A Novel Setup and Protocol to Measure the Range of Motion of the Wrist and the Hand
Abstract
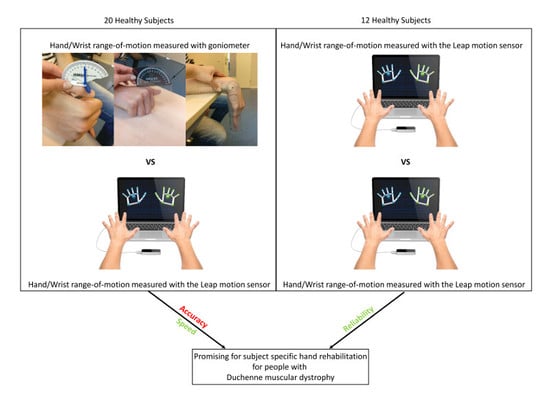
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Materials and Data Acquisition
2.3. Experimental Protocol
2.4. Statistical Analyses
3. Results
3.1. Evaluation of the Leap Motion Sensor
3.2. Test-Retest
3.3. Measurement Time
4. Discussion
4.1. Rationale
4.2. Leap vs. Goniometer
4.3. Test vs. Re-Test
4.4. Time Consumption
4.5. Lessons Learned
4.6. Implications for Clinical Use
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kapandji, I.A. The Physiology of the Joints: Annotated Diagrams of the Mechanics of the Human Joints; Churchill Livingstone: London, UK, 1987. [Google Scholar]
- Lutz, W.; Sanderson, W.; Scherbov, S. The coming acceleration of global population ageing. Nature 2008, 451, 716–719. [Google Scholar] [CrossRef] [PubMed]
- Hung, L.K.; Ho, K.K.; Leung, P.C. Impairment of hand function and loss of earning capacity after occupational hand injury: Prospective cohort study. Hong Kong Med. J. 1999, 5, 245–250. [Google Scholar] [PubMed]
- Bos, R.A.; Haarman, C.J.; Stortelder, T.; Nizamis, K.; Herder, J.L.; Stienen, A.H.; Plettenburg, D.H. A structured overview of trends and technologies used in dynamic hand orthoses. J. Neuroeng. Rehabil. 2016, 13, 62. [Google Scholar] [CrossRef] [PubMed]
- Schaechter, J.D.; Stokes, C.; Connell, B.D.; Perdue, K.; Bonmassar, G. Finger motion sensors for fMRI motor studies. NeuroImage 2006, 31, 1549–1559. [Google Scholar] [CrossRef] [PubMed]
- Romitti, P.A.; Zhu, Y.; Puzhankara, S.; James, K.A.; Nabukera, S.K.; Zamba, G.K.D.; Ciafaloni, E.; Cunniff, C.; Druschel, C.M.; Mathews, K.D.; et al. Prevalence of Duchenne and Becker Muscular Dystrophies in the United States. Pediatrics 2015. [Google Scholar] [CrossRef] [PubMed]
- Oess, N.P.; Wanek, J.; Curt, A. Design and evaluation of a low-cost instrumented glove for hand function assessment. J. Neuroeng. Rehabil. 2012, 9, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gajdosik, R.L.; Bohannon, R.W. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys. Ther. 1987, 67, 1867–1872. [Google Scholar] [CrossRef] [PubMed]
- Mendell, J.R.; Lloyd-Puryear, M. Report of MDA muscle disease symposium on newborn screening for Duchenne muscular dystrophy. Muscle Nerve 2013, 48, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Bartels, B.; Pangalila, R.F.; Bergen, M.P.; Cobben, N.A.; Stam, H.J.; Roebroeck, M.E. Upper limb function in adults with Duchenne muscular dystrophy. J. Rehabil. Med. 2011, 43, 770–775. [Google Scholar] [PubMed] [Green Version]
- Janssen, M.M.; Bergsma, A.; Geurts, A.C.; de Groot, I.J. Patterns of decline in upper limb function of boys and men with DMD: An international survey. J. Neurol. 2014, 261, 1269–1288. [Google Scholar] [CrossRef] [PubMed]
- Weichbrodt, J.; Eriksson, B.M.; Kroksmark, A.K. Evaluation of hand orthoses in Duchenne muscular dystrophy. Disability Rehabil. 2017, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Eagle, M. Report on the muscular dystrophy campaign workshop: Exercise in neuromuscular diseases Newcastle, January 2002. Neuromuscul. Disord. NMD 2002, 12, 975–983. [Google Scholar] [CrossRef]
- Flextension Symbionics Project. Availabe online: http://symbionics.info/project3/ (accessed on 13 March 2018).
