An Advanced First Aid System Based on an Unmanned Aerial Vehicles and a Wireless Body Area Sensor Network for Elderly Persons in Outdoor Environments
Abstract
:1. Introduction
- (i)
- An advanced first aid system (AFAS) for elderly people in outdoor settings, based on a fall detection device (FDD) and an unmanned aerial vehicle (UAV), was practically implemented.
- (ii)
- A new proposed algorithm, called fall detection based on heart rate threshold (FDB-HRT), was presented to improve fall detection for elderly patients.
- (iii)
- The geolocation error of the fallen patients was improved based on advanced GPS using eight satellites for geolocation.
- (iv)
- Heart rate, fall detection, and GPS measurement accuracy were confirmed based on a statistical analysis.
- (v)
- Compared to delivery via ambulance, the UAV-based first aid kit reduces delivery time to patients.
- (vi)
- The results of this work outperformed similar previous research in terms of heart rate measurement accuracy, fall detection accuracy, UAV time savings and mission success.
2. Related Work
2.1. Work Related to FD Systems
2.2. Work Related to the UAV System
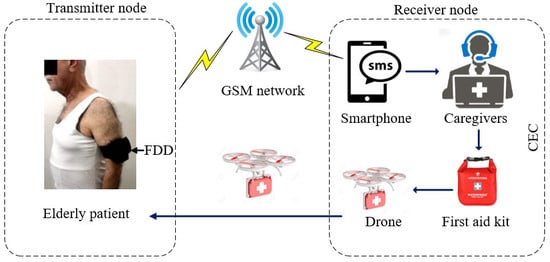
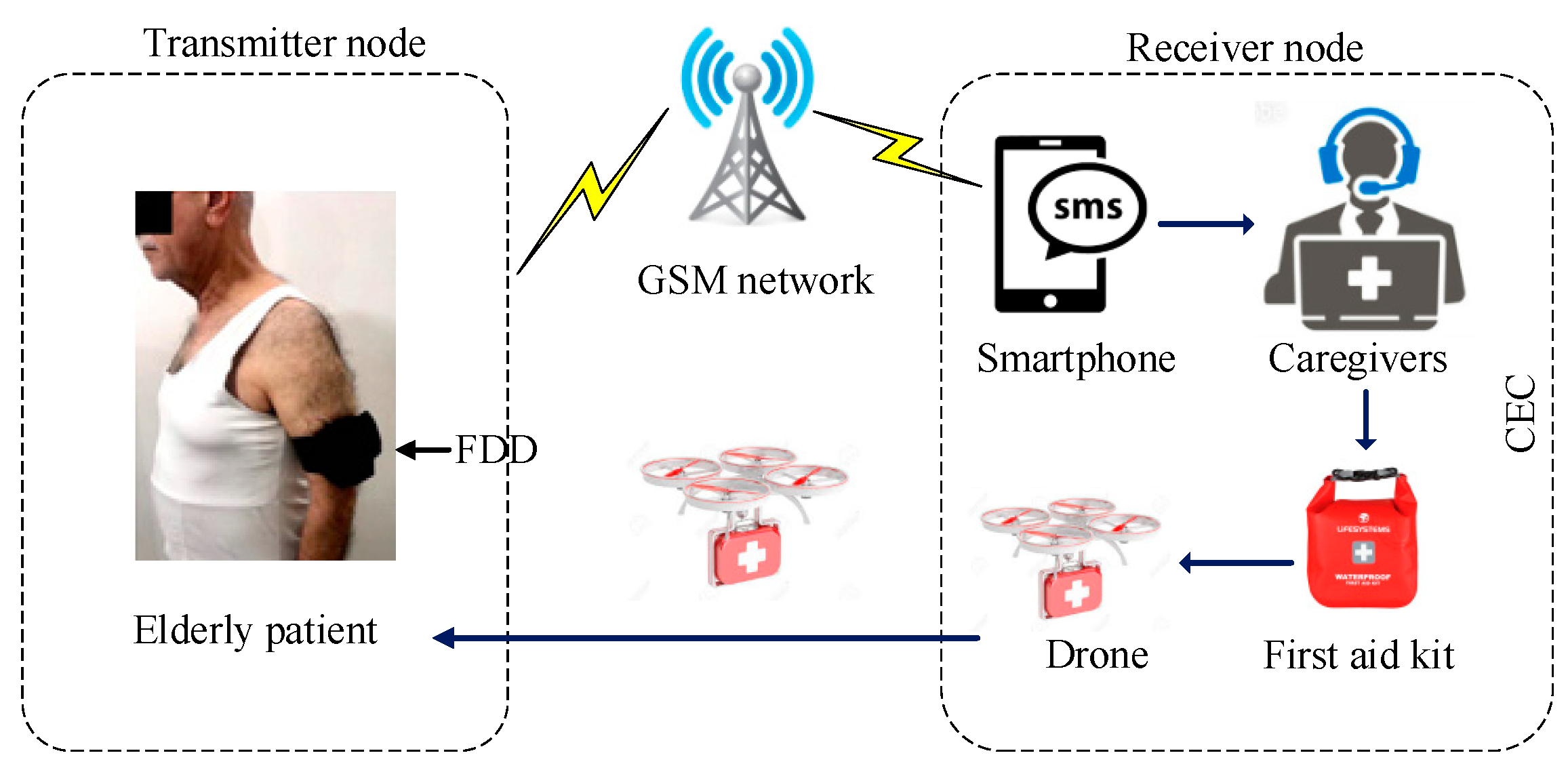
3. System Architecture
3.1. Fall Detection Device (FDD)
3.1.1. Microcontroller
3.1.2. Biomedical Sensors
3.1.3. GSM Module
3.1.4. GPS Module
3.2. Call Emergency Center (CEC)
3.2.1. Smartphone
3.2.2. First Aid Kit
3.2.3. Unmanned Aerial Vehicle
4. Proposed Algorithm
4.1. Fall Detection Algorithm
4.2. CEC Algorithm
5. Experiment Configuration
5.1. Performance Evaluation of FDD
5.1.1. Performance of HB and ACC Sensors
