Medical Robotics in Bone Fracture Reduction Surgery: A Review
Abstract
:1. Introduction
- (1)
- Preoperative scan to analyze the fracture and determine the treatment plan accordingly;
- (2)
- Aligning the fracture segment;
- (3)
- Diagnosing the reduction situation;
- (4)
- Fixing the aligned fracture segments with internal/external fixation;
- (5)
- Postoperative recovery.
- (a)
- Low accuracy, as it is largely dependent on doctor experience;
- (b)
- The manual reduction method requires strong physical strength from the surgeons;
- (c)
- Large external fixation frame is not convenient for postoperative recovery;
- (d)
- Time-consuming during the workflow;
- (e)
- Open surgery causes greater trauma and would damage soft tissues and blood supply, which would lead to a high margin of nonunion and delayed union [6].
- (a)
- High precision;
- (b)
- Large force/torque;
- (c)
- Low effect of radiation;
- (d)
- Time reduction during the workflow.
- (1)
- Ranked the results by relevance (use an algorithm provided by Google);
- (2)
- Divided the past 15 years into three periods, and selected the top 2% articles related to each keyword within each period;
- (3)
- Excluded those articles which do not include “robots” or “medical devices” (e.g., literature that performed case analysis, describing surgical improvements) with brief review.
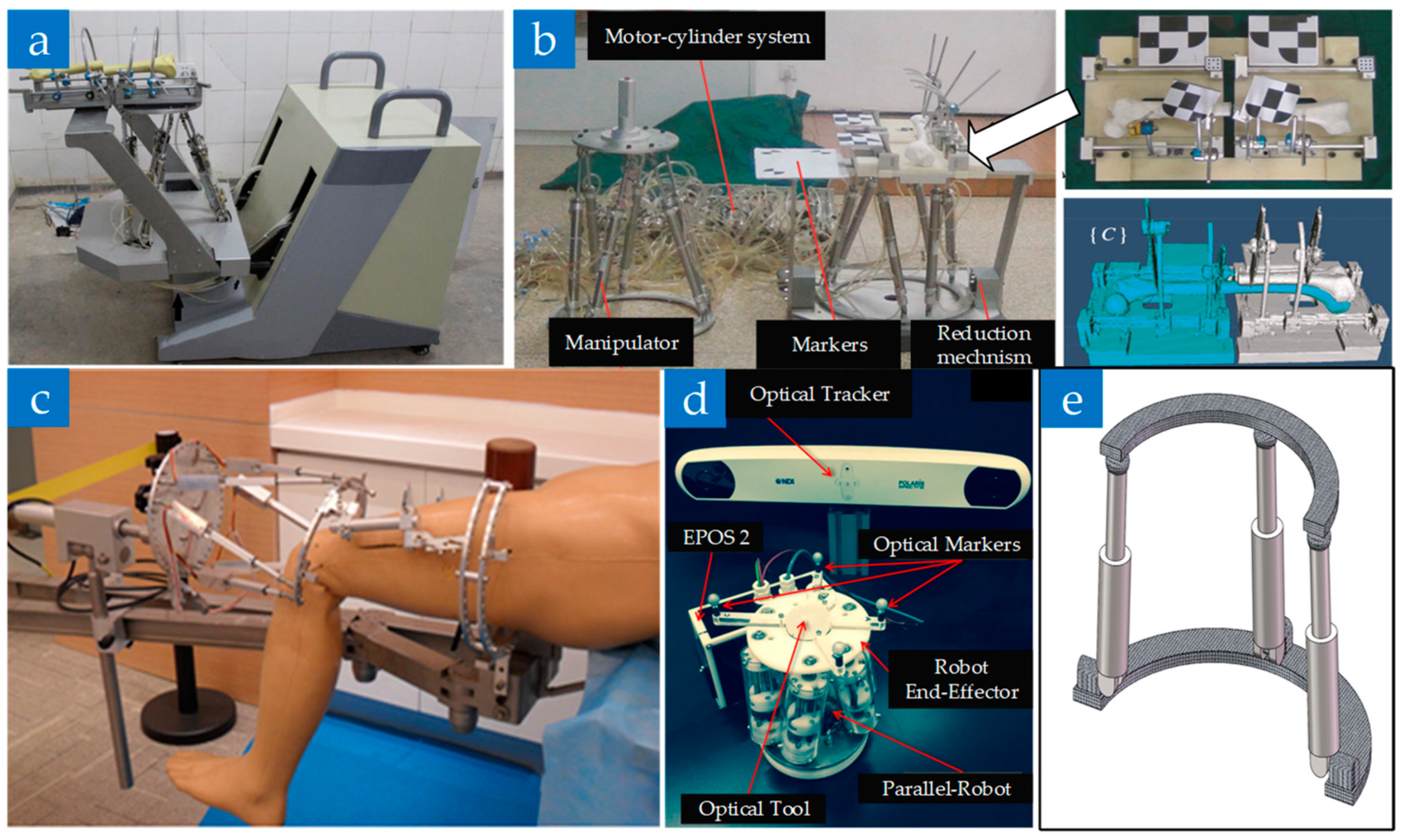
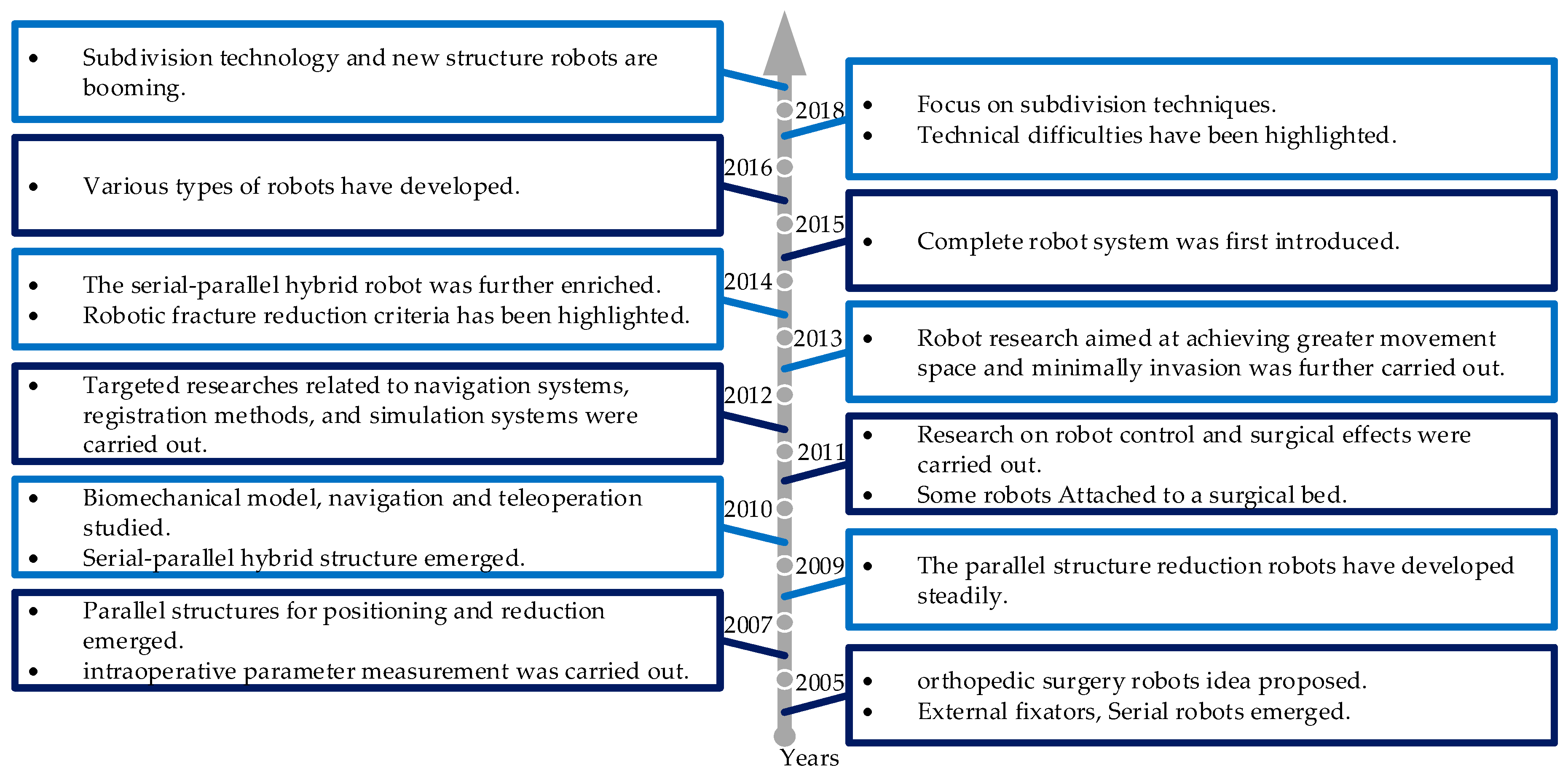
