MW-PPG Sensor: An on-Chip Spectrometer Approach
Abstract
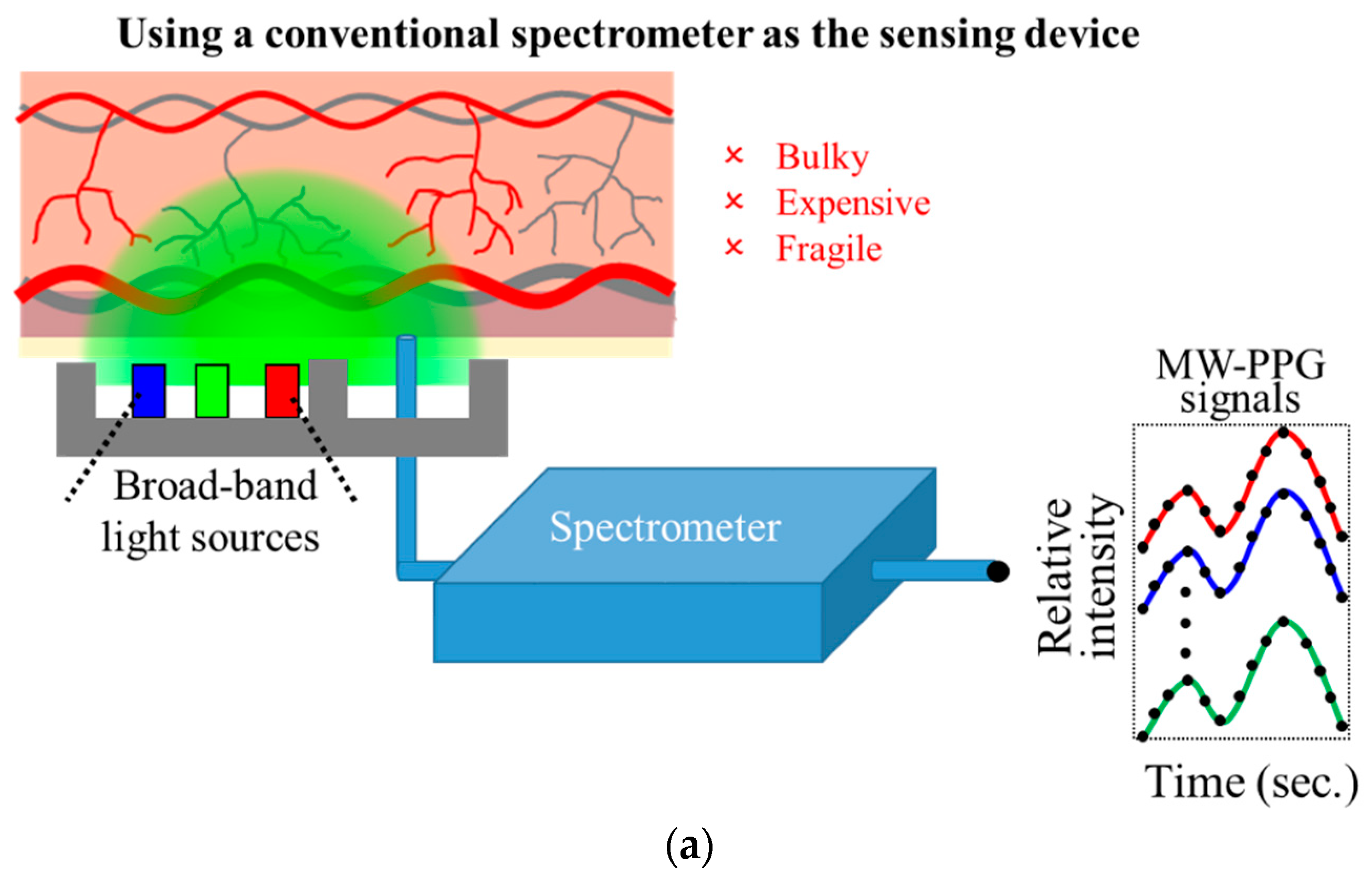
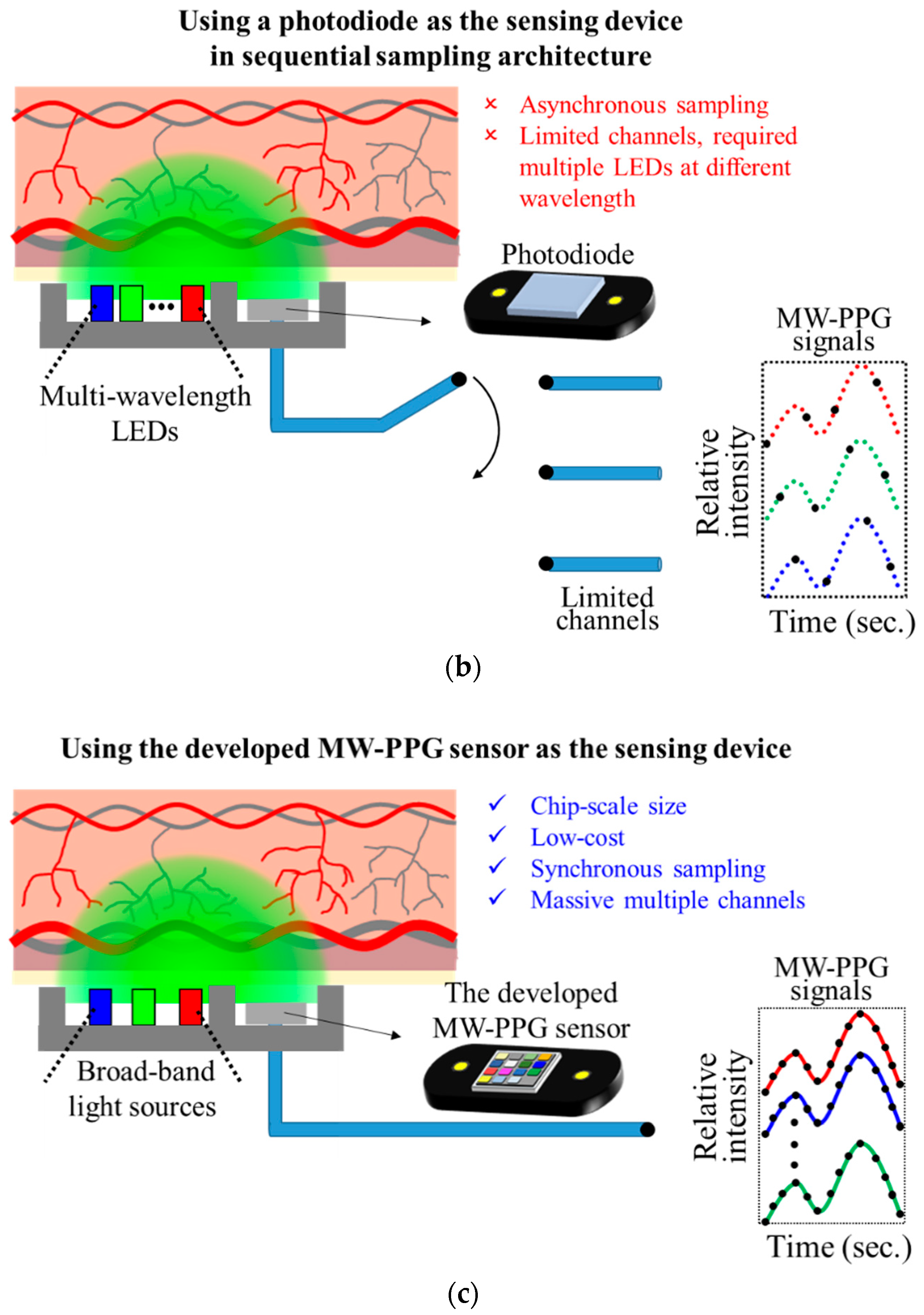
:1. Introduction
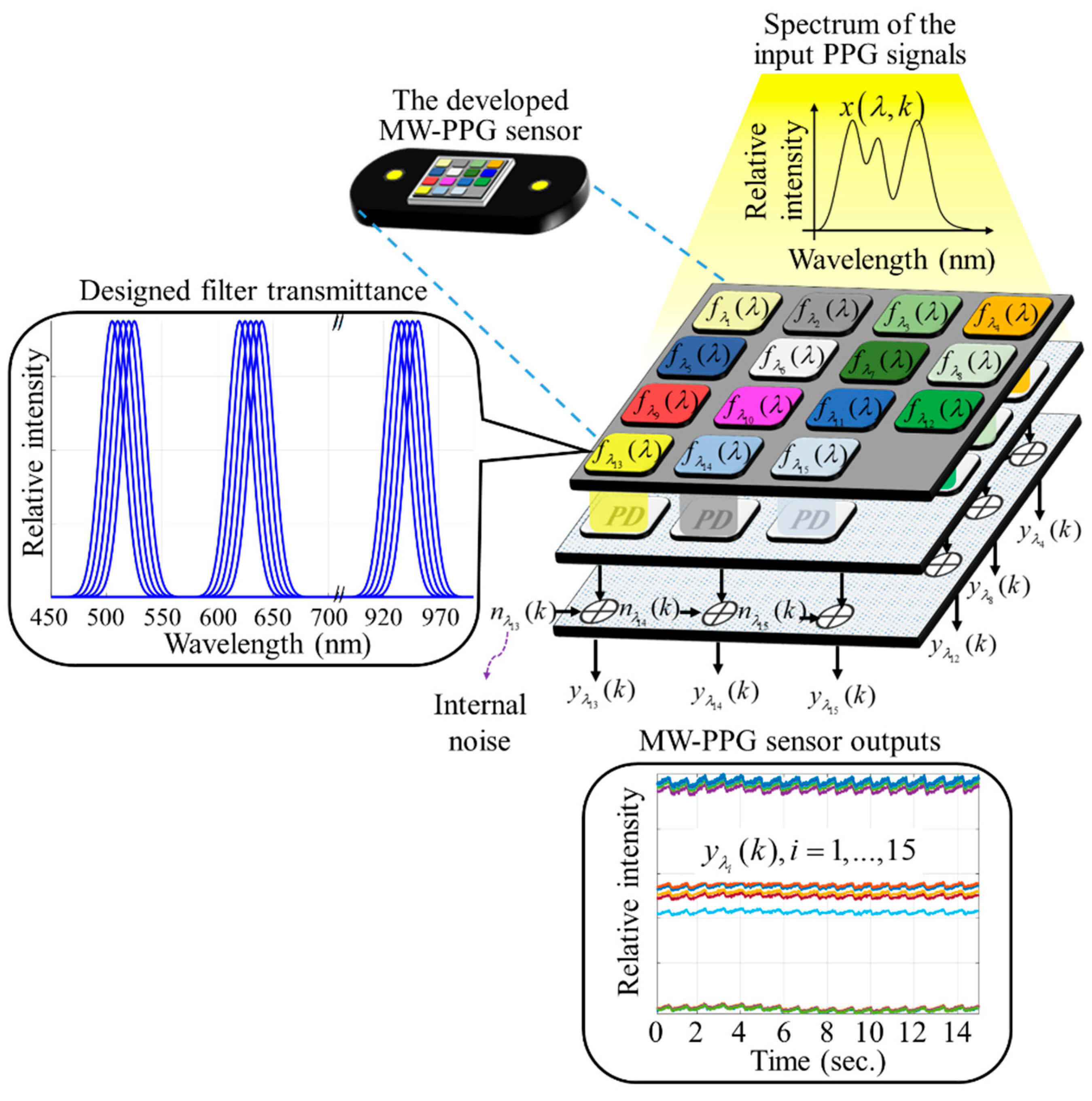
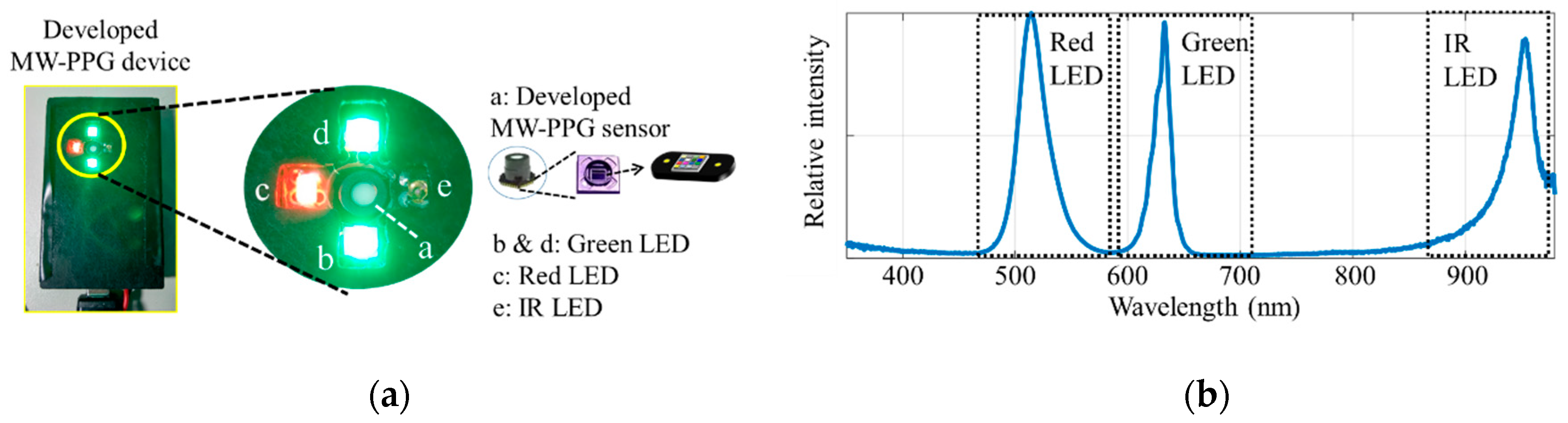
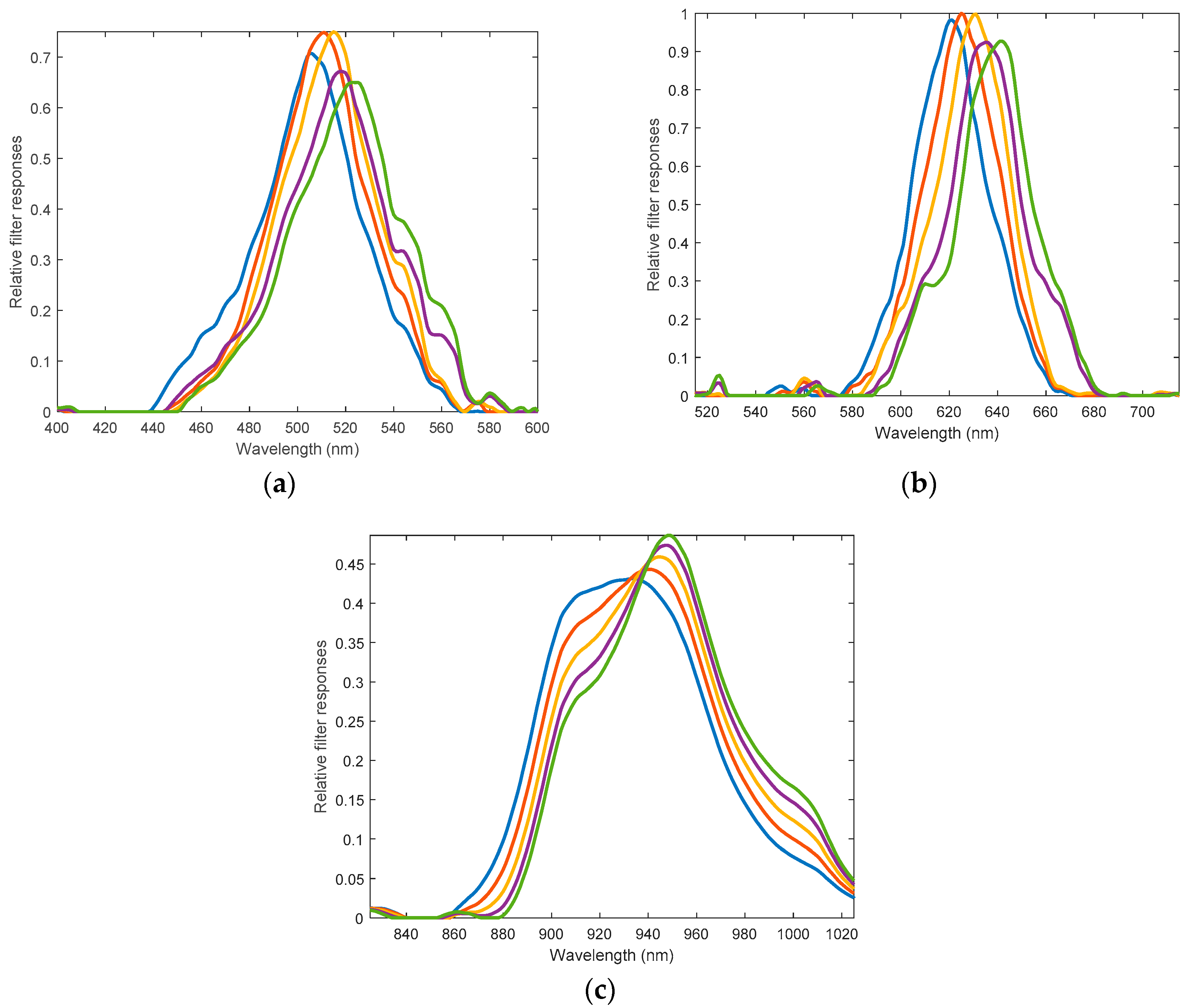
2. Design of the Developed MW-PPG Sensor
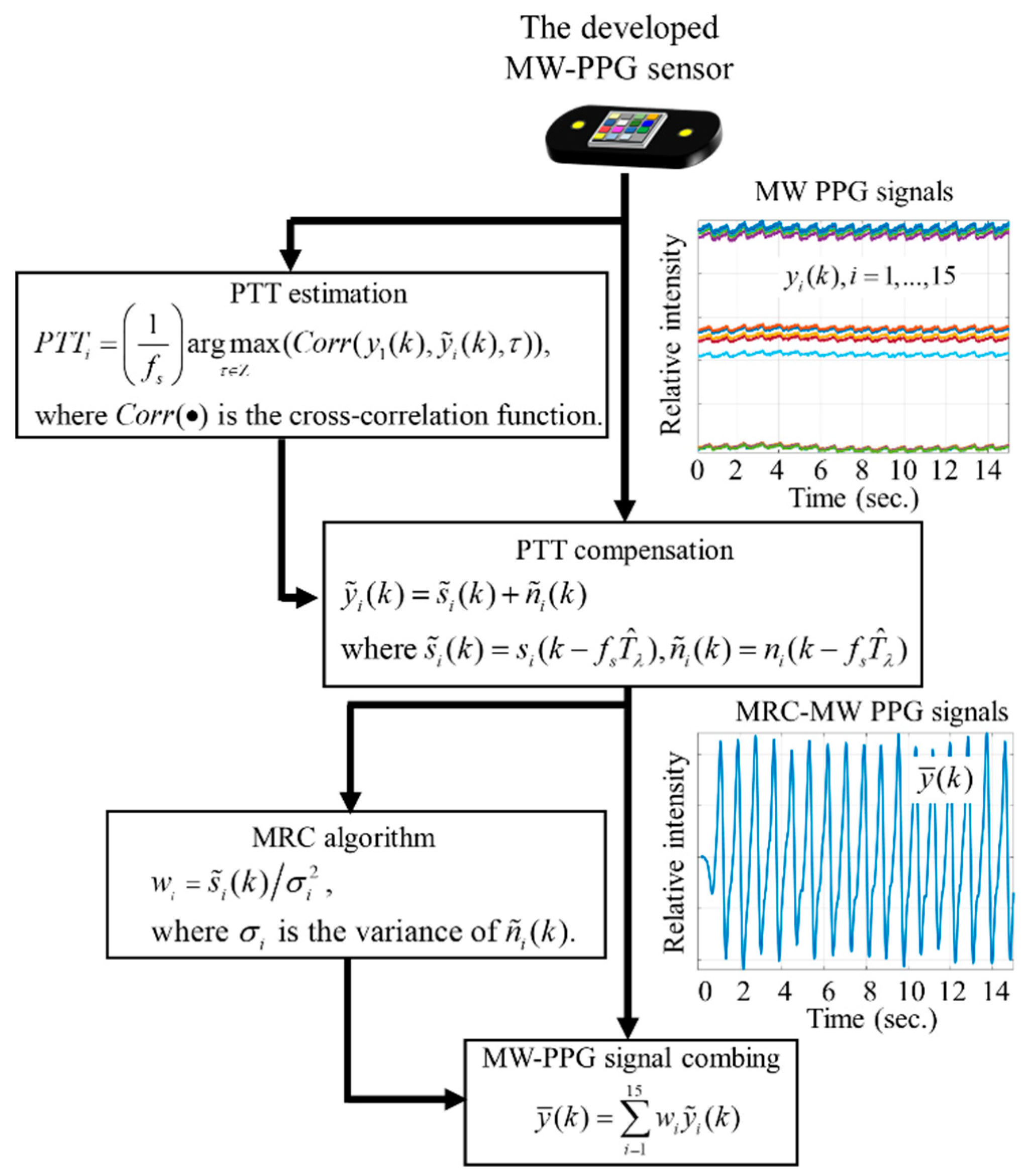
3. Methods for Extraction Robust PPG Signals, SpO2, and Blood Pressure Measurement
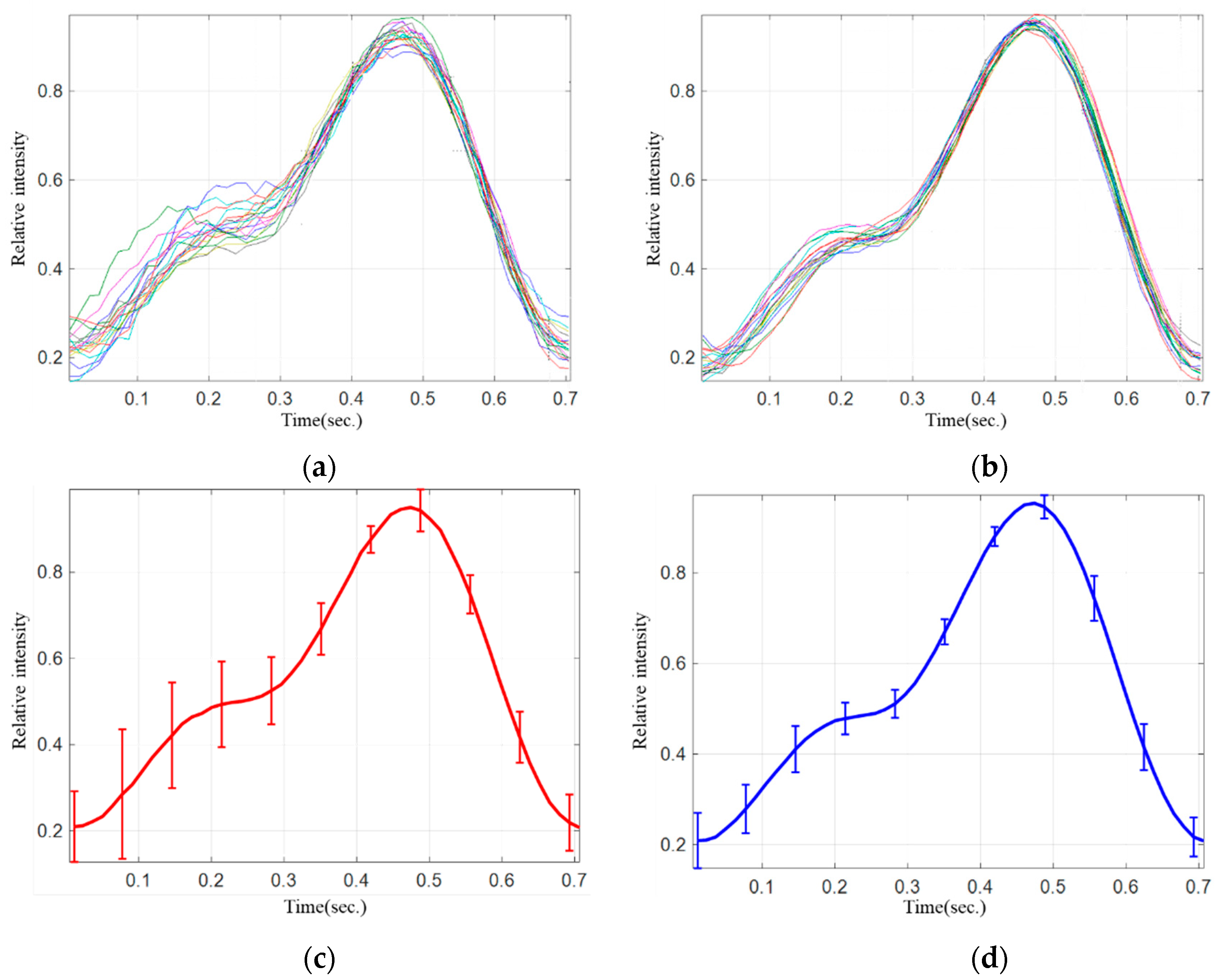
3.1. MW-PPG Signals Combining Methods for Extracting Robust PPG Signals
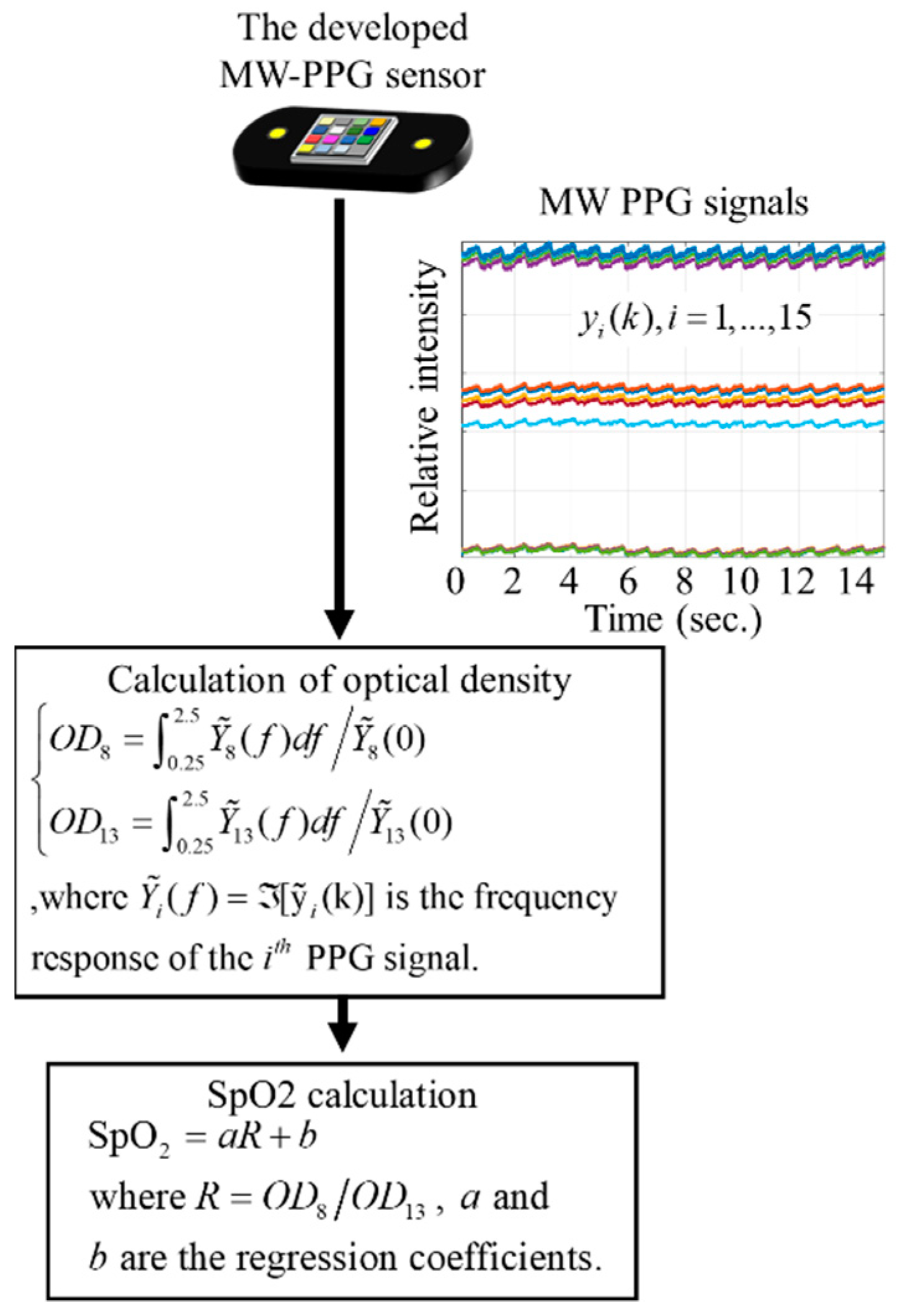
3.2. MW-PPG Signal Processing Methods for SpO2 Measurement
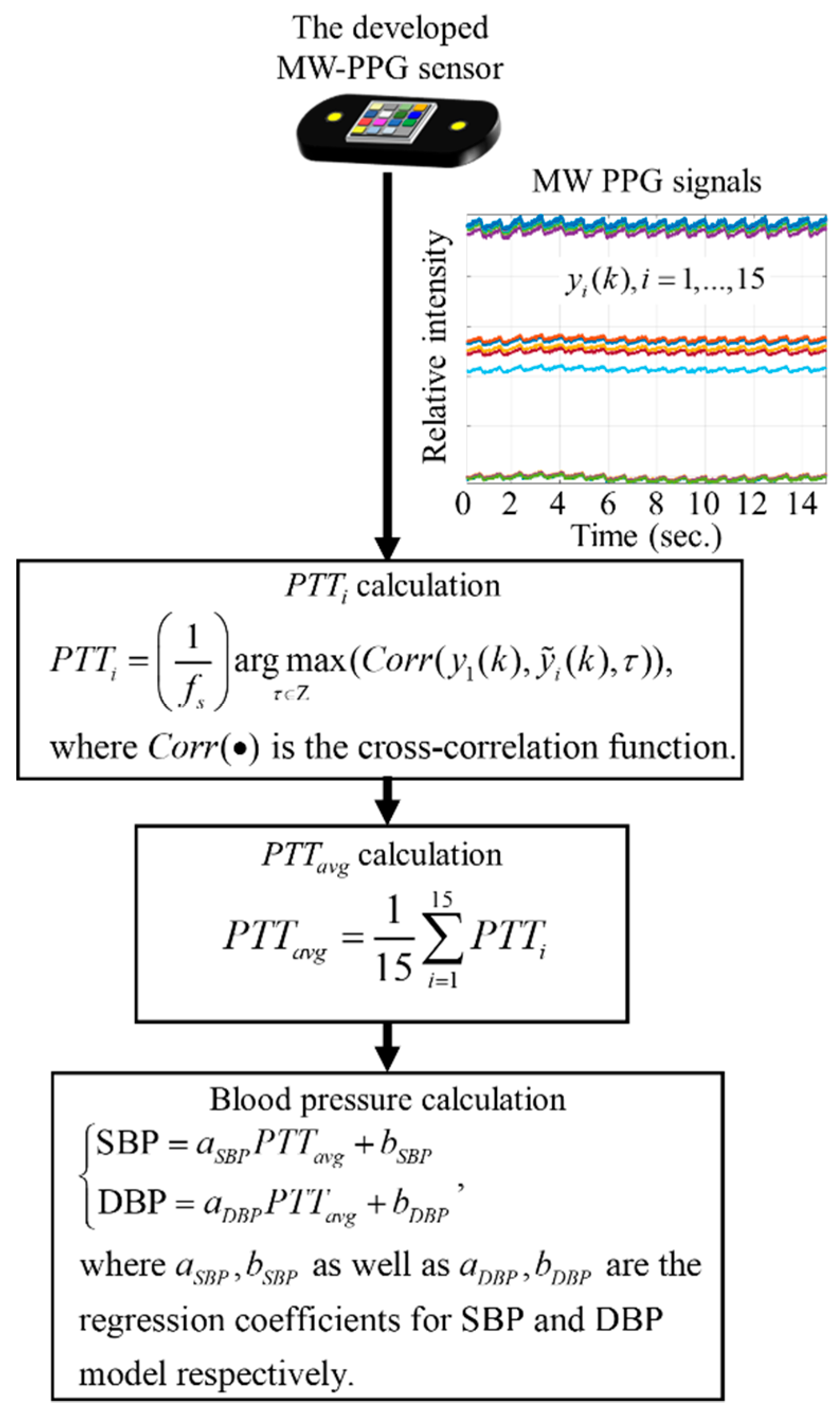
3.3. MW-PPG Signals Processing Methods for Blood Pressure Measurement
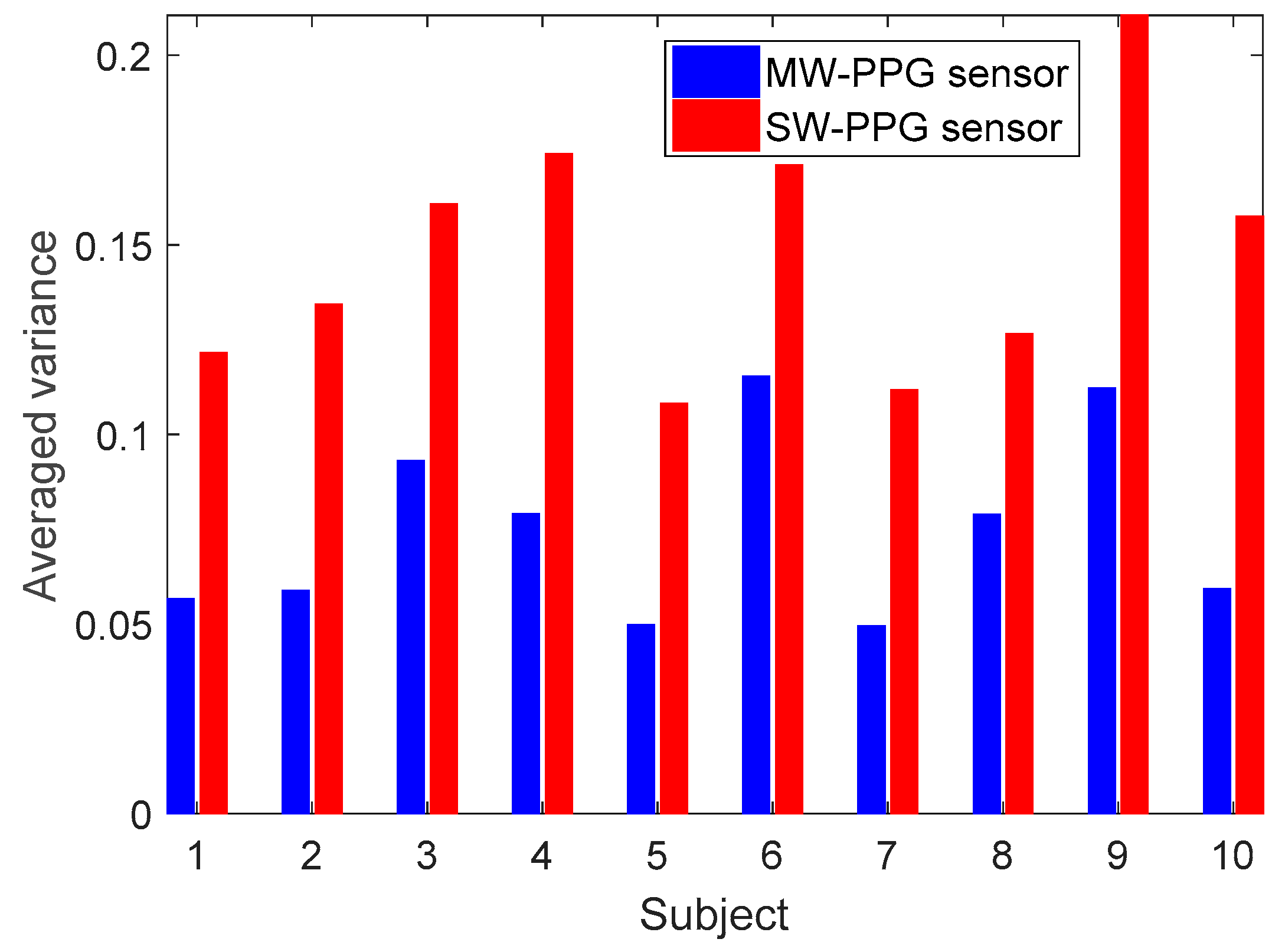
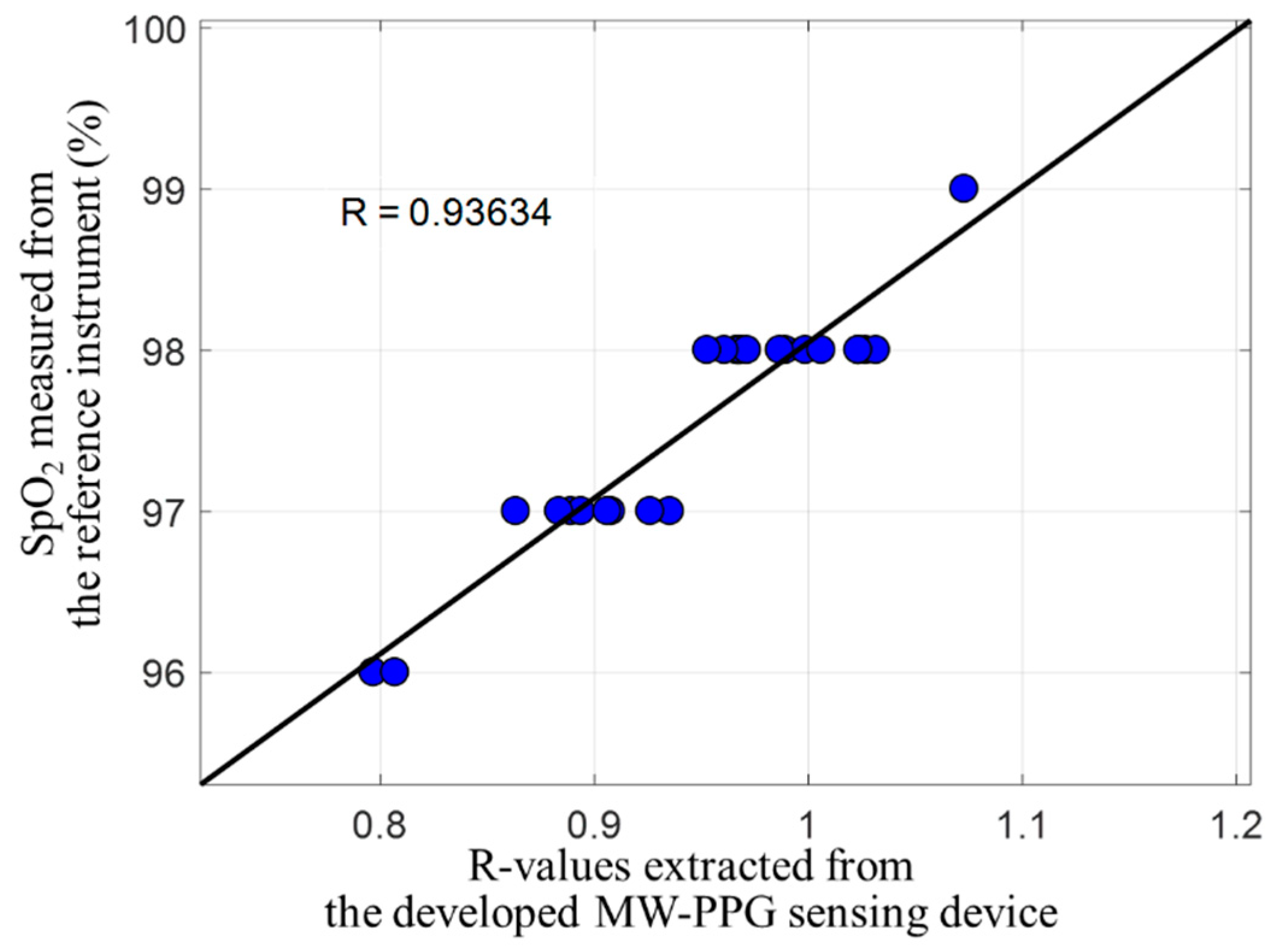
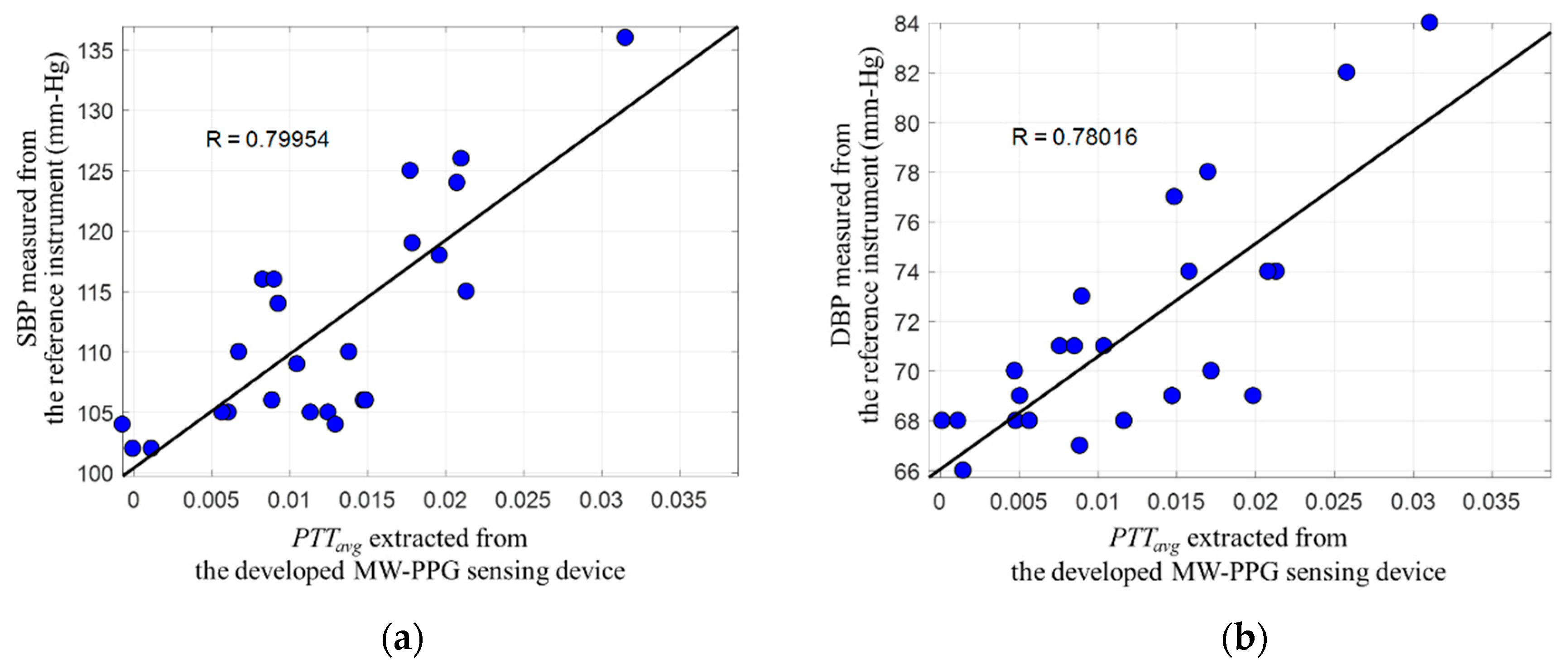
4. Experiment Results
