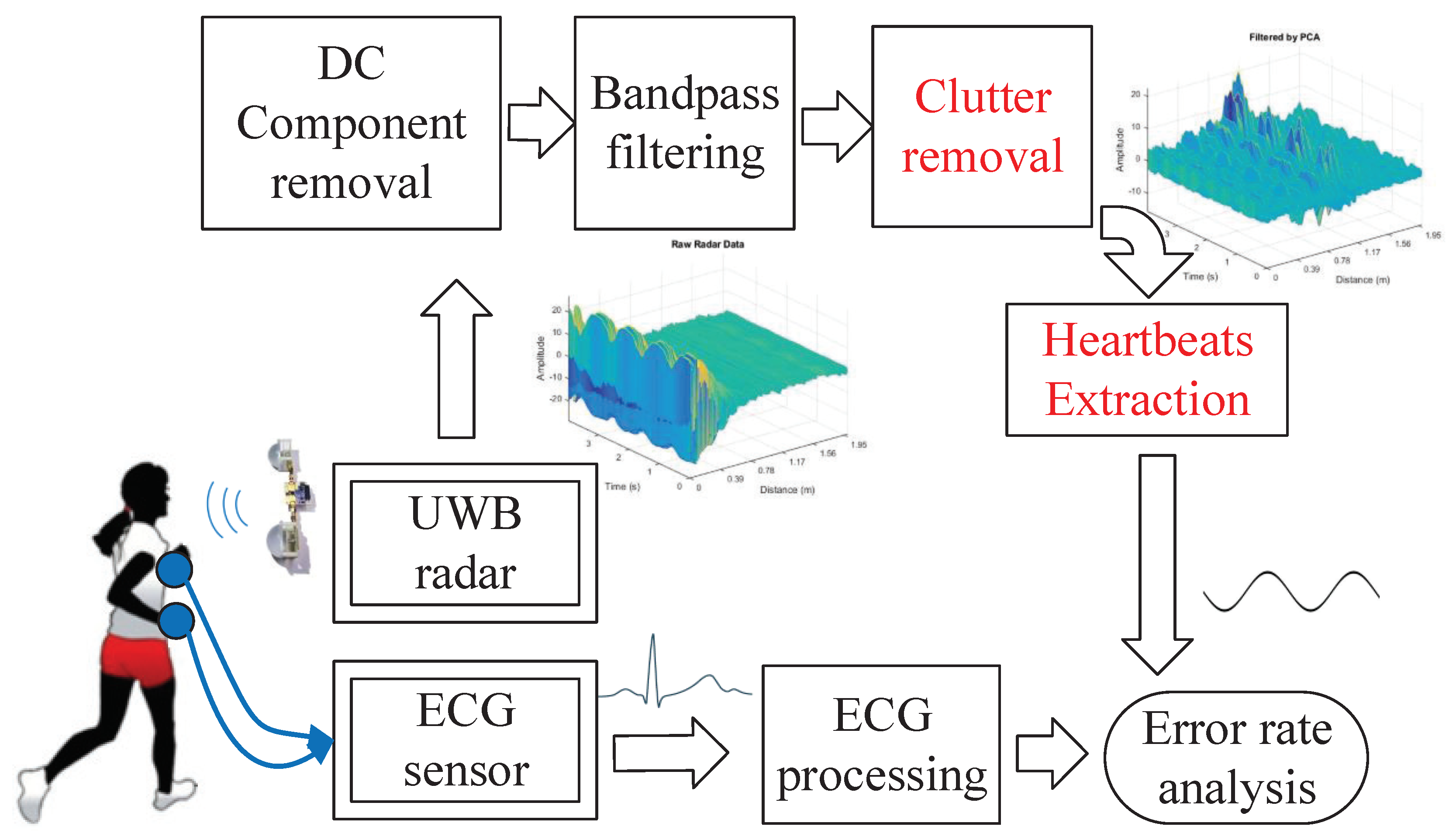
2.1. Static Clutter Removal in IR-UWB Radar
Since heartbeat signals are weak body movements, they are easily buried by the static clutter which is the unwanted reflection from surroundings. It is essential to suppress static clutter, caused by the antenna coupling, the impedance mismatch response and the ambient static clutter. Existing algorithms for clutter removal are based on the principal component analysis (PCA) [
19], the wavelet [
20], the moving averaging and its extensions [
18]. Given that the static clutter is similar in different echo signals, the moving averaging algorithm estimates the static clutter by taking a fraction of the previous clutter and a fraction from the current echo signal. In [
18], the modeling of static clutter is given by
where
t is the slow-time,
is the fast-time delay,
is the current clutter,
is the raw echo signal,
is a previous clutter, and
is the suppressing parameter between
. If
, the current clutter is equal to the previous clutter. If
, the current clutter is equal to the raw echo signal.