2. The Structure of Fracture Reduction Surgery Robot
- (a)
- Based on the external fixed frame structure;
- (b)
- Based on the serial structure of the industrial robot;
- (c)
- Parallel structure;
- (d)
- Serial-parallel hybrid structure.
2.1. Robot Based on the External Fixed Frame Structure
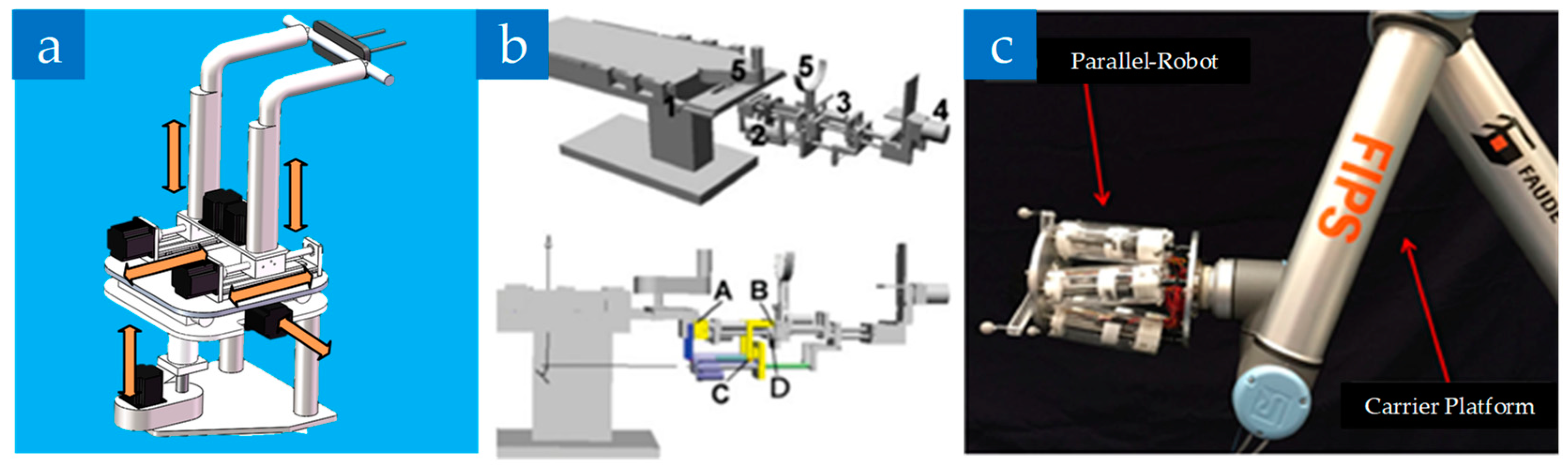
2.2. Robot Based on the Serial Structure of the Industrial Robot
2.3. Robot based on the Parallel Structure
2.4. Robot Based on the Serial-Parallel Hybrid Structure
2.5. Comparison of Different Types of Reduction Robots
- (a)
- The reduction robot based on the external fixed frame structure was first studied because of its lowest transformation cost, but its robotic operation in the form of a unilateral fixed frame is not good.
- (b)
- The serial robot: is almost no longer studied after 2012 due to their obvious disadvantages.
- (c)
- The parallel robot: some were developed from Stewart-structured external fixed frame robot. With the development of navigation technology, the parallel robots are gradually combined with other equipment/technology to form a complete fracture surgery robot system. The parallel structure is also the optional structure that is used to form a more comprehensive fracture reduction surgical robot system.
- (d)
- The serial-parallel hybrid structure: has gradually become the mainstream of research in this field due to its advantages.