5.1.2. Performance of the FDB-HRT Algorithm
5.1.3. Geolocation Error of the GPS Module
5.1.4. Performance of the GSM Module
5.2. Time Savings of UAV Relative to Ambulance
6. Results and Discussions
6.1. HR Measurements and Static Analysis Results
6.1.1. Mean Absolute Error (MAE)
6.1.2. Histogram Analysis
6.2. Fall Detection Accuracy Validation
6.3. Measurements of FDB-HRT Algorithm
6.4. GPS Measurement and Accuracy of Geolocations
6.5. Testing of Information Delivery
6.6. Time Savings of UAV Relative to Ambulance
6.7. Battery Life Estimation of the FDD
7. Comparison of Results with Previous Work
7.1. Comparison of Heart Rate Measurement Accuracy
7.2. Comparison of Fall Detection Accuracy
7.3. Comparison of Response Time
7.4. Comparison of Transmission Information Accuracy
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bergen, G.; Stevens, M.R.; Burns, E.R. Falls and Fall Injuries Among Adults Aged ≥65 Years—United States, 2014. Morb. Mortal. Wkly. Rep. 2016, 65, 993–998. [Google Scholar] [CrossRef] [PubMed]
- WISQARS (Web-Based Injury Statistics Query and Reporting System). Injury Center CDC. Available online: https://www.cdc.gov/injury/wisqars/ (accessed on 19 March 2019).
- Florence, C.S.; Bergen, G.; Atherly, A.; Burns, E.; Stevens, J.; Drake, C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J. Am. Geriatr. Soc. 2018, 66, 693–698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falls May Be Tied to Irregular Heartbeat. Available online: https://www.reuters.com/article/us-health-falls-atrial-fibrillation/falls-may-be-tied-to-irregular-heartbeat-idUSKBN0M91LC20150313 (accessed on 19 March 2019).
