A Wearable Combined Wrist Pulse Measurement System Using Airbags for Pressurization
Abstract
:1. Introduction
2. System Architecture and Validation
2.1. Signal Acquisition and Processing
2.2. Principle and Calibration of Pressurization
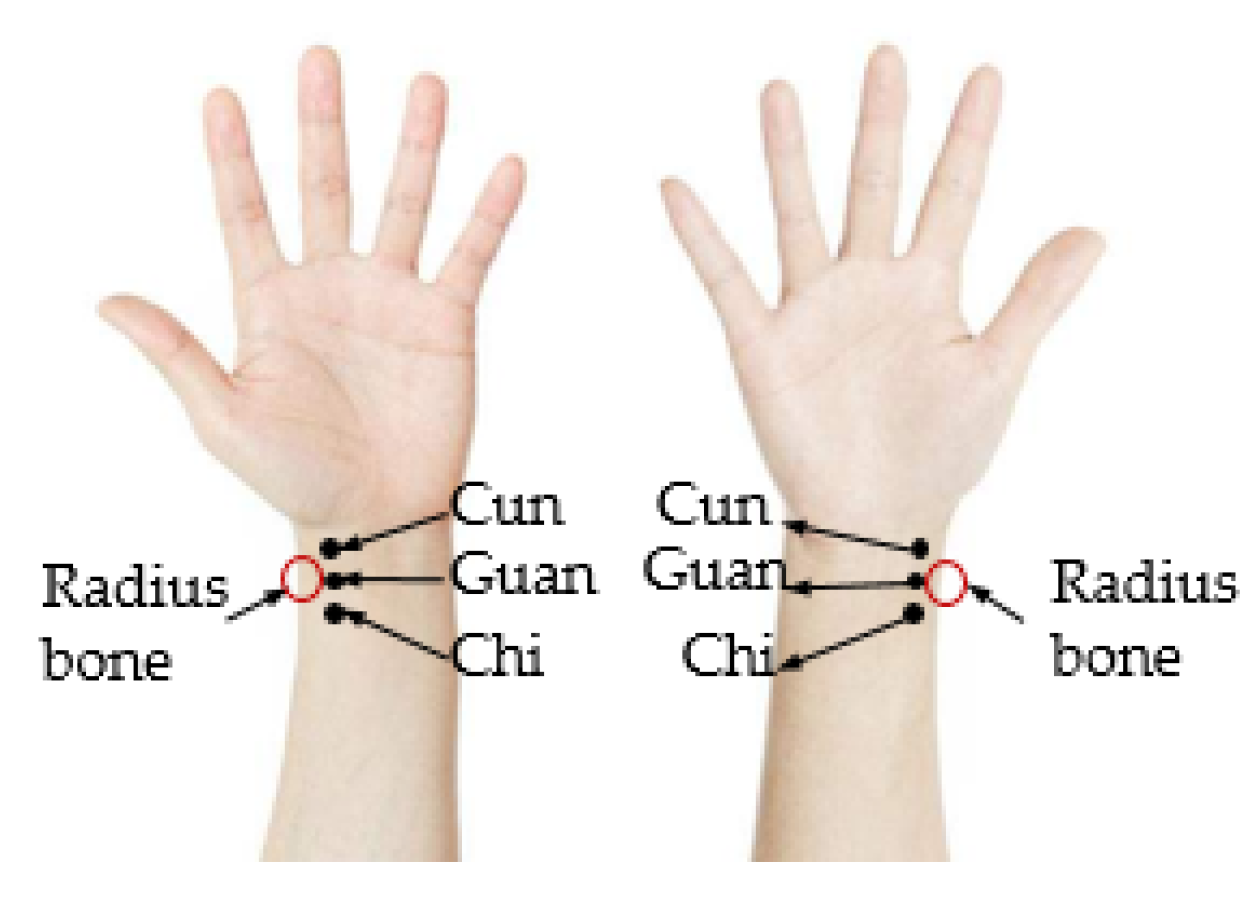
2.3. Position Adjusting
2.4. Validation of the System
3. Results
3.1. Single-Region Measurement Experiment
3.2. Three-Region Measurement Experiment
4. Discussions
Author Contributions
Funding
Conflicts of Interest
References
- Hu, J.; Liu, B. The basic theory, diagnostic, and therapeutic system of traditional Chinese medicine and the challenges they bring to statistics. Stat. Med. 2012, 31, 602–605. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Chang, R.S.; Jwo, K.W.; Hsu, C.C.; Tsao, C.P. A non-contact pulse automatic positioning measurement system for traditional Chinese medicine. Sensors 2015, 15, 9899–9914. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.T.; Wei, L.Y. Spectrum analysis of human pulse. IEEE Trans. Biomed. Eng. 1983, BME-30, 348–352. [Google Scholar] [CrossRef]
- Chu, Y.-W.; Luo, C.-H.; Chung, Y.-F.; Hu, C.-S.; Yeh, C.-C. Using an array sensor to determine differences in pulse diagnosis—Three positions and nine indicators. Eur. J. Integr. Med. 2014, 6, 516–523. [Google Scholar] [CrossRef]
- Zou, C.M.; Jiang, S.H.; Yan, J.J.; Guo, R.; Yan, H.X.; Liu, G.P.; Wang, Y.Q.; Liu, M.S. Analysis of TCM Pulse Instrument Development Progress; World Scientific Publishing Co Pte Ltd.: Singapore, 2016; pp. 69–75. [Google Scholar]
- Wang, Y.Q. Progress and prospect of objectivity study on four diagnostic methods in traditional Chinese medicine. In Proceedings of the IEEE International Conference on Bioinformatics and Biomedicine Workshops, Hong Kong, China, 18–18 December 2010. [Google Scholar]
- Chung, Y.-F.; Hu, C.-S.; Luo, C.-H.; Yeh, C.-C.; Si, X.-C.; Feng, D.-H.; Yeh, S.-M.; Liang, C.-H. Possibility of quantifying tcm finger-reading sensations: II. An example of health standardization. Eur. J. Integr. Med. 2012, 4, e263–e270. [Google Scholar] [CrossRef]
- Malinauskas, K.; Palevicius, P.; Ragulskis, M.; Ostasevicius, V.; Dauksevicius, R. Validation of noninvasive moems-assisted measurement system based on ccd sensor for radial pulse analysis. Sensors 2013, 13, 5368–5380. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.H.; Chang, R.S.; Jiang, J.A. A novel pulse measurement system by using laser triangulation and a cmos image sensor. Sensors 2007, 7, 3366–3385. [Google Scholar] [CrossRef] [PubMed]
- Lin Wang, Y.-Y.; Sze, W.-K.; Bau, J.-G.; Wang, S.-H.; Jan, M.-Y.; Hsu, T.-L.; Wang, W.-K. The ventricular-arterial coupling system can be analyzed by the eigenwave modes of the whole arterial system. Appl. Phys. Lett. 2008, 92, 153901. [Google Scholar] [CrossRef]