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Buchs, A.; Slovik, Y.; Rapoport, M.; Rosenfeld, C.; Khanokh, B.; Nitzan, M. Right-left correlation of the sympathetically induced fluctuations of photoplethysmographic signal in diabetic and non-diabetic subjects. Med. Biol. Eng. Comput. 2005, 43, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Nasimi, S.G.; Mearns, A.J.; Harness, J.B.; Heath, I. Quantitative measurement of sympathetic neuropathy in patients with diabetes mellitus. J. Biomed. Eng. 1991, 13, 203–208. [Google Scholar] [CrossRef]
- Allen, J.; Murray, A. Similarity in bilateral photoplethysmographic peripheral pulse wave characteristics at the ears, thumbs and toes. Physiol. Meas. 2000, 21, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Avnon, Y.; Nitzan, M.; Sprecher, E.; Rogowski, Z.; Yarnitsky, D. Different patterns of parasympathetic activation in uni- and bilateral migraineurs. Brain J. Neurol. 2003, 126, 1660–1670. [Google Scholar] [CrossRef] [PubMed]
- Apple Watch Series 3 Teardown. Available online: https://www.ifixit.com/Teardown/Apple+Watch+Series+3+Teardown/97521 (accessed on 8 May 2018).
- HUAWEI Band 2 Pro. Available online: https://consumer.huawei.com/tw/wearables/band2-pro/ (accessed on 8 May 2019).
- Amazfit. Available online: http://cn.amazfit.com/ (accessed on 10 June 2019).
- Vivofit 4. Available online: https://explore.garmin.com/en-US/vivo-fitness/ (accessed on 8 June 2019).
- Liquid Leap+ Fitness Watch. Available online: https://us-store.acer.com/wearables/liquid-leap-plus-fitness-watch (accessed on 8 May 2018).
- Gear Sport. Available online: https://www.samsung.com/us/mobile/wearables/smartwatches/gear-sport-blue-sm-r600nzbaxar/ (accessed on 8 May 2019).
