Toward an End-to-End Calibration for Mobile C-Arm in Combination with a Depth Sensor for Surgical Augmented Reality Applications
Abstract
:1. Introduction
1.1. Research Overview for AR systems with C-arm
1.2. Instability of C-arm Calibration Parameters
1.3. Contributions
2. Materials and Methodology
2.1. Pre-operative Step
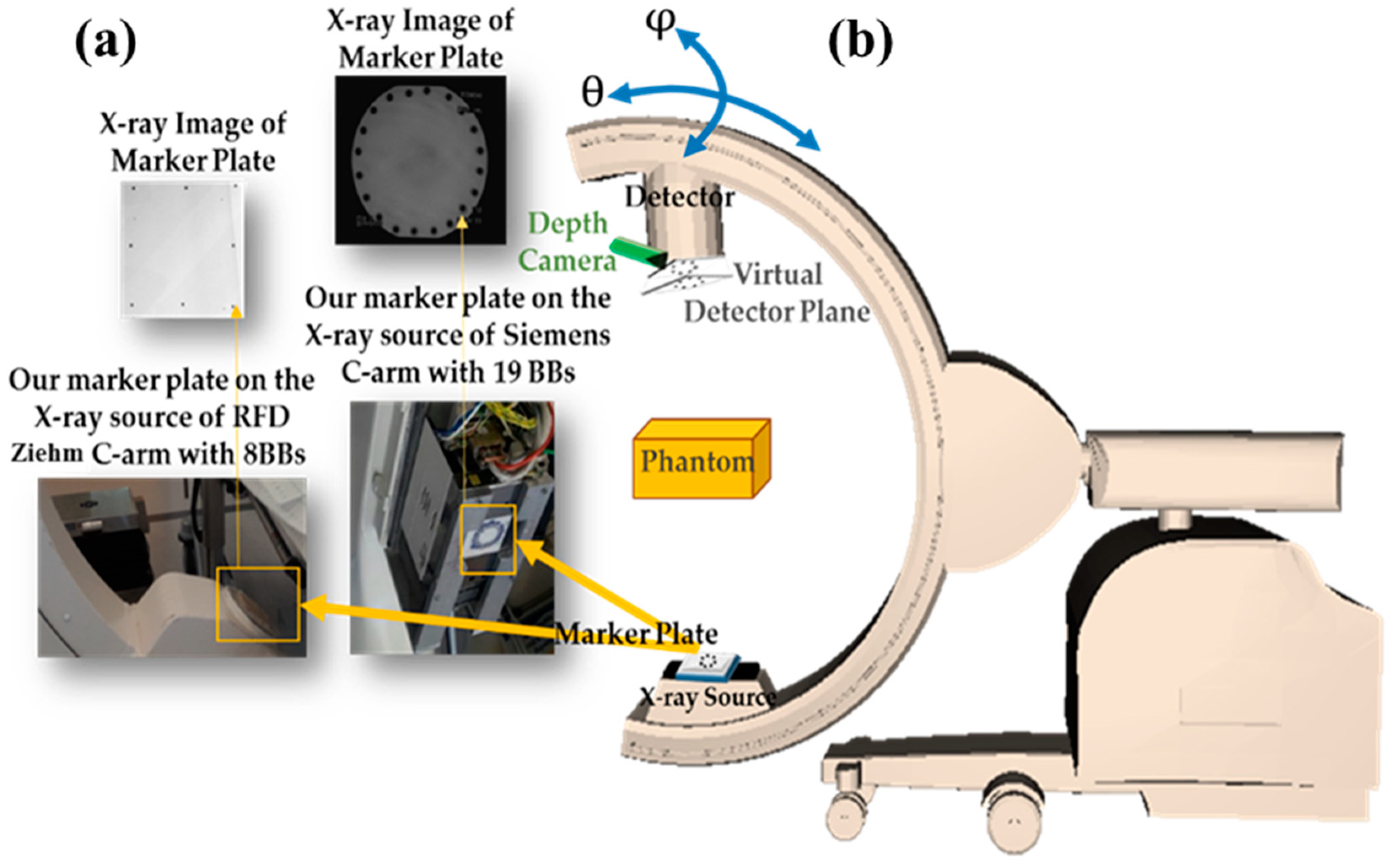
- Setup configuration, which consisted of (1) Designing the 3D phantom for the calibration, (considering geometric network configurations, such as point distribution in object space, convergent imaging, capturing portrait and landscape images, and applying a 3D target field which fills the format of the image to decouple calibration parameters [19]) with a robust procedure considering the limitations of C-arm; (2) Mounting a marker plate for virtual detector concept on the source considering the instability of C-arm calibration parameters; (3) Mounting an RGB-D camera on the C-arm detector for recovering C-arm pose with augmented reality. Then, X-ray images with video and depth images of the new multi-modal phantom could be captured simultaneously, with C-arm in a fixed position.
- Calibration step.