- HyunDae, H.; Fox, M.D. No touch pulse measurement by optical interferometry. IEEE Trans. Biomed. Eng. 1994, 41, 1096–1099. [Google Scholar] [CrossRef] [PubMed]
- Kan-heng, Z.; Peng, Q.; Chun-ming, X.; Yi-qin, W. Research on a Novel Three-Channel Self-Pressurized Wrist Pulse Acquisition System. In Biomedical Engineering Systems and Technologies; Springer: Cham, Germany, 2015; pp. 49–59. [Google Scholar]
- Wang, D.; Zhang, D.; Lu, G. An optimal pulse system design by multichannel sensors fusion. IEEE J. Biomed. Health Inform. 2016, 20, 450–459. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Zuo, W.; Zhang, H.; Zhang, D. Design and implementation of a multi-channel pulse signal acquisition system. In Proceedings of the 5th International Conference on BioMedical Engineering and Informatics, Chongqing, China, 16–18 October 2012. [Google Scholar]
- Joshi, A.; Kulkarni, A.; Chandran, S.; Jayaraman, V.K.; Kulkarni, B.D. Nadi tarangini: A pulse based diagnostic system. In Proceedings of the 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007. [Google Scholar]
- Giri, D.; Rajendra Acharya, U.; Martis, R.J.; Vinitha Sree, S.; Lim, T.-C.; Ahamed, T.; Suri, J.S. Automated diagnosis of coronary artery disease affected patients using LDA, PCA, ICA and discrete wavelet transform. Knowl. Based Syst. 2013, 37, 274–282. [Google Scholar] [CrossRef]
- Warren, K.M.; Harvey, J.R.; Chon, K.H.; Mendelson, Y. Improving pulse rate measurements during random motion using a wearable multichannel reflectance photoplethysmograph. Sensors 2016, 16, 342. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, Y.; Dao, D.K.; Chon, K.H. Multi-Channel Pulse Oximetry for Wearable Physiological Monitoring; IEEE: New York, NY, USA, 2013. [Google Scholar]
- King, E.; Cobbin, D.; Walsh, S.; Ryan, D. The reliable measurement of radial pulse characteristics. Acupunct. Med. 2002, 20, 150. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Lee, J.; Lee, H.J.; Kim, J.Y. A Study on Correlation between BMI and Oriental Medical Pulse Diagnosis Using Ultrasonic Wave. In Proceedings of the 13th International Conference on Biomedical Engineering, Singapore, 3–6 December 2008; Lim, C.T., Goh, J.C.H., Eds.; Springer: Berlin/Heidelberg, Germany, 2009; pp. 2052–2055. [Google Scholar]
- Kim, J.U.; Jeon, Y.J.; Lee, Y.J.; Kim, K.H.; Kim, J.Y. Novel diagnostic algorithm for the floating and sunken pulse qualities and its clinical test. Evid. Based Complement. Alternat. Med. 2011, 2011, 813427. [Google Scholar] [CrossRef] [PubMed]
- Kabigting, J.E.T.; Chen, A.D.; Chang, E.J.; Lee, W.; Roberts, R.C. Mems pressure sensor array wearable for traditional Chinese medicine pulse-taking. In Proceedings of the IEEE 14th International Conference on Wearable and Implantable Body Sensor Networks (BSN), Eindhoven, The Netherlands, 9–12 May 2017. [Google Scholar]