- Measuring Heart Rates with Light Technology Applications Expands in Wearables and Potentially Home Healthcare Applications, Says LED Inside. Available online: https://www.ledinside.com/intelligence/2016/5/measuring_heart_rates_with_light_technology_applications_expands_in_wearables_and_potentially_home_healthcare_applications_says (accessed on 24 December 2017).
- Global Smart Wearable Device Market to Grow at a CAGR of over 16% through 2016–2024 Research Nester. Available online: https://medium.com/@Mresearchnester/global-smart-wearable-device-market-to-grow-at-a-cagr-of-over-16-through-2016-2024-research-nester-3d4178d05a99 (accessed on 24 December 2017).
- Lee, J.; Matsumura, K.; Yamakoshi, K.I.; Rolfe, P.; Tanaka, S.; Yamakoshi, T. Comparison between red, green and blue light reflection photoplethysmography for heart rate monitoring during motion. In Proceedings of the IEEE EMBS, Osaka, Japan, 3–7 June 2013; pp. 1724–1727. [Google Scholar]
- Matsumura, K.; Rolfe, P.; Lee, J.; Yamakoshi, T. iPhone 4s photoplethysmography: Which light color yields the most accurate heart rate and normalized pulse volume using the iPhysioMeter application in the presence of motion artifact? PLoS ONE 2014, 9, e91205. [Google Scholar] [CrossRef] [PubMed]
- Asare, L.; Ozols, M.; Rubins, U.; Rubenis, O.; Spigulis, J. Clinical measurements with multi-spectral photoplethysmography sensors. In Proceedings of the SPIE, Brussels, Belgium, 12–16 April 2010; pp. 842734.1–842734.5. [Google Scholar]
- Asare, L.; Kviesis-Kipge, E.; Grabovskis, A.; Rubins, U.; Erts, R.; Spigulis, J. Multi-spectral photoplethysmography biosensor. In Proceedings of the SPIE, Prague, Czech Republic, 19–20 April 2011; pp. 80731Z.1–80731Z.6. [Google Scholar]
- Kumar, M.; Veeraraghavan, A.; Sabharwal, A. DistancePPG: Robust non-contact vital signs monitoring using a camera. Biomed. Opt. Express 2015, 6, 