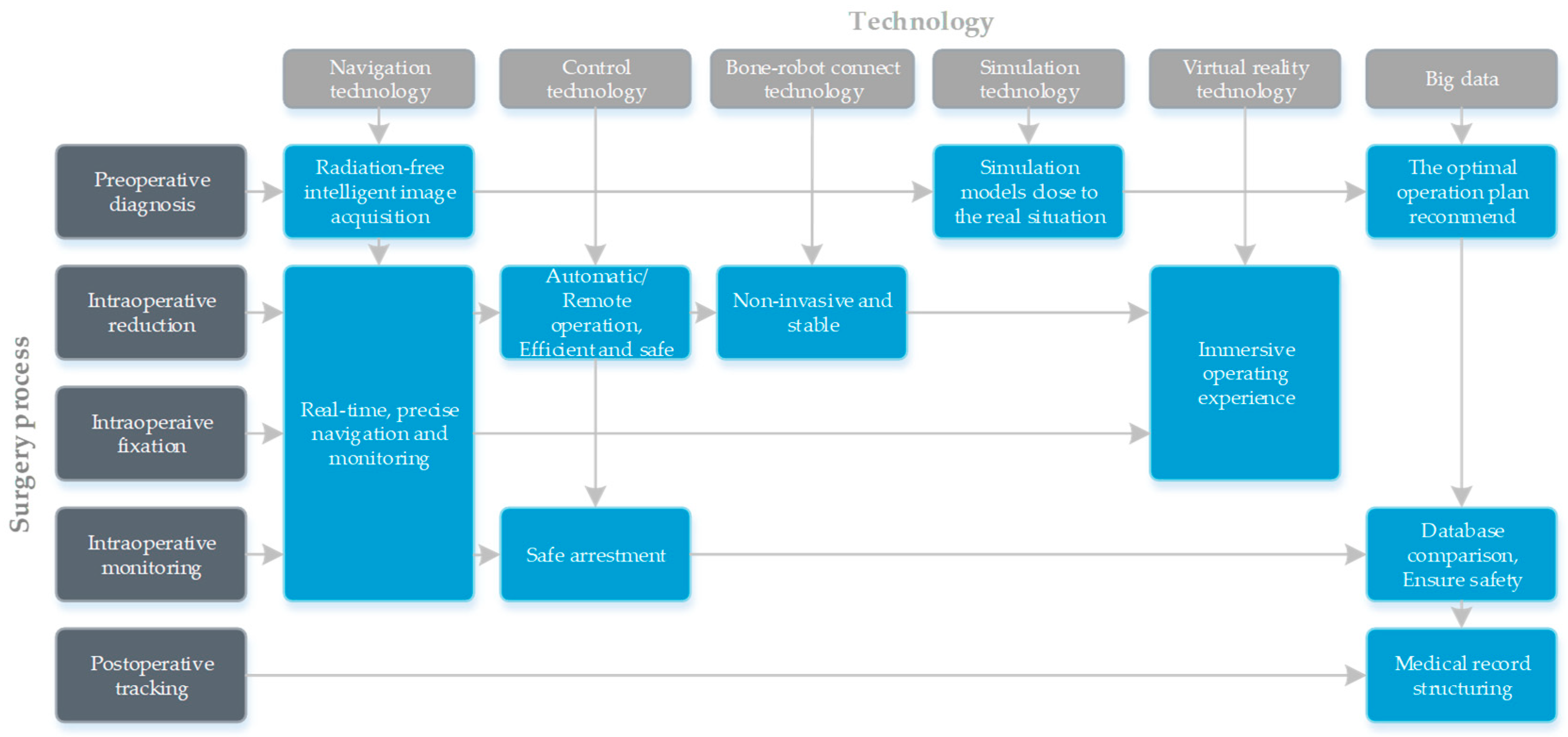
3. The Assistive Technologies of Fracture Reduction Surgery Robot
- (1)
- A scanning diagnosis of the preoperative fracture site is performed, then a three-dimensional image of the reconstructed fracture segment is obtained by processing data, and the coordinate system information between the robot and the fracture segment is obtained by the navigation system.
- (2)
- Calculating the transformation matrix of the robot’s current pose to the target pose through computer algorithm. Then, the path planning is carried out according to the surgical principle.
- (3)
- The robot is automatically or controlled by the surgeon to conduct the reduction.
- (4)
- Effective fixing is necessary after the above operations. It may be slightly different in different systems.
- (a)
- The navigation and the path planning technology play a decisive role;
- (b)
- It can realize low radiation during surgery;
- (c)
- Good interaction (for example, controlling a robot just by clicking a mouse) can help the surgeon complete the surgery more comfortably;
- (d)
- A key issue in robotic orthopedic surgery is the bone–robot connection problem, which involves the size of the wound and the reliability of robotic procedure.
3.1. Navigation Technology
- (a)
- CT navigation: can obtain the high-precision tomographic data of the bone tissue. By the image processing technology, the fracture site can be reconstructed and displayed by a visual image. However, CT scanning is a relatively high-dose procedure [74].
- (b)
- Perspective navigation: uses C-arm, G-arm, or O-arm for image acquisition, which is of high real-time performance. Compared to the 2D perspective, the 3D perspective navigation can provide preciser pre-operative planning and 3D visualization during surgery [83], which has been widely used in surgery. However, due to the volume effect, the three-dimensional image obtained is less effective than that obtained by the CT.
- (c)
- Ultrasonic navigation (based on ultrasound imaging): is an emerging technology, the biggest advantage of which is non-invasive. However, it may be interfered by different factors, such as ultrasonic speed, distance, tissue deformation, etc.
- (d)
- Electromagnetic navigation: besides being non-invasive, the biggest advantage compared to optical tracking is that it is not limited by occlusions of the visual field. However, it will be affected by the surrounding electromagnetic fields and metal medical equipment.
- (e)
- Imageless navigation (optical tracking): refers to the establishment of a virtual representation of a surgical object by determining different anatomical structures and reference marks via a photoelectric tracking system. However, in minimally invasive surgery for fracture reduction, the reference marker will cause extra trauma to the patient.
3.2. Robot Control and Interaction Technology
3.3. Bone–Robot Connection Technology
- (a)
- The external fixation pin or the screw connection;
- (b)
- The connection through the foot boots.
4. Discussion
4.1. Current Difficulties in Fracture Reduction Robot Research
- (a)
- The lack of consideration in realistic biomechanical characters. The human biomechanical model is very complicated. Although Du Z. et al. [92] established a robot model via geometry and dynamics analysis, and Wang M. et al. [93] proposed a tissue dual mechanical model, their studies are only limited in rare cases. The current research in realistic biomechanical characters cannot provide fracture reduction surgery robots with sufficient support to carry out better path planning and other operations.
- (b)
- Not cost-effective. Most of the fracture reduction robots in current study can only perform some simple supportive operations (some even needs the help of traction equipment), while the cost is pretty high.
4.2. Trends and Conjectures
- (a)
- The dexterous five-finger/three-finger manipulator that simulates the rigid-flexible combination of human hands can be used in a reduction robot to achieve a non-invasive bone–robot connection by grasping.
- (b)
- Variable stiffness model (such as the variable stiffness device in Reference [94] achieves stiffness changes by vacuum/non-vacuum control) can be used to design the contact components of the robotic end-connecting device, and to achieve stable bone–robot connection.
- (a)
- Individuation. The operating system may consider more about the surgeons’ habits, and the hardware that is in direct contact with the surgeon may be designed as a modular part that can be personalized as needed.