Figure 3a illustrates the result of moving averaging with strong static clutter. Since static clutter is preserved after the clutter removal based on moving averaging, HEAR proposes to further reduce interferences by subtracting background echos in multiple levels of wavelet decompositions. Specifically, HEAR adopts an adaptive threshold as
where
is the background echos that are collected when there is no target.
is acquired in the scenario with one target. HEAR adopts the biorthogonal wavelet (bior2.6) [
21] to decompose echos into 8 levels. Then,
is applied to the first four levels to remove background echos. The biorthogonal wavelet is selected to denoise IR-UWB radar data and meanwhile reduce distortions produced by reconstructions. Since the biorthogonal wavelet is able to solve the contradiction between symmetry and orthogonality requirements, it offers linear phases and assures an accurate signal reconstruction. Reconstruction errors of six kinds of wavelet families are calculated and the least two errors of each wavelet family are listed in
Table 1.
is the maximum reconstruction error and
is the average reconstruction error. As the comparison shows,
of biorthogonal wavelets is smaller than that of other five categories of wavelets. The energy of bior2.6 is more concentrated in the first four levels than that of bior2.4. For a specific echo, the energy ratio of first four levels to all levels decomposed by bior2.6 is 98.27% while the energy ratio by bior2.4 is 65.85%. Therefore, HEAR chooses bior2.6 to decompose echos into eight levels and performs the threshold-based denoising in the first four levels.
As in [
22], the amplitude of arrival clusters follows an exponential decay with the arrival time of clusters and multipaths. HEAR applies an exponential threshold to detailed coefficients at first four levels of wavelet decompositions as
where
y is the arrival time of clusters and
x is the arrival time of multipaths.
N is the multipath number in a cluster and
M is the total multipath number in all clusters.
b and
c are respectively the attenuation factors of multipaths and clusters.
a is the proportion factor of echos to unit channel models. HEAR determines
N by taking a cluster as 0.5 m.
c is calculated as the ratio of the maximum to the average of an echo.
b is set as 0.5.
is applied to the first four levels to reduce multipath interferences. After background echos and multipath interferences are removed, the inverse wavelet transform is carried out to recover target echos.
Figure 3b depicts echos with static clutter subtracted by the wavelet-based method. As the specific filtered echo in
Figure 3c shows, multipath interferences are reduced effectively.
2.2. Body Movement Compensation
As stated in [
23,
24], a time-varying channel impulse response is set as
where
M denotes the number of channel responses from static backgrounds,
N denotes the number of channel responses from the target,
t is slow-time,
is fast-time,
and
represent the reflection delay,
and
are amplitudes of the channel response. The received echo signal is obtained as a convolution of the channel response and the transmitted impulse
, as
According to [
25], the transmitted impulse is a mixture of derivatives of Gaussian impulse, as
. The formation parameter
and
is the variance of Gaussian pulses. It is supposed that the response of static channel is removed by the clutter removal, i.e.,
. Therefore, the received echo signal is formulated as
where
.
is the amplitude after impulses pass through the channel and
is the vibration of chest.
contains series of sub-echos
reflected from different positions of the target, including the specific echo
from the chest.