- Yan, H.; Xu, L.D.; Bi, Z.; Pang, Z.; Zhang, J.; Chen, Y. An Emerging Technology—Wearable Wireless Sensor Networks with Applications in Human Health Condition Monitoring. J. Manag. Anal. 2015, 2, 121–137. [Google Scholar] [CrossRef]
- Pittet, V.; Burnand, B.; Yersin, B.; Carron, P.N. Trends of pre-hospital emergency medical services activity over 10 Years: a population-based registry analysis. BMC Health Serv. Res. 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhang, Z.; Li, B.; Lee, S.; Sherratt, R. An Enhanced Fall Detection System for Elderly Person Monitoring Using Consumer Home Networks. IEEE Trans. Consum. Electron. 2014, 60, 23–29. [Google Scholar] [CrossRef]
- Mezghani, N.; Ouakrim, Y.; Islam, M.R.; Yared, R.; Abdulrazak, B. Context Aware Adaptable Approach for Fall Detection Bases on Smart Textile. In Proceedings of the 2017 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI), Orlando, FL, USA, 16–19 February 2017. [Google Scholar]
- Cheng, J.; Chen, X.; Shen, M. A Framework for Daily Activity Monitoring and Fall Detection Based on Surface Electromyography and Accelerometer Signals. IEEE J. Biomed. Heal. Inform. 2013, 17, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Fakhri, A.B.; Gharghan, S.K.; Mohammed, S.L. Statistical Validation of Patient Vital Signs Based on Energy-efficient wireless sensor network monitoring system. ARPN J. Eng. App. Sci. 2018, 13, 8258–8270. [Google Scholar]
- Delahoz, Y.S.; Labrador, M.A. Survey on Fall Detection and Fall Prevention Using Wearable and External Sensors. Sensors 2014, 14, 19806–19842. [Google Scholar] [CrossRef] [Green Version]
- Kumar, G.D.; Jeeva, B. Drone Ambulance for Outdoor Sports. Asian J. Appl. Sci. and Technol. 2017, 1, 44–49. [Google Scholar]
- Patel, S.; Lorincz, K.; Hughes, R.; Huggins, N.; Growdon, J.; Standaert, D.; Akay, M.; Dy, J.; Welsh, M.; Bonato, P.; et al. Monitoring Motor Fluctuations in Patients With Parkinson ’ s Disease Using Wearable Sensors. IEEE Trans. Inf. Technol. Biomed. 2009, 13, 864–873. [Google Scholar] [CrossRef]
- Wang, D.; Liu, Y.; Jiang, M. Review on Emergency Medical Response against Terrorist Attack. Mil. Med. Res. 2014, 1, 9. [Google Scholar] [CrossRef] [PubMed]
- Autopilot Hangar. Available online: https://autoflight.hangar.com/ (accessed on 29 March 2019).
- Kantoch, E.; Augustyniak, P.; Markiewicz, M.; Prusak, D. Monitoring Activities of Daily Living Based on Wearable Wireless Body Sensor Network. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014. [Google Scholar]
- Hsieh, S.L.; Chen, C.C.; Wu, S.H.; Yue, T.W. A Wrist -Worn Fall Detection System Using Accelerometers and Gyroscopes. In Proceedings of the 11th IEEE International Conference on Networking, Sensing and Control, Miami, FL, USA, 7–9 April 2014. [Google Scholar]
- Wu, F.; Zhao, H.; Zhao, Y.; Zhong, H. Development of a Wearable-Sensor-Based Fall Detection System. Int. J. Telemed. Appl. 2015, 2015, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, C.; Lu, W.; Redmond, S.J.; Stevens, M.C.; Lord, S.R.; Lovell, N.H. A Low-Power Fall Detector Balancing Sensitivity and False Alarm Rate. IEEE J. Biomed. Heal. Inform. 2018, 22, 1929–1937. [Google Scholar] [CrossRef] [PubMed]
- Gharghan, S.K.; Mohammed, S.L.; Al-Naji, A.; Abu-AlShaeer, M.J.; Jawad, H.M.; Jawad, A.M.; Chahl, J. Accurate Fall Detection and Localization for Elderly People Based on Neural Network and Energy-Efficient Wireless Sensor Network. Energies 2018, 11, 2866. [Google Scholar] [CrossRef]