2.1.1. Setup Configuration
2.1.2. C-arm Calibration
2.1.3. 3D-2D Calibration for Surgical AR
2.2. Intra-Operative Step
2.2.1. C-arm Pose Estimation
2.2.2. Updating C-arm Intrinsic Parameters during Surgery by Virtual Detector
2.2.3. Visualization
3. Experimental Results
3.1. Experiments and Results of Pre-operative Step
3.2. Experiments and Results of Intra-operative Step
3.2.1. C-arm Pose Estimation
3.2.2. Results of Updating Intrinsic Parameters and Stability Analysis with a Marker Plate
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Navab, N.; Heining, S.; Traub, J. Camera augmented mobile C-arm (CAMC): Calibration, accuracy study, and clinical applications. IEEE Trans. Med. Imaging 2010, 29, 1412–1423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsai, R. A versatile camera calibration technique for high-accuracy 3D machine vision metrology using off-the-shelf TV cameras and lenses. IEEE J. Robot. Autom. 1987, 3, 323–344. [Google Scholar] [CrossRef] [Green Version]
- Hofstetter, R.; Slomczykowski, M.; Sati, M.; Nolte, L.P. Fluoroscopy as an Imaging Means for Computer-Assisted Surgical Navigation. Comput. Aided Surg. 1999, 4, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Kaptein, B.L.; Shelburne, K.B.; Torry, M.R.; Giphart, J.E. A comparison of calibration methods for stereo fluoroscopic imaging systems. J. Biomech. 2011, 44, 2511–2515. [Google Scholar] [CrossRef] [PubMed]
- Yaniv, Z.; Joskowicz, L.; Simkin, A.; Garza-Jinich, M.; Milgrom, C. Fluoroscopic image processing for computer-aided orthopedic surgery. In Proceedings of the International Conference on Medical Image Computing and Computer-Assisted Intervention, Cambridge MA, USA, 11–13 October 1998; pp. 325–334. [Google Scholar]
- Habert, S.; Gardiazabal, J.; Fallavollita, P.; Navab, N. RGBDX: First Design and Experimental Validation of a Mirror-Based RGBD X-ray Imaging System. In Proceedings of the 14th IEEE International Symposium on Mixed and Augmented Reality (ISMAR 2015), Fukuoka, Japan, 29 September–3 October 2015; pp. 13–18. [Google Scholar]
- Habert, S. Multi-Modal Visualization Paradigms for RGB-D Augmented X-ray Imaging. Ph.D. Thesis, Technische Universität München, Munich, Germany, 2018. [Google Scholar]
- Habert, S.; Meng, M.; Kehl, W.; Wang, X.; Tombari, F.; Fallavollita, P.; Navab, N. Augmenting Mobile C-arm Fluoroscopes via Stereo-RGBD Sensors for Multimodal Visualization. In Proceedings of the 14th IEEE International Symposium on Mixed and Augmented Reality (ISMAR 2015), Fukuoka, Japan, 29 September–3 October 2015; pp. 72–75. [Google Scholar]
- Zhang, Z. A Flexible New Technique for Camera Calibration. IEEE Trans. Pattern Anal. Mach. Intell. 2000, 22, 1330–1334. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Habert, S.; Ma, M.; Huang, C.H.; Fallavollita, P.; Navab, N. Precise 3D/2D calibration between an RGB-D sensor and a C-arm fluoroscope. Int. J. Comput. Assist. Radiol. Surg. 2016, 11, 1385–1395. [Google Scholar] [CrossRef] [PubMed]
- Groher, M. Development of a Planning and Navigation Tool for Endoscopic Treatment of Aortic Aneurysms-Computer Supported Implantation of a Stent Graft. Ph.D. Thesis, Technische Universität München, Munich, Germany, 2003. [Google Scholar]
- Wang, L. Novel Techniques for Integrating Video Augmented X-ray Imaging into Orthopedic and Trauma Surgery. Ph.D. Dissertation, Technische Universität München, Munich, Germany, 2012. [Google Scholar]
- Wang, X.; Habert, S.; Berge, C.S.; Fallavollita, P.; Navab, N. Inverse visualization concept for RGB-D augmented C-arms. Comput. Biol. Med. 2016, 77, 135–147. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Habert, S.; Ma, M.; Huang, C.H.; Fallavollita, P.; Navab, N. RGB-D/C-arm Calibration and Application in Medical Augmented Reality. In Proceedings of the 14th IEEE International Symposium on Mixed and Augmented Reality (ISMAR 2015), Fukuoka, Japan, 29 September–3 October 2015; pp. 100–103. [Google Scholar]
- Ha, H.; Jeon, S.; Lee, S.; Choi, H.; Hong, J. Perspective Pinhole Model with Planar Source for Augmented Reality Surgical Navigation Based on C-Arm Imaging. Int. J. Comput. Assist. Radiol. Surg. 2018, 13, 1671–1682. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.C.; Fuerst, B.; Fotouhi, J.; Fischer, M.; Osgood, G.; Navab, N. Calibration of RGB-D camera and cone-beam CT for 3D intra-operative mixed reality visualization. Int. J. Comput. Assist. Radiol. Surg. 2016, 11, 967–975. [Google Scholar] [CrossRef] [PubMed]