- Lewis, E.; Fors, L.; Tharion, W.J. Interrater and intrarater reliability of finger goniometric measurements. Am. J. Occup. Ther. Off. Publ. Am. Occup. Ther. Assoc. 2010, 64, 555–561. [Google Scholar] [CrossRef]
- Bovens, A.M.; van Baak, M.A.; Vrencken, J.G.; Wijnen, J.A.; Verstappen, F.T. Variability and reliability of joint measurements. Am. J. Sports Med. 1990, 18, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Norkin, C.C.; White, D.J. Measurement of Joint Motion A Guide to Goniometry, 4th ed.; FA Davis Company: Philadelphia, PA, USA, 2009. [Google Scholar]
- Bassily, D.; Georgoulas, C.; Guettler, J.; Linner, T.; Bock, T. Intuitive and Adaptive Robotic Arm Manipulation using the Leap Motion Controller. In Proceedings of the 41st International Symposium on Robotics (ISR/Robotik 2014), Munich, Germany, 2–3 June 2014; pp. 1–7. [Google Scholar]
- Dipietro, L.; Sabatini, A.M.; Dario, P. Evaluation of an instrumented glove for hand-movement acquisition. J. Rehabil. Res. Dev. 2003, 40, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Chen, I.M.; Yeo, S.H.; Lim, C.K. Development of finger-motion capturing device based on optical linear encoder. J. Rehabil. Res. Dev. 2011, 48, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Gentner, R.; Classen, J. Development and evaluation of a low-cost sensor glove for assessment of human finger movements in neurophysiological settings. J. Neurosci. Methods 2009, 178, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Simone, L.K.; Kamper, D.G. Design considerations for a wearable monitor to measure finger posture. J. Neuroeng. Rehabil. 2005, 2, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kortier, H.G.; Sluiter, V.I.; Roetenberg, D.; Veltink, P.H. Assessment of hand kinematics using inertial and magnetic sensors. J. Neuroeng. Rehabil. 2014, 11, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pham, T.; Pathirana, P.N.; Trinh, H.; Fay, P. A Non-Contact Measurement System for the Range of Motion of the Hand. Sensors 2015, 15, 18315–18333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bachmann, D.; Weichert, F.; Rinkenauer, G. Evaluation of the Leap Motion Controller as a New Contact-Free Pointing Device. Sensors 2015, 15, 214–233. [Google Scholar] [CrossRef] [PubMed]
- Pambudi, R.A.; Ramadijanti, N.; Basuki, A. Psychomotor game learning using skeletal tracking method with leap motion technology. In Proceedings of the 2016 International Electronics Symposium (IES), Denpasar, Indonesia, 29–30 September 2016; pp. 142–147. [Google Scholar]
- Trejo, R.L.; Vázquez, J.P.G.; Ramirez, M.L.G.; Corral, L.E.V.; Marquez, I.R. Hand goniometric measurements using leap motion. In Proceedings of the 2017 14th IEEE Annual Consumer Communications & Networking Conference (CCNC), Las Vegas, NV, USA, 8–11 January 2017; pp. 137–141. [Google Scholar]
- Guna, J.; Jakus, G.; Pogacnik, M.; Tomazic, S.; Sodnik, J. An analysis of the precision and reliability of the leap motion sensor and its suitability for static and dynamic tracking. Sensors 2014, 14, 3702–3720. [Google Scholar] [CrossRef] [PubMed]
- Brekel. Affordable Motion Capture Tools—Pro Hands. Available online: https://brekel.com/brekel-pro-hands/pro-hands-download-trial-buy/ (accessed on 6 June 2018).
- Bo, A.P.L.; Poignet, P.; Geny, C. Pathological Tremor and Voluntary Motion Modeling and Online Estimation for Active Compensation. IEEE Trans. Neural Syst. Rehabil. Eng. 2011, 19, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laerd Statistics. One-Sample T-Test Using SPSS Statistics. Availabe online: https://statistics.laerd.com/spss-tutorials/one-sample-t-test-using-spss-statistics.php (accessed on 20 September 2018).