| Subject No. | Heart Rate (bpm) | Error (%) | BMI | Best Pulse-Taking Pressure (gf) | |||
|---|---|---|---|---|---|---|---|
| YX-303 | Proposed System | Cun | Guan | Chi | |||
| 1 | 96 | 97 | 1.04 | 14.2 | 51.84 | 49.11 | 70.87 |
| 2 | 93 | 93 | 0 | 16.9 | 57.37 | 58.37 | 66.54 |
| 3 | 70 | 71 | 1.43 | 18.3 | 65.71 | 68.34 | 70.82 |
| 4 | 70 | 71 | 1.43 | 19.1 | 68.30 | 67.07 | 73.03 |
| 5 | 87 | 88 | 1.15 | 19.6 | 72.03 | 69.12 | 75.24 |
| 6 | 94 | 94 | 0 | 20.7 | 79.65 | 77.01 | 86.88 |
| 7 | 88 | 89 | 1.14 | 21.9 | 90.75 | 78.91 | 83.07 |
| 8 | 80 | 79 | 1.25 | 22.3 | 89.57 | 80.03 | 98.94 |
| 9 | 73 | 74 | 1.37 | 22.8 | 92.56 | 94.31 | 104.03 |
| 10 | 73 | 73 | 0 | 23.7 | 105.58 | 105.55 | 105.47 |
| 11 | 80 | 80 | 0 | 24.7 | 102.56 | 113.70 | 117.42 |
| 12 | 80 | 79 | 1.25 | 25.0 | 108.76 | 110.31 | 114.49 |
| Subject No. | Pulse Rate | Best Pulse-Taking Pressure | ||||
|---|---|---|---|---|---|---|
| Average (bpm) | SD (bpm) | RE (%) | Average (gf) | SD (gf) | RE (%) | |
| 13 | 84 | 0.6 | 0.73 | 100.72 | 1.83 | 1.81 |
| 14 | 79 | 1.2 | 1.53 | 95.69 | 2.34 | 2.45 |
| 15 | 70 | 1.2 | 1.72 | 102.17 | 2.23 | 2.18 |
| System | Peng Wang [14] | Zhou [12] | Jessica [22] | Proposed |
|---|---|---|---|---|
| Wearable wristbands | No | No | Yes | Yes |
| Combined and detachable | No | No | No | Yes |
| Position adjustable | Yes | Yes | No | Yes |
| Pressurization method | Motor and shaft | Motor and shaft | Manually | Pump and air bag |
| Number of sensors | Sensor array | Three | Three | Three |
| Sampling frequency | Above 50 Hz | 1000 Hz | 11 Hz | 1000 Hz |
| Continuous decompression measurement | No | No | No | Yes |
| Pulse-taking pressure acquiring | Yes | Yes | No | Yes |
| Year of publication | 2012 | 2015 | 2017 | 2019 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, C.; Xia, C.; Zhang, S.; Wang, L.; Wang, Y.; Yan, H. A Wearable Combined Wrist Pulse Measurement System Using Airbags for Pressurization. Sensors 2019, 19, 386. https://doi.org/10.3390/s19020386
Jin C, Xia C, Zhang S, Wang L, Wang Y, Yan H. A Wearable Combined Wrist Pulse Measurement System Using Airbags for Pressurization. Sensors. 2019; 19(2):386. https://doi.org/10.3390/s19020386
Chicago/Turabian StyleJin, Chenling, Chunming Xia, Shiyu Zhang, Liren Wang, Yiqin Wang, and Haixia Yan. 2019. "A Wearable Combined Wrist Pulse Measurement System Using Airbags for Pressurization" Sensors 19, no. 2: 386. https://doi.org/10.3390/s19020386
APA StyleJin, C., Xia, C., Zhang, S., Wang, L., Wang, Y., & Yan, H. (2019). A Wearable Combined Wrist Pulse Measurement System Using Airbags for Pressurization. Sensors, 19(2), 386. https://doi.org/10.3390/s19020386