According to the above modeling, it is feasible to extract the vital signal from the changing fast-time delay related to maximum echo amplitudes. In Equation (5), when
reaches its maximum at the slow time
, the corresponding fast-time delay is denoted as
. The HEAR approach treats the
as a weighted sum of the reflection delay
of sub-echos, as
where
and
are weights related to the energy ratio of each sub-echo to the mixed echo,
is the weight of sub-echos from the chest, and
. As in [
26], the vibration of chest
is modeled as a sum of the antenna-to-target distance
and the vital signal
containing harmonics of respiration and heart beating, as
where
p and
q denote the harmonic order,
and
are respectively the respiratory frequency and the heartbeat frequency, and
and
are respectively initial phases of respiration and heartbeat.
Vital signals are generated by body micromovements such as breathing and heart beating. changes as target’s large body movements including walking or body shifting of a sitting target. In order to reduce interferences of large body movements, HEAR estimates body micromovements by amplitude attenuations and then compensating large body movements by an extended Kalman filter.
• Large body movement estimation
Large body movements are estimated by adopting a distance estimation method which integrates the multi-innovation Kalman (MIK) filter and the k-Nearest Neighbor. MIK filter applies multiple innovations of previous moments to predict antenna-to-target distances, achieving smoother estimations than conventional Kalman filters. MIK updates distance estimations as [
27]
where
is the updated distance estimation at current time
k.
is the posteriori distance estimation at time
k.
is the observation of antenna-to-target distances at time
k.
is the optimal Kalman gain.
is the noise covariance matrix.
p is the number of previous innovations used for current predictions.
Because of multipath interferences, there are multiple observations of distances for one target at time
k. HEAR combines the MIK filter with KNN to avoid deviations imported by selecting one distance from all observations as the input of MIK filtering. Specifically, during each iteration of MIK filtering, KNN is employed to select out the distance value
which is most close to previous
p estimations of distances
. HEAR applies the extended MIK filtering to predict the fast time delay
varying as large body movements.
Figure 4 illustrates large body movements
estimated by the extended Kalman filter and the correlation-based approach.
• Body micromovement estimation
Existing methods recover heartbeat waveforms by decomposing echo amplitudes with EMD, which depends on maximums and minimums of amplitudes. Body movements enlarge multipath interferences in echo amplitudes and therefore cause distortions in heartbeat waveforms reconstructed by EMD. To reduce interferences of body movements in recovering heartbeat waveforms, HEAR transfers amplitude variations into relative fluctuations of the fast time delay.
Supposing the echo amplitude
reaches its maximum
at
along the slow time, amplitude attenuations compared to
are proportional to increments of the fast time delay compared to
. It is assumed that the channel fading follows a Rayleigh distribution. The attenuation ratio of a specific amplitude
to
is equivalent to the ratio of their amplitudes appearing possibilities
and
. As shown in
Figure 5a, the difference of
and
is determined by the attenuation ratio of
to
. Given that
and
are constants,
varies corresponding to variations of
. As to the instance in
Figure 5a, the attenuation ratio of
to
at time
is larger than that at
marked in the red line, and the difference
at
is greater than that at
. Specifically, the transform from amplitudes
to the fast time delay
is calculated by solving the following equation:
where the variance
is set as
. The probability of amplitudes attenuation is
. After acquiring
from Equation (
10), the distance
is obtained as
.
Figure 5b shows the relation between
and
.