- McVeigh, K.H.; Murray, P.M.; Heckman, M.G.; Rawal, B.; Peterson, J.J. Accuracy and Validity of Goniometer and Visual Assessments of Angular Joint Positions of the Hand and Wrist. J. Hand Surg. 2016, 41, e21–e35. [Google Scholar] [CrossRef] [PubMed]
- Placidi, G.; Cinque, L.; Polsinelli, M.; Spezialetti, M. Measurements by A LEAP-Based Virtual Glove for the Hand Rehabilitation. Sensors 2018, 18, 834. [Google Scholar] [CrossRef] [PubMed]
- Levanon, Y. The advantages and disadvantages of using high technology in hand rehabilitation. J. Hand Ther. Off. J. Am. Soc. Hand Ther. 2013, 26, 179–183. [Google Scholar] [CrossRef] [PubMed]






| Joint | Direction | Mean Gonio (sd) | Mean Leap (sd) | Mean Diff | 95% CI of Mean Diff | One Sample t-Test (2-Tailed) |
|---|---|---|---|---|---|---|
| Wrist | Radial dev | 19(4) | 26(9) | −7 | −11; −2 | 0.007 |
| Ulnar dev | −35(5) | −38(6) | 3 | −1;6 | 0.115 | |
| Pronation | 77(10) | 90(12) | −13 | −19; −7 | <0.001 | |
| Supination | −82(16) | −43(24) | −39 | −51; −26 | <0.001 | |
| Flexion | 79(8) | 70(14) | 9 | 4;14 | 0.001 | |
| Extension | −63(12) | −66(12) | 3 | −1;7 | 0.137 | |
| Thumb MCP | Flexion | 59(13) | 36(6) | 24 | 18;30 | <0.001 |
| Extension | −5(15) | 6(7) | −11 | −17; −5 | 0.001 | |
| Thumb IP | Flexion | 76(16) | 28(4) | 48 | 40;56 | <0.001 |
| Extension | −25(6) | −2(8) | −23 | −27; −18 | <0.001 | |
| Index MCP | Flexion | 87(7) | 88(2) | −1 | −5;2 | 0.501 |
| Extension | −18(9) | −11(8) | −7 | −11; −3 | 0.003 | |
| Index PIP | Flexion | 109(5) | 82(2) | 27 | 24;30 | <0.001 |
| Extension | −3(4) | 2(3) | −5 | −8; −3 | <0.001 | |
| Index DIP | Flexion | 70(11) | 43(9) | 27 | 21;33 | <0.001 |
| Extension | −12(6) | 4(3) | −16 | −19; −13 | <0.001 | |
| Middle MCP | Flexion | 90(6) | 83(1) | 7 | 4;10 | <0.001 |
| Extension | −21(9) | −11(8) | −10 | −14; −5 | 0.001 | |
| Middle PIP | Flexion | 108(6) | 85(2) | 23 | 21;26 | <0.001 |
| Extension | −4(6) | 3(3) | −7 | −10; −3 | <0.001 | |
| Middle DIP | Flexion | 81(8) | 41(2) | 39 | 36;43 | <0.001 |
| Extension | −14(6) | 4(4) | −17 | −21; −14 | <0.001 | |
| Ring MCP | Flexion | 87(8) | 80(1) | 8 | 4;11 | <0.001 |
| Extension | −23(9) | −11(9) | −12 | −17; −7 | <0.001 | |
| Ring PIP | Flexion | 108(7) | 81(2) | 27 | 24;30 | <0.001 |
| Extension | −6(10) | 2(4) | −8 | −14; −3 | 0.003 | |
| Ring DIP | Flexion | 77(9) | 40(1) | 37 | 32;41 | <0.001 |
| Extension | −15(8) | 4(4) | −19 | −23; −15 | <0.001 | |
| Little MCP | Flexion | 89(7) | 71(2) | 18 | 15;22 | <0.001 |
| Extension | −27(13) | −14(6) | −13 | −19; −6 | <0.001 | |
| Little PIP | Flexion | 100(6) | 74(3) | 26 | 23;29 | <0.001 |
| Extension | −6(10) | 2(3) | −8 | −13; −4 | 0.001 | |
| Little DIP | Flexion | 79(12) | 40(2) | 40 | 34;45 | <0.001 |
| Extension | −11(9) | 3(4) | −15 | −19; −11 | <0.001 |
| Joint | Direction | Mean Leap Test (sd) | Mean Leap Retest (sd) | Mean Diff | 95% CI of Mean Diff | One Sample t-Test (2-Tailed) |