- (b)
- Virtual reality. By virtual reality technology, surgeons can operate remotely or guide surgery, and can obtain accurate surgical perception in virtual reality. In particular, breakthroughs in the reconstruction of patients’ fracture sites in virtual space will contribute to the ultimate realization of virtual reality operations.
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wang, Y. Campbell’s Operative Orthopaedics, 13th ed.; Peking University Medical Press: Beijing, China, 2009. [Google Scholar]
- Court-Brown, C.M.; Caesar, B. Epidemiology of adult fractures: A review. Injury 2006, 37, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, M.; Guyatt, G.H.; Swiontkowski, M.F.; Tornetta, P., III; Hanson, B.; Weaver, B.; Sprague, S.; Schemitsch, E.H. Surgeons’ preferences for the operative treatment of fractures of the tibial shaft: An international survey. JBJS 2001, 83, 1746–1752. [Google Scholar] [CrossRef] [PubMed]
- Kenwright, J.; Richardson, J. The biology of fracture repair and the role of dynamization. In Orthofix External Fixation in Trauma and Orthopaedics; Springer: Berlin/Heidelberg, Germany, 2000; pp. 8–17. [Google Scholar]
- Leunig, M.; Hertel, R.; Siebenrock, K.A.; Ballmer, F.T.; Mast, J.W.; Ganz, R. The evolution of indirect reduction techniques for the treatment of fractures. Clin. Orthop. Relat. Res. 2000, 375, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Kolodziej, P.; Lee, F.S.; Patel, A.; Kassab, S.S.; Shen, K.-L.; Yang, K.H.; Mast, J.W. Biomechanical evaluation of the schuhli nut. Clin. Orthop. Relat. Res. 1998, 347, 79–85. [Google Scholar] [CrossRef]
- Kempf, I.; Grosse, A.; Beck, G. Closed locked intramedullary nailing. Its application to comminuted fractures of the femur. JBJS 1985, 67, 709–720. [Google Scholar] [CrossRef]
- Westphal, R.; Winkelbach, S.; Gösling, T.; Hüfner, T.; Faulstich, J.; Martin, P.; Krettek, C.; Wahl, F. A surgical telemanipulator for femur shaft fracture reduction. Int. J. Med. Robot. Comput. Assist. Surg. 2006, 2, 238–250. [Google Scholar] [CrossRef]
- Wang, J.-Q.; Wang, J.-F.; Hu, L.; Su, Y.-G.; Wang, Y.; Zhao, C.-P.; Zhou, L.; Wang, T.-M.; Wang, M.-Y. Effects of medical robot-assisted surgical navigation system in distal locking of femoral intramedullary nails: An experimental study. Zhonghua Yi Xue Za Zhi 2006, 86, 614–618. [Google Scholar]
- Sun, X. Development of A Robot-assisted System for Femoral Shaft Fracture Reduction. Master’s Thesis, Southeast University, Nanjing, China, 2016. [Google Scholar]
- Kwoh, Y.S.; Hou, J.; Jonckheere, E.A.; Hayati, S. A robot with improved absolute positioning accuracy for ct guided stereotactic brain surgery. IEEE Trans. Biomed. Eng. 1988, 35, 153–160. [Google Scholar] [CrossRef]
- Kim, H.L.; Schulam, P. The PAKY, HERMES, AESOP, ZEUS, and da Vinci robotic systems. Urol. Clin. N. Am. 2004, 31, 659–669. [Google Scholar] [CrossRef]
- Fu, Y.; Li, H. Master-slave control technology research for abdominal minimally invasive surgery robot. In Proceedings of the Asme International Mechanical Engineering Congress and Exposition 2010, Vancouver, BC, Canada, 12–18 November 2010; Volume 2. [Google Scholar]
- Bauzano, E.; Garcia-Morales, I.; del Saz-Orozco, P.; Fraile, J.C.; Munoz, V.F. A minimally invasive surgery robotic assistant for HALS-SILS techniques. Comput. Methods Programs Biomed. 2013, 112, 272–283. [Google Scholar] [CrossRef]
- Wilson, J.T.; Gerber, M.J.; Prince, S.W.; Chen, C.-W.; Schwartz, S.D.; Hubschman, J.-P.; Tsao, T.-C. Intraocular robotic interventional surgical system (IRISS): Mechanical design, evaluation, and master-slave manipulation. Int. J. Med. Robot. Comput. Assist. Surg. 2018, 14, e1842. [Google Scholar] [CrossRef]
- Bai, L.; Yang, J.; Chen, X.; Jiang, P.; Liu, F.; Zheng, F.; Sun, Y. Solving the Time-Varying Inverse Kinematics Problem for the Da Vinci Surgical Robot. Appl. Sci. 2019, 9, 546. [Google Scholar] [CrossRef]
- Chung, G.B.; Lee, S.G.; Oh, S.M.; Yi, B.-J.; Kim, W.K.; Kim, Y.S.; Park, J.; Oh, S.H. Development of SPINEBOT for spine surgery. In Proceedings of the 2004 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS)(IEEE Cat. No. 04CH37566), Sendai, Japan, 28 September–2 October 2004; pp. 3942–3947. [Google Scholar]
- Gosling, T.; Westphal, R.; Hufner, T.; Faulstich, J.; Kfuri, M.; Wahl, F.; Krettek, C. Robot-assisted fracture reduction: A preliminary study in the femur shaft. Med. Biol. Eng. Comput. 2005, 43, 115–120. [Google Scholar] [CrossRef]
- Karthik, K.; Legate-Stone, T.C.; Dasgupta, P.; Tavakkolizadeh, A.; Sinha, J. Robotic surgery in trauma and orthopaedics a systematic review. Bone Jt. J. 2015, 97, 292–299. [Google Scholar] [CrossRef]
- Shao, Z.; Wenfeng, X.U.; Liao, X.; Xie, W. Application and prospects of orthopedic robots. Mil. Med. Sci. 2016, 40, 1003–1008. [Google Scholar]
- Sugano, N. Computer-assisted orthopaedic surgery and robotic surgery in total hip arthroplasty. Clin. Orthop. Surg. 2013, 5, 1–9. [Google Scholar] [CrossRef]
- Kaye, J.A.; Jick, H. Epidemiology of lower limb fractures in general practice in the United Kingdom. Inj. Prev. 2004, 10, 368–374. [Google Scholar] [CrossRef] [Green Version]
- Gosling, T.; Westphal, R.; Faulstich, J.; Sommer, K.; Wahl, F.; Krettek, C.; Hufner, T. Forces and torques during fracture reduction: Intraoperative measurements in the femur. J. Orthop. Res. 2006, 24, 333–338. [Google Scholar] [CrossRef]