- Wang, Z.; Zhao, C.; Qiu, S. A System of Human Vital Signs Monitoring and Activity Recognition Based on Body Sensor Network. Sens. Rev. 2014, 34, 42–50. [Google Scholar] [CrossRef]
- Kakria, P.; Tripathi, N.K.; Kitipawang, P. A Real-Time Health Monitoring System for Remote Cardiac Patients Using Smartphone and Wearable Sensors. Int. J. Telemed. Appl. 2015, 2015, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Depari, A.; Flammini, A.; Bellagente, P.; Sisinni, E.; Crema, C.; Vezzoli, A. Virtual Respiratory Rate Sensors: An Example of A Smartphone-Based Integrated and Multiparametric MHealth Gateway. IEEE Trans. Instrum. Meas. 2017, 66, 2456–2463. [Google Scholar]
- Modeling, T.; Algorithm, F.; Nosrati, M.; Member, S.; Tavassolian, N. High-Accuracy Heart Rate Variability Monitoring Using Doppler Radar Based on Gaussian Pulse. IEEE Trans. Microw. Theory Tech. 2018, 66, 556–567. [Google Scholar]
- Baba, E.; Jilbab, A.; Hammouch, A. A Health Remote Monitoring Application Based on Wireless Body Area Networks. In Proceedings of the 2018 International Conference on Intelligent Systems and Computer Vision (ISCV), Fez, Morocco, 2–4 April 2018. [Google Scholar]
- Lim, D.; Park, C.; Kim, N.H.; Kim, S.H.; Yu, Y.S. Fall-Detection Algorithm Using 3-Axis Acceleration: Combination with Simple Threshold and Hidden Markov Model. J. Appl. Math. 2014. [Google Scholar] [CrossRef]
- Hollenberg, J.; Österberg, S.; Rosenqvist, M.; Djarv, T.; Claesson, A.; Ban, Y.; Ringh, M.; Fredman, D.; Nordberg, P.; Lennartsson, J.; et al. Unmanned Aerial Vehicles (Drones) in out-of-Hospital-Cardiac-Arrest. Scand. J. Trauma. Resusc. Emerg. Med. 2016, 24, 1–9. [Google Scholar]
- Dayananda, K.R.; Gomes, R.; Straub, J. An Interconnected Architecture for an Emergency Medical Response Unmanned Aerial System. In Proceedings of the 2017 IEEE/AIAA 36th Digital Avionics Systems Conference (DASC), St. Petersburg, FL, USA, 17–21 September 2017. [Google Scholar]
- Pulver, A.; Wei, R.; Mann, C. Locating AED Enabled Medical Drones to Enhance Cardiac Arrest Response Times. Prehospital Emerg. Care 2016, 20, 378–389. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Han, S.; Xiao, J.; Hu, X.; Fan, J. Optik Error Compensation Based on BP Neural Network for Airborne Laser Ranging. Opt. Int. J. Light Electron. Opt. 2016, 127, 4083–4088. [Google Scholar] [CrossRef]
- Gautam, S.A. Path Planning for Unmanned Aerial Vehicle Based on Genetic Algorithm & Artificial Neural Network in 3D. In Proceedings of the 2014 International Conference on Data Mining and Intelligent Computing (ICDMIC), New Delhi, India, 5–6 September 2014. [Google Scholar]
- Roberge, V.; Tarbouchi, M.; Labonté, G. Comparison of Parallel Genetic Algorithm and Particle Swarm Optimization for Real-Time UAV Path Planning. IEEE Trans. Ind. Inf. 2013, 9, 132–141. [Google Scholar] [CrossRef]
- Thiels, C.A.; Aho, J.M.; Zietlow, S.P.; Jenkins, D.H. Use of Unmanned Aerial Vehicles for Medical. Air Med. J. 2015, 34, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Member, S.; Ding, X.; Chung, C.; Poon, Y.; Ping, B.; Lo, L.; Zhang, H.; Zhou, X.; Yang, G.; et al. Unobtrusive Sensing and Wearable Devices for Health Informatics. IEEE Trans. Biomed. Eng. 2014, 61, 1538–1554. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://cdn.sparkfun.com/datasheets/Dev/Arduino/Boards/ProMini16MHzv1.pdf (accessed on 4 March 2019).