1565–1588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, L.; Hu, S.; Alzahrani, A.; Alharbi, S.; Blanos, P. A multi-wavelength opto-electronic patch sensor to effectively detect physiological changes against human skin types. Biosensors 2017, 7, 22. [Google Scholar] [CrossRef] [PubMed]
- Jeong, C.; Yoon, H.; Kang, H.; Yeom, H. Effects of skin surface temperature on photoplethysmograph. J. Healthc. Eng. 2014, 5, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Maeda, Y.; Sekine, M.; Tamura, T. The advantages of wearable green reflected photoplethysmography. J. Med. Syst. 2011, 35, 829–834. [Google Scholar] [CrossRef] [PubMed]
- Spigulis, J.; Gailite, L.; Lihachev, A.; Erts, R. Simultaneous recording of skin blood pulsations at different vascular depths by multiwavelength photoplethysmography. Appl. Opt. 2007, 46, 1754–1759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spigulis, J.; Gailite, L.; Erts, R.; Lihachev, A. Contact probe pressure effects in skin multi-spectral photoplethysmography. In Proceedings of the SPIE Diagnostic Optical Spectroscopy in Biomedicine, Munich, Germany, 11 July 2007; pp. 1–8. [Google Scholar]
- Anderson, R.; Parrish, J. The optics of human skin. J. Investig. Dermatol. 1981, 77, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Vahdani-Manaf, N. Biological assessments by innovative use of multi-wavelength photoplethysmographic signals time differences. J. Appl. Sci. 2015, 15, 1312–1317. [Google Scholar] [CrossRef]
- Asare, L.; Kviesis-Kipge, E.; Rubins, U.; Rubenis, O.; Spigulis, J. Multi-spectral photoplethysmography technique for parallel monitoring of pulse shapes at different tissue depths. In Proceedings of the SPIE Clinical and Biomedical Spectroscopy and Imaging, Munich, Germany, 10 June 2011; pp. 1–6. [Google Scholar]
- AFE4404. Available online: http://www.ti.com/product/AFE4404 (accessed on 8 May 2018).
