Wang, X. Research on ECG De-noising Method Based on Ensemble Empirical Mode Decomposition and Wavelet Transform Using Improved Threshold Function. J. Biomed. Eng. 2014, 31, 567–571. [Google Scholar]
- Chang, K.M. Ensemble empirical mode decomposition for high frequency ECG noise reduction. Biomed. Tech. Biomed. Eng. 2010, 55, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Torres, M.E.; Colominas, M.A.; Schlotthauer, G.; Flandrin, P. A complete ensemble empirical mode decomposition with adaptive noise. In Proceedings of the IEEE International Conference on Acoustics, Speech and Signal Processing, Prague, Czech Republic, 22–27 May 2011. [Google Scholar]
- Wang, J.; Li, Z.C.; Wang, D.Y. A method for wavelet threshold de-noising of seismic data based on CEEMD. Geophys. Prospect. Pet. 2014, 53, 164–172. [Google Scholar]
- Huang, W.; Cai, N.; Xie, W.; Ye, Q.; Yang, Z. ECG baseline wander correction based on ensemble empirical mode decomposition with complementary adaptive noise. J. Med. Imaging Health Inf. 2015, 5, 1796–1799. [Google Scholar] [CrossRef]
- Jin, J.J.; Wang, X.; Wu, X.; Yang, D. Translation-Invariant De-noising of Body Fluttering Signal Based on Improved Threshold Function. J. Northeast. Univ. 2009, 30, 333–336. [Google Scholar]
- Roonizi, E.K.; Sameni, R. Morphological modeling of cardiac signals based on signal decomposition. Comput. Biol. Med. 2013, 43, 1453–1461. [Google Scholar] [CrossRef] [PubMed]









| IMF | IMF1 | IMF2 | IMF3 | IMF4 | IMF5 | IMF6 | IMF7 | IMF8 | IMF9 | IMF10 | IMF11 | Residue |
| ZCR | 246.6 | 119.2 | 61.4 | 33.5 | 18.7 | 11.4 | 6.6 | 4.1 | 2.3 | 0.7 | 0.2 | 0.0 |
| Noise Intensity | Index | Wavelet Based | EMD Partial Reconstruction | CEEMDAN Plus Wavelet Threshold |
|---|---|---|---|---|
| 5 dB | SER | 0.8751 | 6.8711 | 18.3150 |
| MSE | 0.0452 | 0.0218 | 0.0016 | |
| 10 dB | SER | 0.5978 | 5.9251 | 17.0436 |
| MSE | 0.0466 | 0.0271 | 0.0021 | |
| 15 dB | SER | 0.4232 | 4.8161 | 12.5823 |
| MSE | 0.0492 | 0.0295 | 0.0056 | |
| 20 dB | SER | 0.2435 | 3.9363 | 10.4129 |
| MSE | 0.0709 | 0.0638 | 0.0097 |
| Noise Intensity | Index | Wavelet-Based | EMD Partial Reconstruction | CEEMDAN Plus Wavelet Threshold |
|---|---|---|---|---|
| 5 dB | SER | 14.7072 | 16.2526 | 27.8397 |
| MSE | 0.0201 | 0.0113 | 0.0006 | |
| 10 dB | SER | 13.1222 | 15.6894 | 25.3689 |
| MSE | 0.0210 | 0.0129 | 0.0011 | |
| 15 dB | SER | 11.7577 | 13.9286 | 20.4182 |
| MSE | 0.0316 | 0.0154 | 0.0035 | |
| 20 dB | SER | 10.6856 | 11.9397 | 16.1626 |
| MSE | 0.0405 | 0.0217 | 0.0095 |
| Noise Intensity | Index | Wavelet-Based | EMD Partial Reconstruction | CEEMDAN Plus Wavelet Threshold |
|---|---|---|---|---|
| 5 dB | SER | 14.9580 | 17.9656 | 26.6223 |
| MSE | 0.0213 | 0.0096 | 0.0010 | |
| 10 dB | SER | 12.8418 | 16.1767 | 24.8403 |
| MSE | 0.0235 | 0.0105 | 0.0016 | |
| 15 dB | SER | 11.3410 | 14.8742 | 21.6968 |
| MSE | 0.0380 | 0.0124 | 0.0041 | |
| 20 dB | SER | 10.3478 | 13.7996 | 17.8879 |
| MSE | 0.0438 | 0.0198 | 0.0097 |
| MIT–BIH ECG Record | Index | Wavelet-Based | EMD Partial Reconstruction | CEEMDAN Plus Wavelet Threshold |
|---|---|---|---|---|
| No. 109 | SER | 8.2816 | 13.6221 | 19.7232 |
| MSE | 0.0560 | 0.0317 | 0.0196 | |
| No. 203 | SER | 12.0928 | 16.4504 | 21.7684 |
| MSE | 0.0510 | 0.0409 | 0.0284 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, Y.; Luo, M.; Li, T.; Song, G. ECG Signal De-noising and Baseline Wander Correction Based on CEEMDAN and Wavelet Threshold. Sensors 2017, 17, 2754. https://doi.org/10.3390/s17122754
Xu Y, Luo M, Li T, Song G. ECG Signal De-noising and Baseline Wander Correction Based on CEEMDAN and Wavelet Threshold. Sensors. 2017; 17(12):2754. https://doi.org/10.3390/s17122754
Chicago/Turabian StyleXu, Yang, Mingzhang Luo, Tao Li, and Gangbing Song. 2017. "ECG Signal De-noising and Baseline Wander Correction Based on CEEMDAN and Wavelet Threshold" Sensors 17, no. 12: 2754. https://doi.org/10.3390/s17122754
APA StyleXu, Y., Luo, M., Li, T., & Song, G. (2017). ECG Signal De-noising and Baseline Wander Correction Based on CEEMDAN and Wavelet Threshold. Sensors, 17(12), 2754. https://doi.org/10.3390/s17122754