- He, M.; ZHang, T.; Han, W.; Zhou, L.; Wang, J.Q.; Wang, Y.; Zhu, G.; Chen, X.; Zhang, W.; Guo, Z. Bi-planar robot navigation system for insertion of cannulated screws in femoral neck fractures. J. Orthop. Clin. Res. 2018, 3, 195–199. [Google Scholar] [CrossRef]
- Hu, L.; Luan, S.; Wang, M.; Wang, J.; Liu, W. A biplanar robot navigation system for the distal locking of intramedullary nails. Int. J. Med. Robot. Comput. Assist. Surg. 2010, 6, 61–65. [Google Scholar]
- Zhou, L.; Wang, Y.; Wang, J.H.; Wang, J.Q.; Zhao, C.P.; Wang, M.Y. Internal fixation of femoral neck fractures assisted by bi-planar navigation robot system: An experimental study. Chin. J. Orthop. Trauma 2009, 11, 147–151. [Google Scholar]
- Zhang, F.; Du, Z.; Sun, L.; Jia, Z. A new novel virtual simulation system for robot-assisted orthopedic surgery. In Proceedings of the 2007 IEEE International Conference on Robotics and Biomimetics, Sanya, China, 15–18 December 2007; Volumes 1–5, pp. 366–370. [Google Scholar]
- Kuhnapfel, U.; Cakmak, H.K.; Maass, H. Endoscopic surgery training using virtual reality and deformable tissue simulation. Comput. Graph. 2000, 24, 671–682. [Google Scholar] [CrossRef]
- Cooke, T.D.V.; Pichora, D.; Siu, D.; Scudamore, R.A.; Bryant, J.T. Surgical implications of varus deformity of the knee with obliquity of joint surfaces. J. Bone Jt. Surg. Br. Vol. 1989, 71, 560–565. [Google Scholar] [CrossRef]
- Paley, D.; Chaudray, M.; Pirone, A.M.; Lentz, P.; Kautz, D. Treatment of malunions and mal-nonunions of the femur and tibia by detailed preoperative planning and the ilizarov techniques. Orthop. Clin. N. Am. 1990, 21, 667–691. [Google Scholar]
- Chao, E.; Neluheni, E.; Hsu, R.; Paley, D. Biomechanics of malalignment. Orthop. Clin. N. Am. 1994, 25, 379–386. [Google Scholar]
- Warisawa, S.; Ishizuka, T.; Mitsuishi, M.; Sugano, N.; Yonenobu, K.; Nakazawa, T. Development of a femur fracture reduction robot. In Proceedings of the IEEE International Conference on Robotics and Automation, 2004 (ICRA’04), New Orleans, LA, USA, 26 April–1 May 2004; pp. 3999–4004. [Google Scholar]
- Maeda, Y.; Sugan, N.; Saito, M.; Yonenobu, K.; Sakuma, I.; Naiajima, Y.; Warsawa, S.; Mitsuishi, M. Robot-assisted femoral fracture reduction: Preliminary study in patients and healthy volunteers. Comput. Aided Surg. 2008, 13, 148–156. [Google Scholar] [CrossRef]
- Pei, C. Research of The Expert System for Intelligent Fracture-resetting Robot. Master’s Thesis, Harbin Institute of Technology, Harbin, China, 2007. [Google Scholar]
- Sun, X.G.; Zhu, Q.; Wang, X.S.; Liang, B. A remote control robotic surgical system for femur shaft fracture reduction. In Proceedings of the 2015 IEEE International Conference on Robotics and Biomimetics, Zhuhai, China, 6–9 December 2015; pp. 1649–1653. [Google Scholar]
- Manzoor, S.; Kim, M.J.; Choi, Y. Robotic Leg-Lengthening Fixator using Hybrid Position/Force Control. In Proceedings of the 2014 IEEE 4th Annual International Conference on Cyber Technology in Automation, Control, and Intelligent Systems, Hong Kong, China, 4–7 June 2014; pp. 579–584. [Google Scholar]
- Koo, T.K.K.; Chao, E.Y.S.; Mak, A.F.T. Development and validation of a new approach for computer-aided long bone fracture reduction using unilateral external fixator. J. Biomech. 2006, 39, 2104–2112. [Google Scholar] [CrossRef]
- Seide, K.; Wolter, D. Corrections made with the aid of the hexapod. Orthopade 2000, 29, 39–46. [Google Scholar] [CrossRef]
- Koo, T.K.K.; Chao, E.Y.S.; Mak, A.F.T. Fixation stiffness of Dynafix unilateral external fixator in neutral and non-neutral configurations. Bio-Med. Mater. Eng. 2005, 15, 433–444. [Google Scholar]
- Seide, K.; Faschingbauer, M.; Wenzl, M.E.; Weinrich, N.; Juergens, C. A hexapod robot external fixator for computer assisted fracture reduction and deformity correction. Int. J. Med. Robot. Comput. Assist. Surg. 2004, 1, 64–69. [Google Scholar] [CrossRef]
- Majidifakhr, K.; Kazemirad, S.; Farahmand, F. Robotic Assisted Reduction of Femoral Shaft Fractures using Stewart Platform. In Medicine Meets Virtual Reality 17—Nextmed: Design for/the Well Being; Westwood, J.D., Westwood, S.W., Haluck, R.S., Hoffman, H.M., Mogel, G.T., Phillips, R., Eds.; Ios Press: Amsterdam, The Netherlands, 2009; Volume 142, pp. 177–179. [Google Scholar]
- Gong, M.; Xu, Y.; Tang, P.; Hu, L.; Du, H.; Lu, Z.; Yao, T. 3 D CT image-guided parallel mechanism-assisted femur fracture reduction. Jiqiren 2011, 33, 303–306. [Google Scholar] [CrossRef]
- Tang, P.; Hu, L.; Du, H.; Gong, M.; Zhang, L. Novel 3D hexapod computer-assisted orthopaedic surgery system for closed diaphyseal fracture reduction. Int. J. Med. Robot. Comput. Assist. Surg. 2012, 8, 17–24. [Google Scholar] [CrossRef]
- Hu, L.; Zhang, J.; Li, C.; Wang, Y.; Yang, Y.; Tang, P.; Fang, L.; Zhang, L.; Du, H.; Wang, L. A femur fracture reduction method based on anatomy of the contralateral side. Comput. Biol. Med. 2013, 43, 840–846. [Google Scholar] [CrossRef]
- Han, W.; Wang, J.Q.; Lin, H.; Wang, M. Master-slave robot assisted fracture reduction in long bone shaft. Beijing Biomed. Eng. 2015, 34, 12–17. [Google Scholar]
- Leloup, T.; El Kazzi, W.; Schuind, F.; Warzee, N. Conception of a navigation system controlling diaphyseal fracture reduction treated with external fixation. Int. J. Med. Robot. Comput. Assist. Surg. 2009, 5, 99–109. [Google Scholar] [CrossRef]