- Optical Sensor for Heart Rate Monitor—BH1790GLC. Available online: http://www.rohm.com.tw/web/taiwan/products/-/product/BH1790GLC (accessed on 8 May 2018).
- MAX30102, High-Sensitivity Pulse Oximeter and Heart-Rate Sensor for Wearable Health. Available online: https://www.maximintegrated.com/en/products/sensors-and-sensor-interface/MAX30102.html (accessed on 8 May 2018).
- Kurokawa, U.; Choi, B.I.; Chang, C.C. Filter-based miniature spectrometers: Spectrum reconstruction using adaptive regularization. IEEE Sens. J. 2011, 11, 1556–1563. [Google Scholar] [CrossRef]
- Chang, C.C.; Lin, H.Y. Spectrum reconstruction for on-chip spectrum sensor array using a novel blind nonuniformity correction method. IEEE Sens. J. 2012, 12, 2586–2592. [Google Scholar] [CrossRef]
- Lokharan, M.; Lokesh, K.C.; Kumar, V.; Kumar, H.; Kayalvizhi, N.; Aryalekshmi, R.; Goli, S.; Jayanthi, T. Measurement of pulse transit time (PTT) using photoplethysmography. In Proceedings of the 16th International Conference on Biomedical Engineering, Singapore, 30 June 2017; pp. 130–131. [Google Scholar]
- Yoon, Y.; Toon, G. Nonconstrained blood pressure measurement by photoplethysmography. J. Opt. Soc. Korea 2016, 10, 91–95. [Google Scholar] [CrossRef]
- Liu, J.; Yan, B.P.; Zhang, Y.T.; Ding, X.R.; Su, P.; Zhao, N. Multi-wavelength photoplethysmography enabling continuous blood pressure measurement with compact wearable electronics. IEEE Trans. Biomed. Eng. 2018, 66, 1514–1525. [Google Scholar] [CrossRef] [PubMed]
- Maximal-Ratio Combining. Available online: https://en.wikipedia.org/wiki/Maximal-ratio_combining (accessed on 16 June 2018).
- Yang, D.; Zhu, J.; Zhu, P. SpO2 and heart rate measurement with wearable watch based on PPG. In Proceedings of the 2015 IET International Conference on Biomedical Image and Signal Processing, Beijing, China, 19 November 2015. [Google Scholar]
- Carni, D.L.; Grimaldi, D.; Sciammarella, P.F.; Lamonaca, F.; Spagnuolo, V. Setting-up of PPG scaling factors for SpO2% evaluation by smartphone. In Proceedings of the 2016 IEEE International Symposium on Medical Measurements and Applications, Benevento, Italy, 15–18 May 2016. [Google Scholar]
- Subhagya, D.S.; Keshava, M.C.; Aruna, N.; Janardhan, L.; Ramakrishna, H.S. Case study on measurement of SpO2 from PPG Signals in the presence of motion artifact. In Proceedings of the 2017 International Conference on Recent Advances in Electronics and Communication Technology, Bangalore, India, 16–17 March 2017. [Google Scholar]
- Mishra, D.; Priyadarshini, N.; Chakraborty, S.; Sarkar, M. Blood oxygen saturation measurement using polarization-dependent optical sectioning. IEEE Sens. 2017, 17, 3900–3908. [Google Scholar] [CrossRef]
- Fung, P.; Dumont, G.; Ries, C.; Mott, C.; Ansermino, M. Cuff less continuous non-invasive blood pressure. measurement using pulse transit time measurement. In Proceedings of the 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, 1–5 September 2004; pp. 1–5. [Google Scholar]
- Liu, J.; Yan, B.P.Y.; Dai, W.X.; Ding, X.-R.; Zhang, Y.T.; Zhao, N. Multi-wavelength photoplethysmography method for skin arterial pulse extraction. Biomed. Opt. Express 2016, 7, 4313–4326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- V-TRUST Oxymeter TD-8250A Pulse. Available online: https://www.goapotik.com/pulse-oxymeter-v-trust-td-8250a.html (accessed on 16 June 2018).
- Omron HEM-7121 Standard Blood Pressure Monitor. Available online: https://www.omronhealthcare.com.hk/en/product/ins.php?index_prm_id=15&index_id=12&pr_show_status=1 (accessed on 16 June 2019).
- Thomas, P.W.; Burrus, C.S. Digital Filter Design; John Wiley & Sons: New York, NY, USA, 1987; p. 83. [Google Scholar]
- AMS-AS7265X Smart Spectral Sensor. Available online: https://ams.com/as7265x (accessed on 16 June 2018).
- STS-VIS Data Sheet. Available online: http://oceanoptics.com/product/sts-vis-microspectrometer/ (accessed on 16 June 2018).

| Sensor Venders | # of Channels | Synchronous/Sequential Measurement | Cost | Size |
|---|---|---|---|---|
| The developed MW-PPG sensor | 15 | Synchronous | Low | Small |
| AFE4404 (Texas Instruments) [26] | 3 | Sequential | Low | Small |
| BH1790GLC (ROHM Semiconductor) [27] | 1 | Sequential | Low | Small |
| MAX30102 (Maxim Integrated) [28] | 2 | Sequential | Low | Small |
| AS73210 (AMS AG) [44] | 6 | Synchronous | Low | Small |
| STS-VIS (Ocean Optics) [45] | >100 | Synchronous | Very high | Very large |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, C.-C.; Wu, C.-T.; Choi, B.I.; Fang, T.-J. MW-PPG Sensor: An on-Chip Spectrometer Approach. Sensors 2019, 19, 3698. https://doi.org/10.3390/s19173698
Chang C-C, Wu C-T, Choi BI, Fang T-J. MW-PPG Sensor: An on-Chip Spectrometer Approach. Sensors. 2019; 19(17):3698. https://doi.org/10.3390/s19173698
Chicago/Turabian StyleChang, Cheng-Chun, Chien-Ta Wu, Byung Il Choi, and Tong-Jing Fang. 2019. "MW-PPG Sensor: An on-Chip Spectrometer Approach" Sensors 19, no. 17: 3698. https://doi.org/10.3390/s19173698
APA StyleChang, C.-C., Wu, C.-T., Choi, B. I., & Fang, T.-J. (2019). MW-PPG Sensor: An on-Chip Spectrometer Approach. Sensors, 19(17), 3698. https://doi.org/10.3390/s19173698