Figure 6b illustrates the aligned echos after compensating large body movements in
Figure 6a. The large body movement is compensated by subtracting
from
. The vital signal
is contained in the subtraction between
and
as in Equation (11), and therefore it is extractable by applying VNCMD in the following procedure. Algorithm 1 describes specific procedures for capturing the vital signal
:
After mapping maximum amplitudes to the fast time delay, large body movement compensations become feasible by a simple subtraction. In addition, waveform distortions of vital signs caused by large body movements are relieved.
| Algorithm 1: Flow of extracting vital signal . |
| Input: Filtered echo matrix , , .
|
| Output: Chirp signal containing the vital signal , .
|
| 1: Along the ridgeline of , save the amplitudes in to a vector , ;
|
| 2: Along the ridgeline of , save the fast time delay in to a vector , ;
|
| 3: Find the maximum in , note the amplitude as , and save the fast time delay as ;
|
| 4: Obtain the relative fast-time delay as by solving Equation (10); |
| 5: Compensate large body movements as Equation (11); |
| 6: return ; |
2.3. Separation of Heartbeats and Respirations by VNCMD
EMD is a method more general than filtering methods for separating heartbeats and respirations. However, the mode mixing problem in EMD hinders separating heartbeats from those respiratory harmonics whose energies are greater than heartbeats’ in the heartbeat band [1 Hz, 2 Hz]. VMD is an adaptive decomposition method which suppresses mode mixing problems in EMD. As in [
17], VNCMD overcomes limitations that VMD cannot acquire instantaneous amplitudes and instantaneous frequencies from each mode. In order to obtain instantaneous heart rates and heartbeat waveforms, the HEAR approach adopts the VNCMD to extract heartbeat signals.
As in Equation (
11), the vital signal is contained in a chirp signal
, which is equivalent to
where
j,
and
are respectively the number, the fast time delay and the initial phase of intermodulations of respirations and heartbeats. The intermodulations are imported to the fast time delay
by the mapping from amplitudes, since the amplitude is regulated by the intermodulations as well. Specifically, the echo amplitude
in Equation (
6) is expanded by the Taylor series as
where
. To be simplified, the coefficients of Gaussian impulses are omitted and no harmonic of respirations and heartbeats is considered in Equation (
13). Therefore, the chirp signal
comprises multiple frequencies including respiration rate
, heartbeat rate
, their harmonics and intermodulations. VNCMD is capable of recovering the time-varying heartbeat signal as a nonlinear chirp mode (NCM) decomposed from
. VNCMD requires initial frequencies for each NCM to be recovered. It is feasible to initialize modal frequencies by extracting ridge curves of the short time Fourier transform (STFT).
As discussed in [
17], the convergence of VNCMD depends on the noise level and the specified initial modal frequencies. A good initialization of modal frequencies helps VNCMD in converging in noisy situations. If the relative error between initial frequencies and real frequencies is smaller than 60%, the VNCMD still has a great success rate to converge to correct modal frequencies even at a strong noise level. To ensure that the VNCMD converges at the respiratory frequency and the heartbeat frequency rather than their harmonics, the initial modal frequency should contain frequency estimations of respirations and heartbeats. Since respiratory harmonics are stronger than heartbeats in spectrums in some cases, it is not sure that the frequency extracted by STFT in the heartbeat band is the heartbeat frequency. It is necessary to optimize the initial modal frequencies to prevent them from losing the respiratory frequency and the heartbeat frequency. HEAR recovers the initial frequencies of respirations and heartbeats by solving the following quadratic programming issue:
where
is the frequency extracted on ridges in STFT of the vital signal.
is the respiratory frequency and
is the heartbeat frequency.
n,
k,
m and
t are respectively orders of respiratory harmonics and heartbeat harmonics. The lower bound for the vector
to be optimized is set as
, and the upper bound is set as
.
The above optimization assumes that all frequencies extracted from STFT are composed of
kth respiratory harmonics
,
nth heartbeat harmonics
and their intermodulations
. The optimization poses constraints on both harmonic orders and frequencies of respirations and heartbeats. Specifically, values of respiratory harmonics, heartbeat harmonics and their intermodulations are restricted as respectively equal to an extracted frequency in
, as described in formula (16). The optimization is achieved by reducing each discrepancy between the harmonic and the corresponding extracted frequency in
.
Figure 7b illustrates frequencies derived from the STFT in
Figure 7a and estimated by VNCMD.