- Ali, A.S.; Zanzinger, Z.; Debose, D.; Stephens, B. Open Source Building Science Sensors (OSBSS): A Low-Cost Arduino-Based Platform for Long-Term Indoor Environmental Data Collection. Build. Env. 2016, 100, 114–126. [Google Scholar] [CrossRef]
- Butca, C.G.; Suciu, G.; Ochian, A.; Fratu, O.; Halunga, S. Wearable Sensors and Cloud Platform for Monitoring Environmental Parameters in E-Health Applications. In Proceedings of the 2014 11th International Symposium on Electronics and Telecommunications (ISETC), Timisoara, Romania, 14–15 November 2014. [Google Scholar]
- Kirichek, R.; Transmission, D.; Node, S. The Model of Data Delivery from the Wireless Body Area Network to the Cloud Server with the Use of Unmanned Aerial Vehicles. In Proceedings of the 30th European Conference on Modelling and Simulation, Regensburg, Germany, 31 May–3 June 2016. [Google Scholar]
- Mubashir, M.; Shao, L.; Seed, L. Neurocomputing A Survey on Fall Detection: Principles and Approaches. Neurocomputing 2013, 100, 144–152. [Google Scholar] [CrossRef]
- Vikneswaran, S. Elder Monitoring Using Gsm and Gps with an Enhanced Fall Detection System. Int. J. Adv. Res. Sci. Eng. 2015, 8354, 409–416. [Google Scholar]
- Rihana, S.; Mondalak, J. Wearable Fall Detection System. In Proceedings of the 2016 3rd Middle East Conference on Biomedical Engineering (MECBME), Beirut, Lebanon, 6–7 October 2016. [Google Scholar]
- Gia, T.N.; Tcarenko, I.; Sarker, V.K.; Rahmani, A.M.; Westerlund, T.; Liljeberg, P.; Tenhunen, H. IoT-Based Fall Detection System with Energy Efficient Sensor Nodes. In Proceedings of the IEEE Nordic Circuits and Systems (Norcas’16), Copenhagen, Denmark, 1–2 November 2016. [Google Scholar]
- Ning, J. Detecting Human Falls with a 3-Axis Digital Accelerometer. Analog Dialogue 2009, 2009, 3–9. [Google Scholar]
- Adxl345. Available online: http://www.analog.com (accessed on 12 April 2019).
- Desima, M.A.; Ramli, P.; Ramdani, D.F.; Rahman, S. Alarm System to Detect the Location of IOT-Based Public Vehicle Accidents. In Proceedings of the 2017 International Conference on Computing, Engineering, and Design (ICCED), Kuala Lumpur, Malaysia, 23–25 November 2017. [Google Scholar]
- Schwarzmeier, A.; Besser, J.; Weigel, R.; Fischer, G.; Kissinger, D. A Compact Back-Plaster Sensor Node for Dementia and Alzheimer Patient Care. In Proceedings of the 2014 IEEE Sensors Applications Symposium (SAS), Queenstown, New Zealand, 18–20 February 2014. [Google Scholar]
- Tarapiah, S. Smart Real-Time Healthcare Monitoring and Tracking System Using GSM/GPS Technologies. Int. J. Comput. Appl. 2016, 142, 19–26. [Google Scholar] [CrossRef]
- SIMCom. SIM800L_Hardware_Design_V1.00. 2013, pp. 1–70. Available online: https://img.filipeflop.com/files/download/Datasheet_SIM800L.pdf (accessed on 10 September 2018).
- M10 Quectel Cellular Engine AT Commands Set Document Title: M10 AT Commands Set. Available online: https://www.arduino.cc/en/uploads/Main/Quectel_M10_AT_commands.pdf (accessed on 4 November 2018).