- Qiao, F.; Li, D.C.; Jin, Z.M.; Gao, Y.C.; Zhou, T.; He, J.L.; Cheng, L. Application of 3D printed customized external fixator in fracture reduction. Injury 2015, 46, 1150–1155. [Google Scholar] [CrossRef]
- Fuchtmeier, B.; Egersdoerfer, S.; Mai, R.; Hente, R.; Dragoi, D.; Monkman, G.; Nerlich, M. Reduction of femoral shaft fractures in vitro by a new developed reduction robot system ‘RepoRobo’. Injury 2004, 35 (Suppl. 1), S-A113-9. [Google Scholar] [CrossRef]
- Westphal, R.; Winkelbach, S.; Wahl, F.; Gösling, T.; Oszwald, M.; Hüfner, T.; Krettek, C. Robot-assisted long bone fracture reduction. Int. J. Robot. Res. 2009, 28, 1259–1278. [Google Scholar] [CrossRef]
- Oszwald, M.; Ruan, Z.; Westphal, R.; O’loughlin, P.F.; Kendoff, D.; Hufner, T.; Wahl, F.; Krettek, C.; Gosling, T. A rat model for evaluating physiological responses to femoral shaft fracture reduction using a surgical robot. J. Orthop. Res. 2008, 26, 1656–1659. [Google Scholar] [CrossRef]
- Oszwald, M.; Westphal, R.; Bredow, J.; Calafi, A.; Hufner, T.; Wahl, F.; Krettek, C.; Gosling, T. Robot-Assisted Fracture Reduction Using Three-Dimensional Intraoperative Fracture Visualization: An Experimental Study on Human Cadaver Femora. J. Orthop. Res. 2010, 28, 1240–1244. [Google Scholar] [CrossRef]
- Ruan, Z.; Huefner, T.; Luo, C.; Zhang, C. Robotic assisted femoral shaft fracture reduction. China Tissue Eng. Res. 2010, 14, 2292–2294. [Google Scholar]
- Kuang, S.; Leung, K.-S.; Wang, T.; Hu, L.; Chui, E.; Liu, W.; Wang, Y. A novel passive/active hybrid robot for orthopaedic trauma surgery. Int. J. Med. Robot. Comput. Assist. Surg. 2012, 8, 458–467. [Google Scholar] [CrossRef]
- Graham, A.E.; Xie, S.Q.; Aw, K.C.; Xu, W.L.; Mukherjee, S. Design of a parallel long bone fracture reduction robot with planning treatment tool. In Proceedings of the 2006 IEEE/RSJ International Conference on Intelligent Robots and Systems, Beijing, China, 9–15 October 2006; Volumes 1–12, pp. 1255–1260. [Google Scholar]
- Yu, L. Key Techniques of 6-Ptrt Parallel Robot and Their Applycation in Orthopaedic Surgery. Ph.D. Thesis, Harbin Institute of Technology, Harbin, China, 2007. [Google Scholar]
- Wang, T.; Li, C.; Hu, L.; Tang, P.; Zhang, L.; Du, H.; Luan, S.; Wang, L.; Tan, Y.; Peng, C. A Removable Hybrid Robot System for Long Bone Fracture Reduction. Bio-Med. Mater. Eng. 2014, 24, 501–509. [Google Scholar]
- Li, C.; Wang, T.; Hu, L.; Zhang, L.; Du, H.; Wang, L.; Luan, S.; Tang, P. Accuracy analysis of a robot system for closed diaphyseal fracture reduction. Int. J. Adv. Robot. Syst. 2014, 11, 169. [Google Scholar] [CrossRef]
- Du, H.; Hu, L.; Li, C.; Wang, T.; Zhao, L.; Li, Y.; Mao, Z.; Liu, D.; Zhang, L.; He, C.; et al. Advancing computer-assisted orthopaedic surgery using a hexapod device for closed diaphyseal fracture reduction. Int. J. Med. Robot. Comput. Assist. Surg. 2015, 11, 348–359. [Google Scholar] [CrossRef]
- Tang, P.; Wang, T.; Hu, L. Long-Bone Fracture-Reduction Robot. U.S. Patent 9,610,101 B2, 4 April 2017. [Google Scholar]
- Li, C.; Wang, T.; Hu, L.; Tang, P.; Wang, L.; Zhang, L.; Guo, N.; Tan, Y. A novel master-slave teleoperation robot system for diaphyseal fracture reduction: A preliminary study. Comput. Assist. Surg. 2016, 21, 162–167. [Google Scholar] [CrossRef]
- Wang, J.Q.; Han, W.; Lin, H. Femoral fracture reduction with a parallel manipulator robot on a traction table. Int. J. Med. Robot. Comput. Assist. Surg. 2013, 9, 464–471. [Google Scholar] [CrossRef]
- Dagnino, G.; Georgilas, I.; Tarassoli, P.; Atkins, R.; Dogramadzi, S. Design and Real-Time Control of a Robotic System for Fracture Manipulation. In Proceedings of the 2015 37th Annual International Conference of the Ieee Engineering in Medicine and Biology Society, Milan, Italy, 25–29 August 2015; pp. 4865–4868. [Google Scholar]
- Dagnino, G.; Georgilas, I.; Tarassoli, P.; Atkins, R.; Dogramadzi, S. Vision-based real-time position control of a semi-automated system for robot-assisted joint fracture surgery. Int. J. Comput. Assist. Radiol. Surg. 2016, 11, 437–455. [Google Scholar] [CrossRef]
- Abedinnasab, M.H.; Farahmand, F.; Gallardo-Alvarado, J. The Wide-Open Three-Legged Parallel Robot for Long-Bone Fracture Reduction. J. Mech. Robot. 2017, 9, 10. [Google Scholar] [CrossRef]
- Ye, R.; Chen, Y. Development of A Six Degree of Freedom (DOF) Hybrid Robot for Femur Shaft Fracture Reduction. In Proceedings of the 2008 IEEE International Conference on Robotics and Biomimetics, Bangkok, Thailand, 22–25 February 2009; Volumes 1–4, pp. 306–311. [Google Scholar]
- Wang, S.; Chen, Y.; Ping, Z. Control Simulation of a six DOF Parallel-Serial Robot for femur fracture reduction. In Proceedings of the 2009 IEEE International Conference on Virtual Environments, Human-Computer Interfaces and Measurement Systems, Hong Kong, China, 11–13 May 2009; pp. 330–335. [Google Scholar]
- Ye, R.; Chen, Y. Path Planning for Robot Assisted Femur Shaft Fracture Reduction: A Preliminary Investigation. In Proceedings of the 2009 IEEE International Conference on Virtual Environments, Human-Computer Interfaces and Measurement Systems, Hong Kong, China, 11–13 May 2009; pp. 113–117. [Google Scholar]
- Ye, R.; Chen, Y.; Yau, W. A Simple and Novel Hybrid Robotic System for Robot-Assisted Femur Fracture Reduction. Adv. Robot. 2012, 26, 83–104. [Google Scholar] [CrossRef]