- Navab, N.; Mitschke, M.; Schütz, O. Camera-augmented mobile C-arm (CAMC) application: 3D reconstruction using a low-cost mobile C-arm. In Proceedings of the Medical Image Computing and Computer-Assisted Intervention–MICCAI’99, Cambridge, UK, 19–22 September 1999; pp. 688–697. [Google Scholar]
- Kaplan, D.J.; Patel Jay, N.; Liporace Frank, A.; Yoon Richard, S. Intraoperative Radiation Safety in Orthopaedics: A Review of the ALARA (as Low as Reasonably Achievable) Principle. Patient Saf. Surg. 2016, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Remondino, F.; Fraser, C. Digital camera calibration methods: Considerations and comparisons. Int. Arch. Photogramm Remote. Sens. Spat. Inf. Sci. 2006, 36, 266–272. [Google Scholar]
- Kedgley, A.E.; Fox, A.M.V.; Jenkyn, T.R. Image intensifier distortion correction for fluoroscopic RSA: The need for independent accuracy assessment. J. Appl. Clin. Med Phys. 2012, 13, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Lichti, D.; Sharma, G.B.; Kuntze, G.; Mund, B.; Beveridge, J.E.; Ronsky, J.L. Rigorous geometric self-calibrating bundle adjustment for a dual fluoroscopic imaging system. IEEE Trans. Med. Imaging 2015, 34, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Al-Durgham, K.; Lichti, D.; Kuntze, G.; Sharma, G.; Ronsky, J. Toward an Automatic Calibration of Dual Fluoroscopy Imaging Systems. In Proceedings of the International Archives of the Photogrammetry, Remote Sensing and Spatial Information Sciences, Volume XLI-B5, 2016 XXIII ISPRS Congress, Prague, Czech Republic, 12–19 July 2016. [Google Scholar]
- Fraser, C. Automatic Camera Calibration in Close-Range Photogrammetry. Photogramm. Eng. Rem. Sens. 2012, 79, 381–388. [Google Scholar] [CrossRef] [Green Version]
- Hosseinian, S.; Arefi, H. Assessment of Restoration Methods of X-Ray Images with Emphasis on Medical Photogrammetric Usage. In Proceedings of the International Archives of the Photogrammetric, Remote Sensing and Spatial Information Sciences, 2016 XXIII ISPRS Congress, Prague, Czech Republic, 12–19 July 2016. [Google Scholar]
- Cerveri, P.; Forlani, C.; Borghese, N.A.; Ferrigno, G. Distortion correction for x-ray image intensifiers: Local unwarping polynomials and RBF neural networks. Med. Phys. 2002, 29, 1759–1771. [Google Scholar] [CrossRef] [PubMed]
- Triggs, B.; McLauchlan, P.F.; Hartley, R.I.; Fitzgib-bon, A.W. Bundle Adjustmenta Modern Synthesis. In Proceedings of the International Workshop on Vision Algorithms, Corfu, Greece, 21–22 September 1999. [Google Scholar]
- Hosseinian, S.; Arefi, H.; Navab, N. C-Arm Pose Estimation and Navigation in Surgeries for Augmented Reality Application. Int. Arch. Photogramm. Remote Sens. Spatial Inf. Sci. 2019, XLII-4/W18, 497–505. [Google Scholar] [CrossRef] [Green Version]
- Myronenko, A.; Song, X. Point set registration: Coherent Point Draft. IEEE Trans. Pattern Anal. Mach. Intell. 2010, 32, 2262–2275. [Google Scholar] [CrossRef] [PubMed] [Green Version]









| Proposed Method with designed phantoms: | C-arm device | Phantom type | Material | Number of levels | Number of BBs | RMSE (Pixel) |
| Siemens Siemens Siemens Ziehm | 3D 3D 3D 3D | Lego Lego Lego Lego | 3 4 7 7 | 31 32 95 95 | 1.21 0.96 0.33 0.23 | |
| Previous Reference Systems: [7] CAMC [12] Zhang’s method [12] | C-arm Device Siemens Siemens Siemens | Phantom type 2D - 2D | Material PCB (Printed Circuit Board) - PCB (Printed Circuit Board) | Number of levels 1 1 | Number of BBs >200 >200 | RMSE (Pixel) 0.37 1.02 0.48 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hosseinian, S.; Arefi, H.; Navab, N. Toward an End-to-End Calibration for Mobile C-Arm in Combination with a Depth Sensor for Surgical Augmented Reality Applications. Sensors 2020, 20, 36. https://doi.org/10.3390/s20010036
Hosseinian S, Arefi H, Navab N. Toward an End-to-End Calibration for Mobile C-Arm in Combination with a Depth Sensor for Surgical Augmented Reality Applications. Sensors. 2020; 20(1):36. https://doi.org/10.3390/s20010036
Chicago/Turabian StyleHosseinian, Sahar, Hossein Arefi, and Nassir Navab. 2020. "Toward an End-to-End Calibration for Mobile C-Arm in Combination with a Depth Sensor for Surgical Augmented Reality Applications" Sensors 20, no. 1: 36. https://doi.org/10.3390/s20010036