- Borle, V.S.; Kulkarni, P.S.N. An Enhanced Fall Detection System with GSM and GPS Technology. Int. Adv. Res. J.Sci. Eng. Technol. 2016, 4, 345–348. [Google Scholar]
- Tahar, K.N.; Kamarudin, S.S.; Ehsan, S.D. UAV Onboard GPS in Positioning Determination; ISPRS—International Archives of the Photogrammetry, Remote Sensing and Spatial Information Sciences: Hannover, Germany, 2016; Volume XLI, pp. 1037–1042. [Google Scholar]
- Skoglund, M.; Petig, T.; Vedder, B.; Eriksson, H.; Schiller, E.M. Static and Dynamic Performance Evaluation of Low-Cost RTK GPS Receivers. In Proceedings of the 2016 IEEE Intelligent Vehicles Symposium (IV), Gothenburg, Sweden, 19–22 June 2016. [Google Scholar]
- NEO-M8 u-Blox M8 Concurrent GNSS Modules Data Sheet Highlights. Available online: https://www.u-blox.com/sites/default/files/NEO-M8-FW3_DataSheet_%28UBX-15031086%29.pdf (accessed on 27 March 2019).
- Flight School Autopilot. Available online: https://autoflight.hangar.com/autopilot/flightschool#mode-waypoint.html (accessed on 23 June 2019).
- Kim, S.J.; Lim, G.J.; Cho, J.; Cote, M.J. Drone-Aided Healthcare Services for Patients with Chronic Diseases in Rural Areas. J. Intell. Robotic Syst. 2017, 88, 163–180. [Google Scholar] [CrossRef]
- Drone Controller. Available online: https://www.getfpv.com/radios/radio-controllers.html (accessed on 20 May 2019).
- What is a Drone?—Unmanned Aircraft Technology Explained Space. Available online: https://www.space.com/29544-what-is-a-drone.html (accessed on 4 April 2019).
- Phantom 3 Professional—Let Your Creativity Fly with a 4K Camera in the Sky—DJI. Available online: https://www.dji.com/phantom-3-pro (accessed on 9 May 2019).
- Using Waypoints to Do More with Your Drone. Autel Robotics. Available online: https://www.autelrobotics.com/blog /using-waypoints-to-do-more-with-your-drone/ (accessed on 4 April 2019).
- How to Use DJI’s Return to Home (RTH) Safely—DJI Guides. Available online: https://store.dji.com/guides/how-to-use-the-djis-return-to-home/ (accessed on 4 April 2019).
- Verified Reviews®—Home. Available online: http://www.medrounds.org/main/ (accessed on 5 April 2019).
- The Heart Rate in the Elderly. Livestrong.com. Available online: https://www.livestrong.com/article/365449-the-heart-rate-in-the-elderly/ (accessed on 5 April 2019).
- IntelliVue MP40/MP50 Patient Monitor Philips M8003A, M8004A Technical Data Sheet. Available online: http://www.medtechnica.co.il/files/Monitors%20and%20Defibrilators/IntelliVue_MP40_50_Patient_Monitor.pdf (accessed on 7 April 2019).
- El Ghzizal, A.; Motahhir, S.; Derouich, A.; El Hammoumi, A.; Chalh, A. Low-Cost Virtual Instrumentation of PV Panel Characteristics Using Excel and Arduino in Comparison with Traditional Instrumentation. Renew. Wind Water Sol. 2018, 5. [Google Scholar]
- GPS Coordinates, Latitude and Longitude with Google Maps. Available online: https://www.gps-coordinates.net/ (accessed on 28 April 2019).