- Hung, S.-S.; Lee, M.-Y. Functional assessment of a surgical robot for reduction of lower limb fractures. Int. J. Med. Robot. Comput. Assist. Surg. 2010, 6, 413–421. [Google Scholar] [CrossRef]
- Dagnino, G.; Georgilas, I.; Kohler, P.; Atkins, R.; Dogramadzi, S. Image-Based Robotic System for Enhanced Minimally Invasive Intra-Articular Fracture Surgeries. In Proceedings of the 2016 IEEE International Conference on Robotics and Automation, Stockholm, Sweden, 16–21 May 2016; Okamura, A., Menciassi, A., Ude, A., Burschka, D., Lee, D., Arrichiello, F., Liu, H., Moon, H., Neira, J., Sycara, K., et al., Eds.; pp. 696–701. [Google Scholar]
- Wang, L.; Wang, T.; Tang, P.; Hu, L.; Liu, W.; Han, Z.; Hao, M.; Liu, H.; Wang, K.; Zhao, Y.; et al. A new hand-eye calibration approach for fracture reduction robot. Comput. Assist. Surg. 2017, 22, 113–119. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y. Development of a Surgical Robot System for Long Bone Fractures. Ph.D. Thesis, Chinese People’s Liberation Army Medical College, Beijing, China, 2016. [Google Scholar]
- Cao, Y. Development and Testing of Intelligent and Minimally Invasive Surgical Robot System for Fracture of Femoral Shaft. Master’s Thesis, Chinese People’s Liberation Army Medical College, Beijing, China, 2017. [Google Scholar]
- Mettler, F.A., Jr.; Wiest, P.W.; Locken, J.A.; Kelsey, C.A. CT scanning: Patterns of use and dose. J. Radiol. Prot. 2000, 20, 353. [Google Scholar] [CrossRef]
- Kovanda, T.J.; Ansari, S.F.; Qaiser, R.; Fulkerson, D.H. Feasibility of CT-based intraoperative 3D stereotactic image-guided navigation in the upper cervical spine of children 10 years of age or younger: Initial experience. J. Neurosurg. Pediatr. 2015, 16, 590–598. [Google Scholar] [CrossRef]
- Mitschke, M.; Navab, N. Recovering the X-ray projection geometry for three-dimensional tomographic reconstruction with additional sensors: Attached camera versus external navigation system. Med. Image Anal. 2003, 7, 65–78. [Google Scholar] [CrossRef]
- Wendl, K.A.; Wentzensen, A.; Grützner, P. Iso-C (3D0-assisted) navigated implantation of pedicle screws in thoracic lumbar vertebrae. Der Unf. 2003, 106, 907–913. [Google Scholar]
- Amin, D.V.; Kanade, T.; Digioia, A.M.; Jaramaz, B. Ultrasound registration of the bone surface for surgical navigation. Comput. Aided Surg. 2003, 8, 1–16. [Google Scholar] [CrossRef]
- Von Jako, R.A.; Carrino, J.A.; Yonemura, K.S.; Noda, G.A.; Zhue, W.; Blaskiewicz, D.; Rajue, M.; Groszmann, D.E.; Weber, G. Electromagnetic navigation for percutaneous guide-wire insertion: Accuracy and efficiency compared to conventional fluoroscopic guidance. Neuroimage 2009, 47, T127–T132. [Google Scholar] [CrossRef]
- Lionberger, D.R.; Weise, J.; Ho, D.M.; Haddad, J.L. How does electromagnetic navigation stack up against infrared navigation in minimally invasive total knee arthroplasties? J. Arthroplast. 2008, 23, 573–580. [Google Scholar] [CrossRef]
- Sparmann, M.; Wolke, B.; Czupalla, H.; Banzer, D.; Zink, A. Positioning of total knee arthroplasty with and without navigation support—A prospective, randomised study. J. Bone Jt. Surg. Br. Vol. 2003, 85, 830–835. [Google Scholar] [CrossRef]
- Muthu, G.; Vendittoli, P.A.; Lavigne, M.; Gunther, K.P. Femoral Component Positioning in Hip Resurfacing With and Without Navigation. Clin. Orthop. Relat. Res. 2009, 467, 1341–1347. [Google Scholar] [Green Version]
- Wang, M.; Song, Z. Optimal number and distribution of points selected on the vertebra for surface matching in CT-based spinal navigation. Comput. Aided Surg. 2013, 18, 93–100. [Google Scholar] [CrossRef] [Green Version]
- Keast-Butler, O.; Lutz, M.J.; Angelini, M.; Lash, N.; Pearce, D.; Crookshank, M.; Zdero, R.; Schemitsch, E.H. Computer navigation in the reduction and fixation of femoral shaft fractures: A randomized control study. Injury 2012, 43, 749–756. [Google Scholar] [CrossRef]
- Bouazza-Marouf, K.; Browbank, I.; Hewit, J.R. Robotic-assisted internal fixation of femoral fractures. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 1995, 209, 51–58. [Google Scholar] [CrossRef]
- Suero, E.M.; Hartung, T.; Westphal, R.; Hawi, N.; Liodakis, E.; Citak, M.; Krettek, C.; Stuebig, T. Improving the human-robot interface for telemanipulated robotic long bone fracture reduction: Joystick device vs. haptic manipulator. Int. J. Med Robot. Comput. Assist. Surg. 2018, 14, e1863. [Google Scholar] [CrossRef]
- Winkelbach, S.; Molkenstruck, S.; Wahl, F.M. Low-cost laser range scanner and fast surface registration approach. In Pattern Recognition, Proceedings; Franke, K., Muller, K.R., Nickolay, B., Schafer, R., Eds.; Springer: Berlin/Heidelberg, Germany, 2006; Volume 4174, pp. 718–728. [Google Scholar]
- Westphal, R.; Winkelbach, S.; Gosling, T.; Oszwald, M.; Hufner, T.; Krettek, C.; Wahl, F.M. Automated Robot Assisted Fracture Reduction; Springer-Verlag: Berlin, Germany, 2009; p. 251. [Google Scholar]
- Suero, E.M.; Westphal, R.; Citak, M.; Hawi, N.; Liodakis, E.; Omar, M.; Krettek, C.; Stuebig, T. Comparison of algorithms for automated femur fracture reduction. Int. J. Med. Robot. Comput. Assist. Surg. 2018, 14, 6. [Google Scholar] [CrossRef]
- Su, Y.; Sun, Z.; Zhu, G.; Wang, Y. Experiments Research of Somatosensory Interaction Based Control Method for Fracture Reduction Robot. Chin. J. Biomed. Eng. 2016, 35, 380–384. [Google Scholar]