|---|---|---|---|---|---|---|
| Wrist | Radial dev | 27(9) | 26(8) | 1 | −7;8 | 0.798 |
| Ulnar dev | −40(5) | −40(8) | 0 | −6;5 | 0.888 | |
| Pronation | 95(12) | 99(15) | −4 | −13;6 | 0.413 | |
| Supination | −42(25) | −41(35) | −1 | −23;21 | 0.939 | |
| Flexion | 75(11) | 67(18) | 8 | −7;22 | 0.270 | |
| Extension | −71(12) | −70(14) | −1 | −10;7 | 0.724 | |
| Thumb MCP | Flexion | 35(6) | 34(5) | 1 | −3;4 | 0.757 |
| Extension | 5(7) | 6(8) | −1 | −7;6 | 0.862 | |
| Thumb IP | Flexion | 27(4) | 25(3) | 2 | −1;6 | 0.214 |
| Extension | −3(8) | −5(9) | 2 | −5;9 | 0.507 | |
| Index MCP | Flexion | 88(2) | 88(2) | 0 | −2;2 | 0.891 |
| Extension | −8(7) | −9(5) | 1 | −2;4 | 0.537 | |
| Index PIP | Flexion | 82(3) | 81(3) | 1 | −1;3 | 0.380 |
| Extension | 1(4) | 0(2) | 1 | −2;4 | 0.467 | |
| Index DIP | Flexion | 45(12) | 41(2) | 4 | −3;11 | 0.249 |
| Extension | 3(3) | 2(2) | 1 | −1;4 | 0.198 | |
| Middle MCP | Flexion | 83(1) | 83(1) | 0 | −1;1 | 0.597 |
| Extension | −9(7) | −11(6) | 2 | −1;6 | 0.194 | |
| Middle PIP | Flexion | 85(2) | 84(3) | 1 | −1;4 | 0.255 |
| Extension | 2(4) | 1(2) | 1 | −1;4 | 0.300 | |
| Middle DIP | Flexion | 41(3) | 41(2) | 0 | −3;2 | 0.768 |
| Extension | 3(4) | 2(3) | 1 | −2;4 | 0.474 | |
| Ring MCP | Flexion | 80(1) | 80(1) | 0 | −1;1 | 0.884 |
| Extension | −8(9) | −12(6) | 4 | −2;9 | 0.183 | |
| Ring PIP | Flexion | 81(2) | 81(2) | 0 | −1;2 | 0.584 |
| Extension | 2(5) | 0(2) | 2 | −2;6 | 0.300 | |
| Ring DIP | Flexion | 40(1) | 41(1) | −1 | −3;0 | 0.109 |
| Extension | 3(4) | 2(2) | 1 | −2;4 | 0.401 | |
| Little MCP | Flexion | 71(1) | 71(1) | 0 | −1;1 | 0.848 |
| Extension | −13(6) | −16(5) | 3 | −1;6 | 0.130 | |
| Little PIP | Flexion | 75(3) | 76(2) | −1 | −3;0 | 0.122 |
| Extension | 3(3) | 1(2) | 2 | −1;4 | 0.183 | |
| Little DIP | Flexion | 39(2) | 40(2) | −1 | −2;−0 | 0.041 |
| Extension | 3(3) | 2(2) | 1 | −1;3 | 0.389 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nizamis, K.; Rijken, N.H.M.; Mendes, A.; Janssen, M.M.H.P.; Bergsma, A.; Koopman, B.F.J.M. A Novel Setup and Protocol to Measure the Range of Motion of the Wrist and the Hand. Sensors 2018, 18, 3230. https://doi.org/10.3390/s18103230
Nizamis K, Rijken NHM, Mendes A, Janssen MMHP, Bergsma A, Koopman BFJM. A Novel Setup and Protocol to Measure the Range of Motion of the Wrist and the Hand. Sensors. 2018; 18(10):3230. https://doi.org/10.3390/s18103230
Chicago/Turabian StyleNizamis, Kostas, Noortje H. M. Rijken, Ana Mendes, Mariska M. H. P. Janssen, Arjen Bergsma, and Bart F. J. M. Koopman. 2018. "A Novel Setup and Protocol to Measure the Range of Motion of the Wrist and the Hand" Sensors 18, no. 10: 3230. https://doi.org/10.3390/s18103230
APA StyleNizamis, K., Rijken, N. H. M., Mendes, A., Janssen, M. M. H. P., Bergsma, A., & Koopman, B. F. J. M. (2018). A Novel Setup and Protocol to Measure the Range of Motion of the Wrist and the Hand. Sensors, 18(10), 3230. https://doi.org/10.3390/s18103230