- Fouad, H.; Farouk, H. Heart Rate Sensor Node Analysis for Designing Internet of Things Telemedicine Embedded System. Cogent Eng. 2017, 4, 1–12. [Google Scholar] [CrossRef]
- Tarvainen, M.P.; Niskanen, J.P.; Lipponen, J.A.; Ranta-aho, P.O.; Karjalainen, P.A. Kubios HRV—Heart Rate Variability Analysis Software. Comput. Methods Programs Biomed. 2014, 113, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Melillo, P.; Santoro, D.; Vadursi, M. Detection and Compensation of Interchannel Time Offsets in Indirect Fetal ECG Sensing. IEEE Sens. J. 2014, 14, 2327–2334. [Google Scholar] [CrossRef]
- Valdés, S.O.; Miyake, C.Y.; Niu, M.C.; Caridad, M.; Asaki, S.Y.; Landstrom, A.P.; Schneider, A.E.; Rusin, C.G.; Patel, R.; Lam, W.W. Early experience with intravenous sotalol in children with and without congenital heart disease. Heart Rhythm 2018, 15, 1862–1869. [Google Scholar] [CrossRef] [PubMed]
- Aguiar, B.; Rocha, T.; Silva, J.; Sousa, I. Accelerometer-Based Fall Detection for Smartphones. In Proceedings of the 2014 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Lisboa, Portugal, 11–12 June 2014. [Google Scholar]
- Andayani, U.; Fahmi, F.; Seniman; Siregar, B.; Bahri, R.P. Real-Time Monitoring System for Elderly People in Detecting Falling Movement Using Accelerometer and Gyroscope. J. Phys. Conf. Ser. 2018, 978, 012110. [Google Scholar]


















| Parameters | Standard Values [43] | Selected Threshold Values of FDB-HRT Algorithm |
|---|---|---|
| FAMt | 0.313–0.563 (g) | 0.5 (g) |
| FTt | 20–70 (ms) | 40 (ms) |
| AAMt | >2 (g) | 2.5 (g) |
| Type | Experiment Test |
|---|---|
| F1 | Forward fall, lying on ground |
| F2 | Fall to the right, lying on ground |
| F3 | Backward fall from a seated position on a chair |
| F4 | Forward fall, landing on knees |
| NA1 | Walking |
| NA2 | Ascending stairs |
| NA3 | Descending stairs |
| NA3 | Sitting on chair |
| Type | Experiment Test | Test Result |
|---|---|---|
| F1 | Forward fall, lying on ground | 15/15 |
| F2 | Fall to the right, lying on ground | 15/15 |
| F3 | Backward fall from a seated position on a chair | 14/15 |
| F4 | Forward fall, landing on knees | 15/15 |
| NA1 | Walking | 15/15 |
| NA2 | Ascending stairs | 15/15 |
| NA3 | Descending stairs | 15/15 |
| NA3 | Sitting on chair | 16/15 |
| Location | Arrival Time of UAV (s) | Arrival Time of Ambulance (s) | Savings Time (s) |
|---|---|---|---|
| Locations 1 and 2 | 210 | 300 | 90 (based on Equation (2)) |
| Locations 3 and 4 | 240 | 360 | 120 (based on Equation (2)) |
| Average time (s) | 225 | 330 | |
| Average time savings = 105 s (based on Equation (3)) | |||
| Percentage of time saved = 31.81% (based on Equation (5)) | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fakhrulddin, S.S.; Gharghan, S.K.; Al-Naji, A.; Chahl, J. An Advanced First Aid System Based on an Unmanned Aerial Vehicles and a Wireless Body Area Sensor Network for Elderly Persons in Outdoor Environments. Sensors 2019, 19, 2955. https://doi.org/10.3390/s19132955
Fakhrulddin SS, Gharghan SK, Al-Naji A, Chahl J. An Advanced First Aid System Based on an Unmanned Aerial Vehicles and a Wireless Body Area Sensor Network for Elderly Persons in Outdoor Environments. Sensors. 2019; 19(13):2955. https://doi.org/10.3390/s19132955
Chicago/Turabian StyleFakhrulddin, Saif Saad, Sadik Kamel Gharghan, Ali Al-Naji, and Javaan Chahl. 2019. "An Advanced First Aid System Based on an Unmanned Aerial Vehicles and a Wireless Body Area Sensor Network for Elderly Persons in Outdoor Environments" Sensors 19, no. 13: 2955. https://doi.org/10.3390/s19132955
APA StyleFakhrulddin, S. S., Gharghan, S. K., Al-Naji, A., & Chahl, J. (2019). An Advanced First Aid System Based on an Unmanned Aerial Vehicles and a Wireless Body Area Sensor Network for Elderly Persons in Outdoor Environments. Sensors, 19(13), 2955. https://doi.org/10.3390/s19132955