- Weber-Spickschen, T.S.; Oszwald, M.; Westphal, R.; Krettek, C.; Wahl, F.; Gosling, T. Development of a fixation device for robot assisted fracture reduction of femoral shaft fractures: A biomechanical study. Technol. Health Care 2010, 18, 207–216. [Google Scholar]
- Jia, Z.; Du, Z.; Monan, W. A novel finite element method based biomechanical model for HIT-Robot Assisted Orthopedic Surgery System. In Proceedings of the 2006 International Conference of the IEEE Engineering in Medicine and Biology Society, New York, NY, USA, 30 August–3 September 2006; pp. 1735–1738. [Google Scholar]
- Monan, W. Development and Validity of Tissue Biomechanics Modeling for Virtual Robot Assisted Orthopedic Surgery System. In Proceedings of the 2009 3rd International Conference on Bioinformatics and Biomedical Engineering, Beijing, China, 11–13 June 2009; 2009; Volumes 1–11, pp. 1931–1934. [Google Scholar]
- Brown, E.; Rodenberg, N.; Amend, J.; Mozeika, A.; Steltz, E.; Zakin, M.R.; Lipson, H.; Jaeger, H.M. Universal robotic gripper based on the jamming of granular material. Proc. Natl. Acad. Sci. USA 2010, 107, 18809–18814. [Google Scholar] [CrossRef] [Green Version]
- Binder, H.; Blettner, M. Big Data in Medical Science—A Biostatistical View: Part 21 of a Series on Evaluation of Scientific Publications. Dtsch. Ärzteblatt Int. 2015, 112, 137. [Google Scholar]
- Erdman, A.G.; Keefe, D.F.; Schiestl, R. Grand challenge: Applying regulatory science and big data to improve medical device innovation. IEEE Trans. Biomed. Eng. 2013, 60, 700–706. [Google Scholar] [CrossRef]



| Type | The External Fixed Frame Structure | Serial Structure | Parallel Structure | Serial-Parallel Hybrid Structure | ||
|---|---|---|---|---|---|---|
| Comparison Item | ||||||
| robot size | <leg length <2~3 times of leg diameter | general industrial robot size | >fixed frame, <serial structure | larger than the parallel structure (sometimes bigger than the serial structure) | ||
| maximum load | force | / | <300 N | 300~700 N | 200~400 N | |
| torque | / | / | 20~80 N·m | / | ||
| application | 1/3 of the middle long bone fracture | femoral shaft fracture | femur long bone fracture | joint fracture | ||
| Typical robot | six-bar parallel reduction mechanism [43,44] | robot in Brunswick university of technology [50] | precision surgery robot for long bone fracture [71] | serial-parallel hybrid robot (by Giulio) [70] | ||
| test subject * | animal bone | model bone | cadaver | model bone | animal bone | |
| reduction accuracy * | axial deflection | 1.24 ± 0.65 mm | 1.08 ± 0.63 mm | 3.08 ± 1.505 m | 1.67 ± 0.778 mm | the displacement deviation is: 0.09 ± 0.08 mm; the angular deviation is: 0.15 ± 0.04° |
| rotation | 2.83 ± 0.9° | 1.09 ± 0.73° | 2.58 ± 1.240° | 2.08 ± 0.669° | ||
| translation | 1.19 ± 0.37 mm | 1.61 ± 1.23 mm | 1.92 ± 0.606 m | 1.33 ± 0.563 mm | ||
| angulation | 2.34 ± 1.79° | 1.37 ± 1.39° | 1.98 ± 0.619° | 1.50 ± 0.558° | ||
| motion range * | 120 mm × 120 mm × 80 mm | / | 200 mm × 200 mm × 200 mm | serial platform: 4/3 × π13003 mm3 parallel platform: 20.5 mm × 20.5 mm × 30 mm | ||
| Navigation | CT | Perspective | Ultrasound | Electromagnetic | Imageless | |
|---|---|---|---|---|---|---|
| Comparison Item | ||||||
| radiation | very high | high | none | none | none | |
| visualization effect | best | better | common | common | need to combine CT images | |
| trauma | none | none | none | none | great | |
| disturb by environment | none | none | great | great | less | |
| Control Technology | Joystick Based Control | Master Structure-Based Control | Automatic Control | |
|---|---|---|---|---|
| Comparison Item | ||||
| learning curve | short | long | very short | |
| accuracy | common | common | high | |
| feedback ability | lack of tactile feedback | comprehensive feedback can be achieved | none | |
| can it deal with emergencies well? | can | can | can’t | |
| Connection | External Fixator | Reposition-Plate | Three-Point-Device | One-Orthopaedic-Pin | Through Gasbag | |
|---|---|---|---|---|---|---|
| Comparison Item | ||||||
| reliability | stable | stable | stable | stable under small external force | unstable | |
| trauma | multiple holes | 3 holes | 3 holes | 1 hole | none | |
| ultimate load | <411 N; <70N·m | <411 N; <70N·m | 600 N; 80 N·m | 147 N; 1.8 N·m | lateral force 800 N | |
| preoperative preparation time | >5 min | 3~5 min | 3~5 min | 1~3 min | <1 min | |
| customized | no | no | no | yes | no | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bai, L.; Yang, J.; Chen, X.; Sun, Y.; Li, X. Medical Robotics in Bone Fracture Reduction Surgery: A Review. Sensors 2019, 19, 3593. https://doi.org/10.3390/s19163593
Bai L, Yang J, Chen X, Sun Y, Li X. Medical Robotics in Bone Fracture Reduction Surgery: A Review. Sensors. 2019; 19(16):3593. https://doi.org/10.3390/s19163593
Chicago/Turabian StyleBai, Long, Jianxing Yang, Xiaohong Chen, Yuanxi Sun, and Xingyu Li. 2019. "Medical Robotics in Bone Fracture Reduction Surgery: A Review" Sensors 19, no. 16: 3593. https://doi.org/10.3390/s19163593
APA StyleBai, L., Yang, J., Chen, X., Sun, Y., & Li, X. (2019). Medical Robotics in Bone Fracture Reduction Surgery: A Review. Sensors, 19(16), 3593. https://doi.org/10.3390/s19163593








